Abstract
Background:
One mechanism through which social stigma of HIV affects health outcomes for people living with HIV (PLWH) is via internalization of stigma. However, this transformation of social stigma in the community into internalized stigma may not be of the same magnitude for all PLWH. We examined the moderating effects of 3 personality traits—fear of negative social evaluation, attachment-related anxiety, and dispositional resilience—in transforming perceived stigma in the community into internalized stigma. Furthermore, we investigated downstream effects of these moderated associations on depressive symptoms and antiretroviral treatment (ART) adherence.
Setting/Methods:
In Study 1, data from 203 PLWH in the southeast US were analyzed controlling for age, sex, education, race, and time on ART. In Study 2, data from 453 women in a multi-site study were analyzed controlling for age, education, race, time on ART, and substance use.
Results:
In both studies, fear of negative evaluation and attachment-related anxiety moderated the effect of perceived HIV stigma in the community on internalized HIV stigma: People higher on those moderating variables had stronger associations between perceived stigma in the community and internalized stigma. In study 2, resilience was assessed, and also moderated the effect of perceived HIV stigma in the community on internalized stigma. In moderated mediation models, fear of negative evaluation, attachment-related anxiety, and resilience moderated the indirect effect of perceived HIV stigma in the community on ART adherence and depression through internalized stigma.
Conclusions:
Interventions to assuage internalization of HIV stigma should focus on bolstering attachment-related security, social competence, and resilience.
Keywords: Negative evaluation, attachment, resilience, HIV, stigma, adherence
HIV stigma remains a significant threat to health and well-being among people living with HIV (PLWH).1–8 Increasingly, we are learning how PLWH experience and process stigma at the individual level.2,3 In a study using experience sampling method (ecological momentary assessment) among men living with HIV, recent experiences of discrimination predicted current levels of internalized HIV stigma in within-participant analyses.9 In addition, many researchers agree that internalized stigma has its roots in perceptions of stigma in the community,1,2,10,11 and there is evidence that the effect of perceived HIV stigma in the community on health outcomes of PLWH is mediated by the internalization of stigma in the community.1 These findings suggest that intrapersonal mechanisms may be key determinants of how interpersonal experiences such as social stigma in communities become internalized and have downstream effects on individual health.
However, it is possible that the transformation of social stigma in communities into internalized stigma is not of the same magnitude for all PLWH; those with certain traits that trigger insecurities/doubts about their social value or social status may be more vulnerable to internalizing stigma. Research is needed to identify potential buffers (or enhancers) of the internalization of stigma.10,12 We propose that three intrapersonal variables (personality traits)— fear of negative social evaluation, attachment-related anxiety, and dispositional resilience—play important roles in the internalization of stigma perceived in the community.
Individuals who worry that others will judge them negatively may be sensitized to social status issues and may monitor the environment frequently for cues about negative evaluation.13 Social stigma creates a threat to one’s status12,14,15 and may activate worries about one’s value, especially if there are pre-existing insecurities about one’s value. Research in other areas—such as body image and mothering perceptions—suggests that individuals are more likely to internalize negative perceptions in the community about a certain attribute if they fear negative social evaluation.16 Thus, people with higher fear of negative social evaluation may be more vulnerable to being affected by social stigma and more susceptible to internalizing stigma.
Similarly, attachment-related anxiety may moderate the association between perceived HIV stigma in the community and internalized stigma. According to attachment theory, interactions with others shape how people perceive themselves, their relationships with others, and stressors.17–19 Among the two dimensions of attachment insecurity—attachment-related anxiety and attachment-related avoidance—attachment-related anxiety has particular importance in this research. Individuals with high attachment-related anxiety have chronic worries about their value in interpersonal relationships, generalized worries about rejection, and doubts about self-worth.20–22 Furthermore, their perceived self-worth heavily depends on others’ approval.23–26
Research suggests that resilient personality—one’s capacity to overcome adversity27,28—is a key determinant of health disparities in HIV populations,28 and dispositional resilience may buffer the negative effects of HIV stigma on HIV-related health outcomes.29,30 Research in other areas suggests that similar constructs—such as dispositional self-esteem—are protective against negative self-evaluations in the face of upward comparisons with others who possess more valued attributes.31 Therefore, PLWH with higher levels of resilience may view themselves as capable of thriving regardless of perceived HIV stigma in the community—and not internalize stigma.
Thus, we hypothesized that higher fear of negative evaluation and attachment-related anxiety would exacerbate the association between perceived HIV stigma in the community and internalized stigma, while resilience would buffer this association. We further explored whether these associations extend to the downstream health outcomes of depressive symptoms and ART adherence (see Figure 1). Two distinct samples of PLWH were used for the present cross-sectional analyses.
Figure 1.
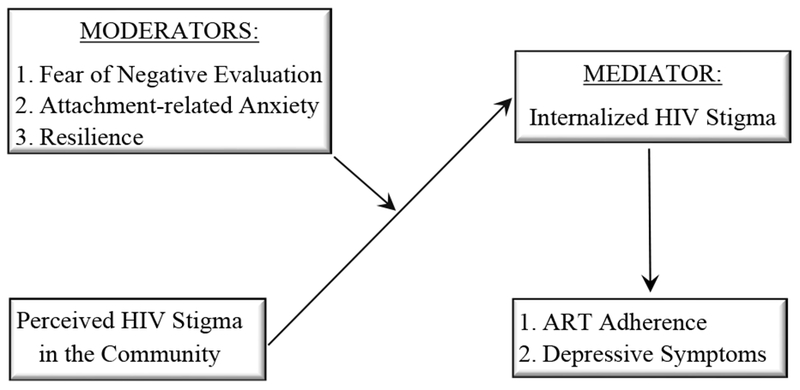
Proposed moderated mediation model.
METHODS
Participants and Procedures
Study 1 included 203 participants recruited from an outpatient HIV care clinic in Birmingham, Alabama. Inclusion criteria were currently being on an antiretroviral treatment (ART) regimen and not reporting current substance use. Participants completed measures via computer-based survey.
Study 2 included 453 women who were part of the Women’s Adherence and Visit Engagement (WAVE) sub-study of the Women’s Interagency HIV Study (WIHS), a multi-site cohort study.32 WAVE includes data on psychosocial aspects of living with HIV among women at four of the 10 WIHS sites, including San Francisco, CA, Atlanta, GA, Birmingham, AL, and Jackson, MS. Data collected through WAVE are linked to data collected through the WIHS core data collection, including self-reported depressive symptoms and ART adherence.
Measures
Demographic Information.
In both studies, participants reported their demographic information including their age, sex, race, education, and time on ART. In study 2, participants reported whether they used substances in the past 6 months.
HIV stigma.
In both studies, two subscales of the revised HIV Stigma Scale33 were used to assess perceived HIV stigma in the community and internalized HIV stigma. Participants responded to questions on a 4-point scale ranging from 1: “strongly disagree” to 4: “strongly agree.” Perceived HIV stigma in the community was measured using the 6-item concern with public attitudes subscale; e.g., “Most people believe that a person with HIV is dirty.” (Study 1 α = .84; Study 2 α = .86). Internalized HIV stigma was measured using the 7-item negative self-image subscale; e.g., “I feel I am not as good as others because I have HIV.” (Study 1 α = .85; Study 2 α = .86).
Fear of negative evaluation.
In both studies, the Brief Fear of Negative Evaluation Scale34 assessed participants’ fear of negative evaluation using 12 questions; e.g., “I am frequently afraid of other people noticing my shortcomings.” Participants responded using a 5-point scale from 1: “not at all characteristic of me” to 5: “extremely characteristic of me” (Study 1 α = .81; Study 2 α = .82).
Attachment-related anxiety:
In both studies, the 18-item version of the Experiences in Close Relationships (ECR35) was used. ECR assesses two dimensions of attachment insecurity: attachment-related anxiety (e.g., “I worry a lot about my relationships;” Study 1 α = .90, Study 2 α = .90) and attachment-related avoidance (e.g., “I prefer not to show a partner how I feel deep down”). Participants responded to each item on a 7-point Likert scale.
Dispositional resilience.
The Brief Resilience Scale36 is a 6-item measure of dispositional resilience; e.g., “I tend to bounce back quickly after hard times.” Participants of only Study 2 responded to each item on a 5-point Likert scale (α = .79).
Depressive symptoms.
In Study 1, depressive symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-937). It queries how often participants were bothered by symptoms (e.g., “little interest of pleasure in doing things”) over the last 2 weeks on a 4-point scale from 0: “not at all,” to 3: “nearly every day.” In Study 2, depressive symptoms were assessed using the Center for Epidemiological Studies Depression scale (CES-D38). CESD asks how often participants experienced symptoms over the past week (e.g., “I thought my life had been a failure.”) on a scale from 0: “rarely or none of the time (less than 1 day),” to 4: “most or all of the time (5-7 days).”
ART Adherence.
In Study 1, participants reported their ability to take all HIV medication prescribed using a 6-point scale ranging from 1 (very poor) to 6 (excellent). Literature suggests this is a valid adherence measure associated with viral suppression.39,40 Responses were dichotomized as 1: excellent adherence (optimal) and 0: less than excellent adherence (sub-optimal). In Study 2, adherence was assessed with one self-reported item asking participants how often they took their ART medications as prescribed over the past 6 months. Responses ranged from 1: “100% of the time” to 5 “I haven’t taken any of my prescribed medications.” As in previous studies, responses were dichotomized using an empirically supported cutoff for optimal versus sub-optimal adherence at 95%; 1: ≥ 95% (optimal adherence) and 0: <95% (sub-optimal adherence).39,40
Data Analysis
The following covariates were used in all Study 1 analyses: age, sex, education attainment, race (0: non-white, and 1: white), and time on ART. For Study 2 analyses, the following covariates were used: age, education attainment, race (0: non-white, and 1: white), substance use, and time on ART. Linear models were used for continuous outcomes and logistic models were used for binary outcomes. We first tested interaction effects of each proposed moderator (fear of negative evaluation, attachment-related anxiety, and resilience) with perceived HIV stigma in the community on internalized HIV stigma. Next, we evaluated moderated mediation models. We tested whether fear of negative evaluation, attachment-related anxiety, and resilience moderated the indirect effect of perceived HIV stigma in the community on depression (and then on ART adherence) through internalized stigma. The overall model hypothesized with its distinct moderator and outcome variables is depicted in Figure 1. We tested fear of negative evaluation and attachment-related anxiety using data from both studies and the additional moderator of resilience with Study 2 data.
Exploratory moderated mediation analyses were conducted with PROCESS, a regression-based macro for SPSS.41 Bootstrapping was used to evaluate indirect effects of the models.41,42 A significant indirect effect is indicated by a (bias-corrected) confidence interval not containing zero. Moderation effects were evaluated examining simple slopes at one standard deviation above and below the mean of each moderator. Unstandardized path/regression coefficients are reported for all analyses.
RESULTS
Descriptive statistics and correlations among study variables are presented in Table 1.
Table 1.
Descriptive Statistics and correlations for key variables of Study 1 and Study 2.
| Study 1 (N=203) | Study 2 (N=453) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | M (SD) range or n (%) | CS | IS | AA | FNE | Dep | Adh | M (SD), range or n (%) | CS | IS | AA | FNE | Res | Dep | Adh |
| Age (years) | 44.8 (11.1) 24-71 | −.007 | −.099 | −.186** | −.121 | .010 | .098 | 49.1 (9.4) 28-82 | −.139** | −.120* | −.068 | −.057 | −.038 | .006 | .024 |
| Female† | 74 (36%) | −.085 | −.027 | −.063 | −.035 | −.165* | .031 | 453 (100%) | --- | --- | --- | --- | --- | --- | --- |
| Non-white Race† | 130 (64%) | .041 | .020 | −.057 | .021 | −.040 | .269*** | 389 (86%) | −.182*** | −.146** | .026 | −.011 | .055 | .041 | .071 |
| Education | 3.1 (1.0) 1-6 | −.001 | −.084 | .027 | −.028 | −.119 | .160* | 4.2 (1.0) 2-7 | .029 | −.024 | −.024 | .023 | .038 | −.085 | −.022 |
| Months on ART | 95.8 (63.1) 12-242 | −.075 | −.050 | −.135 | .026 | −.095 | .041 | 104.1 (71.8) 1-279 | −.166** | −.166** | −.009 | −.019 | −.006 | .067 | .019 |
| No SU† | --- | --- | --- | --- | --- | --- | --- | 304 (68%) | −.054 | .021 | .093 | −.023 | −.015 | .140 | −.182*** |
| Perceived Stigma in Community | 2.7 (0.6) 1-4 | 1 | .531*** | .396*** | .343*** | .284*** | −.142 | 2.7 (0.7) 1-4 | 1 | .456*** | .318*** | .214*** | −.202*** | .186*** | −.071 |
| Internalized HIV Stigma | 2.0 (0.7) 1-4 | 1 | .509*** | .623*** | .280*** | −.174* | 2.0 (0.7) 1-4 | 1 | .394*** | .431*** | −.483*** | .407*** | −.114* | ||
| Attachment-related Anxiety | 3.6 (1.6) 1-7 | 1 | .547*** | .246 *** | −.275*** | 3.4 (1.5) 1-7 | 1 | .462*** | −.434*** | .401*** | −.080 | ||||
| Fear of Negative Evaluation | 2.6 (0.7) 1-5 | 1 | .297*** | −.060 | 2.4 (0.7) 1-5 | 1 | −.458*** | .348*** | −.133** | ||||||
| Dispositional Resilience | --- | --- | --- | --- | --- | --- | --- | 3.6 (0.8) 1-5 | 1 | −.476*** | .026 | ||||
| Depressive Symptoms | 3.7 (4.7) 0-27 | 1 | −.068 | 14.5 (12.1) 0-54 | 1 | −.191*** | |||||||||
| Sub-optimal ART Adherence† | 47 (22%) | 1 | 78 (18%) | 1 | |||||||||||
Notes:
For dichotomous variables, reference group=0.
p<.05.
p<.01.
p<.001.
SU=Substance Use; IS=Internalized HIV stigma; CS=Perceived HIV Stigma in the Community; AA=Attachment-related anxiety; FNE=Fear of Negative Evaluation; Res=Dispositional Resilience; Dep=Depressive Symptoms; Adh=ART adherence
Study 1 Results
The regression equation using internalized HIV stigma as the dependent variable revealed a significant interaction between fear of negative evaluation and perceived HIV stigma in the community (B = 0.25, SE = 0.09, t = 2.72, p = 0.007).a Follow-up simple slope analyses are depicted in Figure 2 and revealed that the effect of perceived HIV stigma in the community was larger at one standard deviation above the mean for fear of negative evaluation (B = 0.55, SE = 0.09, t = 6.15, p < 0.001) compared to the effect of perceived HIV stigma in the community at one standard deviation below the mean for fear of negative evaluation (B = 0.21, SE = 0.08, t = 2.48, p = 0.01). That is, at high levels of fear of negative evaluation (+1SD), internalized HIV stigma increased 0.55 units for every unit increase in perceived HIV stigma in the community; whereas at low levels of fear of negative evaluation (−1 SD) internalized HIV stigma only increased 0.21 units for every unit increase in perceived HIV stigma in the community.
Figure 2.
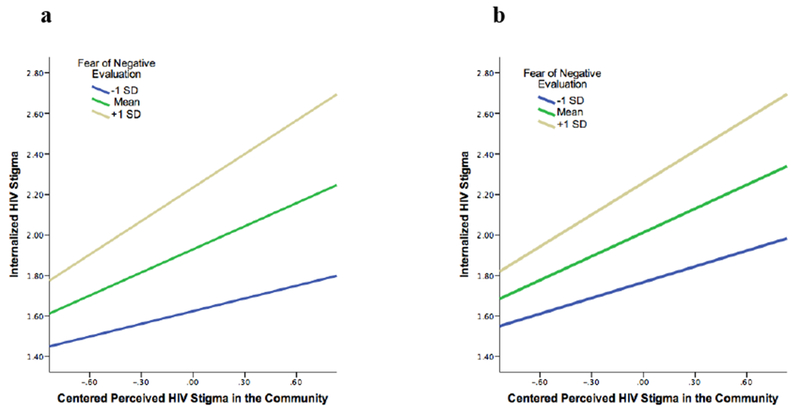
Interaction of fear of negative evaluation with perceived HIV stigma in the community (centered) on internalized HIV stigma in a) Study 1, and b) Study 2.
Next, attachment-related anxiety was entered as a moderator instead of fear of negative evaluation, which produced similar results. The interaction between attachment-related anxiety and perceived HIV stigma in the community had a significant effect (B = 0.10, SE = 0.04, t = 2.80, p = 0.006).b Follow-up simple slope analyses are shown in Figure 3 and revealed that the effect of perceived HIV stigma in the community was larger at one standard deviation above the mean for attachment-related anxiety (B = 0.58, SE = 0.09, t = 6.60, p < 0.001) compared to the effect of perceived HIV stigma in the community at one standard deviation below the mean for attachment-related anxiety (B = 0.25, SE = 0.09, t = 2.81, p = 0.006). Individuals reporting higher attachment-related anxiety had 0.58 units increase in internalized HIV stigma for every unit increase in HIV stigma in the community, compared to individuals with lower attachment-related anxiety whose internalized HIV stigma increased by 0.25 units. Results were very similar when attachment-related avoidance was added as a covariate.
Figure 3.
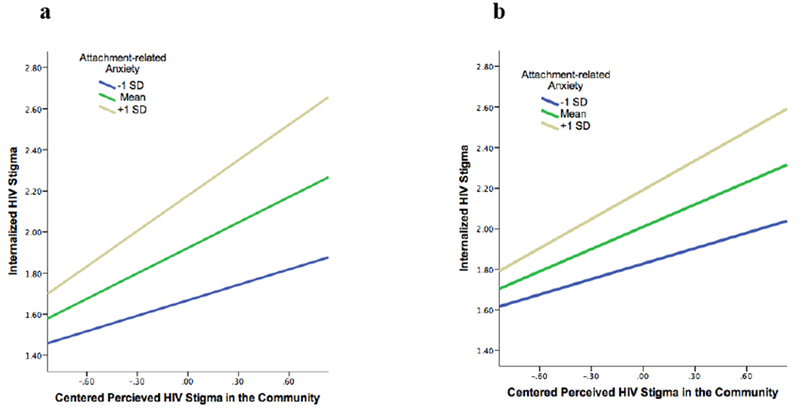
Interaction of attachment-related anxiety with perceived HIV stigma in the community (centered) on internalized HIV stigma in a) Study 1 and b) Study 2.
We tested the moderated mediation hypothesis that the indirect effect of perceived HIV stigma in the community on depressive symptoms through internalized HIV stigma is moderated by fear of negative evaluation and attachment-related anxiety.c The index of moderated mediation was significant: index = 0.33, SE = 0.20, 95% CI = 0.03, 0.81. Individuals with higher fear of negative evaluation (+1 SD) had an increase of 0.74 units in depressive symptoms for every unit increase in perceived HIV stigma in the community through internalized HIV stigma. On the other hand, individuals with lower fear of negative evaluation (−1 SD) had only 0.28 units increase in depressive symptoms for every unit increase in perceived HIV stigma in the community through internalized HIV stigma. The index of moderated mediation was also significant when attachment-related anxiety was the moderator: index = 0.14, SE = 0.09, 95% CI = 0.01, 0.36.c
When ART adherence was the outcome,d fear of negative evaluation did not moderate the indirect effect of perceived HIV stigma in the community through internalized HIV stigma (index = −0.10, SE = 0.10, 95% CI = −0.33, 0.06). When attachment-related anxiety was entered as the moderator, the index of moderated mediation was also not significant (index = −0.05, SE = 0.04, 95% CI = −0.15, 0.02).
Study 2 Results
The regression equation using internalized HIV stigma as the dependent variable again revealed a significant interaction between fear of negative evaluation and perceived HIV stigma in the community (B = 0.18, SE = 0.05, t = 3.40, p < 0.001).e Follow-up simple slope analyses are depicted in Figure 2 and revealed that the effect of perceived HIV stigma in the community was larger at one standard deviation above the mean for fear of negative evaluation (B = 0.53, SE = 0.06, t = 8.43, p < 0.001) compared to the effect of perceived HIV stigma in the community at one standard deviation below the mean for fear of negative evaluation (B = 0.26, SE = 0.06, t = 4.66, p < 0.001). Individuals reporting higher fear of negative evaluation had 0.53 units increase in internalized HIV stigma for every unit increase in perceived HIV stigma in the community; relative to individuals reporting lower fear of negative evaluation whose internalized HIV stigma increased by 0.26 units for every unit increase in perceived HIV stigma in the community.
As in Study 1, results were similar when attachment-related anxiety was used instead of fear of negative evaluation as the moderator. The interaction between attachment-related anxiety and perceived HIV stigma in the community had a significant effect (B = 0.07, SE = 0.03, t = 2.71, p = 0.01).f Follow-up simple slope analyses (Figure 3) revealed that the effect of perceived HIV stigma in the community was larger at one standard deviation above the mean for attachment-related anxiety (B = 0.48, SE = 0.07, t = 7.17, p < 0.001) compared to the effect of perceived HIV stigma in the community at one standard deviation below the mean for attachment-related anxiety (B = 0.25, SE = 0.06, t = 4.10, p < 0.001). Individuals with higher attachment-related anxiety had 0.48 units increase in internalized HIV stigma for every unit increase in perceived HIV stigma in the community compared to individuals with lower attachment-related anxiety whose internalized HIV stigma increased by 0.25 units for every one unit increase in perceived HIV stigma in the community. Results were very similar when attachment-related avoidance was also added as a covariate.
Finally, we examined resilience as a potential moderator. The interaction between resilience and perceived HIV stigma in the community had a significant effect (B = −0.16, SE = 0.05, t = −3.89, p < 0.001).g Follow-up simple slope analyses (Figure 4) revealed that the effect of perceived HIV stigma in the community was larger at one standard deviation below the mean for resilience (B = 0.49, SE = 0.06, t = 8.48, p < 0.001) compared to the effect of perceived HIV stigma in the community at one standard deviation above the mean for resilience (B = 0.24, SE = 0.06, t = 4.34, p < 0.001). Individuals with lower dispositional resilience had 0.49 units increase in internalized HIV stigma for every unit increase in perceived HIV stigma in the community; whereas individuals with higher dispositional resilience only had 0.24 units increase in internalized HIV stigma for one unit increase in perceived HIV stigma in the community.
Figure 4.
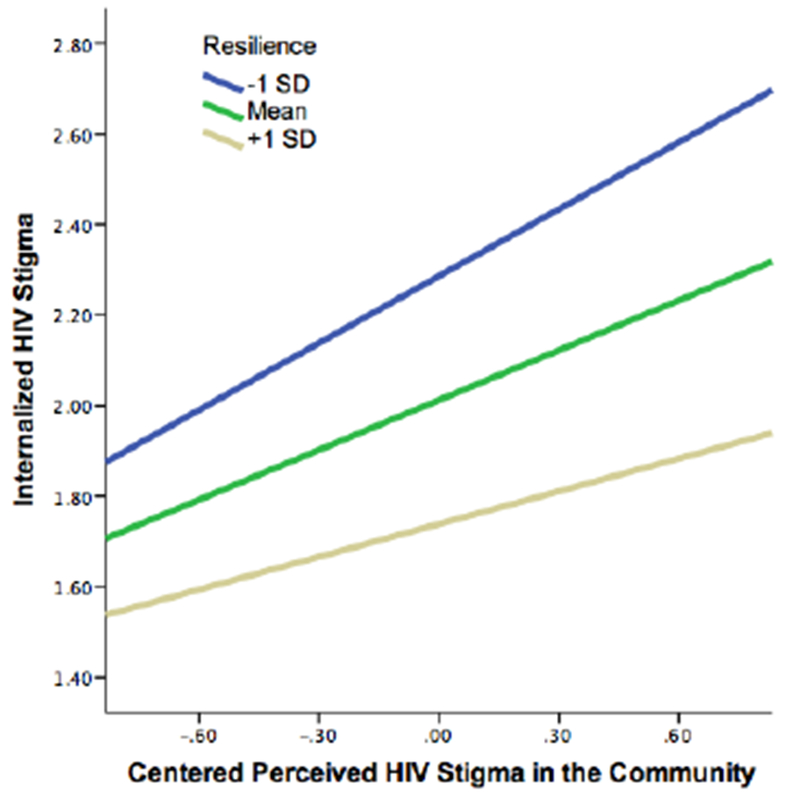
Interaction of resilience with perceived HIV stigma in the community (centered) on internalized HIV stigma in Study 2.
Then we explored the moderated mediation hypothesis using three study moderators (fear of negative evaluation, attachment-related anxiety, and resilience) for the indirect effect of perceived HIV stigma in the community on depressive symptoms through internalized stigma.h The index of moderated mediation was significant for fear of negative evaluation (index = 1.34, SE = 0.42, 95% CI = 0.55, 2.17). Moderated mediation was also significant for attachment-related anxiety (index = 0.52, SE = 0.22, 95% CI = 0.13, 0.98). Dispositional resilience also moderated the indirect effect of perceived HIV stigma in the community on depressive symptoms (index = −1.21, SE = 0.37, 95% CI = −2.01, −0.52).
Moderated mediation was also supported for all three moderators when ART adherence was the outcome: fear of negative evaluation (index = −0.08, SE = 0.05, 95% CI = −0.20, −0.0004); attachment-related anxiety (index = −0.03, SE = 0.02, 95% CI = −0.09, −0.002) and resilience (index = 0.07, SE = 0.05, 95% CI = 0.00, 0.19).i
DISCUSSION
It is essential to understand how stigma is internalized and what variables provide partial protection against internalization so that effective interventions can be developed to challenge stigma and mitigate its effects on health outcomes for PLWH. Results were strikingly similar in two separate samples: fear of negative evaluation and attachment-related anxiety appeared to exacerbate the transformation of perceived HIV stigma in the community to internalized HIV stigma. In other words, fear of negative evaluation and attachment-related anxiety are intrapersonal variables that make people more vulnerable to the internalization of social stigma. On the other hand, dispositional resilience appeared to be protective against the internalization of HIV stigma perceived in the community. These interaction effects may also have downstream consequences for depressive symptoms and ART adherence.
The results should be interpreted in light of limitations. These results represent cross-sectional data and thus we cannot make definitive conclusions about causality. Previous research has evaluated the associations between internalized HIV stigma and poor health outcomes over time,9,43,44 but the moderation analyses presented here will need further exploration in longitudinal research. Both samples were recruited from HIV care clinics and largely included individuals who were engaged in care. Thus, these results may not generalize to PLWH not in care. In Study 1, we did not find any significant associations with ART adherence, though this was likely attributable to the smaller sample of Study 1 compared to Study 2.
Despite these limitations, this study reveals individual differences that moderate the association between perceived HIV stigma in the community and internalized HIV stigma. While these findings focus on individual variables, we must also underscore that these intrapersonal variables interacted with interpersonal sources of stigma. Consequently, interpersonal and structural interventions are also needed to enact change at the community and system levels to reduce HIV stigma in the community that may in turn reduce internalized stigma. Interventions involving churches and faith-based organizations that provide education and positive messages about HIV have shown some success in reducing stigma and increasing HIV testing behavior.45 Similarly, training popular opinion leaders in community settings can reduce HIV stigma through modeling behavior and attitudes to change social norms.46 Another intervention that brings together PLWH and healthcare workers in a workshop setting to address HIV stigma showed feasibility and acceptability.47 However, community-level interventions can take time to enact change.48 Existing individual-level interventions targeting internalized stigma and/or HIV outcomes may need to be tailored to the level of fear of negative evaluation, attachment-related anxiety, and resilience of individual PLWH. Interventions can also include targeted cognitive strategies (and its contemporaries, such as acceptance and commitment therapy), in which thoughts related to societal stigma are challenged, so that they do not activate internalized stigma, but rather trigger resilience beliefs.49–52
Furthermore, existing interventions targeting fear of negative evaluation—such as cognitive-behavioral treatments commonly used for social anxiety disorder and social phobia that include exposure methods—can be delivered in group format or individually.53 Similarly, strategies have been developed in psychology and social work to help people understand and change their generalized attachment models through increasing awareness and challenging dysfunctional beliefs (e.g., “I am not able to deal with life on my own”), identifying maladaptive interpersonal patterns, and challenging maladaptive hyperactivating and deactivating strategies when facing challenges. These can be delivered in group settings54,55 or individually.56 In addition, there is evidence that other (not attachment focused) counseling approaches can also improve interpersonal relationship security.56–59 Interventions targeting resilience also exist that are based on principles of cognitive-behavioral therapy, acceptance and commitment therapy, mindfulness, problem-solving therapy, and stress inoculation.60–62 These interventions could enhance the well-being of PLWH and have downstream effects on reducing internalized HIV stigma, decreasing depression, and improving ART adherence, care engagement, and health outcomes for PLWH.
Supplementary Material
ACKNOWLEDGEMENTS
We wish to acknowledge the assistance of the WIHS program staff and the contributions of the participants who enrolled in this study. This study was funded by Women’s Interagency HIV Study (WIHS) sub-study grants from the National Institute of Mental Health, R01MH104114 and R01MH095683. The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH). WIHS (Principal Investigators): UAB-MS WIHS (Mirjam-Colette Kempf and Deborah Konkle-Parker), U01-AI-103401; Atlanta WIHS (Ighovwerha Ofotokun and Gina Wingood), U01-AI-103408; Bronx WIHS (Kathryn Anastos and Anjali Sharma), U01-AI-035004; Brooklyn WIHS (Howard Minkoff and Deborah Gustafson), U01-AI-031834; Chicago WIHS (Mardge Cohen and Audrey French), U01-AI-034993; Metropolitan Washington WIHS (Seble Kassaye), U01-AI-034994; Miami WIHS (Margaret Fischl and Lisa Metsch), U01-AI-103397; UNC WIHS (Adaora Adimora), U01-AI-103390; Connie Wofsy Women’s HIV Study, Northern California (Ruth Greenblatt, Bradley Aouizerat, and Phyllis Tien), U01-AI-034989; WIHS Data Management and Analysis Center (Stephen Gange and Elizabeth Golub), U01-AI-042590; Southern California WIHS (Joel Milam), U01-HD-032632 (WIHS I – WIHS IV). The WIHS is funded primarily by the National Institute of Allergy and Infectious Diseases (NIAID), with additional co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Cancer Institute (NCI), the National Institute on Drug Abuse (NIDA), and the National Institute on Mental Health (NIMH). Targeted supplemental funding for specific projects is also provided by the National Institute of Dental and Craniofacial Research (NIDCR), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the National Institute on Deafness and other Communication Disorders (NIDCD), and the NIH Office of Research on Women’s Health. WIHS data collection is also supported by UL1-TR000004 (UCSF CTSA), UL1-TR000454 (Atlanta CTSA), and P30-AI-050410 (UNC CFAR). This research was also supported by the University of Alabama at Birmingham (UAB) Center for AIDS Research CFAR, an NIH funded program (P30 AI027767) that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR. Trainee support was provided by the Agency for Healthcare Research and Quality (AHRQ 2T32HS013852-16).
Footnotes
The authors declare no conflicts of interest.
Full regression results reported in Supplemental Table 1.
Full regression results reported in Supplemental Table 2.
Moderated mediation indices and conditional indirect effects are presented in Supplemental Table 4.
Moderated mediation indices and conditional indirect effects are presented in Supplemental Table 5.
Full regression results reported in Supplemental Table 1.
Full regression results reported in Supplemental Table 2.
Full regression results reported in Supplemental Table 3.
Description of moderated mediation indices and conditional indirect effects are presented in Supplemental Table 4.
Description of moderated mediation indices and conditional indirect effects are presented in Supplemental Table 5.
References
- 1.Turan B, Budhwani H, Fazeli PL, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. 2017;21:283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing Mechanisms Linking HIV-Related Stigma, Adherence to Treatment, and Health Outcomes. Am J Public Health. 2017;107(6):863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS and behavior. 2013;17(5):1785–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Logie C, Gadalla T. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS care. 2009;21(6):742–753. [DOI] [PubMed] [Google Scholar]
- 5.Turan B, Smith W, Cohen MH, et al. Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: the mediating roles of social isolation and depression. Journal of acquired immune deficiency syndromes (1999). 2016;72(2):198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS and behavior. 2006;10(5):473–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. Journal of general internal medicine. 2009;24(10):1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social science & medicine. 2007;64(9):1823–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fazeli PL, Turan JM, Budhwani H, et al. Moment-to-moment within-person associations between acts of discrimination and internalized stigma in people living with HIV: An experience sampling study. Stigma and health. 2017;2(3):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore KE, Tangney JP, Stuewig JB. The self-stigma process in criminal offenders. Stigma and health. 2016;1(3):206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Corrigan PW, Watson AC, Barr L. The self–stigma of mental illness: Implications for self–esteem and self–efficacy. J Soc Clin Psychol. 2006;25(8):875–884. [Google Scholar]
- 12.Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: An empirical assessment. Am Sociol Rev 1989:400–423. [Google Scholar]
- 13.Wieser MJ, Pauli P, Weyers P, Alpers GW, Mühlberger A. Fear of negative evaluation and the hypervigilance-avoidance hypothesis: an eye-tracking study. J Neural Transm. 2009;116(6):717–723. [DOI] [PubMed] [Google Scholar]
- 14.Richman LS, Lattanner MR. Self-regulatory processes underlying structural stigma and health. Social science & medicine. 2014;103:94–100. [DOI] [PubMed] [Google Scholar]
- 15.Goffman E Stigma; notes on the management of spoiled identity. Englewood Cliffs, N.J.: Prentice-Hall; 1963. [Google Scholar]
- 16.Liss M, Schiffrin HH, Rizzo KM. Maternal guilt and shame: The role of self-discrepancy and fear of negative evaluation. Journal of Child and Family Studies. 2013;22(8):1112–1119. [Google Scholar]
- 17.Mikulincer M, Shaver PR. Attachment in adulthood: Structure, dynamics, and change. New York: Guilford; 2007. [Google Scholar]
- 18.Bowlby J Attachment and Loss Vol 1 (1969). Attachment and loss. 1980;3. [Google Scholar]
- 19.Turan B, Crockett KB, Kempf M- C, et al. Internal Working Models of Attachment Relationships and HIV Outcomes among Women Living with HIV. JAIDS Journal of Acquired Immune Deficiency Syndromes. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mikulincer M, Florian V. The relationship between adult attachment styles and emotional and cognitive reactions to stressful events In: Simpson JA, Rholes WS, eds. Attachment Theory and Close Relationships. New York, NY: The Guilford Press; 1998. [Google Scholar]
- 21.Brennan KA, Shaver PR. Dimensions of adult attachment, affect regulation, and romantic relationship functioning. Personality and Social Psychology Bulletin. 1995;21(3):267–283. [Google Scholar]
- 22.Guo J, Turan B. Preferences for Social Support During Social Evaluation in Men: The Role of Worry About a Relationship Partner’s Negative Evaluation. The Journal of social psychology. 2016;156(1):122–129. [DOI] [PubMed] [Google Scholar]
- 23.Andersson P, Perris C. Attachment styles and dysfunctional assumptions in adults. Clin Psychol Psychother. 2000;7(1):47–53. [Google Scholar]
- 24.Park LE, Crocker J, Mickelson KD. Attachment styles and contingencies of self-worth. Personality and Social Psychology Bulletin. 2004;30(10):1243–1254. [DOI] [PubMed] [Google Scholar]
- 25.Srivastava S, Beer JS. How self-evaluations relate to being liked by others: Integrating sociometer and attachment perspectives. J Pers Soc Psychol. 2005;89(6):966. [DOI] [PubMed] [Google Scholar]
- 26.Homan KJ, Wild S, Dillon KR, Shimrock R. “Don’t bring me down” Effects of priming secure and anxious attachment on body image. Journal of Social and Personal Relationships. 2017:0265407517701298. [Google Scholar]
- 27.Ungar M Resilience across cultures. The British Journal of Social Work. 2008;38(2):218–235. [Google Scholar]
- 28.Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol 2013;68(4):225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Earnshaw VA, Lang SM, Lippitt M, Jin H, Chaudoir SR. HIV stigma and physical health symptoms: do social support, adaptive coping, and/or identity centrality act as resilience resources? AIDS Behav. 2015;19(1):41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Logie C, James L, Tharao W, Loutfy M. Associations between HIV-related stigma, racial discrimination, gender discrimination, and depression among HIV-positive African, Caribbean, and Black women in Ontario, Canada. AIDS patient care and STDs. 2013;27(2):114–122. [DOI] [PubMed] [Google Scholar]
- 31.Jones AM, Buckingham JT. Self-esteem as a moderator of the effect of social comparison on women’s body image. J Soc Clin Psychol. 2005;24(8):1164. [Google Scholar]
- 32.Adimora AA, Ramirez C, Benning L, et al. Cohort Profile: The Women’s Interagency HIV Study (WIHS). Int J Epidemiol 2018;47(2):393–394i. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: A reexamination of the HIV Stigma Scale. AIDS Education & Prevention. 2007;19(3):198–208. [DOI] [PubMed] [Google Scholar]
- 34.Leary MR. A brief version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin. 1983;9(3):371–375. [Google Scholar]
- 35.Brennan KA, Clark CL, Shaver PR. Self-report measurement of adult attachment: An integrative overview In: Simpson JA, Rholes WS, eds. Attachment theory and close relationships. New York: Guilford Press; 1998:46–76. [Google Scholar]
- 36.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. International journal of behavioral medicine. 2008;15(3):194–200. [DOI] [PubMed] [Google Scholar]
- 37.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatric annals. 2002;32(9):509–515. [Google Scholar]
- 38.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- 39.Lu M, Safren SA, Skolnik PR, et al. Optimal recall period and response task for self-reported HIV medication adherence. AIDS and behavior. 2008;12(1):86–94. [DOI] [PubMed] [Google Scholar]
- 40.Feldman B, Fredericksen R, Crane P, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS Behav. 2013;17(1):307–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- 42.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rendina H, Millar B, Parsons J. The critical role of internalized HIV-related stigma in the daily negative affective experiences of HIV-positive gay and bisexual men. J Affect Disord. 2018(227):289–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Turan B, Rice WS, Crockett KB, et al. Longitudinal association between internalized HIV stigma and ART adherence for women living with HIV: The mediating role of depression. AIDS. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Derose KP, Griffin BA, Kanouse DE, et al. Effects of a pilot church-based intervention to reduce HIV stigma and promote HIV testing among African Americans and Latinos. AIDS and behavior. 2016;20(8):1692–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li L, Guan J, Liang L- J, Lin C, Wu Z. Popular opinion leader intervention for HIV stigma reduction in health care settings. AIDS Education and Prevention. 2013;25(4):327–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Batey DS, Whitfield S, Mulla M, et al. Adaptation and Implementation of an Intervention to Reduce HIV-Related Stigma Among Healthcare Workers in the United States: Piloting of the FRESH Workshop. AIDS Patient Care STDS. 2016;30(11):519–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV‐related stigma and discrimination from 2002 to 2013: how far have we come? Journal of the International AIDS Society. 2013;16:18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moitra E, Herbert JD, Forman EM. Acceptance-based behavior therapy to promote HIV medication adherence. AIDS Care. 2011;23(12):1660–1667. [DOI] [PubMed] [Google Scholar]
- 50.Forman EM, Herbert JD, Moitra E, Yeomans PD, Geller PA. A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behav Modif. 2007;31(6):772–799. [DOI] [PubMed] [Google Scholar]
- 51.Safren SA, Hendriksen ES, Mayer KH, Mimiaga MJ, Pickard R, Otto MW. Cognitive-behavioral therapy for HIV medication adherence and depression. Cognitive and Behavioral Practice. 2004;11(4):415–424. [Google Scholar]
- 52.Antoni MH, Cruess DG, Cruess S, et al. Cognitive–behavioral stress management intervention effects on anxiety, 24-hr urinary norepinephrine output, and T-cytotoxic/suppressor cells over time among symptomatic HIV-infected gay men. J Consult Clin Psychol. 2000;68(1):31. [DOI] [PubMed] [Google Scholar]
- 53.Dogaheh ER, Mohammadkhani P, Dolatshahi B. Comparison of group and individual cognitive-behavioral therapy in reducing fear of negative evaluation. Psychol Rep 2011;108(3):955–962. [DOI] [PubMed] [Google Scholar]
- 54.Page TF. Applications of Attachment Theory to Group Interventions: A Secure Base in Adulthood In: Adult Attachment in Clinical Social Work. New York, NY: Springer; 2011:173–191. [Google Scholar]
- 55.Marmarosh CL. Empirical research on attachment in group psychotherapy: Moving the field forward. Psychotherapy. 2014;51(1):88. [DOI] [PubMed] [Google Scholar]
- 56.Taylor P, Rietzschel J, Danquah A, Berry K. Changes in attachment representations during psychological therapy. Psychotherapy Research. 2015;25(2):222–238. [DOI] [PubMed] [Google Scholar]
- 57.Tasca G, Balfour L, Ritchie K, Bissada H. Change in attachment anxiety is associated with improved depression among women with binge eating disorder. Psychotherapy: Theory, Research, Practice, Training. 2007;44(4):423–433. [DOI] [PubMed] [Google Scholar]
- 58.Muller RT, Rosenkranz SE. Attachment and treatment response among adults in inpatient treatment for posttraumatic stress disorder. Psychotherapy: Theory, Research, Practice, Training. 2009;46(1):82. [DOI] [PubMed] [Google Scholar]
- 59.Kirchmann H, Steyer R, Mayer A, Joraschky P, Schreiber-Willnow K, Strauss B. Effects of adult inpatient group psychotherapy on attachment characteristics: An observational study comparing routine care to an untreated comparison group. Psychotherapy Research. 2012;22(1):95–114. [DOI] [PubMed] [Google Scholar]
- 60.Helmreich I, Kunzler A, Chmitorz A, et al. Psychological interventions for resilience enhancement in adults. Cochrane Database of Systematic Reviews. 2017(2). [Google Scholar]
- 61.Southwick SM, Pietrzak RH, White G. Interventions to enhance resilience and resilience-related constructs in adults In: Litz BT, Charney D, Friedman MJ, Southwick SM, eds. Resilience and Mental Health: Challenges Across the Lifespan. Cambridge: Cambridge University Press; 2011:289–306. [Google Scholar]
- 62.Leppin AL, Bora PR, Tilburt JC, et al. The efficacy of resiliency training programs: a systematic review and meta-analysis of randomized trials. PLoS One. 2014;9(10):e111420. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


