Abstract
Seemingly innocuous nontuberculous mycobacteria (NTM) species, classified by their slow or rapid growth rates, can cause a wide range of illnesses, from skin ulceration to severe pulmonary and disseminated disease. Despite their worldwide prevalence and significant disease burden, NTM do not garner the same financial or research focus as Mycobacterium tuberculosis. In this review, we outline the most abundant of over 170 NTM species and inadequacies of diagnostics and treatments and weigh the advantages and disadvantages of currently available in vivo animal models of NTM. In order to effectively combat this group of mycobacteria, more research focused on appropriate animal models of infection, screening of chemotherapeutic compounds, and development of anti-NTM vaccines and diagnostics is urgently needed.
Key learning points
Pulmonary diseases due to NTM are an increasing global health concern.
Prevalence of NTM is increasing in the US and has surpassed pulmonary tuberculosis (TB).
Successful treatment for NTM infection is complicated by the large number of NTM species (>170), difficulties with diagnosis, and few therapeutic options once diagnosed.
Mycobacterium avium complex (MAC) lung disease treatment is costly, lengthy, and often results in toxic side effects.
New therapeutic strategies are urgently needed, including more efficacious drugs with fewer adverse side effects and novel treatment options that could reduce treatment time and toxicity.
Prioritizing funding and research using NTM animal models to dissect NTM pathogenesis and host-directed responses and test novel therapeutic regimens against these infections may help combat these widespread pathogens.
Top five papers
Griffith DE, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367–416.
Haworth CS, et al. British Thoracic Society guidelines for the management of non-tuberculous mycobacterial pulmonary disease (NTM-PD). Thorax. 2017;72(Suppl 2):ii1-ii64.
Andrejak C, et al. Characterization of mouse models of Mycobacterium avium complex infection and evaluation of drug combinations. Antimicrobial agents and chemotherapy. 2015;59(4):2129–35.
Bryant J, et al. Emergence and spread of a human transmissible multidrug-resistant nontuberculous mycobacterium. Science. 2016;354:751.
Huh HJ, et al. Recent advances in molecular diagnostics and understanding mechanisms of drug resistance in nontuberculous mycobacterial diseases. Infection, Genetics and Evolution, https://doi.org/10.1016/j.meegid.2018.10.003.
Introduction
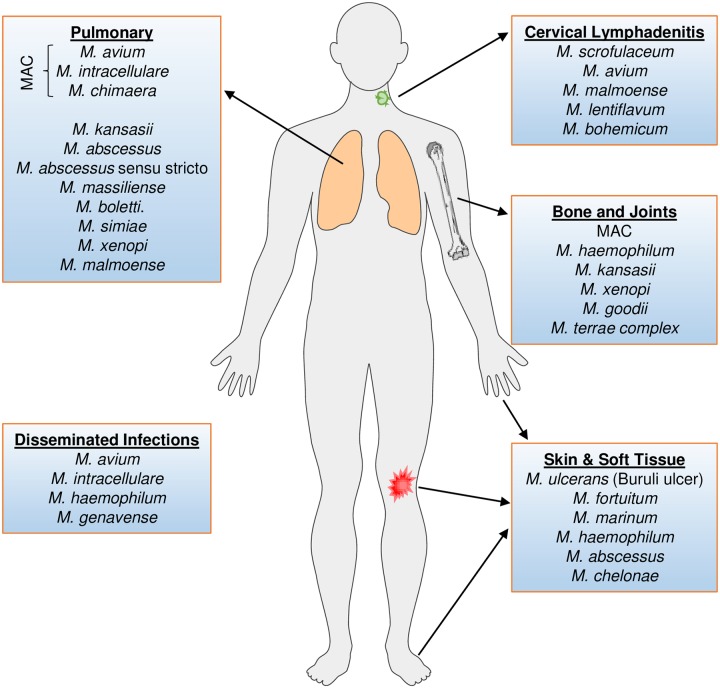
The nontuberculous mycobacteria (NTM), defined as any mycobacterial pathogen other than Mycobacterium tuberculosis (Mtb) or M. leprae, include over 170 different species varying in their ability to cause disease [1]. While some species are implicated worldwide (for example, M. avium complex [MAC], M. abscessus), others (for example, M. malmoense) are regionally significant [2]. NTM are geographically heterogeneous and cause a spectrum of diseases that include tuberculosis (TB)-like pulmonary and extrapulmonary disease, cervical lymphadenitis in young children, and visceral and disseminated disease (Fig 1). Pulmonary NTM infections are most commonly due to MAC, M. kansasii, and M. abscessus, which cause a substantive, often unappreciated, worldwide burden of illness. Although NTM may cause disease similar to Mtb, they generally do not respond to classic TB drug regimens, and therefore a misdiagnosis of Mtb can lead to poor treatment, particularly in resource-poor settings lacking diagnostic infrastructure. NTM-associated disease is more abundant than previously believed and is a quietly unfolding disease epidemic, even overtaking TB prevalence in some areas [3, 4]. A recent nationwide study in a low-TB–incidence country was performed on over half a million mycobacterial cultures to determine the annual incidence of culture-verified NTM disease from 1991 to 2015 [5]. Higher than anticipated incidence rates of disease caused by NTM in the study by Hermansen and colleagues were observed in very young children 0–4 years of age (5.36/105/year) and in older individuals (those aged 65–69; 2.39/105/year) [5]. In the United States, an increased prevalence of NTM-associated lung disease cases in people above 65 years of age has also been observed [6]. This bimodal age association with NTM incidence eludes to the significant contribution of an insufficient immune response in susceptibility. Along with this overall increase in burden from NTM disease is the increase in direct medical costs associated with it, which are also staggeringly high. In 2010 alone, 815 million dollars were used to treat 86,244 cases of NTM in the United States [7]. Furthermore, NTM infection often leads to chronic disease that requires lengthy, complex, and sometimes poorly tolerated drug regimens over many months to years, and following treatment, patients can experience relapse from incomplete treatment or reinfection [8–13]. These studies and intricacies underscore the need to develop effective vaccines and drug treatments for use in highly susceptible populations and settings of emerging drug resistance [14].
Fig 1. Body sites affected by NTM species.
Pulmonary infections are generally due to inhalation from environmental sources. Disseminated infections are most prevalent in immunocompromised persons, such as those on anti-TNF antibody therapy or suffering from HIV. Cervical lymphadenitis presents most commonly in children. Bone and joint infections by NTM are usually introduced via trauma. Lastly, skin and soft tissue infections are initiated via surgery, trauma, or broken skin barriers contacting contaminated water. Figure represents more commonly encountered species; some less-common species are not depicted. HIV, human immunodeficiency virus; MAC, M. avium complex; NTM, nontuberculous mycobacteria; TNF, tumor necrosis factor.
Unfortunately, NTM infection and disease is not a reportable condition across much of the United States, and identification of NTM to the species level is not routinely done. Despite this variance in methodology and reporting across geographical areas, NTM prevalence has steadily risen since 1950 and is likely an underestimate [15]. The most common NTM species to cause lung disease belong to the MAC—composed primarily of M. avium and M. intracellulare. With high-throughput gene sequencing, several more related species have been identified that are under the MAC umbrella, including M. chimaera [16]. MAC species are most abundant across the Americas (85%–35.4%), Australia (83%–67.3%), Europe (82%–22.4%), and regions of Asia (71.4%–39.7%) compared to other species causing pulmonary disease [17]. Other frequently cultured NTM include M. kansasii and M. abscessus, whereas less frequent infections can occur with M. xenopi, M. fortuitum, and M. chelonae [18]. Whole-genome sequencing (WGS) of M. abscessus isolates is advancing our understanding of epidemiology, geographical diversity, and transmissibility [19, 20], and this process could be applied to other clinical NTM isolates. Despite an already large prevalence, species of the Mycobacterium genus are destined to increase further in the coming years; in fact, isolates not fitting any known species are frequently encountered in reference laboratories. This review will specifically highlight MAC and M. abscessus because they represent a significant proportion of disease worldwide. See the excellent reviews highlighting issues surrounding the diagnosis of NTM [21, 22], including this diverse representation of species in any given infection. Importantly, species-level identification of NTM has a large impact on treatment selection and success.
NTM organisms from environmental sources, including drinking and natural water, as well as soil and dust, can colonize human epithelia [23]. Furthermore, the steady increase of NTM infections is likely due to a wide contribution of factors, including an individual’s overall greater exposure to large-volume aerosols, a modernization of plumbing away from antibacterial copper pipes, and lower hot water temperatures, which may promote environmental colonization and NTM persistence. A comparative epidemiologic study evaluated water-aerosol–generating activities and found that these activities were not associated with MAC lung disease in human immunodeficiency virus (HIV)-negative adults; however, colonization of virulent isolates of MAC on faucets or associations in immunocompromised people, etc., were not ruled out by the authors as disease associations [24]. Indirect transmission is also an important epidemiological consideration, particularly for immunosuppressed individuals. Indeed, there is evidence that aerosolized NTM can also survive on fomites, providing another mechanism for spread, particularly for susceptible cystic fibrosis (CF) patients [25]. This nearly ubiquitous presence of NTM in the environment makes them ideal candidates for opportunistic infections and therefore warrants specific and detailed diagnostics and further evaluation for intervention against disease.
Host–pathogen interactions
It is unclear whether the increase in NTM disease is in part due to a change in pathogen virulence over time. Development of preventive and treatment strategies against NTM will require a more comprehensive understanding of these dynamic host–pathogen interactions. While several host and pathogen factors are known to increase risk of NTM infection, greater knowledge pertaining to the molecular mechanisms underlying these factors will be required to develop more targeted therapy and also to develop assays that may be used in clinical and preclinical studies. Certain body morphotypes, gender, and the use of immunomodulatory drugs, such as steroids and tumor necrosis factor (TNF)-α blockers, are associated with a higher risk of NTM infection. Impaired ciliary function also predisposes individuals to NTM disease, and further research into the role of defects in airway clearance in mycobacterial invasion needs to be conducted [26]. The prescription and practice of mechanical airway clearance or airway clearance therapy has been observed to play an important role in reducing negative disease associations in bronchiectasis patients [27] but has not yet been evaluated for a larger role in preventing NTM reinfection. Specific genetic and treatment-induced host factors that increase risk of NTM infection are discussed below.
Increased risk
Disease caused by NTM is influenced by a complex interplay between exposure and host-related factors. A matched case-control study demonstrated positive associations between MAC disease status and chronic obstructive pulmonary disease (COPD), severe pneumonia, steroids, and immunomodulatory drug use [24]. Other host factors contributing to NTM pulmonary disease (NTM-PD) include thoracic skeletal abnormalities and genetic disorders that predispose the patient to bronchiectasis and/or lung infections (for example, CF). While some host risk factors do overlap with those for Mtb infection, others starkly do not; for instance, TB is a relatively rare diagnosis in individuals with CF [28]. Similar to TB, a prominent risk factor for acquiring NTM disease is the immunocompromised status of an individual—due to either an inherited or acquired immunodeficiency—including those with HIV infection, cancer, organ transplants, and inflammatory diseases, such as rheumatoid arthritis treated with anti-TNFα therapy [26, 29, 30]. A recent case-control study revealed several compounding risk factors for NTM disease in rheumatoid arthritis patients in a TB-endemic area, including a history of TB, hypertension, diabetes, interstitial lung disease, COPD, and corticosteroid treatment [31]. Indeed, certain medications can also influence NTM infections, for example, inhaled corticosteroids causing immunosuppression increases the risk of acquiring NTM infections [24, 32, 33]. Although there is a greater incidence of both NTM and TB infections in immunocompromised HIV patients, there is an important dichotomy in the onset of mycobacterial disease with respect to HIV progression. There is great difficulty diagnosing TB in HIV-infected individuals; however, because of the high rates of extrapulmonary TB and frequency of smear-negative disease, it is evident that TB occurs relatively early in HIV infection [34]. Conversely, a recent US study observed NTM-disseminated disease in HIV patients, primarily due to MAC, with the highest incidence in those with cluster of differentiation 4 (CD4+) T-cell counts less than 50 cells/mm3 [35].
Clustering of disease within families suggests a heritable genetic predisposition to disease susceptibility [17, 36–38]. These heritable factors largely align with host immune responses to infection, which are also well documented for Mtb infections. For example, interferon-γ (IFN-γ) is an important host response against NTM in both mice and humans; disseminated NTM disease occurs in mice deficient in either IFN-γ receptor (IFNγR) or IFN-γ [39]. Additional immune deficiencies such as polymorphisms in interleukin 12 (IL-12) (IL-12p40 [40], IL-12 receptorβ1 [41], IFN-γ receptor [IFNγR1] [42] and IFNγR2 [43]) genes and natural-resistance–associated macrophage protein 1 gene (NRAMP1) are risk factors for NTM infection [26]. Interestingly, levels of anti-IFN-γ and anti-granulocyte–macrophage colony-stimulating factor (GM-CSF) autoantibodies are higher in patients with NTM-PD [44]. As previously discussed, host age is also an important and significant factor for acquiring NTM disease. A retrospective cohort study of NTM disease in Denmark showed a relative risk of a positive NTM culture in the elderly (>65 years) greater than 10 times that of adolescents (aged 15–19 years) [5]. Pulmonary NTM infection in the US occurs mostly in tall, thin, nonsmoking postmenopausal white women who have a complex condition involving additive genetic variants in immune, ciliary, connective tissue, and CF transmembrane conductance regulator (CFTR) genes [38]. The disease in this population, sometimes referred to as “Lady Windermere syndrome,” presents with nodular bronchiectasis frequently involving the right middle lobe or left lingula and tends to have a much slower progression than cavitary disease, such that long-term follow-up (months to years) may be necessary [45, 46]. Affected host immune status, genetic polymorphisms, and age thus all play prominent roles in NTM susceptibility.
Beyond host factors, the distinct phenotypes and variability between NTM species can also influence disease states. The ability of NTM to form different morphotypes and robust biofilms [47–52] may play a role in pathogenesis by enabling bronchial epithelial attachment and respiratory infection [53], whereas Mtb biofilms may be involved in the formation of caseous necrosis and cavitation within the lung [47, 49, 50]. Specifically for M. abscessus, the in vitro zebrafish model has revealed smooth (expressing glycopepidolipid [GPL]) and rough (loss of GPL) phenotypes have divergent effects on infected macrophages that induce either protective granulomas and chronic infection or abscess formation and acute infection, respectively [48]. The recognition and characterization of different NTM morphotypes were established in the 1950s, but the mechanism(s) underlying colony phenotype and relationships to pathogenicity is incompletely understood for many NTM species [53, 54].
Other NTM species of clinical importance
Other clinically important species of NTM include, but are not limited to, M. kansasii, M. haemophilum, M. marinum, and M. ulcerans (Fig 1). Some of these NTM infect the skin, often occurring following procedures such as tattooing, liposuction, surgical procedures, or trauma, all of which introduce the mycobacteria into the disrupted skin barrier. M. ulcerans infection (Buruli ulcer) is prevalent in sub-Saharan Africa and some parts of Australia and is usually introduced by trauma from contaminated surfaces and water. Increased risk of mycobacterial infections (including NTM infection) can be attributed to antirheumatic medications, such as anti-TNF therapy [55]. Specifically, monoclonal antibody therapy with TNF inhibitors used for the treatment of psoriasis can be a risk factor for skin infections with M. fortuitum [56]. Anti-TNF therapy can also enhance risk of infection with M. intracellulare and M. avium pathogens [57]. M. kansasii causes lung disease that is clinically indistinguishable from TB and is inherently resistant to standard first-line drugs, such as pyrazinamide [58], used against Mtb. Many of the 170 and counting NTM species have variable but relevant clinical impact and should be identified for successful treatment.
Clinical diagnosis of adult pulmonary NTM infections
Humans encounter environmental mycobacteria with variable clinical disease relevance on a daily basis. Therefore, a single positive culture from nonsterile sources including the respiratory or digestive tract does not necessarily indicate infection or disease and makes treatment decisions less straightforward. Further complicating diagnosis are the nonspecific symptoms of NTM-PD, including a chronic cough, with or without sputum production or hemoptysis, and progressive fatigue or malaise. Weight loss, fever, and night sweats are less frequent—occurring in 30% to 50% of patients—and often indicate advanced disease [59]. Clinical diagnosis of NTM-PD involves the presentation of cough, fatigue, and often weight-loss symptoms, accompanied by positive radiographs and isolation of an NTM from clinical specimens such as sputum [22]. Often, 2 positive microbiological cultures are needed to differentiate NTM disease versus colonization [21, 60]; however, these criteria have not been validated with respect to progression to disease [61, 62]. The exclusion of other infectious (for example, TB, nocardiosis, and fungal infection) and noninfectious diseases (for example, sarcoidosis) is also critical when diagnosing NTM. Clinical, radiographic, and microbiologic criteria are equally important, and all must be met to make a diagnosis of NTM disease.
Microbiology and molecular identification of NTM
Early control of mycobacterial infections is dependent on methods for rapid identification of complex NTM and Mtb infections from a clinical sample and can reduce both morbidity and mortality through implementing the best course of drug treatment. The method for detection of NTM typically involves smear microscopy and culturing specimens, such as sputum, on solid and/or liquid media [63], while the preferred staining procedure is fluorochrome microscopy [64]. To the extent that it is possible, NTM should be identified to the species level using tools such as commonly employed line-probe assays, which can also be used to amplify drug-resistance–determining regions [63]. The GenoType NTM-DR line-probe assay (Hain Lifescience, Nehren, Germany) is one such tool recently described for the identification of clinical M. abscessus subspecies (subsp.) and drug resistance [65]. Rapid species identification can also be determined using commercial DNA probes (MAC, M. kansasii, and M. gordonae), while group- or complex-level identification can be accomplished with high-performance liquid chromatography (HPLC). For some NTM isolates, especially rapidly growing mycobacteria (RGM; M. fortuitum, M abscessus, and M. chelonae), extended antibiotic in vitro susceptibility testing, DNA sequencing, or polymerase chain reaction (PCR) restriction endonuclease assay (PRA) may be necessary. Another assay available for the detection of Mycobacterium species from clinical samples is a PCR-reverse blot hybridization assay (REBA) Myco-ID assay (YD Diagnostics, Yongin, South Korea), in which multiple targeted oligonucleotide specific probes (Mycobacterium-species specific) are bound to a nitrocellulose membrane strip, then hybridized with biotinylated PCR products and subsequently visualized by colorimetric hybridization signals [66, 67].
Molecular identification of different NTM species can also be accomplished via genomic DNA comparison, though this process is labor intensive. A dramatic shift and update in mycobacterial taxonomy came with the ease of DNA sequencing. Early investigations demonstrated that the mycobacterial 16S rRNA gene is highly conserved [68], that it is more accurate than phenotypic methods for species identification [69], and that differences in the sequence of 1% or greater can generally define a new species [70]. Furthermore, in a large study, molecular-based PCR methods were 84.7% sensitive at detecting NTM species from clinical samples, while phenotypic-culture–based methods only reached 78.0% and required significantly more time to complete [71]. For these reasons, 16S rRNA can be used as a standard reference when comparing detection techniques. Recently, Rodríguez-Sánchez and colleagues assessed 125 NTM isolates using matrix-assisted laser desorption ionization-time of flight (MALDI-TOF) mass spectrometry, the GenoType common mycobacteria (CM)/additional species (AS) assay, and a 16S rRNA/hsp65 gene sequencing reference assay to determine the alignment of these different techniques [72]. The MALDI-TOF assay was in agreement with the reference assay in 118/125 cases (94.4%), and the GenoType CM/AS assay was in agreement in 105/125 cases (84%), showing some limitations in loss of sensitivity of the GenoType CM/AS assay [72]. Conversely, while the MALDI-TOF assay requires a mass spectrometer, the GenoType CM/AS assay can be performed using either manual or automated processing, making it more accessible in resource-limited settings. Besides the aforementioned assays, another innovative molecular assay, the Quantamatrix multiplexed assay platform (QMAP) system recently described by Wang and colleagues [73], allows clinicians to discriminate between mycobacterial species. This assay utilizes an automated magnetic-bead–based assay following similar PCR steps as used in the PCR-REBA assay, except denatured biotinylated PCR products are added to species-specific oligonucleotide probes coupled to carboxylated microdisks, followed by the addition of streptavidin R-phycoerythrin conjugate and automated reading of fluorescence intensity. The specificity of the QMAP system was assessed from 295 mycobacterial respiratory clinical isolates, several Mycobacterium reference strains (including Mtb H37Rv and NTM strains), and non-Mycobacterium strains. This process yielded high specificity and sensitivity in a short period (3 hours). The overall percentage agreement between the QMAP system and PRA Myco-ID and REBA Myco-ID was 92.8% and 100%, respectively. Molecular typing methods of Mtb and NTM species have been thoroughly described in a recent review [74], including assay expense, requirement of specialized equipment and trained staff, reproducibility, specificity and sensitivity, and the time required for an accurate diagnosis. Correct identification of NTM species is dependent on an extensive and routinely updated molecular database and is critical for successful treatment of NTM infection.
Pulmonary NTM infection and treatment
The treatment and outcomes of NTM diseases differ depending on the NTM species, and therefore species-level NTM identification is clinically important. Standard treatment of infection with slow-growing NTM (such as MAC-PD) in immunocompetent patients involves the combination of macrolides (azithromycin [AZM], chemically considered an azalide, or clarithromycin [CLR]), ethambutol (EMB), and rifampin (RIF) [21]. Macrolides act by binding to the peptide exit tunnel of the ribosome, thus preventing the peptide chain from exiting the peptidyl transferase center of the ribosome. MAC species are notorious for developing drug resistance to many antibiotics through modifications of the drug-binding site to reduce binding of the agents, as described in a recent review [75], making infections exceedingly difficult to treat. The most important risk factors for developing macrolide-resistant MAC are macrolide monotherapy and the combination of macrolide and fluoroquinolone without a third companion drug. For patients with fibrocavitary MAC lung disease or severe nodular/bronchiectatic disease, regimens that include both macrolides, streptomycin, and aminoglycosides such as kanamycin and amikacin that bind to the bacterial 30S ribosomal subunit and induce cell death are recommended [21].
The American Thoracic Society provides drug guidelines and recommended regimens for NTM, including those based on the severity and disease status of NTM infections [21]. The British Thoracic Society has also recently published guidelines for the management of NTM-PD [60]. A recent review outlines dosages and common adverse events attributed to several drugs used for treatment of NTM-PD [76]. There are a number of toxicities and side effects noted for drugs typically used to treat MAC that could affect treatment compliance, such as CLR-induced headache, nausea, and vomiting or rifamycin-induced anemia, hepatotoxicity, lymphocytopenia, rash, and/or thrombocytopenia [76]. The genetic predisposition to antimicrobial resistance as well as the poor tolerability of the current standard regimens makes the discovery and development of novel drugs for NTM-PD, including both M. abscessus and MAC infections, a research priority. Furthermore, classifying and standardizing treatment success and outcome reporting for comparative assessments may help better identify positive versus negative treatment regimens [14].
Clinicians also have to consider whether a positive culture in the absence of overt symptoms may suggest colonization versus infection, and the significant extent of side effects from prolonged treatment is important when evaluating the need to treat. Indeed, over half (63%) of patients with MAC-PD in a recent study progressed, and these cases correlated with a higher bacterial load and pulmonary destruction. The remaining 47% of MAC-PD patients remained stable [77], and in some cases, those who are untreated revert back to negative cultures spontaneously. Treatment decisions rely on evaluating whether the patient is symptomatic, whether they present with background genetic or pharmacologic factors that would enhance susceptibility, and the extent of radiographic abnormalities, which suggest evidence of disease progression. Further assessment of specific biomarkers that correlate with progression to disease is critical and an active area of research.
Pulmonary MAC and M. abscessus subsp. in the CF patient
The rapidly growing M. abscessus subsp. (including M. abscessus subsp. abscessus, M. abscessus subsp. massiliense, and M. abscessus subsp. bolletii) are emerging pathogens, with outbreaks in surgical patients in Brazil and in CF patients in the United Kingdom [25, 78, 79]. The prevalence of NTM in CF patients, a major health threat, has been steadily increasing since the early 1980s and is estimated to be 7%–13% in this population [28]. Recommendations to enable better NTM-centric healthcare for CF patients have been put forth by the CF Society and the CF Foundation [80]. These recommendations, although not exhaustively listed here, include using sputum but not oropharyngeal swabs for NTM screening, using both solid and liquid cultures for a minimum of 6 weeks for respiratory samples, using molecular identification of NTM isolates, testing susceptibility of MAC to CLR prior to treatment, testing sputum samples for NTM culture every 4–8 weeks throughout the course of treatment, and prescribing NTM antibiotic therapy for 12 months beyond culture conversion [80]. Additional treatment strategies that are relevant for CF patients should be investigated, such as identifying immune pathways that may be leveraged to help those with this disease.
Treatment for M. abscessus subsp. infection
RGM infections can present as an asymptomatic, inert disease with minimal clinical symptoms to severe bronchiectasis and cavitary pulmonary disease with substantial morbidity and mortality. The many subsp. of M. abscessus [81] are a classic example of how species and subsp. identification in an NTM infection can dramatically affect treatment selection and outcomes [12]. Molecular classification can help inform researchers and clinicians about variations in transmissibility, pathogenesis, and drug sensitivity, all within a single species such as M. abscessus. Generally, M. abscessus subsp. abscessus infections are more severe and difficult to treat. CLR and AZM are the standard therapeutic agents for M. abscessus subsp. massiliense, which lacks a functional, active, inducible-macrolide–resistance gene, erythromycin ribosomal methylase (erm) gene [82]. The erm gene—dominant in M. abscessus subsp. abscessus, M. abscessus subsp. bollotii, and M. fortuitum strains (but not in M. chelonae)—promotes methylation of the 23S rRNA, rendering the bacteria resistant against macrolides, lincosamides, and streptogramins. Induction of this gene is not detected by conventional susceptibility testing, however, since this requires extended culture incubation observation for up to 2 weeks. Once samples are cultured for susceptibility over 2 weeks, species and subsp. can be identified as well as helping dictate decisions about the makeup and length of treatment [60]. Mutational resistance is also observed in the ribosomal L4 protein (rrl) encoding gene of some M. abscessus subsp. The high propensity for macrolide resistance underscores why the use of monotherapy for infections caused by RGM is not recommended [21]. There is active research to develop rapid diagnostic tests for these inducible and mutational-based mechanisms of drug resistance [83], which is severely needed to replace lengthy, extended-culture–based methods. Furthermore, species and subsp. identification of NTM can help predict whether there is a higher propensity for recurrence, relapse, or reinfections [8, 84–86], which will also play a part in determining treatment courses.
Experimental animal models for NTM
As discussed above, there are diverse factors that affect NTM disease, including host factors and innate mycobacteria phenotypes and antibiotic resistance. Preclinical animal models can be leveraged to study the influence of these factors and evaluate novel therapeutic drugs and regimens for treatment of NTM infections. Two major categories of NTM disease to consider for animal model development include pulmonary disease and extrapulmonary-disseminated disease (typically presenting in those who are immunocompromised). NTM are generally less virulent than Mtb, and therefore the capacity to induce a sustained progressive infection in a mouse strain is an important criterion and current hurdle for the development of an experimental mouse model. Previous studies have shown that most immunocompetent mouse strains serve as outstanding models for the more virulent MAC species but demonstrate rapid clearance when infected with the less virulent M. abscessus isolate [87], making model development and selection challenging (Tables 1 and 2). Many different mouse strains have been used to screen different drug compounds against MAC, including CLR, RIF, rifapentine (RPT), moxifloxacin (MXF), EMB, and amikacin (AMK) (Table 1). Other diverse preclinical models are available for testing M. abscessus pathogenesis and in vivo activity of drug compounds against M. abscessus, including amoebae, Drosophila melanogaster, and zebrafish embryo models [48]. Exploiting the host-specific conditions required for the successful growth and pathogenicity outcome of each NTM organism will enable the testing and development of treatment strategies in an appropriate preclinical model.
Table 1. Mouse strains/models used for MAC infection.
| Mouse strain | M. avium route of infection and dose | Productive infection (organ) | Compound screening | Reference |
|---|---|---|---|---|
| C57BL/6 | aerosolization; approximately 105/mouse | lung and spleen | CLR | [100] |
| C57BL/6 (modified Cornell-like model) | M. avium complex strains; aerosolization (500–104 CFU/ mouse) | lung | CLR-RIF | [103] |
| C57BL/6 | M. avium subsp. hominissuis; intranasal 2.25 × 107 CFU/mouse | lung | LAI | [150] |
| C57BL/10 | intranasal; 105 CFU/mouse | lung, spleen, and liver | N/A | [101] |
| 129Sv | IV; 106 CFU/mouse | lung, spleen, and liver | N/A | [96] |
| BALB/c | aerosolization; approximately 105 CFU/mouse | lung and spleen | CLR, CLR-EMB-RIF, MXF-EMB-RIF, CLR-MXF-EMB-RIF | [100] |
| iNOS-/- | IV; 106 CFU/mouse | liver | N/A | [151] |
| iNOS-/- | IV; 106 CFU/mouse | lung, spleen, and liver | N/A | [96] |
| TNFα p55 receptor-/- | IV; 106 CFU/mouse | lung and spleen | N/A | [152] |
| Beige | aerosolization; approximately 105 CFU/mouse | lung and spleen | CLR | [100] |
| Beige | IV; 106 CFU/mouse | lung, spleen, liver, and gut | N/A | [90] |
| Nude | aerosolization; approximately 105 CFU/mouse | lung and spleen | CLR, CLR-EMB-RIF, MXF-EMB-RIF, CLR-MXF-EMB-RIF | [100] |
Abbreviations: CFU, colony-forming units; CLR, clarithromycin; EMB, ethambutol; iNOS, inducible NO synthase; IV, intravenous; LAI, liposomal amikacin for inhalation; MXF, moxifloxacin; N/A, not applicable; NO, nitric oxide; RIF, rifampin; TNF, tumor necrosis factor.
Table 2. Mouse strains used for M. abscessus infections and drug screening.
| Mouse strain | NTM used and route of infection | Productive infection (organ) | Compound screening | Reference |
|---|---|---|---|---|
| C57BL/6 | M. abscessus; aerosolization (HDA and LDA) | HDA (lungs and spleens), LDA (no) | N/A | [94] |
| C57BL/6 | M. abscessus and M. massiliense; IV (4 × 106 to 107) | lung | CLR, MXF, CLR/MXF, AZM, AZM/MXF | [153] |
| BALB/c | M. abscessus-R; IV (104/mouse) | lungs and spleen | N/A | [87] |
| Ob/Ob | M. abscessus; aerosolization (HDA and LDA) | HDA (lungs and spleen), LDA (no) | N/A | [94] |
| CF mouse | M. abscessus-R and -S morphotype; IT (1.6 × 106/mouse) | yes | N/A | [154] |
| iNOS-/- | M. abscessus; IV (106/mouse) | lungs, spleen, and liver | N/A | [87] |
| Cybb-/- | M. abscessus; IV (106/mouse) | lungs, spleen, and liver | N/A | [87] |
| TNFα receptor-/- | M. abscessus; IV (106/mouse) | lungs, spleen, and Liver | N/A | [87] |
| MyD88-/- | M. abscessus; IV (106/mouse) | lungs, spleen, and liver | N/A | [87] |
| C3HeB/FeJ | M. abscessus; IV (106/mouse) | lungs, spleen, and liver | N/A | [87] |
| Beige | M. abscessus; IV (106/mouse) | lungs, spleen, and liver | N/A | [87] |
| GKO | M. abscessus; aerosolization | LDA or HDA lungs and spleen | N/A | [94] |
| GKO | M. abscessus; IV (106/mouse) | lungs, spleen, and Liver | CLR, CLF, BDQ, CLF/BDQ, CIP, AMK | [87] |
| GKO | M. abscessus subsp. massiliense | lungs and spleen | N/A | [155] |
| GM-CSF-/- | M. abscessus; aerosolization (106/mouse) | lungs and spleen | AZM | [156] |
| GM-CSF-/- | M. abscessus; IV (106/mouse) | lungs, spleen, and liver | N/A | [87] |
| Nude | M. abscessus; IV (106–108/mouse) | lungs, spleen, liver, and kidneys | FOX, AMK, CLR, FOX/AMK/CLR, TGC | [157] |
| Nude | M. abscessus; IV (106/mouse) | lungs, spleen, and liver | N/A | [87] |
| SCID | M. abscessus-R; IT (104/mouse) | lungs and spleen | N/A | [158] |
| SCID | M. abscessus; IV (106/mouse) | lungs, spleen, and liver | CLR, BDQ, CLF, BDQ/CLF | [87] |
HDA = approximately 1,000 bacilli/mouse, and LDA = approximately 100 bacilli/mouse. Abbreviations: AMK, amikacin; AZM, azithromycin; BDQ, bedaquiline; CF, cystic fibrosis; CIP, ciprofloxacin; CLF, clofazimine; CLR, clarithromycin; FOX, cefoxitin; GKO, IFN-γ knockout; GM-CSF, granulocyte-macrophage colony-stimulating factor; HDA, high-dose aerosol; IFN-γ, interferon-γ; iNOS, inducible NO synthase; IT, intratracheal; IV, intravenous; LDA, low-dose aerosol; MXF, moxifloxacin; N/A, not applicable; NTM, nontuberculous mycobacteria; R, rough morphotype of M. abscessus; S, smooth morphotype of M. abscessus; SCID, severe combined immunodeficiency; TGC, tigecycline; TNF, tumor necrosis factor.
Animal models for slow-growing mycobacteria
The Beige mouse is used as a standard model for MAC disease [88]. This mouse model was developed in the mid-1990s because of the increasing numbers of HIV-seropositive patients becoming coinfected with M. avium [89]. Beige mice display many immune deficiencies similar to those occurring in AIDS patients [88], as well as a susceptibility to infection with NTM following either intravenous or aerosol infection, providing a unique opportunity for the study of MAC infections in this model [88–92] (Table 1). Additionally, Beige mice exhibit a deficiency of neutrophil influx at the site of infection that increases their susceptibility to M. avium, which is rescued by the adoptive transfer of neutrophils from wild-type mice [90]. Corresponding neutrophil-depletion studies with C57BL/6 mice show increased susceptibility to M. avium [90]. The initial discovery and further confirmation of MAC disease in the Beige mouse model have encouraged many investigators to use this model to screen the chemotherapeutic potential of promising compounds for the treatment of MAC disease. Importantly, many chemotherapeutic compounds against MAC disease and other NTM that have shown activity in the Beige mouse model have been successfully translated into clinical application [93, 94]. Therefore, the Beige mouse is an excellent immunocompromised model for NTM infections and compound screening.
Preclinical models can also be used to study mechanisms of host immunity against mycobacterial infections. For example, the effects of nitric oxide (NO) on Mtb and M. avium infection in mice have been well studied. Through these investigations, it has been demonstrated that NO contributes to protective host responses against Mtb in the murine model, both in vitro (in macrophages) and in vivo [95]. However, interesting differences are present in terms of NO and NTM infections. Studies using mice devoid of inducible NO synthase (iNOS-/-) show improved control of M. avium, denoted by reduced mycobacterial burden in multiple organs compared to wild-type 129Sv mice [96]. Furthermore, treatment of bone-marrow–derived macrophages with IFN-γ and TNFα from either wild-type or iNOS-/- mice leads to reduced intracellular M. avium burden. These results suggest that the protective effects of IFN-γ and TNFα against NTM are not mediated by the production of NO. NO has also been suggested to have a regulatory role on IFN-γ–expressing T helper 1 (TH1) CD4+ T cells because iNOS-/- mice show greater IFN-γ production and increased CD4+ T-cell numbers [97]. The mechanism by which NO is protective against Mtb and not against NTM in mouse models of infection remains poorly understood [98]. One study using an intratracheal infection with M. avium showed similar kinetics of cytokine gene expression between TNFα and iNOS, in which expression levels in the lung were low early in infection when bacterial load was higher and cytokine expression was higher late in infection when bacterial levels were lower, suggesting a possible role of NO against M. avium [99].
Evaluating multiple strains of mice can also provide valuable insight into host immune responses and NTM pathogenesis. For example, several mouse strains were compared to evaluate responses following an M. avium aerosol challenge, including 2 immunocompetent mouse strains (BALB/c, and C57BL/6) and 2 immunodeficient mouse strains (Nude and Beige mice). Not surprisingly, Nude mice showed the greatest susceptibility to M. avium infection compared to the other mouse strains, whereas drug treatment efficacy was determined to be most successful in BALB/c mice [100]. In the same study, C57BL/6 mice showed the greatest resistance to M. avium 8 weeks postchallenge. C57BL/10 mice depleted of CD4+ T cells and infected using an intranasal infection of M. avium clearly support a role for CD4+ T cells [101]. Furthermore, IFN-γ depletion before and during M. avium infection leads to increased bacterial burden in the lung, spleen, and liver, suggesting a protective role for IFN-γ against this pathogen [101].
Like Mtb [102], NTM exposure can result in acute and chronic infections, as well as reactivation post-treatment [8]. Preclinical modeling of these different disease states may help isolate treatment options, including harnessing host immunity. NTM infection reactivation has been studied using a modified Cornell-like murine model (typically used to study reactivation of latent Mtb) and has successfully been developed for experimental reactivation of pulmonary MAC infection (Table 1), [103]. In this model, C57BL/6 mice are infected by the aerosol route with MAC strains and are treated with CLR and rifampicin for 6 weeks, and then treatment is stopped. Twelve weeks following drug treatment, mice are given immunosuppressants (dexamethasone or sulfasalazine) for 5 weeks to expose any remaining bacteria post-treatment. Bacterial burden is assessed in the organs at different times after immunosuppression to measure reactivation. This model could also be useful for determining the potential efficacy of combined drug and immunotherapy regimens by quantifying the numbers of bacilli remaining after treatment.
Animal models for RGM
The most clinically important RGM to cause human lung disease belongs to M. abscessus. M. abscessus subsp. abscessus and M. abscessus subsp. bollettii have a functional erm41 gene; therefore, resistance to macrolides may be identified. It has been challenging to develop an animal model for screening compounds against RGMs because of gaps in fully understanding their pathogenesis of infection and relative avirulence. One study [94] has shown, for example, that C57BL/6 and leptin-deficient (Ob/Ob) mice challenged with a low-dose aerosol (LDA, approximately 100 bacilli per mouse) of M. abscessus did not develop a progressive infection. Additional studies using a high-dose aerosol (HDA, approximately 1,000 bacilli per mouse) in C57BL/6 and Ob/Ob mice have resulted in an established infection and an early pulmonary influx of IFN-γ+ CD4+ T cells. This early influx of CD4+ T cells producing IFN-γ resulted in clearance of M. abscessus in both mouse strains. It is important to note that mycobacterial elimination was delayed in the Ob/Ob mice, demonstrating an increase in susceptibility to infection in this mouse model. Conversely, IFN-γ knockout (GKO) mice challenged with a LDA or HDA of M. abscessus showed progressive lung infection, associated with the influx of T cells, macrophages, and dendritic cells and subsequent granuloma development, despite a lower bacterial load [94]. In addition, HDA challenge of the GKO mice induced IL-4 and IL-10, producing CD4+ and CD8+ T cells within the lungs, capable of suppressing of protective immunity. The thorough and systematic evaluation of host immune factors influencing NTM infection progression and disease can be achieved with selective mouse modeling and comparisons across strains.
A progressive aerosol infection model has proven elusive since most mouse models with significant deficits in innate or acquired immunity are still able to clear an infection with a high level of RGM. This highlights the need for improved understanding of the NTM pathogenesis of infection [87]. Importantly, even some mouse strains with specific defects in innate or acquired immunity infected with 1 × 106 M. abscessus intravenously were able to control the infection [87]. Mouse strains capable of bacterial clearance include Beige (dominant TH2 immunity), iNOS-/-, Cybb-/- (devoid of superoxide generating enzyme), TNFα receptor (R)-/-, C3HeB/FeJ, GKO, and MyD88-/- mice. During chronic infection (40 days), M. abscessus was still present at levels below the initial inoculum in the lungs of the C3HeB/FeJ, GKO, and MyD88-/- mice. Moreover, the GKO and MyD88-/- mice maintained viable but reduced levels of M. abscessus in the spleen and liver after 40 days. SCID, Nude, and GM-CSF-/- mice infected intravenously with M. abscessus demonstrated sustained or progressive bacterial burden [87], which supports an important role for T cells and GM-CSF–dependent cell phenotypes in protective immunity against M. abscessus and other rapid growing subsp.
Acute and chronic compound efficacy have been tested in the M. abscessus-infected SCID mice (Table 2), [87]. Single and combination treatment studies using standard anti-NTM compounds (CLR, clofazimine [CLF], AMK, ciprofloxacin [CIP], bedaquiline [BDQ], and CLF-BDQ) have been completed. An advantage of using severely immunocompromised mice (SCID, Nude, and GM-CSF-/-) for modeling M. abscessus infection is the presence of foamy cells in the lungs after 40 days of infection, a cellular phenotype commonly seen in the histopathologic specimens of human NTM lung disease [87]. Murine models of NTM infection are capable of developing non-necrotic and necrotizing granulomas, mimicking diverse pulmonary pathology in NTM patients. Additional models such as the embryonic zebrafish have been developed to assay M. abscessus [104] for rapid compound screening, while a hollow-fiber model has been utilized for RGM compound screening [87]. The biggest challenge that remains to advance our knowledge in NTM pathogenesis and protection is to fully understand the process of human NTM infections (environmental, nosocomial, and endogenous/exogenous reinfection), which would allow us to better emulate these processes in our animal models.
Vaccines for NTM
Despite the significant global impact of opportunistic NTM and the need to stop subsequent reinfection from the environment in susceptible hosts [105, 106], there are no vaccines currently available against these pathogens. However, various approaches may be exploited to develop and advance vaccines against NTM [107–110]. For example, similar virulence factors are expressed during infection with other pathogens, and cross-reactive antigens may afford induction of protective immunity against NTM [108]. This important gap in healthcare can be closed with the appropriate tools (models) and experience to develop a candidate vaccine targeting mycobacterial infections [111]. A therapeutic vaccine could also help overcome issues with acquired drug resistance to drugs such as CLR, following treatment against both slow-growing mycobacteria (SGM) including MAC [112] and RGM such as M. abscessus [113, 114]. For immunotherapeutic vaccine development, the NTM field can borrow strategies currently being used and evaluated for efficacy against Mtb. For example, our group has engineered a vaccine against Mtb, ID93 (a clinical TB antigen) + glucopyranosyl lipid adjuvant (GLA) formulated in an oil-in-water stable nanoemulsion (SE), which is currently being tested in a Phase 2a trial in South Africa for safety, immunogenicity, and dose selection in 60 TB patients administered post-treatment [115]. Escalating preclinical studies with ID93 + GLA-SE have demonstrated protective and therapeutic efficacy [116–122], and clinical results suggest the vaccine is safe and immunogenic [120, 122]. This strategy hinges on optimizing mycobacterial antigen selection and an immune-stimulating adjuvant, the synthetic Toll-like receptor 4 (TLR4) GLA-SE, capable of enhancing adaptive immune responses to many infectious pathogens [123]. Numerous preclinical and clinical vaccine studies for infectious diseases, allergy, and cancer [117, 124–141] have used a protein/adjuvant strategy that could be emulated for the development of vaccines targeted against NTM infections. Although correlates of protection have been elusive for mycobacterial diseases, more and more recent success has emerged from the TB vaccine community. This includes a cutting-edge correlate of risk RNA blood signature that predicts treatment outcomes and relapse in certain populations [142], providing a new benchmark for other vaccine candidates to reach, as well as recently published data demonstrating a protein antigen with immune-stimulating adjuvant (M72/AS01E) candidate vaccine produced 54% efficacy of preventing active TB in adults in a Phase 2b clinical trial [143]. As the TB research community continues to make strides in developing and testing vaccine candidates, these successes and tools should and could be cross-applied to the NTM field.
Variable host factors and mycobacterial experience are particularly important considerations for rational anti-NTM vaccine design. It has long been hypothesized that NTM-based preexisting immunity could lead to variability and/or lack of Bacillus Calmette–Guérin (BCG) vaccine efficacy [144]. Conversely, if BCG is given prior to NTM exposure in a mouse model, there is some protection against M. avium and M. kansasii [145]. BCG was ineffective against M. intracellulare and M. simiae, perhaps because BCG lacks cross-reactive antigens against these NTM [145]. Fraga and colleagues demonstrated transient protection (delayed onset of bacterial growth and foot swelling) against M. ulcerans, including increased CD4+ TH1 responses, following vaccination with BCG [146]. Recently, unexpected cross-reactivity of NTM/Mtb-specific chemokine (C-X-C motif) (CXCR3+ and CCR6+, respectively) memory T cells in non-TB–exposed healthy control (HC) donors has been observed [147]. The possibility of “boosting” NTM T-cell responses in NTM-exposed individuals with protein/adjuvant vaccines, either alone or as an adjunct to drug treatment, is currently being explored by our team. Adjuvant is likely to play a role in a robust vaccine response against several NTM, including the well-characterized TH1-inducing adjuvant GLA-SE [123]. For example, early IFN-γ induction has been shown to be critical for immunity against M. ulcerans infection, as shown by delayed progression of infection and reduced bacterial burden in wild-type compared to GKO mice [148]. Other data demonstrate promising protective responses in mice, including increased survival, decreased pathology, and reduced bacterial load compared to BCG, using a recombinant BCG-expressing M. ulcerans Ag85A in the Buruli ulcer mouse model [149]. Progress towards an effective NTM vaccine strategy will require careful consideration of the influence(s) of historical NTM exposure in addition to BCG or Mtb experience for possible immune interference or boosting effects and should be a major priority for the research community.
Conclusion
Challenges facing the prevention and treatment of NTM disease include inadequate research—in part no doubt due to insufficient funding—the lack of knowledge of factors leading to susceptibility in mouse strains with different genetic backgrounds, and a poor understanding of the mechanisms utilized by NTM that allow for the evasion of host immunity resulting in bacterial persistence. By addressing these challenges, more effective prophylactic and therapeutic approaches for the prevention and treatment of NTM will likely emerge.
Use of the current minimum inhibitory and minimum bactericidal concentration (MIC/MBC) method in the clinic may need to be updated and/or complemented with newer techniques, and there is continued debate over an optimal animal model for compound screening ongoing in the research community [87]. Nevertheless, new and more effective drug treatments are unlikely to eliminate NTM infection and disease in NTM-susceptible individuals who are frequently reinfected with clinical NTM. Vaccination has the potential to protect patients from primary exposure to clinical NTM and could be used as immunotherapy treatment in combination with standard drugs. Furthermore, vaccines may represent the only realistic way of preventing the significant issue of reinfection. The call to action now lies with the urgent need to stimulate development of and advance effective vaccines and targeted immunotherapy against NTM.
Funding Statement
This work was funded in whole or in part with federal funds from the National Institute of Allergy and Infectious Diseases National Institutes of Health, Department of Health and Human Services [https://www.niaid.nih.gov/] under Contract No. HHSN272200800045C and Grant Number U01AI078054 (RNC), R21AIO99534-02 (DO), AIO99534-02 (DO), HHSN272201000009I/HHSN27200001 (DO), HHSN272201000009I/HHSN27200005 (DO), and R01AI125160-03 (RNC, SLB). The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, National Institute of Allergy and Infectious Diseases, or the National Institutes of Health nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hoefsloot W, van Ingen J, Andrejak C, Angeby K, Bauriaud R, Bemer P, et al. The geographic diversity of nontuberculous mycobacteria isolated from pulmonary samples: an NTM-NET collaborative study. Eur Respir J. 2013;42(6):1604–13. 10.1183/09031936.00149212 . [DOI] [PubMed] [Google Scholar]
- 2.Jing H, Wang H, Wang Y, Deng Y, Li X, Liu Z, et al. Prevalence of nontuberculous mycobacteria infection, China, 2004–2009. Emerg Infect Dis. 2012;18(3):527–8. 10.3201/eid1803.110175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brode SK, Daley CL, Marras TK. The epidemiologic relationship between tuberculosis and non-tuberculous mycobacterial disease: a systematic review. Int J Tuberc Lung Dis. 2014;18(11):1370–7. 10.5588/ijtld.14.0120 . [DOI] [PubMed] [Google Scholar]
- 4.Falkinham JO 3rd,. Epidemiology of infection by nontuberculous mycobacteria. Clin Microbiol Rev. 1996;9(2):177–215. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hermansen TS, Ravn P, Svensson E, Lillebaek T. Nontuberculous mycobacteria in Denmark, incidence and clinical importance during the last quarter-century. Sci Rep. 2017;7(1):6696 10.1038/s41598-017-06931-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adjemian J, Olivier KN, Seitz AE, Holland SM, Prevots DR. Prevalence of nontuberculous mycobacterial lung disease in U.S. Medicare beneficiaries. Am J Respir Crit Care Med. 2012;185(8):881–6. 10.1164/rccm.201111-2016OC . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strollo SE, Adjemian J, Adjemian MK, Prevots DR. The burden of pulmonary nontuberculous mycobacterial disease in the United States. Ann Am Thorac Soc. 2015;12(10):1458–64. 10.1513/AnnalsATS.201503-173OC . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boyle DP, Zembower TR, Qi C. Relapse versus reinfection of Mycobacterium avium Complex pulmonary disease. Patient characteristics and macrolide susceptibility. Ann Am Thorac Soc. 2016;13(11):1956–61. 10.1513/AnnalsATS.201605-344BC . [DOI] [PubMed] [Google Scholar]
- 9.Eddyani M, Vandelannoote K, Meehan CJ, Bhuju S, Porter JL, Aguiar J, et al. A genomic approach to resolving relapse versus reinfection among four cases of Buruli Ulcer. PLoS Negl Trop Dis. 2015;9(11):e0004158 10.1371/journal.pntd.0004158 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeong SH, Kim SY, Huh HJ, Ki CS, Lee NY, Kang CI, et al. Mycobacteriological characteristics and treatment outcomes in extrapulmonary Mycobacterium abscessus complex infections. Int J Infect Dis. 2017;60:49–56. 10.1016/j.ijid.2017.05.007 . [DOI] [PubMed] [Google Scholar]
- 11.Jhun BW, Kim SY, Moon SM, Jeon K, Kwon OJ, Huh HJ, et al. Development of macrolide resistance and reinfection in refractory Mycobacterium avium Complex lung disease. Am J Respir Crit Care Med. 2018; 198(10):1322–1330. 10.1164/rccm.201802-0321OC . [DOI] [PubMed] [Google Scholar]
- 12.Koh WJ, Jeong BH, Kim SY, Jeon K, Park KU, Jhun BW, et al. Mycobacterial characteristics and treatment outcomes in Mycobacterium abscessus lung disease. Clin Infect Dis. 2017;64(3):309–16. 10.1093/cid/ciw724 . [DOI] [PubMed] [Google Scholar]
- 13.Koh WJ, Moon SM, Kim SY, Woo MA, Kim S, Jhun BW, et al. Outcomes of Mycobacterium avium complex lung disease based on clinical phenotype. Eur Respir J. 2017;50(3):1602503 10.1183/13993003.02503-2016 . [DOI] [PubMed] [Google Scholar]
- 14.Diel R, Nienhaus A, Ringshausen FC, Richter E, Welte T, Rabe KF, et al. Microbiologic outcome of interventions against Mycobacterium avium Complex pulmonary disease: A systematic review. Chest. 2018;153(4):888–921. 10.1016/j.chest.2018.01.024 . [DOI] [PubMed] [Google Scholar]
- 15.Nishiuchi Y, Iwamoto T, Maruyama F. Infection sources of a common non-tuberculous mycobacterial pathogen, Mycobacterium avium Complex. Front Med (Lausanne). 2017;4:27 10.3389/fmed.2017.00027 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wallace RJ Jr., Iakhiaeva E, Williams MD, Brown-Elliott BA, Vasireddy S, Vasireddy R, et al. Absence of Mycobacterium intracellulare and presence of Mycobacterium chimaera in household water and biofilm samples of patients in the United States with Mycobacterium avium complex respiratory disease. J Clin Microbiol. 2013;51(6):1747–52. 10.1128/JCM.00186-13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prevots DR, Marras TK. Epidemiology of human pulmonary infection with nontuberculous mycobacteria: a review. Clin Chest Med. 2015;36(1):13–34. 10.1016/j.ccm.2014.10.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Ingen J, Ferro BE, Hoefsloot W, Boeree MJ, van Soolingen D. Drug treatment of pulmonary nontuberculous mycobacterial disease in HIV-negative patients: the evidence. Expert Rev Anti Infect Ther. 2013;11(10):1065–77. 10.1586/14787210.2013.830413 . [DOI] [PubMed] [Google Scholar]
- 19.Davidson RM, Hasan NA, Reynolds PR, Totten S, Garcia B, Levin A, et al. Genome sequencing of Mycobacterium abscessus isolates from patients in the united states and comparisons to globally diverse clinical strains. J Clin Microbiol. 2014;52(10):3573–82. 10.1128/JCM.01144-14 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris KA, Underwood A, Kenna DT, Brooks A, Kavaliunaite E, Kapatai G, et al. Whole-genome sequencing and epidemiological analysis do not provide evidence for cross-transmission of Mycobacterium abscessus in a cohort of pediatric cystic fibrosis patients. Clin Infect Dis. 2015;60(7):1007–16. 10.1093/cid/ciu967 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367–416. 10.1164/rccm.200604-571ST . [DOI] [PubMed] [Google Scholar]
- 22.Ryu YJ, Koh WJ, Daley CL. Diagnosis and treatment of nontuberculous mycobacterial lung disease: Clinicians’ perspectives. Tuberc Respir Dis (Seoul). 2016;79(2):74–84. 10.4046/trd.2016.79.2.74 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Falkinham JO 3rd,. Environmental sources of nontuberculous mycobacteria. Clin Chest Med. 2015;36(1):35–41. 10.1016/j.ccm.2014.10.003 . [DOI] [PubMed] [Google Scholar]
- 24.Dirac MA, Horan KL, Doody DR, Meschke JS, Park DR, Jackson LA, et al. Environment or host?: A case-control study of risk factors for Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2012;186(7):684–91. 10.1164/rccm.201205-0825OC . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bryant JM, Grogono DM, Rodriguez-Rincon D, Everall I, Brown KP, Moreno P, et al. Emergence and spread of a human-transmissible multidrug-resistant nontuberculous mycobacterium. Science. 2016;354(6313):751–7. 10.1126/science.aaf8156 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Honda JR, Knight V, Chan ED. Pathogenesis and risk factors for nontuberculous mycobacterial lung disease. Clin Chest Med. 2015;36(1):1–11. 10.1016/j.ccm.2014.10.001 . [DOI] [PubMed] [Google Scholar]
- 27.Munoz G, de Gracia J, Buxo M, Alvarez A, Vendrell M. Long-term benefits of airway clearance in bronchiectasis: a randomised placebo-controlled trial. Eur Respir J. 2018;51(1):1701926 10.1183/13993003.01926-2017 . [DOI] [PubMed] [Google Scholar]
- 28.Patil N, Marco A, Montales MT, Bhaskar N, Mittadodla P, Mukasa LN. Pulmonary tuberculosis in a patient with Cystic Fibrosis. N Am J Med Sci. 2015;7(5):233–5. 10.4103/1947-2714.157494 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Henkle E, Winthrop KL. Nontuberculous mycobacteria infections in immunosuppressed hosts. Clin Chest Med. 2015;36(1):91–9. 10.1016/j.ccm.2014.11.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Winthrop KL, Baxter R, Liu L, Varley CD, Curtis JR, Baddley JW, et al. Mycobacterial diseases and antitumour necrosis factor therapy in USA. Ann Rheum Dis. 2013;72(1):37–42. 10.1136/annrheumdis-2011-200690 . [DOI] [PubMed] [Google Scholar]
- 31.Liao TL, Lin CF, Chen YM, Liu HJ, Chen DY. Risk factors and outcomes of nontuberculous mycobacterial disease among rheumatoid arthritis patients: A case-control study in a TB endemic area. Sci Rep. 2016;6:29443 10.1038/srep29443 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andrejak C, Nielsen R, Thomsen VO, Duhaut P, Sorensen HT, Thomsen RW. Chronic respiratory disease, inhaled corticosteroids and risk of non-tuberculous mycobacteriosis. Thorax. 2013;68(3):256–62. 10.1136/thoraxjnl-2012-201772 . [DOI] [PubMed] [Google Scholar]
- 33.Hojo M, Iikura M, Hirano S, Sugiyama H, Kobayashi N, Kudo K. Increased risk of nontuberculous mycobacterial infection in asthmatic patients using long-term inhaled corticosteroid therapy. Respirology. 2012;17(1):185–90. 10.1111/j.1440-1843.2011.02076.x . [DOI] [PubMed] [Google Scholar]
- 34.Mendez-Samperio P. Diagnosis of tuberculosis in HIV co-infected individuals: Current status, challenges and opportunities for the future. Scand J Immunol. 2017;86(2):76–82. 10.1111/sji.12567 . [DOI] [PubMed] [Google Scholar]
- 35.Varley CD, Ku JH, Henkle E, Schafer SD, Winthrop KL. Disseminated nontuberculous mycobacteria in HIV-infected patients, Oregon, USA, 2007–2012. Emerg Infect Dis. 2017;23(3):533–5. 10.3201/eid2303.161708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Colombo RE, Hill SC, Claypool RJ, Holland SM, Olivier KN. Familial clustering of pulmonary nontuberculous mycobacterial disease. Chest. 2010;137(3):629–34. 10.1378/chest.09-1173 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leung JM, Fowler C, Smith C, Adjemian J, Frein C, Claypool RJ, et al. A familial syndrome of pulmonary nontuberculous mycobacteria infections. Am J Respir Crit Care Med. 2013;188(11):1373–6. 10.1164/rccm.201306-1059LE . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Szymanski EP, Leung JM, Fowler CJ, Haney C, Hsu AP, Chen F, et al. Pulmonary nontuberculous mycobacterial infection. A multisystem, multigenic disease. Am J Respir Crit Care Med. 2015;192(5):618–28. 10.1164/rccm.201502-0387OC . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chan ED, Bai X, Kartalija M, Orme IM, Ordway DJ. Host immune response to rapidly growing mycobacteria, an emerging cause of chronic lung disease. Am J Respir Cell Mol Biol. 2010;43(4):387–93. 10.1165/rcmb.2009-0276TR . [DOI] [PubMed] [Google Scholar]
- 40.Prando C, Samarina A, Bustamante J, Boisson-Dupuis S, Cobat A, Picard C, et al. Inherited IL-12p40 deficiency: genetic, immunologic, and clinical features of 49 patients from 30 kindreds. Medicine (Baltimore). 2013;92(2):109–22. 10.1097/MD.0b013e31828a01f9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haverkamp MH, van de Vosse E, van Dissel JT. Nontuberculous mycobacterial infections in children with inborn errors of the immune system. J Infect. 2014;68 Suppl 1:S134–50. 10.1016/j.jinf.2013.09.024 . [DOI] [PubMed] [Google Scholar]
- 42.Dorman SE, Picard C, Lammas D, Heyne K, van Dissel JT, Baretto R, et al. Clinical features of dominant and recessive interferon gamma receptor 1 deficiencies. Lancet. 2004;364(9451):2113–21. 10.1016/S0140-6736(04)17552-1 . [DOI] [PubMed] [Google Scholar]
- 43.Doffinger R, Jouanguy E, Dupuis S, Fondaneche MC, Stephan JL, Emile JF, et al. Partial interferon-gamma receptor signaling chain deficiency in a patient with bacille Calmette-Guerin and Mycobacterium abscessus infection. J Infect Dis. 2000;181(1):379–84. 10.1086/315197 [DOI] [PubMed] [Google Scholar]
- 44.Kim K, Waterer G, Thomson R, Yang IA, Nashi N, Tan DB, et al. Levels of anti-cytokine antibodies may be elevated in patients with pulmonary disease associated with non-tuberculous mycobacteria. Cytokine. 2014;66(2):160–3. 10.1016/j.cyto.2014.01.005 . [DOI] [PubMed] [Google Scholar]
- 45.Chan ED, Iseman MD. Slender, older women appear to be more susceptible to nontuberculous mycobacterial lung disease. Gend Med. 2010;7(1):5–18. 10.1016/j.genm.2010.01.005 . [DOI] [PubMed] [Google Scholar]
- 46.Kim RD, Greenberg DE, Ehrmantraut ME, Guide SV, Ding L, Shea Y, et al. Pulmonary nontuberculous mycobacterial disease: prospective study of a distinct preexisting syndrome. Am J Respir Crit Care Med. 2008;178(10):1066–74. 10.1164/rccm.200805-686OC . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Basaraba RJ, Ojha AK. Mycobacterial biofilms: Revisiting tuberculosis bacilli in extracellular necrotizing lesions. Microbiol Spectr. 2017;5(3):TBTB2-0024-2016. 10.1128/microbiolspec.TBTB2-0024-2016 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bernut A, Herrmann JL, Ordway D, Kremer L. The diverse cellular and animal models to decipher the physiopathological traits of Mycobacterium abscessus infection. Front Cell Infect Microbiol. 2017;7:100 10.3389/fcimb.2017.00100 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Esteban J, Garcia-Coca M. Mycobacterium biofilms. Front Microbiol. 2017;8:2651 10.3389/fmicb.2017.02651 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kulka K, Hatfull G, Ojha AK. Growth of Mycobacterium tuberculosis biofilms. J Vis Exp. 2012;(60):3820 10.3791/3820 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rose SJ, Babrak LM, Bermudez LE. Mycobacterium avium possesses extracellular DNA that contributes to biofilm formation, structural integrity, and tolerance to antibiotics. PLoS ONE. 2015;10(5):e0128772 10.1371/journal.pone.0128772 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rose SJ, Bermudez LE. Mycobacterium avium biofilm attenuates mononuclear phagocyte function by triggering hyperstimulation and apoptosis during early infection. Infect Immun. 2014;82(1):405–12. 10.1128/IAI.00820-13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yamazaki Y, Danelishvili L, Wu M, Hidaka E, Katsuyama T, Stang B, et al. The ability to form biofilm influences Mycobacterium avium invasion and translocation of bronchial epithelial cells. Cell Microbiol. 2006;8(5):806–14. 10.1111/j.1462-5822.2005.00667.x . [DOI] [PubMed] [Google Scholar]
- 54.Fennelly KP, Ojano-Dirain C, Yang Q, Liu L, Lu L, Progulske-Fox A, et al. Biofilm formation by Mycobacterium abscessus in a lung cavity. Am J Respir Crit Care Med. 2016;193(6):692–3. 10.1164/rccm.201508-1586IM . [DOI] [PubMed] [Google Scholar]
- 55.Brode SK, Jamieson FB, Ng R, Campitelli MA, Kwong JC, Paterson JM, et al. Increased risk of mycobacterial infections associated with anti-rheumatic medications. Thorax. 2015;70(7):677–82. 10.1136/thoraxjnl-2014-206470 . [DOI] [PubMed] [Google Scholar]
- 56.Chang MB, Sri JC, Driscoll M, Gaspari AA. Mycobacterium fortuitum infection following adalimumab treatment for psoriasis and subsequent complication-free treatment with alternate TNF-a blockers. J Drugs Dermatol. 2011;10(8):914–6. . [PubMed] [Google Scholar]
- 57.Yoo JW, Jo KW, Kang BH, Kim MY, Yoo B, Lee CK, et al. Mycobacterial diseases developed during anti-tumour necrosis factor-alpha therapy. Eur Respir J. 2014;44(5):1289–95. 10.1183/09031936.00063514 [DOI] [PubMed] [Google Scholar]
- 58.Raynaud C, Laneelle MA, Senaratne RH, Draper P, Laneelle G, Daffe M. Mechanisms of pyrazinamide resistance in mycobacteria: importance of lack of uptake in addition to lack of pyrazinamidase activity. Microbiology. 1999;145 (Pt 6):1359–67. 10.1099/13500872-145-6-1359 . [DOI] [PubMed] [Google Scholar]
- 59.Huang JH, Kao PN, Adi V, Ruoss SJ. Mycobacterium avium-intracellulare pulmonary infection in HIV-negative patients without preexisting lung disease: diagnostic and management limitations. Chest. 1999;115(4):1033–40. . [DOI] [PubMed] [Google Scholar]
- 60.Haworth CS, Banks J, Capstick T, Fisher AJ, Gorsuch T, Laurenson IF, et al. British Thoracic Society guidelines for the management of non-tuberculous mycobacterial pulmonary disease (NTM-PD). Thorax. 2017;72(Suppl 2):ii1–ii64. 10.1136/thoraxjnl-2017-210927 . [DOI] [PubMed] [Google Scholar]
- 61.Koh WJ, Chang B, Ko Y, Jeong BH, Hong G, Park HY, et al. Clinical significance of a single isolation of pathogenic nontuberculous mycobacteria from sputum specimens. Diagn Microbiol Infect Dis. 2013;75(2):225–6. 10.1016/j.diagmicrobio.2012.09.021 . [DOI] [PubMed] [Google Scholar]
- 62.Martiniano SL, Sontag MK, Daley CL, Nick JA, Sagel SD. Clinical significance of a first positive nontuberculous mycobacteria culture in cystic fibrosis. Ann Am Thorac Soc. 2014;11(1):36–44. 10.1513/AnnalsATS.201309-310OC . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.van der Werf MJ, Kodmon C, Katalinic-Jankovic V, Kummik T, Soini H, Richter E, et al. Inventory study of non-tuberculous mycobacteria in the European Union. BMC Infect Dis. 2014;14:62 10.1186/1471-2334-14-62 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wright PW, Wallace RJ Jr., Wright NW, Brown BA, Griffith DE. Sensitivity of fluorochrome microscopy for detection of Mycobacterium tuberculosis versus nontuberculous mycobacteria. J Clin Microbiol. 1998;36(4):1046–9. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kehrmann J, Kurt N, Rueger K, Bange FC, Buer J. Genotype NTM-DR for identifying Mycobacterium abscessus subspecies and determining molecular resistance. J Clin Microbiol. 2016;54(6):1653–5. 10.1128/JCM.00147-16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang HY, Kim H, Kim S, Bang H, Kim DK, Lee H. Evaluation of PCR-reverse blot hybridization assay for the differentiation and identification of Mycobacterium species in liquid cultures. J Appl Microbiol. 2015;118(1):142–51. 10.1111/jam.12670 . [DOI] [PubMed] [Google Scholar]
- 67.Wang HY, Kim J, Kim S, Park SD, Kim HY, Choi HK, et al. Performance of PCR-REBA assay for screening and identifying pathogens directly in whole blood of patients with suspected sepsis. J Appl Microbiol. 2015;119(5):1433–42. 10.1111/jam.12941 . [DOI] [PubMed] [Google Scholar]
- 68.Rogall T, Wolters J, Flohr T, Bottger EC. Towards a phylogeny and definition of species at the molecular level within the genus Mycobacterium. Int J Syst Bacteriol. 1990;40(4):323–30. 10.1099/00207713-40-4-323 . [DOI] [PubMed] [Google Scholar]
- 69.Springer B, Stockman L, Teschner K, Roberts GD, Bottger EC. Two-laboratory collaborative study on identification of mycobacteria: molecular versus phenotypic methods. J Clin Microbiol. 1996;34(2):296–303. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tortoli E. Impact of genotypic studies on mycobacterial taxonomy: the new mycobacteria of the 1990s. Clin Microbiol Rev. 2003;16(2):319–54. 10.1128/CMR.16.2.319-354.2003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Deggim-Messmer V, Bloemberg GV, Ritter C, Voit A, Homke R, Keller PM, et al. Diagnostic molecular mycobacteriology in regions with low tuberculosis endemicity: Combining real-time PCR assays for detection of multiple mycobacterial pathogens with line probe assays for identification of resistance mutations. EBioMedicine. 2016;9:228–37. 10.1016/j.ebiom.2016.06.016 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rodriguez-Sanchez B, Ruiz-Serrano MJ, Marin M, Lopez Roa P, Rodriguez-Creixems M, Bouza E. Evaluation of matrix-assisted laser desorption ionization-time of flight mass spectrometry for identification of nontuberculous mycobacteria from clinical isolates. J Clin Microbiol. 2015;53(8):2737–40. 10.1128/JCM.01380-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang HY, Uh Y, Kim S, Lee H. Performance of the Quantamatrix multiplexed assay platform system for the differentiation and identification of Mycobacterium species. J Med Microbiol. 2017;66(6):777–87. 10.1099/jmm.0.000495 . [DOI] [PubMed] [Google Scholar]
- 74.Jagielski T, Minias A, van Ingen J, Rastogi N, Brzostek A, Zaczek A, et al. Methodological and clinical aspects of the molecular epidemiology of Mycobacterium tuberculosis and other mycobacteria. Clin Microbiol Rev. 2016;29(2):239–90. 10.1128/CMR.00055-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Huh HJ, Kim SY, Jhun BW, Shin SJ, Koh WJ. Recent advances in molecular diagnostics and understanding mechanisms of drug resistance in nontuberculous mycobacterial diseases. Infect Genet Evol. 2018. October 11. 10.1016/j.meegid.2018.10.003 . [DOI] [PubMed] [Google Scholar]
- 76.Wassilew N, Hoffmann H, Andrejak C, Lange C. Pulmonary disease caused by non-tuberculous mycobacteria. Respiration. 2016;91(5):386–402. 10.1159/000445906 . [DOI] [PubMed] [Google Scholar]
- 77.Hwang JA, Kim S, Jo KW, Shim TS. Natural history of Mycobacterium avium Complex lung disease in untreated patients with stable course. Eur Respir J. 2017;49(3). 10.1183/13993003.00537-2016 . [DOI] [PubMed] [Google Scholar]
- 78.Bryant JM, Grogono DM, Greaves D, Foweraker J, Roddick I, Inns T, et al. Whole-genome sequencing to identify transmission of Mycobacterium abscessus between patients with cystic fibrosis: a retrospective cohort study. Lancet. 2013;381(9877):1551–60. 10.1016/S0140-6736(13)60632-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Davidson RM, Hasan NA, de Moura VC, Duarte RS, Jackson M, Strong M. Phylogenomics of Brazilian epidemic isolates of Mycobacterium abscessus subsp. bolletii reveals relationships of global outbreak strains. Infect Genet Evol. 2013;20:292–7. 10.1016/j.meegid.2013.09.012 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Floto RA, Olivier KN, Saiman L, Daley CL, Herrmann JL, Nick JA, et al. US Cystic Fibrosis Foundation and European Cystic Fibrosis Society consensus recommendations for the management of non-tuberculous mycobacteria in individuals with cystic fibrosis. Thorax. 2016;71 (Suppl 1):i1–22. 10.1136/thoraxjnl-2015-207360 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cho YJ, Yi H, Chun J, Cho SN, Daley CL, Koh WJ, et al. The genome sequence of 'Mycobacterium massiliense' strain CIP 108297 suggests the independent taxonomic status of the Mycobacterium abscessus complex at the subspecies level. PLoS ONE. 2013;8(11):e81560 10.1371/journal.pone.0081560 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brown-Elliott BA, Nash KA, Wallace RJ Jr,. Antimicrobial susceptibility testing, drug resistance mechanisms, and therapy of infections with nontuberculous mycobacteria. Clin Microbiol Rev. 2012;25(3):545–82. 10.1128/CMR.05030-11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Liu W, Li B, Chu H, Zhang Z, Luo L, Ma W, et al. Rapid detection of mutations in erm(41) and rrl associated with clarithromycin resistance in Mycobacterium abscessus complex by denaturing gradient gel electrophoresis. J Microbiol Methods. 2017;143:87–93. 10.1016/j.mimet.2017.10.010 . [DOI] [PubMed] [Google Scholar]
- 84.Boyle DP, Zembower TR, Reddy S, Qi C. Comparison of clinical features, virulence, and relapse among Mycobacterium avium Complex species. Am J Respir Crit Care Med. 2015;191(11):1310–7. 10.1164/rccm.201501-0067OC . [DOI] [PubMed] [Google Scholar]
- 85.Park J, Cho J, Lee CH, Han SK, Yim JJ. Progression and treatment outcomes of lung disease caused by Mycobacterium abscessus and Mycobacterium massiliense. Clin Infect Dis. 2017;64(3):301–8. 10.1093/cid/ciw723 . [DOI] [PubMed] [Google Scholar]
- 86.Wallace RJ Jr., Brown-Elliott BA, McNulty S, Philley JV, Killingley J, Wilson RW, et al. Macrolide/Azalide therapy for nodular/bronchiectatic Mycobacterium avium complex lung disease. Chest. 2014;146(2):276–82. 10.1378/chest.13-2538 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Obregon-Henao A, Arnett KA, Henao-Tamayo M, Massoudi L, Creissen E, Andries K, et al. Susceptibility of Mycobacterium abscessus to antimycobacterial drugs in preclinical models. Antimicrob Agents Chemother. 2015;59(11):6904–12. 10.1128/AAC.00459-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gangadharam PR. Beige mouse model for Mycobacterium avium complex disease. Antimicrob Agents Chemother. 1995;39(8):1647–54. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bermudez LE, Inderlied CB, Young LS. Mycobacterium avium complex in AIDS. Curr Clin Top Infect Dis. 1992;12:257–81. . [PubMed] [Google Scholar]
- 90.Appelberg R, Castro AG, Gomes S, Pedrosa J, Silva MT. Susceptibility of beige mice to Mycobacterium avium: role of neutrophils. Infect Immun. 1995;63(9):3381–7. 1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Appelberg R, Castro AG, Pedrosa J, Silva RA, Orme IM, Minoprio P. Role of gamma interferon and tumor necrosis factor alpha during T-cell- independent and -dependent phases of Mycobacterium avium infection [published erratum appears in Infect Immun 1995 Mar;63(3):1145]. Infect Immun. 1994;62(9):3962–71. 1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bermudez LE, Petrofsky M, Kolonoski P, Young LS. An animal model of Mycobacterium avium complex disseminated infection after colonization of the intestinal tract. J Infect Dis. 1992;165(1):75–9. . [DOI] [PubMed] [Google Scholar]
- 93.Barrow WW. Treatment of mycobacterial infections. Rev Sci Tech. 2001;20(1):55–70. . [DOI] [PubMed] [Google Scholar]
- 94.Ordway D, Henao-Tamayo M, Smith E, Shanley C, Harton M, Troudt J, et al. Animal model of Mycobacterium abscessus lung infection. J Leukoc Biol. 2008;83(6):1502–11. 10.1189/jlb.1007696 . [DOI] [PubMed] [Google Scholar]
- 95.Shiloh MU, Nathan CF. Reactive nitrogen intermediates and the pathogenesis of Salmonella and mycobacteria. Curr Opin Microbiol. 2000;3(1):35–42. . [DOI] [PubMed] [Google Scholar]
- 96.Gomes MS, Florido M, Pais TF, Appelberg R. Improved clearance of Mycobacterium avium upon disruption of the inducible nitric oxide synthase gene. J Immunol. 1999;162(11):6734–9. . [PubMed] [Google Scholar]
- 97.Taylor-Robinson AW, Liew FY, Severn A, Xu D, McSorley SJ, Garside P, et al. Regulation of the immune response by nitric oxide differentially produced by T helper type 1 and T helper type 2 cells. Eur J Immunol. 1994;24(4):980–4. 10.1002/eji.1830240430 . [DOI] [PubMed] [Google Scholar]
- 98.Florido M, Goncalves AS, Silva RA, Ehlers S, Cooper AM, Appelberg R. Resistance of virulent Mycobacterium avium to gamma interferon-mediated antimicrobial activity suggests additional signals for induction of mycobacteriostasis. Infect Immun. 1999;67(7):3610–8. 1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gonzalez-Perez M, Marino-Ramirez L, Parra-Lopez CA, Murcia MI, Marquina B, Mata-Espinoza D, et al. Virulence and immune response induced by Mycobacterium avium complex strains in a model of progressive pulmonary tuberculosis and subcutaneous infection in BALB/c mice. Infect Immun. 2013;81(11):4001–12. 10.1128/IAI.00150-13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Andrejak C, Almeida DV, Tyagi S, Converse PJ, Ammerman NC, Grosset JH. Characterization of mouse models of Mycobacterium avium complex infection and evaluation of drug combinations. Antimicrob Agents Chemother. 2015;59(4):2129–35. 10.1128/AAC.04841-14 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Saunders BM, Cheers C. Inflammatory response following intranasal infection with Mycobacterium avium Complex: role of T-cell subsets and gamma interferon. Infect Immun. 1995;63(6):2282–7. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Behr MA, Edelstein PH, Ramakrishnan L. Revisiting the timetable of tuberculosis. BMJ. 2018;362:k2738 10.1136/bmj.k2738 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cha SB, Jeon BY, Kim WS, Kim JS, Kim HM, Kwon KW, et al. Experimental reactivation of pulmonary Mycobacterium avium Complex infection in a modified Cornell-like murine model. PLoS ONE. 2015;10(9):e0139251 10.1371/journal.pone.0139251 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bernut A, Le Moigne V, Lesne T, Lutfalla G, Herrmann JL, Kremer L. In vivo assessment of drug efficacy against Mycobacterium abscessus using the embryonic zebrafish test system. Antimicrob Agents Chemother. 2014;58(7):4054–63. 10.1128/AAC.00142-14 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Checkley AM, Wyllie DH, Scriba TJ, Golubchik T, Hill AV, Hanekom WA, et al. Identification of antigens specific to non-tuberculous mycobacteria: the Mce family of proteins as a target of T cell immune responses. PLoS ONE. 2011;6(10):e26434 10.1371/journal.pone.0026434 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lee SJ, Jang JH, Yun GY, Kang DR, Park HJ, Shin SJ, et al. Mycobacterium abscessus D-alanyl-D-alanine dipeptidase induces the maturation of dendritic cells and promotes Th1-biased immunity. BMB Rep. 2016;49(10):554–9. 10.5483/BMBRep.2016.49.10.080 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Le Moigne V, Belon C, Goulard C, Accard G, Bernut A, Pitard B, et al. MgtC as a host-induced factor and vaccine candidate against Mycobacterium abscessus infection. Infect Immun. 2016;84(10):2895–903. 10.1128/IAI.00359-16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Le Moigne V, Gaillard JL, Herrmann JL. Vaccine strategies against bacterial pathogens in cystic fibrosis patients. Med Mal Infect. 2016;46(1):4–9. 10.1016/j.medmal.2015.11.013 . [DOI] [PubMed] [Google Scholar]
- 109.Le Moigne V, Gaillard JL, Herrmann JL. Vaccine strategies against cystic fibrosis pathogens. Hum Vaccin Immunother. 2016;12(3):751–6. 10.1080/21645515.2015.1102810 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Le Moigne V, Rottman M, Goulard C, Barteau B, Poncin I, Soismier N, et al. Bacterial phospholipases C as vaccine candidate antigens against cystic fibrosis respiratory pathogens: the Mycobacterium abscessus model. Vaccine. 2015;33(18):2118–24. 10.1016/j.vaccine.2015.03.030 . [DOI] [PubMed] [Google Scholar]
- 111.Bertholet S, Ireton GC, Kahn M, Guderian J, Mohamath R, Stride N, et al. Identification of human T cell antigens for the development of vaccines against Mycobacterium tuberculosis. J Immunol. 2008;181(11):7948–57. Epub 2008/11/20. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Meier A, Kirschner P, Springer B, Steingrube VA, Brown BA, Wallace RJ Jr., et al. Identification of mutations in 23S rRNA gene of clarithromycin-resistant Mycobacterium intracellulare. Antimicrob Agents Chemother. 1994;38(2):381–4. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Maurer FP, Ruegger V, Ritter C, Bloemberg GV, Bottger EC. Acquisition of clarithromycin resistance mutations in the 23S rRNA gene of Mycobacterium abscessus in the presence of inducible erm(41). J Antimicrob Chemother. 2012;67(11):2606–11. 10.1093/jac/dks279 . [DOI] [PubMed] [Google Scholar]
- 114.Wallace RJ Jr., Meier A, Brown BA, Zhang Y, Sander P, Onyi GO, et al. Genetic basis for clarithromycin resistance among isolates of Mycobacterium chelonae and Mycobacterium abscessus. Antimicrob Agents Chemother. 1996;40(7):1676–81. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Day TA, Luabeya AKK, Penn-Nicholson A, Loxton A, Reid T, Toefy A, et al. Safety and immunogenicity of the adjunct therapeutic vaccine ID93+GLA-SE in treated tuberculosis patients: A randomized double-blind placebo-controlled trial. [clinical trial] IDRI-TBVPX-203; https://clinicaltrials.gov/ct2/show/NCT02465216?term=ID93&rank=2. https://clinicaltrials.gov/ct2/show/NCT02465216?term=ID93&rank=2. [Google Scholar]
- 116.Baldwin SL, Bertholet S, Reese VA, Ching LK, Reed SG, Coler RN. The importance of adjuvant formulation in the development of a tuberculosis vaccine. J Immunol. 2012;188(5):2189–97. Epub 2012/02/01. 10.4049/jimmunol.1102696 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Baldwin SL, Reese VA, Huang PD, Beebe EA, Podell BK, Reed SG, et al. Protection and long-lived immunity induced by the ID93/GLA-SE vaccine candidate against a clinical Mycobacterium tuberculosis isolate. Clin Vaccine Immunol. 2015. 10.1128/CVI.00458-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bertholet S, Ireton GC, Ordway DJ, Windish HP, Pine SO, Kahn M, et al. A defined tuberculosis vaccine candidate boosts BCG and protects against multidrug-resistant Mycobacterium tuberculosis. Sci Transl Med. 2010;2(53):53ra74 Epub 2010/10/15. 10.1126/scitranslmed.3001094 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Coler RN, Bertholet S, Pine SO, Orr MT, Reese V, Windish HP, et al. Therapeutic immunization against Mycobacterium tuberculosis is an effective adjunct to antibiotic treatment. J Infect Dis. 2013;207(8):1242–52. Epub 2012 Aug 15. 10.1093/infdis/jis425 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Coler RN, Day TA, Ellis R, Piazza FM, Beckmann AM, Vergara J, et al. The TLR-4 agonist adjuvant, GLA-SE, improves magnitude and quality of immune responses elicited by the ID93 tuberculosis vaccine: first-in-human trial. NPJ Vaccines. 2018;3:34 10.1038/s41541-018-0057-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Larsen SE, Baldwin SL, Orr MT, Reese VA, Pecor T, Granger B, et al. Enhanced anti-Mycobacterium tuberculosis immunity over time with combined drug and immunotherapy treatment. Vaccines (Basel). 2018;6(2). 10.3390/vaccines6020030 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Penn-Nicholson A, Tameris M, Smit E, Day TA, Musvosvi M, Jayashankar L, et al. Safety and immunogenicity of the novel tuberculosis vaccine ID93 + GLA-SE in BCG-vaccinated healthy adults in South Africa: a randomised, double-blind, placebo-controlled phase 1 trial. Lancet Respir Med. 2018;6(4):287–98. 10.1016/S2213-2600(18)30077-8 [DOI] [PubMed] [Google Scholar]
- 123.Coler RN, Bertholet S, Moutaftsi M, Guderian JA, Windish HP, Baldwin SL, et al. Development and characterization of synthetic glucopyranosyl lipid adjuvant system as a vaccine adjuvant. PLoS ONE. 2011;6(1):e16333 Epub 2011/02/08. 10.1371/journal.pone.0016333 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Reed SG, Orr MT, Fox CB. Key roles of adjuvants in modern vaccines. Nat Med. 2013;19(12):1597–608. 10.1038/nm.3409 . [DOI] [PubMed] [Google Scholar]
- 125.Treanor JJ, Essink B, Hull S, Reed S, Izikson R, Patriarca P, et al. Evaluation of safety and immunogenicity of recombinant influenza hemagglutinin (H5/Indonesia/05/2005) formulated with and without a stable oil-in-water emulsion containing glucopyranosyl-lipid A (SE+GLA) adjuvant. Vaccine. 2013;31(48):5760–5. 10.1016/j.vaccine.2013.08.064 . [DOI] [PubMed] [Google Scholar]
- 126.Santini-Oliveira M, Coler RN, Parra J, Veloso V, Jayashankar L, Pinto PM, et al. Schistosomiasis vaccine candidate Sm14/GLA-SE: Phase 1 safety and immunogenicity clinical trial in healthy, male adults. Vaccine. 2016;34(4):586–94. 10.1016/j.vaccine.2015.10.027 . [DOI] [PubMed] [Google Scholar]
- 127.Anderson RC, Fox CB, Dutill TS, Shaverdian N, Evers TL, Poshusta GR, et al. Physicochemical characterization and biological activity of synthetic TLR4 agonist formulations. Colloids Surf B Biointerfaces. 2010;75(1):123–32. 10.1016/j.colsurfb.2009.08.022 . [DOI] [PubMed] [Google Scholar]
- 128.Weinberger B, Joos C, Reed SG, Coler R, Grubeck-Loebenstein B. The stimulatory effect of the TLR4-mediated adjuvant glucopyranosyl lipid A is well preserved in old age. Biogerontology. 2016;17(1):177–87. 10.1007/s10522-015-9576-x . [DOI] [PubMed] [Google Scholar]
- 129.Van Hoeven N, Joshi SW, Nana GI, Bosco-Lauth A, Fox C, Bowen RA, et al. A novel synthetic TLR-4 agonist adjuvant increases the protective response to a clinical-stage West Nile Virus vaccine antigen in multiple formulations. PLoS ONE. 2016;11(2):e0149610 10.1371/journal.pone.0149610 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Seder R, Reed SG, O’Hagan D, Malyala P, D’Oro U, Laera D, et al. Gaps in knowledge and prospects for research of adjuvanted vaccines. Vaccine. 2015;33 Suppl 2:B40–3. 10.1016/j.vaccine.2015.03.057 . [DOI] [PubMed] [Google Scholar]
- 131.Coler RN, Duthie MS, Hofmeyer KA, Guderian J, Jayashankar L, Vergara J, et al. From mouse to man: safety, immunogenicity and efficacy of a candidate leishmaniasis vaccine LEISH-F3+GLA-SE. Clin Transl Immunology. 2015;4(4):e35 10.1038/cti.2015.6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Thomas MA, Tuero I, Demberg T, Vargas-Inchaustegui DA, Musich T, Xiao P, et al. HIV-1 CD4-induced (CD4i) gp120 epitope vaccines promote B and T-cell responses that contribute to reduced viral loads in rhesus macaques. Virology. 2014;471–473:81–92. 10.1016/j.virol.2014.10.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Reed SG. Engineering adjuvants for predictable immunity. J Exp Med. 2014;211(6):1008–9. 10.1084/jem.2116insight2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.McKay PF, Cope AV, Mann JF, Joseph S, Esteban M, Tatoud R, et al. Glucopyranosyl lipid A adjuvant significantly enhances HIV specific T and B cell responses elicited by a DNA-MVA-protein vaccine regimen. PLoS ONE. 2014;9(1):e84707 10.1371/journal.pone.0084707 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ireton GC, Reed SG. Adjuvants containing natural and synthetic Toll-like receptor 4 ligands. Expert Rev Vaccines. 2013;12(7):793–807. 10.1586/14760584.2013.811204 . [DOI] [PubMed] [Google Scholar]
- 136.Wiley SR, Raman VS, Desbien A, Bailor HR, Bhardwaj R, Shakri AR, et al. Targeting TLRs expands the antibody repertoire in response to a malaria vaccine. Sci Transl Med. 2011;3(93):93ra69 Epub 2011/07/29. 10.1126/scitranslmed.3002135 . [DOI] [PubMed] [Google Scholar]
- 137.Ching LK, Mompoint F, Guderian JA, Picone A, Orme IM, Coler RN, et al. Transcriptional profiling of TLR-4/7/8-stimulated guinea pig splenocytes and whole blood by bDNA assay. J Immunol Methods. 2011;373:54–62. Epub 2011/08/16. 10.1016/j.jim.2011.07.021 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Fox CB, Friede M, Reed SG, Ireton GC. Synthetic and natural TLR4 agonists as safe and effective vaccine adjuvants. Subcell Biochem. 2010;53:303–21. 10.1007/978-90-481-9078-2_14 . [DOI] [PubMed] [Google Scholar]
- 139.Coler RN, Baldwin SL, Shaverdian N, Bertholet S, Reed SJ, Raman VS, et al. A synthetic adjuvant to enhance and expand immune responses to influenza vaccines. PLoS ONE. 2010;5(10):e13677 Epub 2010/11/10. 10.1371/journal.pone.0013677 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Carter D, Reed SG. Role of adjuvants in modeling the immune response. Curr Opin HIV AIDS. 2010;5(5):409–13. 10.1097/COH.0b013e32833d2cdb . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Knudsen NP, Olsen A, Buonsanti C, Follmann F, Zhang Y, Coler RN, et al. Different human vaccine adjuvants promote distinct antigen-independent immunological signatures tailored to different pathogens. Sci Rep. 2016;6:19570 10.1038/srep19570 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Thompson EG, Du Y, Malherbe ST, Shankar S, Braun J, Valvo J, et al. Host blood RNA signatures predict the outcome of tuberculosis treatment. Tuberculosis (Edinb). 2017;107:48–58. 10.1016/j.tube.2017.08.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Van Der Meeren O, Hatherill M, Nduba V, Wilkinson RJ, Muyoyeta M, Van Brakel E, et al. Phase 2b controlled trial of M72/AS01E vaccine to prevent tuberculosis. N Engl J Med. 2018;379(17):1621–34. 10.1056/NEJMoa1803484 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Poyntz HC, Stylianou E, Griffiths KL, Marsay L, Checkley AM, McShane H. Non-tuberculous mycobacteria have diverse effects on BCG efficacy against Mycobacterium tuberculosis. Tuberculosis (Edinb). 2014;94(3):226–37. 10.1016/j.tube.2013.12.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Orme IM, Collins FM. Prophylactic effect in mice of BCG vaccination against nontuberculous mycobacterial infections. Tubercle. 1985;66(2):117–20. . [DOI] [PubMed] [Google Scholar]
- 146.Fraga AG, Martins TG, Torrado E, Huygen K, Portaels F, Silva MT, et al. Cellular immunity confers transient protection in experimental Buruli ulcer following BCG or mycolactone-negative Mycobacterium ulcerans vaccination. PLoS ONE. 2012;7(3):e33406 10.1371/journal.pone.0033406 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lindestam Arlehamn CS, Paul S, Mele F, Huang C, Greenbaum JA, Vita R, et al. Immunological consequences of intragenus conservation of Mycobacterium tuberculosis T-cell epitopes. Proc Natl Acad Sci U S A. 2015;112(2):E147–55. 10.1073/pnas.1416537112 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Bieri R, Bolz M, Ruf MT, Pluschke G. Interferon-gamma is a crucial activator of early host immune defense against Mycobacterium ulcerans infection in mice. PLoS Negl Trop Dis. 2016;10(2):e0004450 10.1371/journal.pntd.0004450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Hart BE, Hale LP, Lee S. Recombinant BCG expressing Mycobacterium ulcerans Ag85A imparts enhanced protection against experimental Buruli ulcer. PLoS Negl Trop Dis. 2015;9(9):e0004046 10.1371/journal.pntd.0004046 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Rose SJ, Neville ME, Gupta R, Bermudez LE. Delivery of aerosolized liposomal amikacin as a novel approach for the treatment of nontuberculous mycobacteria in an experimental model of pulmonary infection. PLoS ONE. 2014;9(9):e108703 10.1371/journal.pone.0108703 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lousada S, Florido M, Appelberg R. Regulation of granuloma fibrosis by nitric oxide during Mycobacterium avium experimental infection. Int J Exp Pathol. 2006;87(4):307–15. 10.1111/j.1365-2613.2006.00487.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ehlers S, Benini J, Kutsch S, Endres R, Rietschel ET, Pfeffer K. Fatal granuloma necrosis without exacerbated mycobacterial growth in tumor necrosis factor receptor p55 gene-deficient mice intravenously infected with Mycobacterium avium. Infect Immun. 1999;67(7):3571–9. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Choi GE, Min KN, Won CJ, Jeon K, Shin SJ, Koh WJ. Activities of moxifloxacin in combination with macrolides against clinical isolates of Mycobacterium abscessus and Mycobacterium massiliense. Antimicrob Agents Chemother. 2012;56(7):3549–55. 10.1128/AAC.00685-12 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Caverly LJ, Caceres SM, Fratelli C, Happoldt C, Kidwell KM, Malcolm KC, et al. Mycobacterium abscessus morphotype comparison in a murine model. PLoS ONE. 2015;10(2):e0117657 10.1371/journal.pone.0117657 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Shang S, Gibbs S, Henao-Tamayo M, Shanley CA, McDonnell G, Duarte RS, et al. Increased virulence of an epidemic strain of Mycobacterium massiliense in mice. PLoS ONE. 2011;6(9):e24726 10.1371/journal.pone.0024726 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.De Groote MA, Johnson L, Podell B, Brooks E, Basaraba R, Gonzalez-Juarrero M. GM-CSF knockout mice for preclinical testing of agents with antimicrobial activity against Mycobacterium abscessus. J Antimicrob Chemother. 2014;69(4):1057–64. 10.1093/jac/dkt451 . [DOI] [PubMed] [Google Scholar]
- 157.Lerat I, Cambau E, Roth Dit Bettoni R, Gaillard JL, Jarlier V, Truffot C, et al. In vivo evaluation of antibiotic activity against Mycobacterium abscessus. J Infect Dis. 2014;209(6):905–12. 10.1093/infdis/jit614 . [DOI] [PubMed] [Google Scholar]
- 158.Byrd TF, Lyons CR. Preliminary characterization of a Mycobacterium abscessus mutant in human and murine models of infection. Infect Immun. 1999;67(9):4700–7. . [DOI] [PMC free article] [PubMed] [Google Scholar]