The U.S. 2017–18 influenza season was a high-severity season, with the highest number of outpatient visits for influenza-like illness* (ILI) since the 2009–10 pandemic and the highest rate of influenza-associated hospitalizations since surveillance expanded to include adult hospitalizations during the 2005–06 season (1). The severe season was characterized by reports of strained emergency departments and hospitals and spot shortages of influenza antiviral medications (2). Influenza activity can vary widely across geographic regions (3), and local severity assessments might better guide public health actions and health care needs and support the development of tailored communication messages to prevent influenza morbidity and mortality. CDC assesses influenza season severity at the national level (4),† but the applicability of this approach at state or local levels has not been tested.
In February 2018, field investigations were conducted in Minnesota and Utah to identify potential indicators of state-level influenza activity and pilot a state-level approach to assessing influenza season severity in real time. Indicators were selected using three criteria: 1) availability of data for 2017–18 and at least five previous influenza seasons; 2) completeness and representativeness of data on observed influenza seasonality; and 3) timeliness. Two indicators selected in both states were weekly ILI activity (percentage of outpatient visits to sentinel providers for ILI) and influenza-associated hospitalizations (counts or population-based rates). A third indicator included weekly counts of influenza-associated deaths in Minnesota and weekly percentage of specimens testing positive for influenza reported by sentinel clinical laboratories in Utah. Using state-level data from five earlier seasons (2012–13 through 2016–17) and following previously published procedures (3), indicator-specific intensity thresholds (ITs) for a 50% chance (IT50), 10% chance (IT90), and a 2% chance (IT98) of observing higher values during the 2017–18 season were calculated. Severity was classified as low, moderate, high, or very high if at least two of three indicators peaked during the 2017–18 season below their IT50 value, between their IT50 and IT90 values, between their IT90 and IT98 values, and above their IT98 value, respectively.
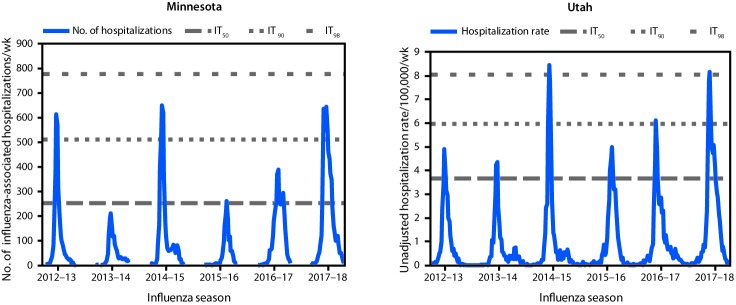
The interim severity of the 2017–18 influenza season (assessed in mid-February 2018) for both Minnesota and Utah was categorized as high. As an example of one of the three indicators, influenza-associated hospitalizations through the end of the 2017–18 season (May 2018) peaked above the IT90 (Minnesota) and IT98 (Utah) values (Figure). End-of-season severity assessments for both states remained high, aligning with national trends and the subsequent high severity classification for the entire United States (1).
FIGURE.
Influenza-associated hospitalizations indicators and intensity thresholds — Minnesota*,† and Utah,§,¶ 2012–18 influenza seasons
Abbreviations: IT50 = intensity threshold at which there is a 50% chance of observing a higher value during 2017–18 based on historical (2012–13 through 2016–17) peak values; IT90 = intensity threshold at which there is a 10% chance of observing a higher value during 2017–18 based on historical (2012–13 through 2016–17) peak values; IT98 = intensity threshold at which there is a 2% chance of observing a higher value during 2017–18 based on historical (2012–13 through 2016–17) peak values.
* Reported to the Minnesota Department of Health.
† Minnesota intensity thresholds: IT50 = 255; IT90 = 511; IT98 = 778.
§ Reported to the Utah Department of Health.
¶ Utah intensity thresholds: IT50 = 3.66; IT90 = 5.99; IT98 = 8.06.
The national severity assessment framework was successfully adapted for use in Minnesota and Utah. Utah is piloting the report of the weekly severity assessments for the 2018–19 season (5). Additional states might find this method useful for improving local public health messaging, preparedness, and response during an influenza season and in the event of a pandemic. CDC continues to develop resources to support local assessments of influenza season severity; interested jurisdictions are encouraged to contact CDC’s Influenza Division for assistance.
All authors have completed and submitted the ICMJE form for disclosure of potential conflicts of interest. Keegan McCaffrey reports grants from the Council of State and Territorial Epidemiologists during the course of the study. No other potential conflicts of interest were disclosed.
Footnotes
Fever (temperature ≥100°F [37.8°C]) and a cough and/or a sore throat without a known cause other than influenza.
Nationally, CDC assesses flu severity using three indicators: 1) percentage of visits to outpatient clinics for ILI; 2) the rates of influenza-associated hospitalizations; and 3) the percentage of deaths resulting from pneumonia or influenza that occurred during each season.
References
- 1.Garten R, Blanton L, Elal AIA, et al. Update: influenza activity in the United States during the 2017–18 season and composition of the 2018–19 influenza vaccine. MMWR Morb Mortal Wkly Rep 2018;67:634–42. 10.15585/mmwr.mm6722a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uyeki TM, Fowler RA, Fischer WA2nd. Gaps in the clinical management of influenza: a century since the 1918 pandemic. JAMA 2018;320:755–6. 10.1001/jama.2018.8113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dahlgren FS, Shay DK, Izurieta HS, et al. Patterns of seasonal influenza activity in U.S. core based statistical areas, described using prescriptions of oseltamivir in Medicare claims data. Epidemics 2018; 18:30014–8. 10.1016/j.epidem.2018.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Biggerstaff M, Kniss K, Jernigan DB, et al. Systematic assessment of multiple routine and near-real time indicators to classify the severity of influenza seasons and pandemics in the United States, 2003–2004 through 2015–2016. Am J Epidemiol 2018;187:1040–50. 10.1093/aje/kwx334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Utah Department of Health. Influenza weekly updates: 2018–2019 influenza season severity measures. Salt Lake City, UT: Utah Department of Health; 2018; http://health.utah.gov/epi/diseases/influenza/surveillance/