Abstract
Increasing access to mental health and substance use services, particularly through integrated care models, as well as addressing issues of HIV-related stigma, may positively impact engagement in HIV clinical care.
The VHA is the largest single provider of human immunodeficiency virus (HIV) care in the U.S., with over 26,000 HIV-positive veterans in care in 2013.1 HIV care in the VHA is delivered across 152 hospitals and nearly 1,400 health care facilities, including community-based outpatient clinics, skilled nursing facilities, veteran centers, rehabilitation centers, hospices, and domiciliaries in the U.S. and its territories.2
The structure of HIV care in the VHA has been described in more detail elsewhere and, for context, is briefly highlighted here.3 Many veterans with HIV infection receive both HIV care and primary care through an infectious disease or HIV specialist, whereas others receive HIV care and primary care in separate clinics. Every medical center has a designated HIV lead clinician who serves as the point of contact for the VHA National HIV Program. This network facilitates rapid dissemination of policy changes and clinical updates to HIV providers nationally, as well communication to the National HIV Program about barriers and challenges to providing high-quality care at the local level. The National HIV Program monitors and evaluates comprehensive HIV care programming, which includes increasing HIV testing, availability of pre-exposure prophylaxis, and access to and quality of comorbidity care (for more information on VHA HIV care, please visit: http://www.hiv.va.gov).
Comorbidity care is a particular focus of the National HIV Program. The majority of veterans with HIV in VHA care are now in late middle-age; in 2011, 66% were aged between 50 and 69 years.4 As the population of veterans with HIV grows older, age-related chronic medical comorbidities (eg, diabetes mellitus, cardiovascular disease) and mental health considerations (eg, cognitive impairment, depression, substance use) become increasingly critical areas of clinical focus at the individual and the population level.
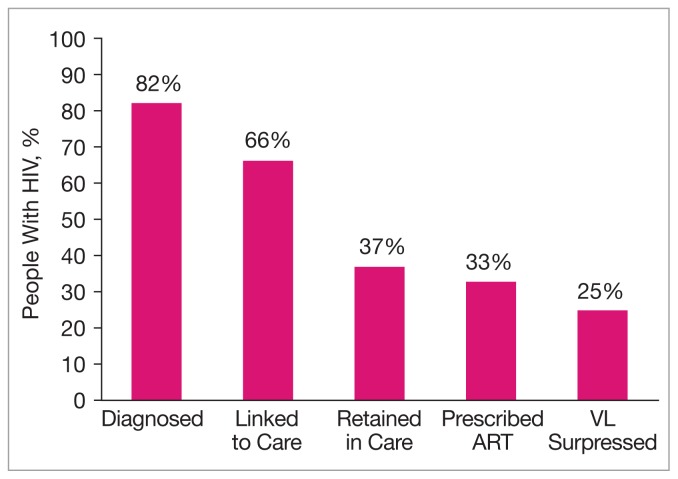
The HIV care continuum provides a useful model to conceptualize critical components of providing high-quality comprehensive HIV clinical care, including diagnosis, linkage to care, retention in care, prescription of antiretroviral therapy (ART), and viral suppression. Achieving virologic suppression is the primary goal of HIV care. It decreases morbidity and mortality for the HIV-infected individual and decreases the risk of transmission to others.5
This continuum of care is used increasingly by federal agencies and other health care systems to assess engagement at each critical juncture. The Centers for Disease Control and Prevention has estimated that, due to significant drop-offs between each step of the continuum, only 25% of the 1.1 million people living with HIV in the U. S. are virally suppressed (Figure 1).6,7
Figure 1.
HIV Care Continuum in the U.S.7
Abbreviations: ART, antiretroviral therapy; HIV, human immunodeficiency virus; VL, HIV viral load.
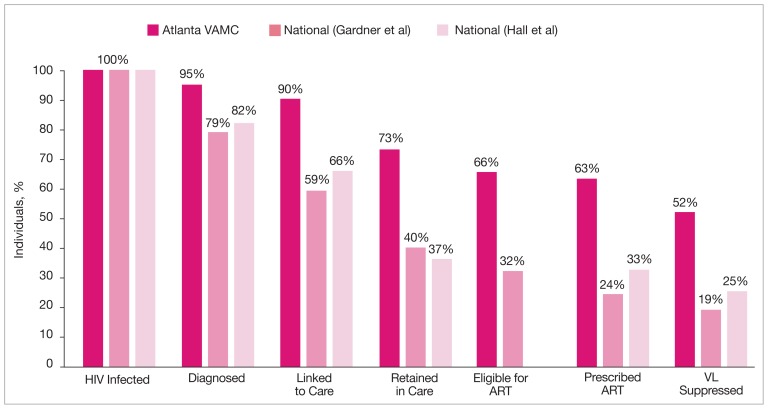
Recently, the HIV care continuum cascade was used to assess HIV care within a VA medical facility.8 The authors assessed performance along the HIV care continuum at the Atlanta VAMC (AVAMC) Infectious Disease Clinic, an urban clinic providing care to over 1,400 veterans with HIV. Using an independent stage categorization analysis, they found that the AVAMC outperformed national estimates at every stage of the HIV care continuum. Notably, 62.8% of the clinical population diagnosed with HIV was prescribed ART and 52.3% had achieved viral suppression, more than double the national rate (Figure 2).8–10 Although national VHA data on the HIV Care Continuum Initiative are not currently available, this study helps to illustrate the high quality of HIV care in the VHA relative to other national samples.
Figure 2.
VA Facility-Level Performance Across the HIV Care Continuum Compared With National Samples8–10,a
Reprinted with permission from AIDS RESEARCH AND HUMAN RETROVIRUSES, 2014, published by Mary Ann Liebert, Inc., New Rochelle, NY.
Abbreviations: ART, antiretroviral therapy; HIV, human immunodeficiency virus; VL, HIV viral load.
a Proportions of people living with HIV and receiving care at the Atlanta VAMC who are engaged in selected stages of the continuum of HIV care where stages are dependent subsets of upstream stages (dark pink) vs national proportions of HIV-infected individuals engaged in selected stages of the cascade of HIV care as estimated by Gardner et al9 (pink) and Hall et al10 (light pink).
MENTAL HEALTH AND SUBSTANCE USE
Although individual facilities within VHA may perform better across the care continuum compared with national samples, as a health care system, significant drop-offs remain at each stage, particularly in the transition from linkage to care to retention in care. The barriers to engagement in care at various steps along this continuum are not well understood, although mental health and substance use disorder (MH/SUD) comorbidities likely play an important role.
Mental health and substance use disorder comorbidities impact over half of veterans with HIV infection in VHA care. In 2012, 55% of veterans with HIV infection in care had ever been diagnosed with depression, 31% with anxiety, 16% with posttraumatic stress disorder (PTSD), and 62% with any mental illness (Table).11 Substance use is also quite prevalent in veterans with HIV infection, with 34% reporting a history of alcohol abuse, 28% a history of stimulant use, and 16% a history of cannabis use in 2012; nearly 50% reported tobacco use.
Table.
| HIVb | |||
|---|---|---|---|
| Comorbid Condition Group | Comorbid Condition | Patients With Ever Diagnosis, No. | Patients With Ever Diagnosis, % |
| Mental health | Bipolar disorder | 2,482 | 10% |
| Depression | 14,416 | 55% | |
| Neuroses and anxiety states | 8,019 | 31% | |
| Posttraumatic stress disorder | 4,291 | 16% | |
| Schizophrenia | 1,720 | 7% | |
| Any mental illness | 16,193 | 62% | |
| Substance use | Alcohol use | 8,810 | 34% |
| Cannabis | 4058 | 16% | |
| Opioids | 3021 | 12% | |
| Other and unspecified drug use | 6544 | 25% | |
| Sedatives and anxiolytics | 475 | 2% | |
| Stimulants | 7223 | 28% | |
| Tobacco use | 12,381 | 48% | |
Data from National HIV Registry Reports: 2012 personal communication from Office of Public Health/Population Health.1
Number of veterans in care in year used as denominator: 26,033.
Compared with that of the general population, MH/SUDs are much higher among people living with HIV/acquired immune deficiency syndrome (AIDS) and higher still among veterans living with HIV/AIDS.11–13 Mental health conditions such as depression, anxiety, and PTSD as well as substance use have been linked not only to increases in HIV risk behavior, but also to more rapid progression of HIV and increases in AIDS-defining illnesses and death.14–16 The high burden of MH/SUD among veterans with HIV is further complicated by the fact that this is an aging population. The risk of HIV-associated neurocognitive disorders (HAND) as well as non–HIV-related neurocognitive disorders increases with age.17,18 These risks may be higher for those with comorbid MH/SUD, and this interaction may increase patients’ vulnerability to HAND.12,19,20
The HIV care continuum is characterized by engagement at each step. Psychiatric and substance use problems represent potential engagement-limiting comorbidities. Several studies highlight the importance of addressing MH/SUDs that have adverse effects on adherence, linkage to and retention in care, and care utilization patterns.13,18,21–24 HIV-related stigma may also play a significant role in disengagement in care, adherence, patient satisfaction with care, and follow-up.25–28
Overall, integrated HIV care has been found to positively impact hospital utilization, quality of life and functioning, adherence, patient satisfaction, and process outcomes.29 Integrated HIV care is a specific intervention that could positively impact the HIV care continuum, particularly in managing depression and substance use.28,30,31 In the VHA, integrated HIV care is associated with increased access to mental health services and increased viral suppression compared with nonintegrated HIV clinics in VHA.32,33
A qualitative study of care integration found that in VHA HIV clinics that were integrated, patients reported less stigma and more positive relationships with their providers.34 The VHA Office of Public Health, in collaboration with the Office of Academic Affiliations, has supported the expansion of a postdoctoral fellowship in clinical psychology with a specific focus on integrated HIV and hepatitis C clinical care in an effort to increase the availability of mental health providers specifically trained to address MH/SUDs in the HIV-infected population. This national fellowship program has been described in detail elsewhere.11
CONCLUSION
The HIV care continuum is a useful model to describe the cascade of HIV care and opportunities for points of engagement. Although VHA may be performing higher along the care continuum than national samples, there is still much work to be done to better understand the barriers to engagement and interventions that will boost each step so that more veterans with HIV infection achieve viral suppression.
Increasing access to mental health and substance use services, particularly through integrated care models, as well as addressing issues of HIV-related stigma, may positively impact engagement in HIV clinical care. Given the use of electronic medical records, the availability of MH/SUD treatment, and the increasing emphasis on integrated HIV care at multiple facilities across the system, the VHA is well positioned to address gaps in care, with a particular focus on the role that MH/SUDs have in HIV care continuum drop-offs.
Footnotes
Author disclosures:
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
References
- 1.Office of Public Health/Population Health. National HIV Registry Reports: 2013. Personal Communication October 1, 2014.
- 2.Veterans Health Administration. Where do I get the care I need? VA website. [Accessed October 3, 2014]. http://www.va.gov/health/findcare.asp.
- 3.Maier M, Chartier M. Department of Veterans Affairs: HIV program, policies, and infrastructure. HIV Specialist. 2014;6(2):19–25. [Google Scholar]
- 4.Center for Quality Management in Public Health. The State of Care for Veterans with HIV/AIDS: 2011 Summary Report. Washington, DC: U.S. Department of Veterans Affairs; 2012. [Google Scholar]
- 5.Cohen MS, Chen YQ, McCauley M, et al. HPTN 052 Study Team. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.HIV/AIDS Care Continuum. AIDS.gov Website. [Accessed October 6, 2014]. http://aids.gov/federal-resources/policies/care-continuum. Updated December 18, 2013.
- 7.National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Key graphics from CDC analysis showing proportion of people engaged in each of the five main stages of HIV care. Centers for Disease Control and Prevention Website. [Accessed November 18, 2014]. http://www.cdc.gov/nchhstp/newsroom/2012/Continuum-of-Care-Graphics.html. Updated December 27, 2013.
- 8.Mangal JP, Rimland D, Marconi VC. The continuum of HIV care in a Veterans’ Affairs clinic. AIDS Res Hum Retroviruses. 2014;30(5):409–415. doi: 10.1089/aid.2013.0232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hall HI, Frazier EL, Rhodes P, et al. Differences in human immunodeficiency virus care and treatment among subpopulations in the United States. JAMA Intern Med. 2013;173(14):1337–1344. doi: 10.1001/jamainternmed.2013.6841. [DOI] [PubMed] [Google Scholar]
- 11.Chartier M, Blais RK, Steinberg T, et al. A psychology postdoctoral fellowship program in integrated HIV and hepatitis C clinical care: Rationale, progress and future directions. Training Educ Professional Psychol. doi: 10.1037/tep0000038. [DOI] [Google Scholar]
- 12.Hinkin CH, Castellon SA, Atkinson JH, Goodkin K. Neuropsychiatric aspects of HIV infection among older adults. J Clin Epidemiol. 2001;54(suppl 1):S44–S52. doi: 10.1016/s0895-4356(01)00446-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klinkenberg WD, Sacks S HIV/AIDS Treatment Adherence, Health Outcomes and Cost Study Group. Mental disorders and drug abuse in persons living with HIV/AIDS. AIDS Care. 2004;16(suppl 1):S22–S42. doi: 10.1080/09540120412331315303. [DOI] [PubMed] [Google Scholar]
- 14.Carrico AW, Riley ED, Johnson MO, et al. Psychiatric risk factors for HIV disease progression: The role of inconsistent patterns of antiretroviral therapy utilization. J Acquir Immune Defic Syndr. 2011;56(2):146–150. doi: 10.1097/QAI.0b013e318201df63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leserman J. HIV disease progression: Depression, stress, and possible mechanisms. Biol Psychiatry. 2003;54(3):295–306. doi: 10.1016/s0006-3223(03)00323-8. [DOI] [PubMed] [Google Scholar]
- 16.Nurutdinova D, Abdallah AB, Bradford S, O’Leary CC, Cottler LB. Risk factors associated with hepatitis C among female substance users enrolled in community-based HIV prevention studies. BMC Res Notes. 2011;4:126. doi: 10.1186/1756-0500-4-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heaton RK, Clifford DB, Franklin DR, Jr, et al. CHARTER Group. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology. 2010;75(23):2087–2096. doi: 10.1212/WNL.0b013e318200d727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simoni JM, Amico KR, Smith L, Nelson K. Antiretroviral adherence interventions: Translating research findings to the real world clinic. Curr HIV/AIDS Rep. 2010;7(1):44–51. doi: 10.1007/s11904-009-0037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Becker JT, Lopez OL, Dew MA, Aizenstein HJ. Prevalence of cognitive disorders differs as a function of age in HIV virus infection. AIDS. 2004;18(suppl 1):S11–S18. [PubMed] [Google Scholar]
- 20.Valcour VG, Shikuma CM, Watters MR, Sacktor NC. Cognitive impairment in older HIV-1-seropositive individuals: Prevalence and potential mechanisms. AIDS. 2004;18(suppl 1):S79–S86. doi: 10.1097/00002030-200401001-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carrico AW, Bangsberg DR, Weiser SD, Chartier M, Dilworth SE, Riley ED. Psychiatric correlates of HAART utilization and viral load among HIV-positive impoverished persons. AIDS. 2011;25(8):1113–1118. doi: 10.1097/QAD.0b013e3283463f09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chartier M, Carrico AW, Weiser SD, Kushel MB, Riley ED. Specific psychiatric correlates of acute care utilization among unstably housed HIV-positive adults. AIDS Care. 2012;24(12):1514–1518. doi: 10.1080/09540121.2012.672720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Palmer NB, Salcedo J, Miller AL, Winiarski M, Arno P. Psychiatric and social barriers to HIV medication adherence in a triply diagnosed methadone population. AIDS Patient Care STDS. 2003;17(12):635–644. doi: 10.1089/108729103771928690. [DOI] [PubMed] [Google Scholar]
- 24.Sternhell PS, Corr MJ. Psychiatric morbidity and adherence to antiretroviral medication in patients with HIV/AIDS. Aust N Z J Psychiatry. 2002;36(4):528–533. doi: 10.1046/j.1440-1614.2002.00999.x. [DOI] [PubMed] [Google Scholar]
- 25.Chesney MA, Smith AW. Critical delays in HIV testing and care: The potential role of stigma. Am Behav Sci. 1999;42(7):1162–1174. [Google Scholar]
- 26.Li L, Comulada WS, Wu Z, Ding Y, Zhu W. Providers’ HIV-related avoidance attitude and patient satisfaction. Health Expect. 2013;16(1):105–112. doi: 10.1111/j.1369-7625.2011.00705.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kinsler JJ, Wong MD, Sayles JN, Davis C, Cunningham WE. The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care STDS. 2007;21(8):584–592. doi: 10.1089/apc.2006.0202. [DOI] [PubMed] [Google Scholar]
- 28.Treisman GJ. Impact of depression on ART adherence and retention in care. HIV Specialist. 2014;6(2):26–29. [Google Scholar]
- 29.Willenbring ML. Integrating care for patients with infectious, psychiatric, and substance use disorders: Concepts and approaches. AIDS. 2005;19(suppl 3):S227–S237. doi: 10.1097/01.aids.0000192094.84624.c2. [DOI] [PubMed] [Google Scholar]
- 30.Farber EW. Psychological aspects of HIV. HIV Specialist. 2013;6(4):10–13. [Google Scholar]
- 31.Durvasula R, Miller T. Management of substance abuse in HIV care. HIV Specialist. 2013;6(4):26–29. [Google Scholar]
- 32.Chartier M, Carmody T, Lamipris H. HIV psychology: Mental health integration and co-location. Poster presented at: The American Conference for the Treatment of HIV; May 20–23, 2010; Denver, CO. Poster SPC-6. [Google Scholar]
- 33.Hoang T, Goetz MB, Yano EM, et al. The impact of integrated HIV care on patient health outcomes. Med Care. 2009;47(5):560–567. doi: 10.1097/MLR.0b013e31819432a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fix GM, Asch SM, Saifu HN, Fletcher MD, Gifford AL, Bokhour BG. Delivering PACT-principled care: Are specialty care patients being left behind? J Gen Intern Med. 2014;29(suppl 2):S695–S702. doi: 10.1007/s11606-013-2677-9. [DOI] [PMC free article] [PubMed] [Google Scholar]