Abstract
Objective:
Although suicide is the second most frequent cause of death in American youth, suicide research has heretofore been confined to convenience samples (1) representing neither psychiatric nor general populations and (2) failing to include individuals dying on first attempts. We sought to address these limitations by assembling a youth cohort followed from first medically recorded attempt (index attempts=IA). We hypothesized this approach would more accurately represent prevalence of completed suicide after attempt and underscore lethality based on method.
Method:
This study draws from a previously reported retrospective-prospective all-age cohort identified through the Rochester Epidemiology Project. The original 1490 subject sample included 813 Olmsted County youth aged 10–24yrs (n=258 males, n=555 females; 54.6% of the total cohort) making IAs between 01-Jan-1986 and 31-Dec-2007 and followed until 31-Dec-2010.
Results:
29/813 (3.6%) subjects killed themselves during the study period, with 28/29 dying before their 25th birthdays and 20/28 (71.4%) dying on first attempt. Comprising only 31.7% (258/813) of the cohort, males comprised the majority of suicides: 23/29 (79.3% of suicides; 8.9% of males) versus 6/29 females (20.7% of suicides; 1.1% of females). 85.0% of all IA deaths involved firearms. More than a third of youth—41.2%—lacked prior psychiatric history.
Conclusion:
Our data shows over half of IAs occurring in youth with approximately three-quarters of completed youth suicides happening on IAs. In parsing cause of death in the all-age-cohort, the contribution of firearms figured even more prominently in the subsample of youth (85.0%) than those 25 and older (64.3%). The high IA lethality suggests that prevention efforts commencing after IA are too late for most victims.
Keywords: suicide attempt, completed suicide, Epidemiology
Introduction
In 2010, suicide was the second leading cause of death in American youth ages 10 to 24, with 12.7% of all suicides occurring in this age range.1 Although suicidal behavior occurs across the entire lifespan, it first emerges into prominence with the transition from childhood to adolescence,2,3 with suicide attempts peaking in mid-adolescence before decreasing with the transition into young adulthood.3–5
A recent study of suicidal behavior in adolescents 13 to 18 years old found the prevalence of suicidal ideation, plans, and attempts to be 12.1%, 4.0%, and 4.1%, respectively.6 Adolescent females are more likely to make suicide attempts,6 whereas males are more likely to die by suicide.7 Recurrent suicidal behavior is recognized to increase the likelihood of completed suicide8 and the surveys report between 50 and 200 suicide attempts for every completed suicide.7,9,10 The process of attempting suicide is theorized to sensitize the individual to suicidal actions; thereby making eventual suicide completion more likely.11 A key clinical tenet has, therefore, been that a history of prior suicide attempts is the most important risk factor for further attempts12 and future completed suicide.5,13
To date, most studies examining suicide risk after suicide attempt have relied on convenience samples limited to a particular attempt method, a specific treatment setting, or a specific type of care received after an attempt. As a result, these approaches have systematically overlooked those dying on IA. Our recent publication using an all-age cohort1 attempted to address this crucial omission14.For the first time, subjects were followed from their first suicide attempts coming to medical attention [index attempt (IA)], with those dead on their IA included in the findings. Using this novel approach in this all age cohort, we found that 60% of individuals died on their IA. This is the group convenience samples overlook. Firearms were disproportionately associated with IA lethality (OR=140; 95% CI=60–325). Moreover, over 80% of subsequent completed suicides in this cohort occurred within a year of the IA. Striking was the fact that over half (813/1490; 54.6%) of this cohort were under the age of 25 at the time of their IA.14
Having noticed not only the preponderance of youth in the all-age cohort but also the dearth of studies in the literature on this age group we decided to embark upon an investigation of the youth subsample, applying the novel approach of including youth dead on IA. We also chose to explore the role suicide method plays in completed youth suicides. Our goal was to more accurately define the risk of suicide after suicide attempt in youth.
In defining our age range of interest, we recognize that there is no universally accepted definition of what constitutes adolescence, youth, or young people.15 We have chosen to include subjects up until their twenty-fifth birthday, in accordance with the convention of many other suicide papers and consistent with Center for Disease Control definitions.
Method
The study cohort was comprised of residents from Olmsted County, Minnesota, USA. Located in southeastern Minnesota, Olmsted County is geographically isolated with the result that its residents almost exclusively receive medical care from two medical facilities within the county: Mayo Clinic and Olmsted Medical Center. All medical records from these facilities are contained in the Rochester Epidemiology Project (REP), a repository of medical and autopsy records for every patient seen in Olmsted County since the early 20th century. The REP data have generated hundreds of studies of this population isolate, with findings considered generalizable to much of the United States.16
Youth in the current study are a subsample of an all-age population-based cohort of suicide attempters upon which we have previously reported.14 We used a retrospective-prospective cohort study design. To identify the cohort, we searched the REP using billing codes (ICD-9) and Hospital International Classification of Diseases, Adapted, or International Classification of Disease that corresponded to any episode coded for suicidal ideation, suicidal behavior, or self-injurious behavior resulting in medical, surgical, and/or psychiatric evaluation. Once identified, records were searched manually and electronically for index suicide attempts occurring between January 1, 1986, and December 31, 2007. An IA was defined as a first lifetime suicide attempt coming to medical attention during the study period. We found 17,288 coded suicide events, corresponding to 8,352 individuals, of whom 5,283 were listed as Olmsted County residents at the time of the event. Of these 5,283 patients, 1,490 proved to have made IAs during the study period, with 813 (males, n=258; females, n=555) of these IAs inflicted by subjects between the ages 10 to 24.
Having identified the youth cohort, we compiled information regarding age at IA, method of IA, and care received following the IA, both immediately and after hospital release. We screened this cohort through the National Death Index database up to January 1, 2011 to determine who had died, and when and how they had died. For those patients who died within Olmsted County, we were able to confirm the National Death Index data with autopsy and coroner reports through the REP database.
Using chi-square tests for categorical variables and one-way analysis of variance with Tukey’s pairwise tests for age, demographic and clinical characteristics were compared among those who were alive at the end of the study period or who died by means other than suicide, those who died after their first suicide attempt, and those who died on subsequent attempt (Table 1). Multivariable logistic regression models were used to test age, gender, clinical factors, and method as predictors of death on initial attempt, or subsequent attempt. Time until completed suicide was plotted on a Kaplan-Meier curve. All analyses were conducted using SAS 9.4 (Cary, N.C.).
Table 1.
Demographics by Outcome of Initial Suicide Attempt
| Total | Death on First Attempt |
Death on Subsequent Attempt |
Alive or Death From Other Cause |
||||||
|---|---|---|---|---|---|---|---|---|---|
| N=813 | n=20 | n=9 | n=784 | ||||||
| Characteristic | Mean | SD | Mean | SD | Mean | SD | Mean | SD | p-value |
| Age (years) | 18 | 3.3 | 19.3 | 2.9 | 19.1 | 2.2 | 17.9 | 3.3 | 0.0978 |
| n | % | n | % | n | % | n | % | ||
| Sex (male) | 258 | 31.7 | 16 | 80.0 | 7 | 77.8 | 235 | 30.0 | <0.0001 |
| Method of index attempt | |||||||||
| Hanging/asphyxiation | 24 | 3.0 | 1 | 5.0 | 23 | 2.9 | |||
| Firearms/explosives | 27 | 3.3 | 17 | 85.0 | 5 | 55.6 | 5 | 0.6 | |
| Medication Overdose | 480 | 59.0 | 2 | 10.0 | 1 | 11.1 | 477 | 60.8 | |
| Non-medication Overdose | 30 | 3.7 | 1 | 11.1 | 29 | 3.7 | |||
| Poisoning | 19 | 2.3 | 1 | 11.1 | 18 | 2.3 | |||
| Motor vehicle accident | 13 | 1.6 | 13 | 1.7 | |||||
| Cutting/piercing | 198 | 24.4 | 1 | 11.1 | 197 | 25.1 | |||
| Other | 22 | 2.7 | 22 | 2.8 | |||||
| Type of index attempt management | |||||||||
| Medical hospitalization | 194 | 23.9 | 2 | 10.0 | 3 | 33.3 | 189 | 24.1 | |
| Surgical Hospitalization | 10 | 1.2 | 1 | 5.0 | 1 | 11.1 | 8 | 1.0 | |
| Psychiatric hospitalization | 351 | 43.2 | 1 | 5.0 | 3 | 33.3 | 347 | 44.3 | |
| No hospitalization | 341 | 41.9 | 18 | 90.0 | 4 | 44.4 | 319 | 40.7 | |
| Index attempt after-care follow-up | <0.0001 | ||||||||
| Present | 567 | 70.0 | - | - | 4 | 44.4 | 563 | 71.8 | |
| Absent | 226 | 30.0 | - | - | 5 | 55.6 | 221 | 28.2 | |
Results
813 youth were identified and followed for up to 25 years with 32 dying (3.9%) during the study period. Of these deaths, 29 were suicides accounting for 90.6% of the deaths and 3.6% of the cohort. Of these 29, 20 of these suicides occurred on IA and the nine remaining suicides occurred on subsequent attempt with all but one occurring before their 25th birthday. This meant that 71.4% (20/28) of suicides in youth occurred on IA. The mean age of the sample was 18.0 (SD=3.3), the mean age of those dying on IA was 19.3 (SD=2.9), and the mean age of those dying on subsequent attempts was 19.1 (SD=2.2; Table 1). We have chosen to include all 29 completed suicides in the subsequent calculations, as they occurred in subjects that made their first attempt prior to the age of 25.
The sample was sub-divided for analysis into three age brackets (10–14, 15–19, 20–24). At 53.1% (432/813), the majority of youth IAs occurred in the middle bracket, with the youngest age bracket of 10–14 accounting for 20.2% (164/813) of all IAs (Table 2). 1.8% (3/164) of 10–14 year olds, 2.1% (9/432) of 15–19 year olds and 3.7% (8/217) of 20–24 year olds died on their IA. Although members of the 20–24 year old age group killed themselves at the highest rate, the highest number of completed suicides by raw number were observed in the largest bracket comprised of the 15–19 year olds. Males disproportionately contributed to IA deaths, with 6.3% of males in the 15–19 year old group and 7.5% of males in the 20–24 year old group completing suicide on IA versus 0.3% of 15–24 and 0.8% of 20–24 year old females (Table 2).
Table 2.
Rate of Death by Age Group
| Index Death Rate | Subsequent Death Rate | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Attempt | Suicide | Survival | Suicide | Other Death | Any Death | |||||||
| Age Cohort | n | % of total | n | % | n | % | n | % | n | % | n | % |
| ALL | ||||||||||||
| 10–14 years old | 164 | 20.1 | 3 | 1.8 | 161 | 98.2 | 0 | 0 | 1 | 0.6 | 1 | 0.6 |
| 15–19 years old | 432 | 53.1 | 9 | 2.1 | 423 | 97.9 | 6 | 1.4 | 0 | 0 | 6 | 1.4 |
| 20–24 years old | 217 | 26.7 | 8 | 3.7 | 209 | 96.3 | 3 | 1.4 | 2 | 0.9 | 5 | 2.4 |
| Overall | 813 | 20 | 2.5 | 793 | 97.5 | 9 | 1.1 | 3 | 0.4 | 12 | 1.5 | |
| MALE | ||||||||||||
| 10–14 years old | 36 | 14 | 1 | 2.8 | 35 | 97.2 | 0 | 0 | 0 | 0 | 0 | 0 |
| 15–19 years old | 128 | 49.6 | 8 | 6.3 | 120 | 93.7 | 6 | 5 | 0 | 0 | 6 | 5 |
| 20–24 years old | 94 | 36.4 | 7 | 7.5 | 87 | 92.5 | 1 | 1.2 | 1 | 1.1 | 2 | 2.3 |
| Overall | 258 | 16 | 6.2 | 242 | 93.8 | 7 | 2.9 | 1 | 0.4 | 8 | 3.3 | |
| FEMALE | ||||||||||||
| 10–14 years old | 128 | 23.1 | 2 | 1.6 | 126 | 98.4 | 0 | 0 | 1 | 0.8 | 1 | 0.8 |
| 15–19 years old | 304 | 54.8 | 1 | 0.3 | 303 | 99.7 | 0 | 0 | 0 | 0 | 0 | 0 |
| 20–24 years old | 123 | 22.2 | 1 | 0.8 | 122 | 99.2 | 2 | 1.6 | 1 | 0.8 | 3 | 2.5 |
| Overall | 555 | 4 | 0.7 | 551 | 99.3 | 2 | 0.4 | 2 | 0.4 | 4 | 0.7 | |
Overall, males represented less than a third (258/813; 31.7%) of the youth sample but accounted for approximately four-fifths of the deaths by suicide (23/29: 79.3% of suicides; 8.9% of males). 16 of 23 suicides (69.6%; 6.2% males) occurred on IA. 7 subsequent male deaths occurred by suicide with only one of these occurring after his 25th birthday. Overall, 2.9% of males surviving their IAs subsequently died by suicide. In contrast, females comprised more than two-thirds (555/813: 68.3%) of the sample but accounted for approximately a fifth of the suicides (6/29: 20.7% of suicides; 1.1% of females). Four of 6 female suicides (66.7%) happened on IA, representing 0.7% of females. 0.4% of female IA survivors died on a subsequent attempt (Table 2).
The attempt method was highly associated with lethality. Of those dying on IA, 85.0% used firearms. Gunshot was implicated in 87.0% (20/23) of all male deaths, with 7.8% (20/258) of the male cohort dead by this method. Of the nine IA survivors who perished on subsequent attempt, seven (77.8%) also died by firearms. Underscoring the high lethality of this method is the odds of dying by firearm on IA relative to other suicide methods (OR=334; 95% CI=75.6, >999; p<0.0001; Table 3). Given the wide confidence intervals we observed, the lower bound likely reflects a more accurate estimate of this relationship.
Table 3.
Risk of Death on Initial and Subsequent Attempt
| Event | Odds Ratio | 95 % CI | p |
|---|---|---|---|
| Death at first attempt | |||
| Predictor | |||
| Age | 1.097 | 0.882, 1.365 | 0.4072 |
| Male | 1.797 | 0.386, 8.378 | 0.4554 |
| Shooting method | 334.049 | 75.566, >999 | <0.0001 |
| Subsequent completed suicide attempt (index survivors only) | |||
| Predictor | |||
| Male | 6.598 | 1.394, 34.716 | 0.0180 |
| Follow-up psych appt | 0.304 | 0.073, 1.262 | 0.1011 |
| Psych hosp | 1.373 | 0.312, 6.044 | 0.6754 |
| Surg hosp | 0.094 | 0.009, 1.031 | 0.0530 |
| Medical hosp | 0.632 | 0.149, 2.682 | 0.5334 |
Note: Hosp = hospital.
For those dying from subsequent attempts, male sex was associated with a higher risk of completed suicide attempt (OR=6.6, 95% CI= 1.394, 34.716; p=0.018). Hospitalization after IA did not achieve statistical significance in terms of reducing the risk for subsequent death by suicide. The presence of after-care follow-up was found to be protective in the univariate analysis (p<0.0001), but statistical significance did not hold for the multivariate analysis (0R=0.304; 95% CI=0.073, 1.262; p<0.1011; Table 3).
Prior to their IA, 41.2% had no history of psychiatric diagnosis, mental health visits of any sort, or psychotropic medication trials. The presence of a medically documented psychiatric history was lowest in the 10–14 year old group (Table 4).
Table 4.
Mental Health Care History
| Age Group | 10–14 | 15–19 | 20–24 | p | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Past psychiatric history | 83 | 50.6 | 233 | 53.9 | 125 | 57.6 | 0.391 |
| Past psychiatric medication | 51 | 31.1 | 129 | 29.9 | 75 | 34.6 | 0.475 |
| Past psychiatric diagnosis | 77 | 47.0 | 199 | 46.1 | 111 | 51.2 | 0.465 |
| No past psychiatric record | 72 | 43.9 | 181 | 41.9 | 82 | 37.8 | 0.444 |
Of survivors dying in subsequent suicide attempts, both females (2/2; 100%) and 4/7 males (57.1%) did so within a year of their IA. Indeed, all four males died within six months of their IAs (Figure 1).
Figure 1.
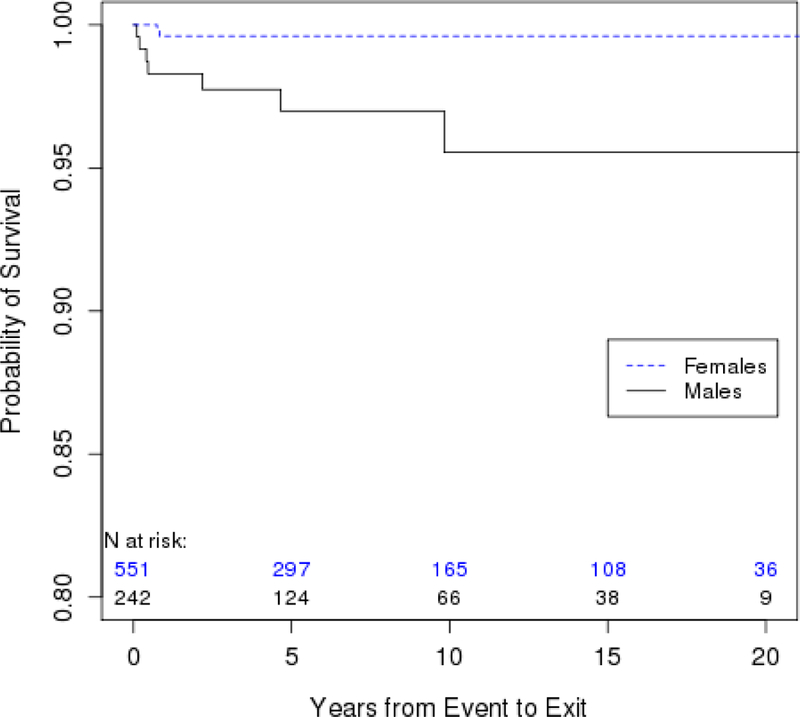
Kaplan-Meier Curve Corresponding to Survival Probability From Completed Suicide Attempt Either at Index Attempt (IA) or After IA, by Sex.
Discussion
This is the first study examining suicide risk in youth via a cohort defined by their IA. Including youth presenting to the coroner as well as the emergency room more accurately captures the prevalence of completed suicide on IA. By including youth that died on their IA, we show that the outcome for any suicide attempt is grimmer for this population—in particular for males—than was previously thought.
In our original all-age publication, we reported that the highest rates of suicide completion on IA were found in the 25–44 and ≥65 year old age groups at 4.2% and 6.5%, respectively. In contrast, the rate of completed suicide in youth age 10–24 was lower at 2.5%.
This lower percentage is deceptive, however, in that it does not reflect the disproportionate contribution in absolute numbers of the youth group to both initial suicide attempts and completed suicides. The 813 IAs in youth constituted more than half of all-age IAs (54.6%: 813/1490) as well as 41.7% (20/48) of deaths on IA. Moreover, youth attempters were more likely to die on initial attempts than their elders: 71.4% (20/28) versus 52.8% (28/53) in those 25 years or older. Firearms likely play a pivotal role in this discrepancy, with 85.0% (17/20) of youth IA suicides the result of gunshot versus 64.3% (18/28) in those 25 years or older. This risk is further magnified when one considers that the 15-year time span of youth is being compared with all of adulthood.
In raw numbers, we found—consistent with other published reports—four times as many male compared to female suicides. The raw numbers do not tell an accurate story. One in 11 males in our cohort died by suicide, versus one in 93 females. The overall ratio of male-to-female suicide deaths relative to number attempting was 8.2:1, more than double the gender discordance of the previously established 4:1 ratio.17 Additionally, the suicide literature frequently cites 50:1 to 200:1 attempts per completed suicide.7,9,10 We would underscore that these previously reported numbers do not distinguish between IA and subsequent attempt deaths. For the first time in youth we report on suicides that make this distinction and share a number that is more serious than previously thought, with 1 in 41 completed suicides occurring on IA.
Our data challenge previous reports that proportionately more males than females who succeed in killing themselves do so on IA. Two prior psychological autopsy studies reported that more females than males had histories of prior attempts, thus suggesting that more males than females died on IA.18,19 Our study contradicts this finding, given nearly identical proportions of IA deaths—69.6% of male suicides and 66.7% of female suicides occurring on IA—in our cohort.
Our study emphasizes the deadliness of firearms in completed suicides. Guns accounted for 17/20 (85.0%) of deaths on IA and 7/9 (77.8%) of subsequent deaths in survivors. Firearms disproportionately accounted for method of death on IA with an odds ratio of 334 (95% CI = 75.6, >999; p<0.0001). While we recognize that the wide confidence interval may weaken the robustness of this finding, we would note that the lower bound of the confidence interval is still indicative of a very large effect and also 25.2% higher than the lowest margin reported in the all-age cohort. This concurs with other studies that show that firearms access is linked to higher risk of completed suicide.18,20 and that reduced access to firearms is a protective factor against suicide.21 A recent study reports that suicide rates in rural youth are twice as high compared with urban youth, a discrepancy in part linked to firearms.22 Consistent with this study’s finding, the rural setting of Olmsted County from which we drew our cohort may contribute to the high incidence of firearm use. Furthermore, a recent publication found that while firearms were present in 43.5% of households with children with self-harm risk factors, firearm storage did not significantly change in these households versus those without such a child.23 This concerning report dovetails with our finding of firearms being implicated in a high percentage of subsequent completed suicides in IA survivors, and suggests the potential life-saving value of limiting gun access in first-attempt survivors.
Concurring with our findings from the overall all-age sample, the failure to include IA deaths underestimates the completion rate in youth attempters.14 In this youth cohort, 20/813 (2.5%) died on IA, however, of the survivors, only 9/793 (1.1%) went on to die by suicide. This rate decline between the cohort as a whole and the cohort of IA survivors was seen in both males and females (males: from 6.2% to 2.9%; females: from 0.7% to 0.4%).
Our findings also suggest that for a sizeable number of youth, an IA is also the first psychiatric evidence of psychopathology coming to the attention of medical providers. Over a third of our cohort (41.2%) had no identifiable psychiatric history prior to their IA. This correlates closely with a recent consecutive case series of youth suicide from the United Kingdom that found 46% had no history of psychiatric diagnosis and 43% had no prior service contacts.24 Overall, our data underscore the challenge suicide prevention poses when a suicide attempt is the first presenting psychiatric complaint.
Our study has some methodological limitations. The inclusion of subjects into the cohort required the IAs to have been coded as suicide related deaths. It has been reported in youth that medical examiners do not always code the deaths of individuals perishing under suspicious circumstances as suicides, thereby undercutting reported suicides.25 A recent national survey on suicidal behavior in 13-to 18-year-olds found 4.1% reporting a history of a suicide attempt.6 Clearly, as clinical practice and the literature affirm, many suicidal actions go undetected by patients’ families and clinicians, thus our findings potentially underestimate the number of attempts occurring in the community. While valuable, retrospective surveys of patients’ suicidal behavior are also prone to recall biases and lack a clinical assessment. While our approach risks not including covert suicide attempts, it is grounded in documented attempts and clearly shows the mortality and morbidity associated with suicide attempts that come to medical attention. Finally, by the nature of the enrollment process, the follow-up ranged from 3 to 25 years; completed suicides after January 1, 2011, will not have been detected, even as our findings suggest that most subsequent suicides will happen comparatively soon after the IA.
It is well established in youth that prior suicide attempt is a risk factor for completed suicide. Our findings from a naturalistic community sample followed from IA shows that the lethality of any suicide attempt in youth is higher than previously appreciated. In considering youth in the context of the all-age-cohort we previously report, risk in the youth subsample is magnified. Our study shows that 71.4% of youth dying by suicide succumbed on IA, 18.6 percentage points higher than for those 25 and older in the all-age cohort. It also shows firearms implicated in 85.0% of lethal IAs in youth. Finally, for more than a third of the youth sample, their IAs were their first mental health encounters.
These findings have substantial public health implications and suggest that suicide prevention efforts that target suicide survivors have missed the majority of those who die by suicide. We believe that suicide prevention strategies must therefore target youth prior to their first attempt, in particular males, in whom index attempts are particularly lethal. Reducing ease of access to firearms is critical in this age group in order to prevent deaths not only on IA but also in subsequent attempts.
Acknowledgements:
The authors wish to thank Lori Solmonson, Dr. McKean’s research secretary, for her generous and enthusiastic assistance in helping to prepare this manuscript for submission.
Funding: All authors report no grant funding for the work on this manuscript.
Footnotes
Disclosures:
Dr. Bostwick has received funding from the National Institute on Aging (grant U01AG-45390; PI: Boeve) and has delivered non-industry-sponsored CME lectures.
Drs. McKean and Pabbati and Ms. Geske report no biomedical financial interests or potential conflicts of interest.
Previously presented: Part of this study was presented at the Mayo Clinic School of Continuous Professional Development, Aeschi West, in Vail, CO, June 8–10, 2017 and Grand Rounds, Medical College of Wisconsin, in Milwaukee, WI, April 12, 2017.
Ms. Geske served as the statistical expert for this research.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. 10 Leading Causes of Death by Age Group, United States −2010. 2010; https://www.cdc.gov/injury/wisqars/pdf/10lcid_all_deaths_by_age_group_2010-a.pdf. Accessed August 9, 2018.
- 2.Bolger N, Downey G, Walker E, Steininger P. The onset of suicidal ideation in childhood and adolescence. J Youth Adolesc. 1989;18(2):175–190. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–626. [DOI] [PubMed] [Google Scholar]
- 4.Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL. Gender differences in suicide attempts from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry. 2001;40(4):427–434. [DOI] [PubMed] [Google Scholar]
- 5.Shaffer D, Gould MS, Fisher P, et al. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry. 1996;53(4):339–348. [DOI] [PubMed] [Google Scholar]
- 6.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shain B, Committee On Adolescence. Suicide and suicide attempts in adolescents. Pediatrics. 2016;138(1). [DOI] [PubMed] [Google Scholar]
- 8.Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47(3–4):372–394. [DOI] [PubMed] [Google Scholar]
- 9.Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE, eds. Reducing Suicide: A National Imperative. Washington, DC: National Academy Press Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 10.Husain SA. Current perspective on the role of psychosocial factors in adolescent suicide. Psychiatr Ann. 1990;20(3):122–127. [Google Scholar]
- 11.Spirito A, Esposito-Smythers C. Attempted and completed suicide in adolescence. Annu Rev Clin Psychol. 2006;2:237–266. [DOI] [PubMed] [Google Scholar]
- 12.Lewinshohn PM, Rhode P, Seeley JR. Psychosocial risk factors for future adolescent suicide attempts. Journal of Consultative Clinical Psychology. 1994;62(287–305). [DOI] [PubMed] [Google Scholar]
- 13.Beautrais AL. Further suicidal behavior among medically serious suicide attempters. Suicide Life Threat Behav. 2004;34(1):1–11. [DOI] [PubMed] [Google Scholar]
- 14.Bostwick JM, Pabbati C, Geske JR, McKean AJ. Suicide attempt as a risk factor for completed suicide: Even more lethal than we knew. Am J Psychiatry. 2016;173(11):1094–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hawton K, Saunders KE, O’Connor RC. Self-harm and suicide in adolescents. Lancet. 2012;379(9834):2373–2382. [DOI] [PubMed] [Google Scholar]
- 16.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brendel RW, Lagomasino IT, Perlis RH, Stern TA. The Suicidal Patient. In: Stern TA, ed. Massachusetts General Hospital Comprehensive Clinical Psychiatry, 1st ed Philadelphia, PA: Mosby/Elsevier; 2008. [Google Scholar]
- 18.Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age-and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry. 1999;38(12):1497–1505. [DOI] [PubMed] [Google Scholar]
- 19.Marttunen MJ, Aro HM, Lonnqvist JK. Adolescent suicide: endpoint of long-term difficulties. J Am Acad Child Adolesc Psychiatry. 1992;31(4):649–654. [DOI] [PubMed] [Google Scholar]
- 20.Brent DA. Firearms and suicide. Ann N YAcadSci. 2001;932:225–239; discussion; 239–240. [DOI] [PubMed] [Google Scholar]
- 21.Grossman DC, Mueller BA, Riedy C, et al. Gun storage practices and risk of youth suicide and unintentional firearm injuries. JAMA. 2005;293(6):707–714. [DOI] [PubMed] [Google Scholar]
- 22.Fontanella CA, Hiance-Steelesmith DL, Phillips GS, et al. Widening rural-urban disparities in youth suicides, United States, 1996–2010. JAMA Pediatr. 2015;169(5):466–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scott J, Azrael D, Miller M. Firearm Storage in Homes With Children With Self-Harm Risk Factors. Pediatrics. 2018;141(3):e20172600. [DOI] [PubMed] [Google Scholar]
- 24.Rodway C, Tham SG, Ibrahim S, et al. Suicide in children and young people in England: a consecutive case series. Lancet Psychiatry. 2016;3(8):751–759. [DOI] [PubMed] [Google Scholar]
- 25.Gosney H, Hawton K. Inquest verdicts: Youth suicides lost. Psychiatr Bull. 2007;31:203–205. [Google Scholar]


