Abstract
Background:
Prescription opioid overdose (POD) and heroin overdose (HOD) rates have quadrupled since 1999. Community-level socioeconomic characteristics are associated with opioid overdoses, but whether this varies by urbanicity is unknown.
Methods:
In this serial cross-sectional study of zip codes in 17 states, 2002–2014 (n = 145,241 space-time units), we used hierarchical Bayesian Poisson space-time models to analyze the association between zip code-level socioeconomic features (poverty, unemployment, educational attainment, and income) and counts of POD or HOD hospital discharges. We tested multiplicative interactions between each socioeconomic feature and zip code urbanicity measured with Rural-Urban Commuting Area codes.
Results:
Percent in poverty and of adults with ≤ high school education were associated with higher POD rates (Rate Ratio [RR], 5% poverty: 1.07 [95% credible interval: 1.06–1.07]; 5% low education: 1.02 [1.02–1.03]), while median household income was associated with lower rates (RR, $10,000: 0.88 [0.87–0.89]). Urbanicity modified the association between socioeconomic features and HOD. Poverty and unemployment were associated with increased HOD in metropolitan areas (RR, 5% poverty: 1.12 [1.11–1.13]; 5% unemployment: 1.04 [1.02–1.05]), and median household income was associated with decreased HOD (RR, $10000: 0.88 [0.87–0.90]). In rural areas, low educational attainment alone was associated with HOD (RR, 5%: 1.09 [1.02–1.16]).
Conclusions:
Regardless of urbanicity, elevated rates of POD were found in more economically disadvantaged zip codes. Economic disadvantage played a larger role in HOD in urban than rural areas, suggesting rural HOD rates may have alternative drivers. Identifying social determinants of opioid overdoses is particularly important for creating effective population-level interventions.
Keywords: Opioid-Related Disorders, Heroin, Prescription Drug Misuse, Socioeconomic Factors, Rural Health, Urban Health
1. Introduction
North America is in the midst of an opioid abuse epidemic. Rates of opioid overdose deaths in the United States (US) increased more than 400% since 1999, resulting in over 42,000 deaths in 2016 alone (Centers for Disease Control and Prevention, 2018). Nonfatal overdoses are even more common (Darke et al., 2003; Paulozzi et al., 2012).
There is substantial variation in rates of prescription opioid overdose (POD) and heroin overdose (HOD) between and within states over time as well as spatial clustering of particularly high rates in the Rust Belt and Industrial North (Paulozzi, 2011; Ruhm, 2017). Rates of fatal POD grew much faster in rural than urban areas at the start of the epidemic (Paulozzi and Xi, 2008), and largely rural states, such as West Virginia and Ohio, have some of the highest rates of POD mortality in the country (Rudd et al., 2016). Studies in Australia and Canada have also found POD to be more concentrated in rural areas, suggesting that at least some of the rural-urban differences in risk cut across national boundaries (Rintoul et al., 2011; Pulver et al., 2014). In contrast to POD, heroin has been thought of as an urban problem that has only affected rural and suburban areas more recently (Cicero et al., 2014; Quinones, 2015). The spatial patterns of nonfatal opioid overdoses remain less clear.
Low-income communities with multiple macroeconomic stressors (e.g., high unemployment, poverty, and low education) have been disproportionately affected by drug use over time, yet we know little about the relationship between macroeconomic conditions and opioid overdose. Descriptive data indicate that lower income groups, such as those enrolled in Medicaid, show higher rates of opioid overdose (Coolen et al., 2009; Compton et al., 2016), and ample evidence exists about the role played by features of the spatial context such as unemployment, poverty, and median household income in shaping other types of drug use (Boardman et al., 2001; Galea et al., 2003). There are multiple mechanisms through which community-level economic stressors could influence opioid overdose rates, including lack of access to health care, low informal social control and social cohesion among neighbors, and availability of isolated spaces where people can use drugs and overdose without being identified by anyone who could get help (Galea et al., 2003, 2004, 2005). Also consistent with a self-medication hypothesis, communities with a greater concentration of economic stressors such as poverty, unemployment, and low educational attainment may exhibit higher rates of opioid overdose as residents misuse opioids to manage chronic stress stemming from direct (personal) or indirect (community) exposure to economic hardship and the ensuing symptoms of depression and anxiety (Boardman et al., 2001).
Moreover, the impact of community macroeconomic conditions on POD and HOD may vary between rural and urban areas. The consequences of exposure to economic stressors, such as mental health complications or substance abuse, could be exacerbated in rural areas where at-risk residents lack accessible medical and social services, evidence-based treatment programs, and public transportation options that are widely available in urban areas (Laditka et al., 2009; Pullen and Oser, 2014; Schroeder, 2017). Therefore, residents in economically disadvantaged rural areas may be less able to access treatment than their urban counterparts, potentially increasing the risk of opioid use and overdose associated with these local economic stressors.
Only one previous study, to our knowledge, has evaluated the association between the economic characteristics of local communities and opioid overdose across multiple states and years (Hollingsworth et al., 2017); however, this study did not account for spatial autocorrelation among neighboring communities nor did it compare these relationships between urban and rural areas. Not adjusting for spatial autocorrelation can result in artificially narrow confidence intervals, increasing Type 1 errors. Further, if economic characteristics have a different effect on POD and HOD in rural and urban areas, pooled results will “average out” such variation and ignore risks that are specific to one of these two contexts, thus missing potential areas for intervention. The current study aims to fill these gaps. We intend to advance the understanding of the social drivers of POD and HOD across the US by examining the distribution of inpatient hospital discharges related to POD and HOD across zip codes in 17 geographically and culturally diverse states from 2002–2014. Specifically, our study aims to answer the questions: 1) Are zip code-level economic characteristics associated with zip code-level hospital discharges for POD and HOD? and 2) Do these relationships vary by level of urbanicity?
2. Methods
This ecological time-series study evaluated the association between zip code-level economic characteristics and zip code-level hospitalizations for POD and HOD from 2002 to 2014 across 17 states for which we had spatially identified hospitalization data across the study period: Arizona, Arkansas, California, Colorado, Florida, Iowa, Kentucky, Michigan, North Carolina, Nebraska, New Jersey, New York, Oklahoma, Oregon, South Carolina, Vermont, and Washington (n = 145,241 space-time units). These states represent all Census Bureau designated geographic divisions of the United States (United States Cansus Bureau, 2018) and have diverse populations and varying rates of POD and HOD. The study period adequately captures the precipitous rise of both POD and HOD in the country.
2.1. Data sources and variables
2.1.1. Outcome measures.
Annual 5-digit zip code-level counts of community hospital discharges related to POD and HOD for patients aged 12 years and older were obtained through the Healthcare Cost and Utilization Project’s State Inpatient Databases for all states other than Arkansas, California, Oklahoma, and South Carolina; data for the latter states were obtained through separate requests to the state governments. Community hospitals include all short-term, non-Federal hospitals and exclude hospital units within other institutions (e.g., prisons) (Agency for Healthcare Research and Quality, 2018). Roughly 2% of POD-related discharges and 4% of HOD-related discharges were fatal.
POD-related discharges were identified with the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic codes for opium poisoning (965.00), methadone poisoning (965.02), and poisoning by other opioids (965.09), and with external cause of injury codes for accidental poisoning by methadone (E850.1) and accidental poisoning by other opiates (E850.2). These codes do not distinguish between licit and illicit drug use. HOD-related discharges were identified with the ICD-9-CM diagnostic code for heroin poisoning (965.01) and the external cause of injury code for accidental poisoning by heroin (E850.0). We searched all primary and secondary diagnoses, as well as external cause of injury codes, over the study period to identify the number of opioid overdoses per zip code-year. Location was based on patients’ residential zip code at the time of hospitalization.
2.1.2. Exposure measures.
We measured four indicators of zip code-level economic characteristics: percent of families in poverty (“poverty”), percent of unemployed adults (“unemployment”), percent of residents aged 25 and older with a high school education or less (“low education”), and median household income (“income”). Annual estimates on poverty, unemployment, education, and income were obtained from GeoLytics, Inc. (GeoLytics, 2016).
Zip code urbanicity was measured with a modified version of the United States Department of Agriculture’s (USDA) 2010 Rural-Urban Commuting Area codes, which are based on data from the 2010 Census and 2006–2010 American Community Survey. These codes are updated every 10 years but are not directly comparable over time due to reconfiguration of census tracts and changes in census methodologies. To ensure an adequate number of zip codes in each strata, we collapsed the 10 USDA categories into the following 4 categories: in metropolitan zip codes, 10% or more of the commuting flow was into an urbanized area of at least 50,000 residents; in micropolitan zip codes, 10% of more of the commuting flow was into a large urban center of 10,000–49,999 residents; in small town zip codes, 10% or more of the commuting flow was into a small urban center of 2,500 to 9,999 residents; and in rural zip codes, the primary commuting flow was to areas outside of urbanized areas or urban centers having fewer than 2,500 residents (USDA Economic Research Service, 2016). Zip codes with no population were coded as rural.
2.1.3. Covariate measures.
Additional zip code-level features were included as covariates if they were theorized to confound the association of interest. We controlled for differences in demographic features, namely: percentages of resident who were non-Hispanic white, male, and aged 20–24, 25–44, 45–64, and 65+. Annual demographic and economic estimates were obtained from GeoLytics, Inc. at the block group level. Variables were aggregated up to the zip code by assigning block group values to all Census blocks nested within each zip code and then aggregating these to zip codes using appropriate block weights. To account for varying access to inpatient medical care, we also used the aforementioned hospital discharge data to control for differences in baseline hospital use measured by the total number of hospital discharges per capita.
2.2. Data analysis
Because zip code boundaries are frequently redefined by postal authorities, we used a Bayesian space-time misalignment Poisson model (Zhu et al., 2013) to analyze the association between economic characteristics and counts of hospital discharges related to POD or HOD across levels of urbanicity. These models use conditional autoregressive (CAR) random effects to control for spatial autocorrelation of outcome rates between adjacent zip codes within each year. The CAR approach helps to avoid Type 1 errors that can arise from a lack of independence between neighboring zip codes, helps to avoid small-area biases by letting estimates in low-population zip codes “borrow strength” from nearby zip codes (Waller and Gotway, 2004), and accounts for excess zero counts as well as negative binomial specifications (Lord et al., 2005; Aguero-Valverde and Jovanis, 2006).
Our analysis included four main models: two examining POD and the other two examining HOD. For each outcome, the base model did not include any interactions, and the full model included multiplicative interactions between each economic characteristic and the 4-level zip code urbanicity variable. Models 1 and 2, the POD and HOD base models, included the following annual zip code covariates: urbanicity, poverty, unemployment, low education, income, race, gender, age, baseline hospital use, year, state, CAR-spatial and non-spatial random intercepts, and county random effects. Models 3 and 4, the full POD and HOD models, included everything in the base models as well as multiplicative interactions between urbanicity and poverty, urbanicity and unemployment, urbanicity and low education, and urbanicity and income. The time trend was modeled as a linear function in all models. Alternative specifications of the time trend were tested, but none improved model fit. State fixed effects were included to adjust for all time-invariant sources of differences across areas. Likelihood ratio tests were used to determine whether the interaction terms improved model fit. To get estimated associations for a given level of urbanicity, we calculated a linear combination of the estimate for the reference group (metropolitan) and the interaction term. A rate ratio (RR) was determined to be statistically significant when its associated 95% credible interval (CI) did not include the null (1.00).
Rate differences were approximated by multiplying the mean population weighted rate of POD or HOD by the rate ratio for a given determinant, estimating the counterfactual rate for the population if all zip codes were to have a unit increase in that determinant (e.g., to estimate the population POD rate if every zip code’s income were to increase by $10,000, we multiplied the mean rate of POD by the RR for income). Finally, we subtracted the counterfactual rate by the observed mean rate to approximate the rate difference.
Analyses were performed with WinBUGS version 1.4.3 software (Lunn et al., 2000). Models were allowed to burn-in for 10,000 to 500,000 Markov Chain Monte Carlo (MCMC) iterations, which were sufficient for all parameter estimates to stabilize and converge between two chains with different initial values. Posterior estimates were then sampled for an additional 50,000 iterations.
This study was approved by the Institutional Review Board at the University of California, Davis.
3. Results
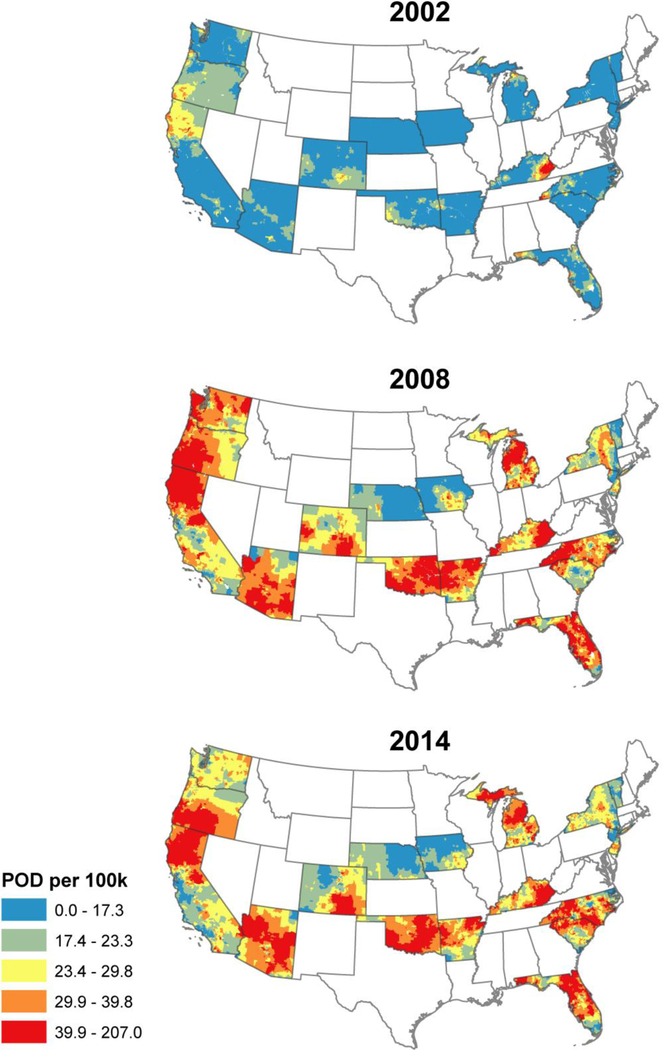
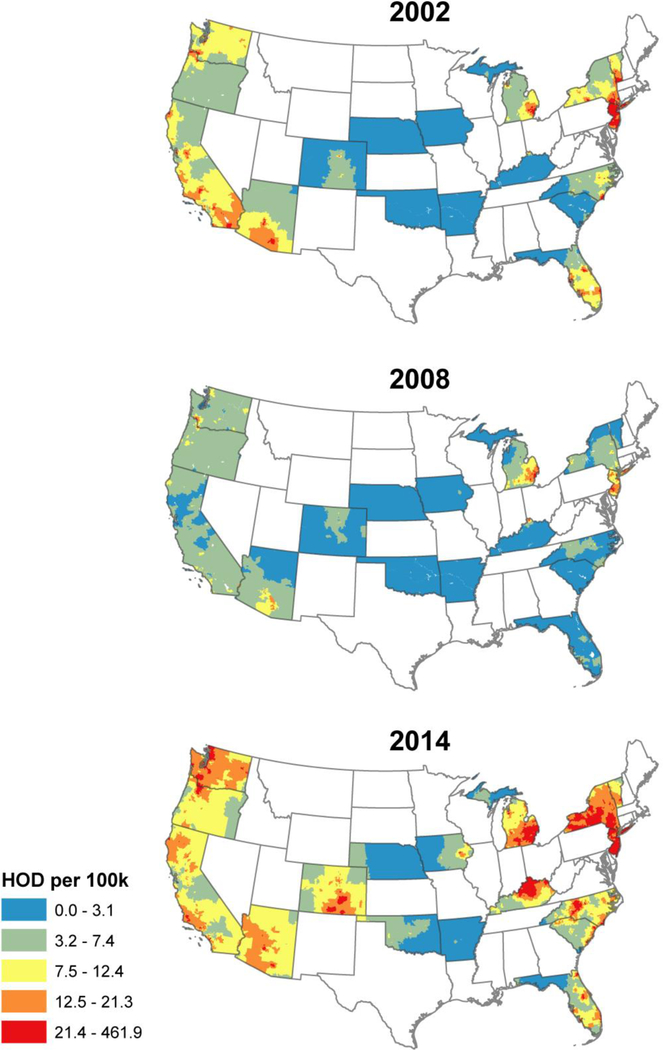
Table 1 presents descriptive zip code-level characteristics stratified by zip code urbanicity. POD and HOD were concentrated in different areas of the country. The population-weighted average annual crude rate of hospital discharges related to POD ranged from 24.3 cases per 100,000 residents in micropolitan zip codes to 18.8 cases per 100,000 residents in metropolitan zip codes. Average annual rates of hospital discharges related to HOD were highest in metropolitan zip codes (2.6 per 100,000) and lowest in rural zip codes (0.6 per 100,000). Indicators of economic stressors tended to decrease with zip code urbanicity, with small town zip codes often faring the worst, on average. Figure 1 presents maps of the smoothed crude rates of POD at the beginning, middle, and end of our study (i.e., 2002, 2008, and 2014). This is repeated for HOD in Figure 2. A map of the urban-rural distribution of zip codes included in our study is included as Supplemental Figure 11.
Table 1.
Descriptive statistics by zip code urbanicity. a
| Characteristic | Metropolitan | Micropolitan | Small town | Rural |
|---|---|---|---|---|
| Zip code-year units | 96,234 | 22,449 | 16,732 | 34,017 |
| POD rate per 100,000b | 18.84 (20.56) | 24.33 (27.66) | 22.00 (37.31) | 20.21 (196.37) |
| HOD rate per 100,000b | 2.58 (8.61) | 1.07 (4.21) | 0.62 (3.99) | 0.61 (7.87) |
| Poverty (%) | 9.29 (8.21) | 12.04 (7.00) | 14.21 (8.78) | 12.59 (7.90) |
| Unemployment (%) | 7.44 (7.40) | 8.07 (6.65) | 8.75 (7.25) | 8.09 (8.02) |
| ≤ HS education (%) | 46.99 (16.84) | 57.97 (12.73) | 60.82 (12.65) | 57.34 (12.63) |
| Income ($) | 60,618 (24,541) | 43,926 (10,463) | 40,533 (10,043) | 41,693 (11,085) |
| White (%) | 69.87 (25.42) | 80.59 (19.59) | 79.05 (21.27) | 82.64 (21.42) |
| Male (%) | 49.56 (3.90) | 50.01 (3.51) | 49.84 (3.27) | 49.59 (7.19) |
| Age 65+ (%) | 14.80 (7.00) | 15.95 (5.13) | 16.47 (5.31) | 18.35 (6.35) |
| Hospital discharges per 100 peopleb | 9.79 (3.64) | 10.85 (3.87) | 11.14 (4.97) | 10.70 (6.52) |
. All characteristics are described with mean (SD), except for zip code-time units, which are described by the total N per level of urbanicity.
. Population-weighted average annual rates
Figure 1.
Quintiles of zip code rates of hospital discharges for POD in select years.
Figure 2.
Quintiles of zip code rates of hospital discharges for HOD in select years.
Table 2 presents the overall association between the four economic characteristics and each of our opioid outcomes as computed by the base models without interaction terms. Across all zip codes, each 5% increase in families in poverty was associated with a 7% increase in POD (95% CI: 1.06–1.07) and a 12% increase in HOD (95% CI: 1.10–1.13). A 5% increase in unemployment was not significantly associated with POD (RR: 1.01, 95% CI: 1.00–1.02) but was associated with a 3% increase in HOD (95% CI: 1.02, 1.05), while a 5% increase in residents aged 25 and older with a high school education or less was associated with a 2% increase in POD (95% CI: 1.02–1.03) and a (not significant) 1% increase in HOD (95% CI: 1.00–1.02). Higher median household income was associated with decreased overdose rates: each $10,000 increase in median household income was associated with a 12% decline in both POD (95% CI: 0.87–0.88) and HOD (95% CI: 0.87–0.90).
Table 2.
Adjusted rate ratios for zip code-level POD and HOD.
| POD | HOD | |||
|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | |
| Urbanicity | ||||
| Metropolitan | 1.00 | (Ref.) | 1.00 | (Ref.) |
| Micropolitan | 0.97 | (0.94, 0.99) | 0.68 | (0.63, 0.75) |
| Small town | 0.91 | (0.89, 0.94) | 0.42 | (0.37, 0.48) |
| Rural | 0.77 | (0.75, 0.80) | 0.34 | (0.29, 0.39) |
| Poverty (per 5%) | 1.07 | (1.06, 1.07) | 1.12 | (1.10, 1.13) |
| Unemployment (per 5%) | 1.01 | (1.00, 1.02) | 1.03 | (1.02, 1.05) |
| ≤ HS education (per 5 %) | 1.02 | (1.02, 1.03) | 1.01 | (1.00, 1.02) |
| Income (per $10,000) | 0.88 | (0.87, 0.88) | 0.88 | (0.87, 0.90) |
| White (per 5%) | 1.05 | (1.05, 1.05) | 1.02 | (1.01, 1.02) |
| Male (%) | 0.98 | (0.98, 0.98) | 1.01 | (1.01, 1.02) |
| Age 20–24 (%) | 0.95 | (0.95, 0.96) | 0.97 | (0.95, 0.98) |
| Age 25–44 (%) | 0.99 | (0.99, 1.00) | 1.01 | (1.00, 1.01) |
| Age 45–64 (%) | 1.02 | (1.02, 1.02) | 1.03 | (1.03, 1.04) |
| Age 65+ (%) | 0.99 | (0.99, 1.00) | 1.00 | (1.00, 1.01) |
| Discharges per capita | 1.02 | (1.01, 1.02) | 1.02 | (1.01, 1.02) |
| Year | 1.07 | (1.07, 1.07) | 1.09 | (1.08, 1.10) |
Bold indicates 95% CI does not include the null.
Additional adjustments included state fixed effects, county random effects, and CAR random effects.
The full POD model did not improve the model fit over the base model (likelihood ratio test p-value = 1.00), suggesting that the association between the four economic characteristics and POD did not vary significantly by urbanicity.
In contrast, relationships between economic stressors and HOD varied substantially across levels of urbanicity (likelihood ratio test p-value: 0.01). Detailed results of the full HOD model with interactions are presented in Table 3. In metropolitan areas, all stressors except education were significantly associated with HOD. Poverty and unemployment were associated with more HOD (RR, 5% increase in poverty: 1.12 [1.11–1.13]; RR, 5% increase in unemployment: 1.04 [1.02–1.05]), and income was associated with less HOD (RR per $10,000: 0.88, 95% CI: 0.87–0.90). In micropolitan zip codes, increased poverty was associated with increased HOD rates (RR, poverty: 1.08 [1.01–1.16]), but the associations with unemployment, education, and income did not reach significance. None of the economic stressors were significantly associated with HOD in small town zip codes. However, in rural areas, low education was a significant risk factor for HOD (RR, per 5% increase in low education: 1.09 [1.02–1.16]). Our data also suggest that higher income may be associated with increased HOD, though the credible interval for this estimate contained the null (RR, per $10,000: 1.16, 95% CI: 0.99–1.34). The associations with poverty and unemployment were not significant in rural zip codes.
Table 3.
Adjusted rate ratios for HOD by urbanicity.
| HOD | ||||
|---|---|---|---|---|
| RR | 95% CI | |||
| White (per 5%) | 1.02 | (1.01, 1.02) | ||
| Male (%) | 1.01 | (1.01, 1.02) | ||
| Age 20–24 (%) | 0.97 | (0.95, 0.99) | ||
| Age 25–44 (%) | 1.01 | (1.00, 1.02) | ||
| Age 45–64 (%) | 1.03 | (1.03, 1.04) | ||
| Age 65+ (%) | 1.00 | (1.00, 1.01) | ||
| Discharges per capita | 1.02 | (1.01, 1.02) | ||
| Year | 1.09 | (1.08, 1.10) | ||
| Metropolitan | Micropolitan | Small town | Rural | |
| Poverty (per 5%) | 1.12 (1.11, 1.13) | 1.08 (1.01, 1.16) | 1.04 (0.93, 1.15) | 1.05 (0.95, 1.15) |
| Unemployment (per 5%) | 1.04 (1.02, 1.05) | 0.98* (0.94, 1.03) | 0.99 (0.91, 1.06) | 1.06 (0.99, 1.12) |
| ≤HS education (per 5%) | 1.01 (1.00, 1.02) | 1.00 (0.97, 1.04) | 0.97 (0.91, 1.03) | 1.09* (1.02, 1.16) |
| Income (per $10,000) | 0.88 (0.87, 0.90) | 0.95 (0.88, 1.04) | 0.90 (0.78, 1.07) | 1.16* (0.99, 1.34) |
Additional adjustments include state fixed effects, county random effects, and CAR random effects. Bold indicates 95% CI does not include the null.
Significantly different than estimate for metropolitan areas.
These rate ratios reflect fairly modest changes in the absolute rates of POD and HOD. Income was associated with the largest approximated rate differences for both types of overdose. On average across all zip codes, an increase of $10,000 in median household income would be associated with a decrease in POD of 2.56 cases per 100,000 (95% CI: −2.77, −2.56). In metropolitan zip codes, an increase of $10,000 in median household income would be associated with a decrease the average annual HOD rate by 0.31 cases per 100,000 (95% CI: −0.33, −0.26).
4. Discussion
Our study shows that across 17 states in 2002–2014, opioid overdoses were concentrated in more economically disadvantaged zip codes, indicated by higher rates of poverty and unemployment as well as lower education and median household income. Furthermore, the associations between economic stressors and HOD varied substantially by zip code urbanicity. In the most urban areas, HOD was concentrated in communities marked by poverty, unemployment, and/or low median household income, while in the most rural areas, only limited educational attainment was associated with increased HOD.
The finding that communities with greater economic stress tend to have higher rates of opioid overdose can be understood by tracing opioid abuse to upstream causes, including restricted economic opportunities, limited access to health care, and social disadvantages (Dasgupta et al., 2018). Community poverty, unemployment, and low educational attainment can create an environment of entrenched stress and despair that fosters drug use among residents, including abuse of opioids (Galea et al., 2003). Moreover, once drug use has been initiated, individuals in economically disadvantaged neighborhoods have a harder time quitting, possibly due to the presence of established drug-use networks in these areas (Nandi et al., 2010), high exposure to daily life stressors such as insecure employment that make it difficult to attend and adhere to substance abuse treatment regimens (McLellan et al., 2000), and lack of access to social networks to support treatment adherence (Panebianco et al., 2016). There are, additionally, environmental barriers to accessing substance abuse treatment in economically disadvantaged areas, such as neighborhood violence (Tung et al., 2018), as well as financial barriers that prevent residents from accessing high-quality, private drug treatment programs (Abraham et al., 2013). Higher income, on the other hand, is indicative of access to a larger number of health resources and social capital (Altschuler et al., 2004), both of which work to prevent the occurrence of opioid overdoses.
Our findings from the base models are also largely supported by the extant literature. Studies of Wisconsin, West Virginia, and San Francisco found community-level poverty to be a risk factor for opioid overdoses (Hall et al., 2008; Meiman et al., 2015; Visconti et al., 2015). County unemployment was found to be a risk factor for fatal HOD nationwide and nonfatal HOD in 5 states (Hollingsworth et al., 2017). Single state individual- and county-level studies have shown low education to be associated with increased POD (Hall et al., 2008; Han et al., 2012) and with drug overdose mortality overall (Zoorob and Salemi, 2017). Previous studies have also found low household income to be associated with nonmedical use of prescription opioids among adolescents (Sung et al., 2005), with POD at the zip code level in California (Cerdá et al., 2016), and with heroin use nationwide (Jones et al., 2015). It is important to note that results from individual- and community-level studies should not be conflated. For example, our findings of risks associated with zip code-level economic stressors means that the economic characteristics of one’s zip code (e.g., percent unemployed) confer risks and benefits to individuals within that zip code irrespective of whether or not those individuals have the corresponding individual-level economic risk factor (e.g., personal unemployment). By evaluating economic features of zip codes over multiple states and years, we were able to answer questions not previously addressed by individual-level studies or by studies with limited geographic coverage.
The relationships between community economic features and opioid overdose varied by area urbanicity for HOD but not for POD. This may be understood, in part, as stemming from the differences in availability of POs and heroin. The availability-proneness theory of drug use posits that drug use occurs when individuals who are prone to using are exposed to high availability (Smart, 1980). It is possible that the most salient feature of urbanicity for opioid use is drug availability. If this is true, it would make sense that we would not see modification by urbanicity for POD because POs are widely available in both urban and rural areas. Heroin, on the other hand, is much more available in urban rather that rural areas.
In metropolitan areas, increased poverty and unemployment were associated with higher rates of HOD, and increased income was associated with lower rates of HOD. This is consistent with the availability-proneness theory, which would predict areas with both high availability (metropolitan areas) and proneness (areas with socioeconomic stressors) would have the highest rates. In rural areas, however, higher rates of HOD were only found in zip codes with higher percent of adults with a high school education or less. In areas with low availability, heroin users are likely to have comparatively high proneness than users in areas with high availability. It is possible that this is harder to capture with area-level measures, which would explain why most socioeconomic stressors were not associated with HOD in rural areas. It is also possible that some socioeconomic indicators matter more for HOD in rural than in urban areas for contextual reasons (e.g., cultural norms about drug use, services available, etc.). To ascertain the role that drug availability has on HOD, future studies should examine whether distance to urban centers modifies the impact that economic features in rural communities have on HOD.
This study’s findings should be considered in light of several strengths and limitations. We were able to add substantially to the literature, as this is the first study to our knowledge to examine the role that economic stressors in small areas play in shaping POD and HOD across 17 states from all regions of the country and across different levels of urbanicity. Previous community-level studies have had limited generalizability due to geographically restricted samples, and most were analyzed at larger levels of resolution, such as the county. Our focus on zip codes allowed us to examine the impact of economic features at a spatial dimension where they are likely to affect individual behaviors–that is, in local neighborhoods. In addition, we used statistical methods that allowed us to account for the substantial spatial autocorrelation in overdoses across zip codes. This improves the accuracy of standard errors by adjusting for failure of independence between spatial units. Finally, we were able to compare the impact of community economic characteristics on prescription opioid and heroin nonfatal overdoses, whereas previous studies have tended to focus on fatal overdoses cause by either POs or heroin but not both.
Limitations of this study include potential time-dependent confounding; for example, areas with lower education are likely to also have lower median income, and people living in areas with lower income are, in turn, less able to afford higher education. However, insofar as we are controlling for mediation, the estimates for variables with time-dependent confounding should be conservative. Also, our data are limited to community hospital discharges from 17 states, so we were unable to capture overdose cases that presented at the emergency room, federal hospitals, long-term acute care facilities, or in states outside of our study area. In addition, there may be some uncertainty regarding the accuracy of hospital discharge data, which rely on the transcription of doctors’ notes by medical coders; however, ICD-9-CM diagnostic codes have previously been found to have a high positive predictive value for identifying opioid overdose (Reardon et al., 2016). Finally, it is possible that zip codes do not represent meaningful community boundaries, although it is a better approximation that the county, which has been used in previous studies.
5. Conclusions
This ecological multi-state study suggests that community-level opioid overdose may be partly driven by community-level macroeconomic conditions. Across 17 states, higher rates of prescription opioid and heroin overdose were found in areas characterized by socioeconomic deprivation. While economic stressors were associated with POD across rural and urban areas, they seemed to play a particularly important role in HOD in urban areas. This suggests that the social determinants of heroin overdose may differ across rural and urban areas. While the magnitudes of our findings were relatively small, this study adds to the limited body of research on contextual factors related to POD and HOD. As the United States searches for population-level solutions to the opioid crisis, identifying the social drivers of this problem is a particular priority.
Supplementary Material
Highlights.
Prescription opioid overdose is concentrated in economically disadvantaged areas.
Economic stress plays a larger role in heroin overdoses in urban than rural areas.
Alternative contextual factors may be driving heroin overdoses in rural areas.
Acknowledgements
This work was supported by grants 1R01DA039962-01 and 5T32DA031099-03, both from the National Institute on Drug Abuse.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Disclosures
Conflict of Interest
No conflict declared.
Role of the Funding Source
The funding sources played no role in the study design, the collection, analysis, or interpretation of data, the writing of the manuscript, or the decision to submit the manuscript for publication.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
References
- Abraham AJ, Knudsen HK, Rieckmann T, Roman PM, 2013. Disparities in access to physicians and medications for the treatment of substance use disorders between publicly and privately funded treatment programs in the United States. J. Stud. Alcohol Drugs 74, 258–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality, 2018. Introduction to the HCUP State Inpatient Databases. Agency for Healthcare Research and Quality, Rockville, MD. [Google Scholar]
- Aguero-Valverde J, Jovanis PP, 2006. Spatial analysis of fatal and injury crashes in Pennsylvania. Accid. Anal. Prev 38, 618–625. [DOI] [PubMed] [Google Scholar]
- Altschuler A, Somkin CP, Adler NE, 2004. Local services and amenities, neighborhood social capital, and health. Soc. Sci. Med 59, 1219–1229. [DOI] [PubMed] [Google Scholar]
- Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS, 2001. Neighborhood disadvantage, stress, and drug use among adults. J. Health Soc. Behav 42, 151–165. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2018. Wide-ranging online data for epidemiologic research Centers for Disease Control and Prevention, Altanta, GA. [Google Scholar]
- Cerdá M, Gaidus A, Keyes KM, Ponicki W, Martins S, Galea S, Gruenewald P, 2017. Prescription opioid poisoning across urban and rural areas: Identifying vulnerable groups and geographic areas. Addiction 112, 103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, Surratt HL, Kurtz SP, 2014. The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry 71, 821–826. [DOI] [PubMed] [Google Scholar]
- Compton WM, Jones CM, Baldwin GT, 2016. Relationship between nonmedical prescription-opioid use and heroin use. N. Engl. J. Med 374, 154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coolen P, Best S, Lima A, Sabel J, Paulozzi L, 2009. Overdose deaths involving prescription opioids among Medicaid enrollees— Washington, 2004–2007. Morb. Mortal. Wkly. Rep 58, 1171–1175. [PubMed] [Google Scholar]
- Darke S, Mattick R, Degenhardt L, 2003. The ratio of non-fatal to fatal heroin overdose. Addiction 98, 1169–1172. [DOI] [PubMed] [Google Scholar]
- Dasgupta N, Beletsky L, Ciccarone D, 2018. Opioid crisis: No easy fix to its social and economic determinants. Am. J. Public Health 108, 182–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Ahern J, Vlahov D, 2003. Contextual determinants of drug use risk behavior: A theoretic framework. J. Urban Health 80(Suppl.), iii50–iii58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Nandi A, Vlahov D, 2004. The social epidemiology of substance use. Epidemiol. Rev 26, 36–52. [DOI] [PubMed] [Google Scholar]
- Galea S, Rudenstine S, Vlahov D, 2005. Drug use, misuse, and the urban environment. Drug Alcohol Rev 24, 127–136. [DOI] [PubMed] [Google Scholar]
- GeoLytics, 2016. GeoLytics estimates premium [data DVD] Geolytics, Inc., East Brunswick, NJ. [Google Scholar]
- Hall AJ, Logan JE, Toblin RL, Kaplan JA, Kraner JC, Bixler D, Crosby AE, Paulozzi LJ, 2008. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA 300, 2613–2620. [DOI] [PubMed] [Google Scholar]
- Han H, Kass PH, Wilsey BL, Li CS, 2012. Individual and county-level factors associated with use of multiple prescribers and multiple pharmacies to obtain opioid prescriptions in California. PLoS One 7, e46246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingsworth A, Ruhm CJ, Simon K, 2017. Macroeconomic conditions and opioid abuse. J. Health Econ 56, 222–233. [DOI] [PubMed] [Google Scholar]
- Jones CM, Logan J, Gladden RM, Bohm MK, 2015. Demographic and substance use trends among heroin users— United States, 2002–2013. Morb. Mortal. Wkly. Rep 64, 719–725. [PMC free article] [PubMed] [Google Scholar]
- Laditka JN, Laditka SB, Probst JC, 2009. Health care access in rural areas: Evidence that hospitalization for ambulatory care-sensitive conditions in the United States may increase with the level of rurality. Health Place 15, 761–770. [DOI] [PubMed] [Google Scholar]
- Lord D, Washington SP, Ivan JN, 2005. Poisson, Poisson-Gamma and zero-inflated regression models of motor vehicle crashes: Balancing statistical fit and theory. Accid. Anal. Prev 37, 35–46. [DOI] [PubMed] [Google Scholar]
- Lunn DJ, Thomas A, Best N, Spiegelhalter D, 2000. WinBUGS—A Bayesian modeling framework: Concepts, structure, and extensibility. Stat. Comput 10, 325–337. [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD, 2000. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA 284, 1689–1695. [DOI] [PubMed] [Google Scholar]
- Meiman J, Tomasallo C, Paulozzi L, 2015. Trends and characteristics of heroin overdoses in Wisconsin, 2003–2012. Drug Alcohol Depend 152, 177–184. [DOI] [PubMed] [Google Scholar]
- Nandi A, Glass TA, Cole SR, Chu H, Galea S, Celentano DD, Kirk GD, Vlahov D, Latimer WW, Mehta SH, 2010. Neighborhood poverty and injection cessation in a sample of injection drug users. Am. J. Epidemiol 171, 391–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panebianco D, Gallupe O, Carrington PJ, Colozzi I, 2016. Personal support networks, social capital, and risk of relapse among individuals treated for substance use issues. Int. J. Drug Policy 27, 146–153. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Xi Y, 2008. Recent changes in drug poisoning mortality in the United States by urban-rural status and by drug type. Pharmacoepidemiol. Drug Saf 17, 997–1005. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Jones CM, Mack KA, Rudd RA, 2011. Vital signs: Overdoses of prescription opioid pain relievers— United States, 1999–2008. Morb. Mortal. Wkly. Rep 60, 1487–1492. [PubMed] [Google Scholar]
- Paulozzi L, Baldwin G, Franklin G, Kerlikowske RG, Jones CM, Ghiya N, Popovic T, 2012. CDC grand rounds: Prescription drug overdoses—A U.S. epidemic. Morb. Mortal. Wkly. Rep 61, 10–13. [PubMed] [Google Scholar]
- Pullen E, Oser C, 2014. Barriers to substance abuse treatment in rural and urban communities: A counselor perspective. Subst. Use Misuse 49, 891–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulver A, Davidson C, Pickett W, 2014. Recreational use of prescription medications among Canadian young people: Identifying disparities. Can. J. Public Health 105, e121–e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinones S, 2015. Dreamland: The true tale of America’s opiate epidemic Bloomsbury Press, New York, NY. [Google Scholar]
- Reardon JM, Harmon KJ, Schult GC, Staton CA, Waller AE, 2016. Use of diagnosis codes for detection of clinically significant opioid poisoning in the emergency department: A retrospective analysis of a surveillance case definition. BMC Emerg. Med 16, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rintoul AC, Dobbin MD, Drummer OH, Ozanne-Smith J, 2011. Increasing deaths involving oxycodone, Victoria, Australia, 2000–09. Inj. Prev 17, 254–259. [DOI] [PubMed] [Google Scholar]
- Rudd RA, Seth P, David F, Scholl L, 2016. Increases in drug and opioid-involved overdose deaths— United States, 2010–2015. Morb. Mortal. Wkly. Rep 65, 1445–1452. [DOI] [PubMed] [Google Scholar]
- Ruhm CJ, 2017. Geographic variation in opioid and heroin involved drug poisoning mortality rates. Am. J. Prev. Med 53, 745–753. [DOI] [PubMed] [Google Scholar]
- Schroeder S, 2017. Rural behavioral health. Rural Health Research Recap Rural Health Research Gateway, Grand Forks, ND. [Google Scholar]
- Smart RG, 1980. An availability-proneness theory of illcity drug use. Theories on drug abuse: Selected contemporary perspectives. NIDA Res. Monogr 30, 89–92. [Google Scholar]
- Sung HE, Richter L, Vaughan R, Johnson PB, Thom B, 2005. Nonmedical use of prescription opioids among teenagers in the United States: Trends and correlates. J. Adolesc. Health 37, 44–51. [DOI] [PubMed] [Google Scholar]
- Tung EL, Boyd K, Lindau ST, Peek ME, 2018. Neighborhood crime and access to health-enabling resources in Chicago. Prev. Med. Rep 9, 153–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau Geography Division, 2018. Census regions and divisions of the United States United States Census Bureau, Suitland, MD. [Google Scholar]
- United States Department of Agriculture Economic Research Service, 2016. Documentation: 2010 Rural-Urban Commuting Area (RUCA) Codes United States Department of Agriculture, Washington, D.C. [Google Scholar]
- Visconti AJ, Santos GM, Lemos NP, Burke C, Coffin PO, 2015. Opioid overdose deaths in the city and county of San Francisco: Prevalence, distribution, and disparities. J. Urban Health 92, 758–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller L, Gotway C, 2004. Applied spatial statistics for public health data John Wiley and Sons, Hoboken, NJ. [Google Scholar]
- Zhu L, Waller LA, Ma J, 2013. Spatial–temporal disease mapping of illicit drug abuse or dependence in the presence of misaligned ZIP codes. GeoJournal 78, 463–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoorob MJ, Salemi JL, 2017. Bowling alone, dying together: The role of social capital in mitigating the drug overdose epidemic in the United States. Drug Alcohol Depend 173, 1–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.