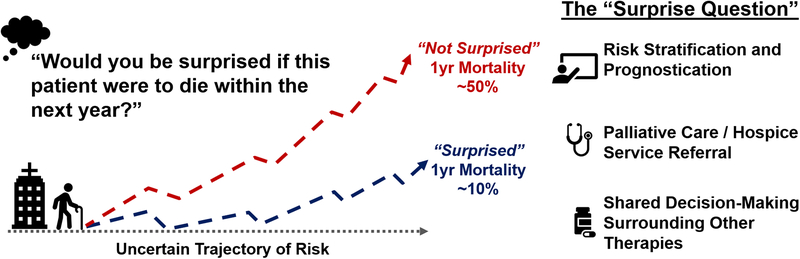
Historically, the cornerstones of therapy for heart failure (HF) have involved modification of disease progression and amelioration of symptoms with drugs and/or devices (1, 2). Specialized palliative care is specifically pertinent to the advanced HF population, a cohort with poor prognosis and high symptom burden. Despite the growing advanced HF population globally, palliative care utilization is both infrequent and delayed (3). Indeed, only 5% of elderly patients discharged after HF hospitalization receive specialized palliative care via hospice, and 34% of these patients die within 72 hours of arrival to a hospice facility (4). In contrast, 53% of advanced HF patients discharged without hospice died within 1 year, representing a vulnerable group that may have benefited from specialized palliative care (4). Variable disease trajectory in advanced HF introduces difficulty in accurate prognostication, which may partially explain the underutilization of palliative care in this at-risk cohort (5). The Surprise Question (Would you be surprised if this patient were to die within the next year?) is a simple query employed in other chronic illnesses, can be proposed to a wide spectrum of clinicians, and may provide insight into prognosis of HF patients, thereby identifying those who may benefit from specialized palliative care referral.
The Surprise Question: Simple to Answer, Simple to Interpret?
In this issue, Straw et al. aimed to determine 1) the prognostic value of the Surprise Question among 129 consecutive patients hospitalized with acute HF and 2) the agreement in the responses to the Surprise Question between various healthcare professionals (6). After accounting for several clinical covariates, a response of “Not Surprised” to the Surprise Question by cardiologists was significantly associated with 1-year all-cause mortality. While the Surprise Question exhibited adequate sensitivity (85%) and negative predictive value (88%) by cardiologists, it tended to overclassify patients who did not ultimately experience death at 1 year (specificity 59%). Additionally, the authors discovered that there was modest agreement in responses among cardiologists, HF nurses, and residents/fellows, but weaker agreement among these groups and non-HF nurses. It should be noted that 34% of patients died at 1 year despite only 10% of the study population having New York Heart Association IV symptoms and no patients receiving intensive care unit-level care or inotropes; this 1-year mortality rate is substantially higher than in trial populations, but comparable to that of the Medicare population (7, 8).
The application of the Surprise Question to the advanced HF population has been previously examined, exhibiting a test characteristic profile similar to that observed in the current study. In cancer, the question predicts 1-year survival more accurately as compared with those with non-cancer related illnesses (9). Among the HF population, previous studies have also demonstrated that “Not Surprised” responses tend to over-classify patients who ultimately do not experience death at 1 year (10), supporting the overall variability in the natural progression of this disease, highlighted by periods of stability, interrupted by acute periods of decompensation, and punctuated by sudden events. Overestimation of mortality in HF contrasts with the performance of the Surprise Question in cancer, which tended to underestimate mortality (11). Despite the limitations of the Surprise Question, it is reassuring that this study noted modest agreement across several types of healthcare professionals. Furthermore, specificity of estimates increased with concordance across clinician type, emphasizing the role of team-based care and decision-making in this population.
Identifying High-Risk Advanced Heart Failure Patients
In order to initiate important conversations regarding end of life care, patients with advanced HF at highest near-term risk of disease progression, death, or adverse quality of life need to be identified. Such patients may be recognized through objective risk scores, incorporating clinical demographics, laboratory variables, imaging data, and hospitalization history (e.g., Meta-Analysis Global Group in Chronic Heart Failure [MAGGIC] risk score and Seattle Heart Failure Model). Indeed, the recent Palliative Care in Heart Failure (PAL-HF) trial utilized the Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness (ESCAPE) discharge score, a 10-item model incorporating age, laboratory values, medication use, and in-hospital complications, as part of the inclusion criteria for the trial (12). Among patients recently discharged for acute HF with an ESCAPE score of ≥4 (corresponding to a 1-year mortality of >50%), palliative care interventions improved quality of life and anxiety/depression compared with usual care (12). Thus, objective risk scores such as ESCAPE can reliably and objectively identify an enriched advanced HF cohort who benefit from specialized palliative care. Challenges do exist in applying such risk scores toward real-world advanced HF populations, as many objective scores are cumbersome to complete due to the requirement of multiple data elements, and thus routine calculation may not be feasible during a busy outpatient clinic. These barriers may be navigated in the future through automated methods of score calculation using artificial intelligence and electronic health record (EHR) data. More importantly, it is unclear if providing objective data regarding risk of death influences physician communication regarding end of life care, as intensive care unit physicians who received 6-month survival estimates of their patients exhibited no improvement in patient-physician communication (13). Finally, as mode of death within certain HF types is quite heterogeneous (14), communication of these differential risks may be challenging. However, given the overall declining risk of sudden death in HF, predicting prognosis in these patients may become more reliable using risk scores (15).
While the Surprise Question carries inherent limitations in prognostic estimates, it possesses certain unique advantages. First, the simplicity of the question allows for integration into a typical advanced HF clinic visit. Additionally, the question forces clinicians to think quickly but also critically regarding their patients through a lens that may not always be appreciated during a standard visit. As a result, the striking nature of the Surprise Question may prompt clinicians to discuss end of life care, hospice, and palliative services that a numerical risk model may not achieve. The simplicity of the question and its answer also lends to a straightforward discussion with the patient, who may struggle to grasp complex probabilities associated with risk scores. Given the modest agreement in this study among several types of healthcare professionals, there are greater opportunities to pose this question at multiple points of patient contact to ultimately prompt palliative care consideration. The weak agreement between non-HF nurses and other healthcare professionals may be explained by the cognitive incorporation of certain clinical variables used in traditional risk scores by HF specialists into their answers. Targeted education of the prognostic ability of such clinical variables to non-HF nurses may improve agreement across all healthcare professionals.
Further research is required to determine if the cohort that screens “Not Surprised” do in fact experience quality of life improvement with palliative care interventions. Due to its low specificity, there is a possibility that the question identifies a group of patients who are not sick enough to benefit from specialized palliative care. Such a possibility raises some concern given the high resource utilization required for palliative interventions. On the other hand, it is plausible that a number of patients who were excluded from PAL-HF due to ESCAPE score < 4, who are likely identified by the Surprise Question, may in fact benefit from targeted palliative therapies.
Palliative Care Referral Pathways in Heart Failure
The incorporation of strategies to identify high-risk HF patients into everyday clinical practice is an important first step in improving global care of this population (Figure). The integration of the Surprise Question as a referral pathway for hospice care services through the EHR or mobile health applications would allow for the administration of the question at various levels of care (inpatient services, outpatient clinics) and by multiple clinicians (trainees, attending physicians, advance practice providers, nurses). However, identification of a high-risk HF cohort is only the first step in providing necessary and appropriate care. HF physician-initiated conversations regarding overall risk, palliative options, and patient wishes are required to improve access to palliative services. Furthermore, similar to paradigms pioneered in cancer medicine, the addition of specialized palliative care teams to standard HF care teams may allow for increased access to resources and enhanced utilization of such services.
Figure.
Integration of the “Surprise Question” in the Care of Patients with Advanced Heart Failure.
While there remain gaps in the palliative treatment of the advanced HF population, there has been steady progress. A simple but critical approach toward identifying those at highest risk may allow for increased utilization of specialized resources to improve quality of life of this complex patient population.
Footnotes
Disclosures:
Dr. Ravi Patel is supported by the NHLBI T32 postdoctoral training grant (T32HL069771).
Dr. Haider J. Warraich reports no disclosures related to this work.
Dr. Javed Butler has received research support from the NIH and European Union; and has been a consultant for Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, CVRx, Janssen, Luitpold Pharmaceuticals, Medtronic, Merck, Novartis, Relypsa, Vifor Pharma, and ZS Pharma.
Dr. Muthiah Vaduganathan is supported by the KL2/Catalyst Medical Research Investigator Training award from Harvard Catalyst | The Harvard Clinical and Translational Science Center (NIH/NCATS UL 1TR002541), and serves on advisory boards for AstraZeneca, Bayer AG, and Baxter Healthcare.
References:
- 1.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18(8):891–975. [DOI] [PubMed] [Google Scholar]
- 2.Braun LT, Grady KL, Kutner JS, Adler E, Berlinger N, Boss R, Butler J, Enguidanos S, Friebert S, Gardner TJ, Higgins P, Holloway R, Konig M, Meier D, Morrissey MB, Quest TE, Wiegand DL, Coombs-Lee B, Fitchett G, Gupta C, Roach WH Jr. Palliative Care and Cardiovascular Disease and Stroke: A Policy Statement From the American Heart Association/American Stroke Association. Circulation. 2016;134(11):e198–225. [DOI] [PubMed] [Google Scholar]
- 3.Butler J, Binney Z, Kalogeropoulos A, Owen M, Clevenger C, Gunter D, Georgiopoulou V, Quest T. Advance directives among hospitalized patients with heart failure. JACC Heart Fail. 2015;3(2):112–121. [DOI] [PubMed] [Google Scholar]
- 4.Warraich HJ, Xu H, DeVore AD, Matsouaka R, Heidenreich PA, Bhatt DL, Hernandez AF, Yancy CW, Fonarow GC, Allen LA. Trends in Hospice Discharge and Relative Outcomes Among Medicare Patients in the Get With The Guidelines-Heart Failure Registry. JAMA Cardiol. 2018;3(10):917–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warraich HJ, Allen LA, Mukamal KJ, Ship A, Kociol RD. Accuracy of physician prognosis in heart failure and lung cancer: Comparison between physician estimates and model predicted survival. Palliat Med. 2016;30(7):684–689. [DOI] [PubMed] [Google Scholar]
- 6.Straw S, Byrom R, Gierula J, Paton MF, Koshy A, Cubbon R, Drozd M, Kearney M, Witte K. Predicting one-year mortality in heart failure using the ‘surprise question’: a prospective pilot study. Eur J Heart Fail. 2018. (in press). [DOI] [PubMed] [Google Scholar]
- 7.Konstam MA, Gheorghiade M, Burnett JC Jr., Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST Outcome Trial. JAMA. 2007;297(12):1319–1331. [DOI] [PubMed] [Google Scholar]
- 8.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011;306(15):1669–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Downar J, Goldman R, Pinto R, Englesakis M, Adhikari NK. The “surprise question” for predicting death in seriously ill patients: a systematic review and meta-analysis. CMAJ. 2017;189(13):E484–E493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haga K, Murray S, Reid J, Ness A, O’Donnell M, Yellowlees D, Denvir MA. Identifying community based chronic heart failure patients in the last year of life: a comparison of the Gold Standards Framework Prognostic Indicator Guide and the Seattle Heart Failure Model. Heart. 2012;98(7):579–583. [DOI] [PubMed] [Google Scholar]
- 11.Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ. 2000;320(7233):469–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rogers JG, Patel CB, Mentz RJ, Granger BB, Steinhauser KE, Fiuzat M, Adams PA, Speck A, Johnson KS, Krishnamoorthy A, Yang H, Anstrom KJ, Dodson GC, Taylor DH Jr., Kirchner JL, Mark DB, O’Connor CM, Tulsky JA. Palliative Care in Heart Failure: The PAL-HF Randomized, Controlled Clinical Trial. J Am Coll Cardiol. 2017;70(3):331–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA. 1995;274(20):1591–1598. [PubMed] [Google Scholar]
- 14.Vaduganathan M, Patel RB, Michel A, Shah SJ, Senni M, Gheorghiade M, Butler J. Mode of Death in Heart Failure With Preserved Ejection Fraction. J Am Coll Cardiol. 2017;69(5):556–569. [DOI] [PubMed] [Google Scholar]
- 15.Shen L, Jhund PS, Petrie MC, Claggett BL, Barlera S, Cleland JGF, Dargie HJ, Granger CB, Kjekshus J, Kober L, Latini R, Maggioni AP, Packer M, Pitt B, Solomon SD, Swedberg K, Tavazzi L, Wikstrand J, Zannad F, Zile MR, McMurray JJV. Declining Risk of Sudden Death in Heart Failure. N Engl J Med. 2017;377(1):41–51. [DOI] [PubMed] [Google Scholar]