Abstract
In this study, multilayer perceptron artificial neural networks are used to predict orthodontic treatment plans, including the determination of extraction-nonextraction, extraction patterns, and anchorage patterns. The neural network can output the feasibilities of several applicable treatment plans, offering orthodontists flexibility in making decisions. The neural network models show an accuracy of 94.0% for extraction-nonextraction prediction, with an area under the curve (AUC) of 0.982, a sensitivity of 94.6%, and a specificity of 93.8%. The accuracies of the extraction patterns and anchorage patterns are 84.2% and 92.8%, respectively. The most important features for prediction of the neural networks are “crowding, upper arch” “ANB” and “curve of Spee”. For handling discrete input features with missing data, the average value method has a better complement performance than the k-nearest neighbors (k-NN) method; for handling continuous features with missing data, k-NN performs better than the other methods most of the time. These results indicate that the proposed method based on artificial neural networks can provide good guidance for orthodontic treatment planning for less-experienced orthodontists.
Introduction
Malocclusion is a common disease that impairs occlusal function, increases the incidence of caries, causes psychological discomfort, endangers health and reduces the quality of life1–3. An epidemiologic survey in America showed that 57% to 59% of each racial group has at least some degree of orthodontic treatment need4. The Health Policy Institute of the American Dental Association reported that 33% of young adults avoid smiling due to the condition of their mouth and teeth, and 82% of adults believe that the good appearance of the mouth and teeth can help them advance in life5. To achieve satisfactory orthodontic treatment effects, treatment planning must be carefully performed before the treatment process begins6. Comprehensive and deliberate evaluation of many factors makes treatment planning a complex process without any objective patterns, and heavily depends on the subjective judgment of the orthodontists.
Researchers have attempted to make orthodontic treatment planning procedures more objective by using some prediction methods. Rule-based expert systems (RBESs) were used to help orthodontic students and inexperienced practitioners with problem-solving and decision-making7. RBESs use formulated rules to construct a decision tree but suffer from considerable knowledge lost in the rule determination. To overcome the limitations of RBESs, case-based expert systems (CBESs) have been developed. CBESs acquire new knowledge by analyzing and taking in new cases, thereby acquiring better indexing features7. The difficulty of using CBES lies in finding an exact case that matches the new case; thus, some new cases have to be properly modified to be identified. A software that combined RBES and CBES was proposed in Noroozi’s work8, and the application of fuzzy logic made it more practical. Takada9 and Yagi10 proposed a CBES that used a k-nearest neighbors (k-NN) algorithm to perform classification in tooth-extraction decisions. However, the k-NN algorithm is a type of instance-based learning that is sensitive to the local structure of data and requires an increasing number of calculations as the number of cases increases. The artificial neural network (ANN) has the advantage of excavating features from massive medical data11,12, and the past decade has witnessed the rapid development of this approach. It has also been applied to determine necessary tooth extraction13 and extraction patterns (specific teeth to be removed)14 in orthodontic treatment planning.
It is important to note that different orthodontists can have markedly different plans for a specific case15. Considerable variety can occur particularly in the decision of which teeth to extract16. In addition to outputting a recommended treatment plan, an ANN that can output the feasibilities of multiple extraction options will allow orthodontists greater flexibility. Additionally, anchorage (resistance to unwanted tooth movement) is another important factor that should be considered when making plans6. In extraction cases using maximum anchorage, the early use of appropriate means to reinforce anchorage must be taken into account in the beginning. Related data are not always available in the actual application environment of ANNs17–19. ANN models cannot predict missing data; and thus a case with incomplete data may not be predicted by the models20–22. Providing methods that can handle missing data may make the model more applicable. Statistical approaches, such as imputation with average value or normal value, and k-NN imputation method have been intensively studied22,23. However, the comparison of different methods have showed different results and there is not a unique solution that can obtain best results in each neural network18,21,24. In this study, the traditional statistical approaches (average value method, frequent value method, specific value method and median value method) and the k-NN method are used to evaluate which method may be the best for increasing the accuracy.
The ANN in this study can promptly output both a recommended plan and feasible probabilities of several alternative options. The plan covers the most crucial concerns of orthodontists for most cases, including the extraction-nonextraction decision, extraction patterns and anchorage patterns (whether to use maximum anchorage to retract anterior teeth). We further calculated the relative contribution of features in each network model with the partial derivatives (PaD) method25 and, for the first time, investigated the effect of several complementary methods on handling missing data in orthodontic treatment planning.
Results
Orthodontic treatment planning with ANNs
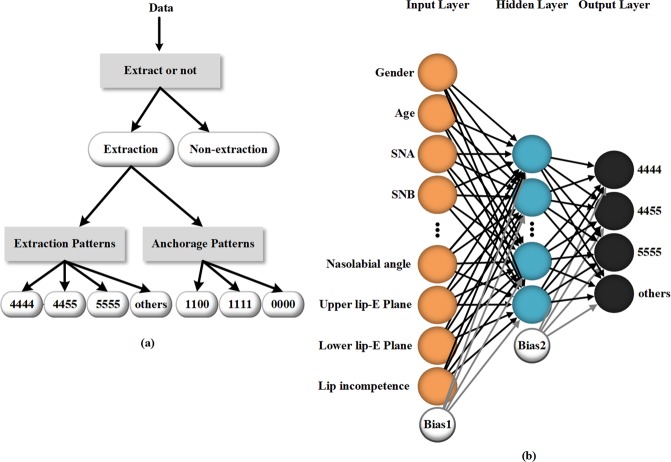
Three neural networks are trained with 302 cases from the Department of Orthodontics, West China Hospital of Stomatology. As shown in Fig. 1a, the first neural network determines whether a patient needs tooth extraction. If the patient needs extraction, the second and third neural networks then predict the specific extraction pattern and anchorage pattern, respectively. The network to determine extraction patterns, for example, is a three-layer fully connected multilayer perceptron (MLP), as shown in Fig. 1b, which consists of 24 input nodes, 10 hidden nodes, and 4 output nodes. The other two neural networks share the same model structure as this network but have different numbers of output nodes. The extraction-nonextraction neural network has 2 output nodes, and the anchorage patterns neural network has 3. The trained neural network models are provided in the Supplementary Information, together with the demonstration of the treatment planning process.
Figure 1.
(a) The data processing flow chart; (b) structure of the neural network to predict the extraction patterns. The network structure is a three-layer fully connected multilayer perceptron consisting of 24 input nodes, 10 hidden nodes, and 4 output nodes.
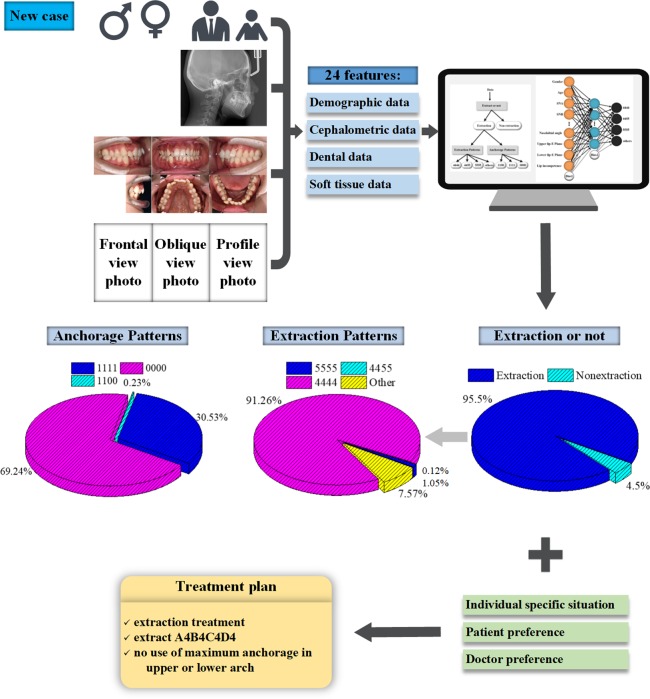
The accuracies of the ANNs
As illustrated in Fig. 2, the receiver operating characteristic (ROC) curve shows the performance of the ANN on the extraction decision. The model yields an area under the curve (AUC) of 0.982 (95% CI 0.968–0.995). The closer the point on the ROC curve is to the upper left corner, the higher the accuracy of the model, and the point closest to the upper left corner is the best cutoff value with the least error. The optimum diagnostic cutoff value of this model is 0.692, with which the model reaches a sensitivity of 94.6% (95% CI 0.894–0.964) and a specificity of 93.8% (95% CI 0.870–0.984). If the prediction probability of a case for extraction is greater than 0.692, it will be diagnosed as an extraction case and passed to the other two models to determine the extraction pattern and anchorage pattern. Figure 3 shows the predictive accuracies of the ANNs. The accuracy of the extraction-nonextraction decision-making is 94.0%, and the accuracies of the learning set, validation set, and test set are 94.0%, 95.0%, and 93.3%, respectively. The predictive accuracy of the extraction patterns is 83.3%, and the accuracies of the learning set, validation set, and test set are 83.6%, 84.1%, and 81.8%, respectively. The overall accuracy of the anchorage patterns is 92.8%, and the accuracies of the learning set, validation set, and test set are 93.3%, 90.9%, and 93.2%, respectively. The decision-making of the extraction patterns is the most complicated part of the treatment planning, and different doctors may use different extraction patterns16. This explains why its prediction accuracy is lower than the other two parts of the treatment planning, and this gap is comparable to the results of another study14. Considering the subjectivity of decision-making on extraction patterns, the model offers several practicable alternatives for doctors to choose, which makes it more applicable.
Figure 2.
The ROC curve of the neural network to predict extraction. The model yields an AUC of 0.982 (95% CI 0.968–0.995). The optimum diagnostic cutoff value is 0.692, where the sensitivity of the model reaches 94.6% (95% CI 0.894–0.964) and the specificity reaches 93.8% (95% CI 0.870–0.984).
Figure 3.
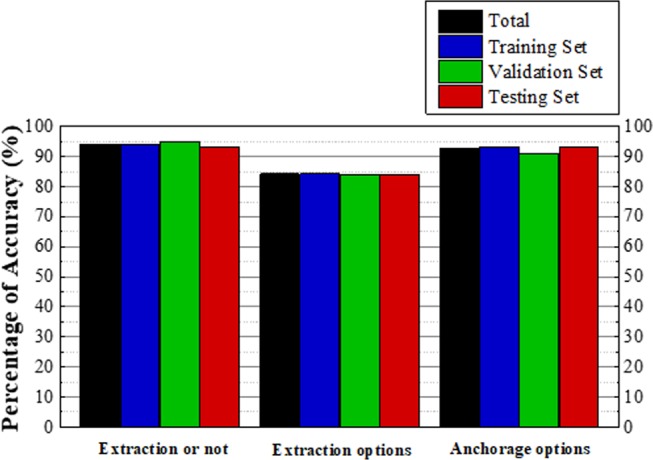
The accuracies of the ANNs. The accuracy of the extraction-nonextraction prediction is 94.0%, and the accuracies of the learning set, the validation set, and the test set are 94.0%, 95.0% and 93.3%, respectively. The predictive accuracy of the extraction patterns is 83.3%, and the accuracies of the learning set, validation set, and test set are 83.6%, 84.1%, and 81.8%, respectively. The overall accuracy of the anchorage patterns is 92.8%, and the accuracies of the learning set, validation set, and test set are 93.3%, 90.9%, and 93.2%, respectively.
Relative contribution of features for planning decisions
In clinical practice, doctors may not always have access to all the required data used by ANNs. Therefore, investigating the contribution of all features for each decision part will be of practical importance. We used the PaD method25 to calculate the features’ relative contributions and ranked them in order. The results are illustrated in Table 1. With respect to extraction decision-making, features “crowding, upper arch” “crowding, lower arch” and “U1-NA°” are the three that contributed most. “ANB” “overbite” and “lip incompetence” are the three features that are most related to the prediction of extraction patterns. The three most important features for anchorage pattern determination by the model are the “curve of Spee”, “nasolabial angle” and “UL-EP”. The results demonstrate that these features are selected or “thought” as important by the models when making decisions. When the models make different predictions, they treat different features as the most important.
Table 1.
Rank of the relative contribution of every feature.
| Rank | Extraction or Non-extraction | Extraction Patterns | Anchorage Patterns | |||
|---|---|---|---|---|---|---|
| Features | Contribution | Features | Contribution | Features | Contribution | |
| 1 | Crowding, Upper arch | 85711.28105 | ANB | 118465.2103 | Curve of Spee | 18547.57224 |
| 2 | Crowding, Lower arch | 57736.71377 | Overbite | 114032.7377 | Nasolabial angle | 15026.78087 |
| 3 | U1-NA° | 15012.78143 | Lip incompetence | 41415.55706 | UL-EP | 14657.07879 |
| 4 | UL-EP | 4954.977657 | U1-NA° | 18085.09864 | Overbite | 12976.87069 |
| 5 | LL-EP | 4177.450009 | Age | 17473.38386 | L1-NB° | 7938.055508 |
| 6 | L1-NB° | 3401.656971 | Curve of Spee | 17302.13528 | Profile | 7680.987385 |
| 7 | Lip incompetence | 3286.95674 | Crowding, Lower arch | 16905.04732 | FMIA | 7414.201627 |
| 8 | Overbite | 2942.413326 | Nasolabial angle | 13745.41489 | Age | 6187.604495 |
| 9 | Molar Relationship | 1417.233 | Overjet | 13667.56045 | LL-EP | 2391.518896 |
| 10 | Age | 589.4921089 | Molar Relationship | 8798.718 | ANB | 2347.936804 |
| 11 | S-Go/N-Me | 588.7796549 | U1-NA(mm) | 7288.337735 | S-Go/N-Me | 1974.048274 |
| 12 | Nasolabial angle | 555.4425076 | L1-NB(mm) | 6406.556758 | U1-NA° | 1720.918869 |
| 13 | Profile | 343.9300483 | UL-EP | 5119.782824 | Crowding, Lower arch | 1467.612 |
| 14 | Sex | 307.2066295 | FMIA | 4089.027359 | Lip incompetence | 903.411461 |
| 15 | U1-NA(mm) | 208.265139 | SNA | 4056.661967 | SNB | 684.2875872 |
| 16 | IMPA | 150.1288817 | Crowding, Upper arch | 2949.948301 | Sex | 336.7110245 |
| 17 | SNA | 100.592332 | FMA | 1812.552422 | U1-NA(mm) | 258.1374941 |
| 18 | FMIA | 67.34319702 | Profile | 1437.646045 | Molar Relationship | 236.3783781 |
| 19 | Overjet | 57.1657521 | SNB | 1270.734428 | IMPA | 151.8654525 |
| 20 | Curve of Spee | 34.93226494 | Sex | 983.4392023 | Crowding, Upper arch | 106.1314566 |
| 21 | SNB | 5.236208966 | IMPA | 786.2672013 | FMA | 91.21057528 |
| 22 | L1-NB(mm) | 4.394215177 | LL-EP | 262.3915409 | SNA | 82.06470102 |
| 23 | ANB | 3.231616444 | L1-NB° | 93.51224553 | L1-NB(mm) | 34.28285845 |
| 24 | FMA | 1.03176361 | S-Go/N-Me | 4.960991795 | Overjet | 16.99804082 |
Comparison of different complement methods
In the present study, we took a step further to investigate when the data of the most important features are missing, whether the impact of data loss on accuracies can be reduced or minimized by complement methods21,23,24,26. The complement effects are displayed in Table 2. The results show that the average value method has better performance than k-NN when dealing with discrete features regarding “lip incompetence” and “nasolabial angle”. The accuracies of the four traditional methods (average value, frequent value, specified value and median value methods) are consistent for processing the “nasolabial angle”. When dealing with continuous variables, k-NN performs better than the other methods, except for “crowding, lower arch”. With respect to the three features that the models “consider” to make the largest contribution to the treatment decisions, k-NN has the best complement performance. The effect of 2-k-NN is similar to that of 3-k-NN, in general.
Table 2.
Complement effects of different methods on important features with missing data.
| Complement methods | Average Value | Frequent Value | Specified Value | Median Value | 2-k-NN | 3-k-NN |
|---|---|---|---|---|---|---|
| Network | Extraction or Non-extraction (accuracy of complete data: 0.9404) | |||||
| Crowding, Upper arch | 0.8642 | 0.8113 | 0.8113 | 0.8742 | 0.8775 | 0.8841 |
| Crowding, Lower arch | 0.8974 | 0.8742 | 0.8709 | 0.8642 | 0.8808 | 0.8808 |
| U1-NA° | 0.9106 | 0.9073 | 0.8974 | 0.9007 | 0.9238 | 0.9172 |
| Network | Extraction Patterns (accuracy of complete data: 0.8333) | |||||
| ANB | 0.8198 | 0.8063 | 0.8198 | 0.8153 | 0.8268 | 0.8268 |
| Overbite | 0.8198 | 0.8153 | 0.8153 | 0.8108 | 0.8288 | 0.8243 |
| Lip incompetence | 0.8288 | 0.8243 | 0.8243 | 0.6982 | 0.8063 | 0.8018 |
| Network | Anchorage Patterns (accuracy of complete data: 0.9279) | |||||
| Curve of Spee | 0.8649 | 0.8694 | 0.8694 | 0.8649 | 0.8874 | 0.8829 |
| Nasolabial angle | 0.8784 | 0.8784 | 0.8784 | 0.8784 | 0.8468 | 0.8559 |
| UL-EP | 0.8739 | 0.8333 | 0.8739 | 0.8739 | 0.8694 | 0.8919 |
The highest complement accuracy for each feature is shown in bold.
Discussion
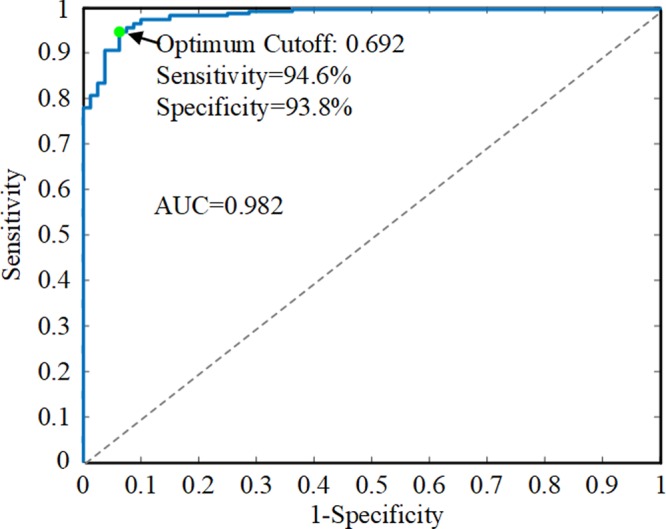
In this study, we propose an MLP-based classifier to analyze patients’ medical records and output both a recommended treatment plan and the feasibilities of various treatment plans regarding the aspects of extraction vs. nonextraction, extraction patterns and anchorage patterns. The feature importance is calculated and ranked, and we compared the effects of different complement methods. Since there can be several feasible treatment plans regarding a certain case, the output probabilities of extraction and anchorage patterns offer users considerable flexibility as well as guidance. The users can review the recommended plan, compare various treatment options, take other aspects into account, and finally, develop a standardized, accurate, and effective treatment plan. Figure 4 illustrates the clinical application process of the ANNs. An example patient was used for demonstration. Informed consent to publish the information and images in an online open-access publication was obtained, and the example patient’s medical data (patient A) can be found in the Supplementary Note 2.
Figure 4.
Clinical application illustration of the ANNs. The medical records of a new case were collected, and 24 input features, including demographic data, cephalometric data, dental data and soft tissue data, were extracted for neural network prediction. The extraction probability (0.955) was higher than 0.692; thus, it was determined as an extraction case and was passed to the other two networks. The other networks output the feasibilities of different extraction patterns and anchorage patterns. The doctor evaluated these treatment options, took other aspects into account, and finally determined an effective treatment plan.
Our neural network models have better performance compared with previous prediction methods. The predictive accuracy of extraction reached 94.0%, higher than the other prediction models13,27, and made a one percent improvement on the 93% accuracy of Jung’s study14. The AUC of 0.9815 is also higher than the result of 0.904 in a previous study based on the CBES and the k-NN algorithm9. For the most complex part of extraction pattern prediction, the model reached 84.2% accuracy, similar to the result of Jung’s model14, which is also based on a neural network. In addition, this study is the first to make a prediction of the use of maximum anchorage by an ANN, to the best of our knowledge. The accuracy was 92.8%, suggesting the potential of ANN in assisting orthodontists in making more detailed treatment plans.
We used the PaD method to study the contribution of features to the outcome and ranked them in order. Xie13 used the “weights” method in a previous study and investigated the connection strengths of each neuron in the input layer with each neuron in the hidden layer to represent the contribution of every input index. They used different input indexes and different methods to calculate the contribution, and they found that “anterior teeth uncovered by incompetent lips” and “IMPA” were the two indexes that presented the largest contributions to the extraction decision vs. nonextraction. The “weights” method allows for a good classification of the input features but lacks stability25. The PaD method presents more complete results and makes a more severe discrimination between minor and major contributing variables in comparison to the “weights”25,28.
It is also the first time to investigate the effect of complement methods in similar studies. Our results suggested that the average value method outperformed k-NN when dealing with discrete variables, but k-NN performed better for the continuous variable. Meanwhile, k-NN is also a better choice when the data of the most important feature for each output decision is missing. This research contributes to the handling of missing data and can make the model more applicable.
It takes a relatively long time for orthodontists to accumulate experience. Doctors with less experience often require consultation with experts. Since medical developments are uneven and severely affected by economic conditions, expert consultation is especially deficient in areas with poor medical conditions. The proposed ANN system can not only assist less-experienced orthodontists and students in learning but also help patients obtain a clear understanding of their treatment plans.
Methods
Cases Collection
A total of 302 patients who received orthodontic treatment at the Department of Orthodontics, West China Hospital of Stomatology in Chengdu, China, from 2014 to 2018 were included in this study. The inclusion criteria were fixed labial appliance patients with full permanent dentition (except for second or third molars) without functional appliance treatment or orthognathic surgery. Their medical records before orthodontic treatment were collected, including demographic information, extraoral photos, intraoral photos, pretreatment dental casts and lateral cephalometric measurements6,29. Twenty-four commonly used feature variables were extracted from these clinical records as input features. The input features were preprocessed to ensure that all of them were quantified before being used for model training. Nonquantitative data were converted into numerical values by the encoding method. Supplementary Table S3 shows the detailed features used in the ANNs and how the nonquantitative data were encoded. All treatment planning was carefully performed by Dr. Zhao and Dr. Tang, who are both orthodontic specialists and have 26 and 12 years of clinical work experience, respectively. This study was approved by the West China Hospital of Stomatology Institutional Review Board (WCHSIRB-D-2018-094). Informed consent was obtained from all participants or their legal guardians. Informed consent for publication of the medical records of four example patients in an online open-access publication was also obtained. All experiments were performed in accordance with relevant guidelines and regulations.
The composition of the cases and datasets
Among the total population, 222 persons were extraction cases, accounting for 73.5%, and the other 80 persons were nonextraction cases, accounting for 26.5%. The tooth extraction patterns were divided into four types: maxillary and mandibular first premolar extraction (4444), maxillary first premolar and mandibular second premolar extraction (4455), maxillary and mandibular second premolar extraction (5555) and other extraction patterns including only maxillary first premolar extraction, maxillary second premolar and mandibular first premolar extraction. These four patterns comprise 41.9%, 19.8%, 18.5% and 18.5% of the extraction cases, respectively. The anchorage patterns included three types, i.e., maxillary maximum anchorage (1100), maxillary and mandibular maximum anchorage (1111), and no use of maximum anchorage (0000), accounting for 29.7%, 21.6% and 48.6% of the extraction cases, respectively. Descriptions of the extraction patterns and anchorage patterns are shown in Table 3.
Table 3.
Descriptions of the extraction patterns and anchorage patterns.
| Pattern | Description | |
|---|---|---|
| Extraction Patterns | 4444 | maxillary and mandibular first premolar extraction |
| 4455 | maxillary first premolar and mandibular second premolar extraction | |
| 5555 | maxillary and mandibular second premolar extraction | |
| others | other extraction patterns including only maxillary first premolar extraction, maxillary second premolar and mandibular first premolar extraction | |
| Anchorage Patterns | 1100 | maxillary maximum anchorage |
| 1111 | maxillary and mandibular maximum anchorage | |
| 0000 | no use of maximum anchorage | |
The dataset is split into a training set, a validation set and a test set. The neural networks do not have access to the test set during the training process until the final evaluation of the accuracy. The reserve part of the dataset is split into a training set and a validation set with a ratio of 3/1, which is optimized according to the learning curve30. The training set is used to update the weights of the network. The validation set is used to avoid overfitting13. Considering that we had a smaller dataset, we used a greater percentage of data to test the models. Therefore, the training set, validation set and test set were set with a typical 60/20/20 split to maintain a balance between the sets. Cases with different tags were randomly distributed to the three datasets in each simulation so that the proportions of various cases are similar among the three sets, reducing the additional bias introduced by the data partitioning process. There are 222 extraction cases; thus, the 222 cases are used in the neural network models for predicting extraction patterns and anchorage patterns. The number and percentage of different kinds of treatment plans in each set are shown in Table 4.
Table 4.
Number and percentage of different kinds of treatment plans in each set.
| Sets | Extraction or Non-extraction | Extraction Patterns | Anchorage Patterns | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Extraction (73.5%) | Nonextraction (26.5%) | Total (100%) | 4444 (41.9%) | 4455 (19.8%) | 5555 (18.5%) | Others (18.5%) | Total (100%) | 1100 (29.7%) | 1111 (21.6%) | 0000 (48.6%) | Total (100%) | |
| Training (60%) | 134 | 48 | 182 | 57 | 26 | 25 | 26 | 134 | 40 | 28 | 66 | 134 |
| Validation (20%) | 44 | 16 | 60 | 18 | 9 | 8 | 9 | 44 | 13 | 10 | 21 | 44 |
| Test (20%) | 44 | 16 | 60 | 18 | 9 | 8 | 9 | 44 | 13 | 10 | 21 | 44 |
| Total (100%) | 222 | 80 | 302 | 93 | 44 | 41 | 44 | 222 | 66 | 48 | 108 | 222 |
Network models
All three neural networks used in this work are three-layer MLPs. Each MLP consists of three full connection layers. The MLP used to determine extraction patterns is illustrated in Fig. 1b. The activation function of the hidden layer is tanh. A softmax layer of 4 outputs is applied at the end of the model31,32. The cross-entropy33,34 CEtanh is given by
| 1 |
where t is the target value and y is the output of the MLP. Equation (1) returns a numerical value approaching infinity, which heavily penalizes output when y approaches −1 or 1. CEtanh approaches its minimum value when y approaches t. The weight and bias values are updated according to the scaled conjugate gradient method35. Although minimizing CEtanh leads to a good accuracy of classification, considerably minimizing CEtanh may cause overfitting. The dropout method is used to prevent overfitting36,37. The detailed training setting including learning rate, number of epochs, batch size, et al., are provided in Supplementary Note 4.
For the extraction prediction, the model outputs a probability of extraction. We define a determination of extraction treatment for each case as the probability of extraction being higher than a cutoff value. The algorithm computes sensitivity and specificity by testing a variety of cutoff values. Varying the cutoff point in the interval 0–1 generates a conventional ROC curve. Youden’s index38 is applied to obtain the optimum cutoff. If the probability is higher than the optimum cutoff, the case will be passed to the prediction of extraction patterns and anchorage patterns.
Relative contribution calculation of features and complement of the missing data
The PaD method, which is supposed to be the most useful method in giving the relative contribution and the contribution profile of the input factors, was used to evaluate the relative contribution calculation of the input features. The PaD method computes the partial derivatives of the ANN’s output with respect to the input to obtain the profile of the variations of the output for small changes of one input variable. For a network with ni inputs (where i represents the feature index and i = 1, 2, …, 24 in this work), one hidden tanh layer with nh neurons, and no outputs, the partial derivatives of the output yj with respect to input xj (where j represents the case index and j = 1, 2, …, 302 in this work) are:
| 2 |
where Sj is the derivative of the output neuron with respect to the input, which is the weights between the output neuron and hth hidden neuron, Ihj is the output of the hth hidden neuron, and wih is the weights between the ith input neuron and the hth hidden neuron.
Then, the relative contribution of the ANN’s output to the dataset with respect to the ith input feature can be calculated by a sum of the square partial derivatives as:
| 3 |
where N is the data size and equals 302 in this work. The SSD values enable direct access to the influence of each input variable on the output.
We use the average value method, frequent value method, specific value method, median value method, and k-NN method to study their complement effects. The four traditional methods complement the missing data with the average value, the frequent value, the specified value (standard value of normal population), and the median value. The k-NN method is a method to look for the new case’s nearest neighbors from the complete cases and use an estimated value to replace the missing data26,39. This value is the weighted average of the values of its k nearest neighbors. We used 2-k-NN (2 nearest neighbors) and 3-k-NN (3 nearest neighbors) in this study. Each neighbor is given a weight of 1/d, where d is the distance to the neighbor. The neighbors are taken from the dataset for which the object property value is known.
Supplementary information
Author Contributions
P.L., D.K., Z.Z. and Y.L. conceived and designed the experiments. Z.Z. and T.T. made the orthodontic treatment plans of the patients. P.L., D.S., P.Y. and H.W. collected the medical records. P.L., D.K. analyzed the data and wrote the main manuscript text. All authors reviewed the manuscript.
Data Availability
The present neural network models, medical data of example patients, features descriptions and training setting are provided in the Supplementary Information.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zhihe Zhao, Email: zhzhao@scu.edu.cn.
Yang Liu, Email: yliu1975@uestc.edu.cn.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-38439-w.
References
- 1.Krooks L, Pirttiniemi P, Kanavakis G, Lahdesmaki R. Prevalence of malocclusion traits and orthodontic treatment in a Finnish adult population. Acta odontologica Scandinavica. 2016;74:362–367. doi: 10.3109/00016357.2016.1151547. [DOI] [PubMed] [Google Scholar]
- 2.Feldens, C. A. et al. Impact of malocclusion and dentofacial anomalies on the prevalence and severity of dental caries among adolescents. The Angle orthodontist, 10.2319/100914.1 (2015). [DOI] [PMC free article] [PubMed]
- 3.Mary AV, et al. Assessing Quality of Life using the Oral Health Impact Profile (OHIP-14) in Subjects with and without Orthodontic Treatment need in Chennai, Tamil Nadu, India. Journal of clinical and diagnostic research: JCDR. 2017;11:Zc78–zc81. doi: 10.7860/jcdr/2017/27309.10442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Proffit WR, Fields HW, Jr., Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. The International journal of adult orthodontics and orthognathic surgery. 1998;13:97–106. [PubMed] [Google Scholar]
- 5.Association, A. D. Oral Health and Well-Being in the United States, https://www.ada.org/en/science-research/health-policy-institute/oral-health-and-well-being (2015).
- 6.Proffit, W. R., Fields, H. W. Jr. & Sarver, D. M. Contemporary orthodontics. 5th edn, (Mosby, 2013).
- 7.Hammond R, Freer TJ. Application of a case-based expert system to orthodontic diagnosis and treatment planning: a review of the literature. Australian orthodontic journal. 1996;14:150. [PubMed] [Google Scholar]
- 8.Noroozi H. Orthodontic treatment planning software. American journal of orthodontics and dentofacial orthopedics. 2006;129:834–837. doi: 10.1016/j.ajodo.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 9.Takada K, Yagi M, Horiguchi E. Computational formulation of orthodontic tooth-extraction decisions. Part I: to extract or not to extract. The Angle orthodontist. 2009;79:885–891. doi: 10.2319/081908-436.1. [DOI] [PubMed] [Google Scholar]
- 10.Yagi M, Ohno H, Takada K. Computational formulation of orthodontic tooth-extraction decisions. Part II: which tooth should be extracted? The Angle orthodontist. 2009;79:892–898. doi: 10.2319/081908-439.1. [DOI] [PubMed] [Google Scholar]
- 11.Worden K, Staszewski WJ, Hensman JJ. Natural computing for mechanical systems research: A tutorial overview. Mechanical Systems and Signal Processing. 2011;25:4–111. doi: 10.1016/j.ymssp.2010.07.013. [DOI] [Google Scholar]
- 12.Jia F, Lei Y, Lin J, Zhou X, Lu N. Deep neural networks: A promising tool for fault characteristic mining and intelligent diagnosis of rotating machinery with massive data. Mechanical Systems and Signal Processing. 2016;72:303–315. doi: 10.1016/j.ymssp.2015.10.025. [DOI] [Google Scholar]
- 13.Xie X, Wang L, Wang A. Artificial neural network modeling for deciding if extractions are necessary prior to orthodontic treatment. The Angle orthodontist. 2010;80:262–266. doi: 10.2319/111608-588.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jung SK, Kim TW. New approach for the diagnosis of extractions with neural network machine learning. American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 2016;149:127–133. doi: 10.1016/j.ajodo.2015.07.030. [DOI] [PubMed] [Google Scholar]
- 15.Lee R, Macfarlane T, O’Brien K. Consistency of orthodontic treatment planning decisions. Clinical Orthodontics & Research. 1999;2:79–84. doi: 10.1111/ocr.1999.2.2.79. [DOI] [PubMed] [Google Scholar]
- 16.Luke LS, Atchison KA, White SC. Consistency of patient classification in orthodontic diagnosis and treatment planning. Angle Orthodontist. 1998;68:513. doi: 10.1043/0003-3219(1998)068<0513:COPCIO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Sterne JA, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. British medical journal. 2009;339:157–160. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jerez JM, et al. Missing data imputation using statistical and machine learning methods in a real breast cancer problem. Artificial intelligence in medicine. 2010;50:105–115. doi: 10.1016/j.artmed.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 19.García-Laencina PJ, Abreu PH, Abreu MH, Afonoso N. Missing data imputation on the 5-year survival prediction of breast cancer patients with unknown discrete values. Computers in biology and medicine. 2015;59:125–133. doi: 10.1016/j.compbiomed.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 20.Aydilek IB, Arslan A. A novel hybrid approach to estimating missing values in databases using k-nearest neighbors and neural networks. International Journal of Innovative Computing, Information and Control. 2012;7:4705–4717. [Google Scholar]
- 21.Jayalakshmi, T. & Santhakumaran, A. In Data Storage and Data Engineering (DSDE), 2010 International Conference on. 159–163 (IEEE, 2010).
- 22.García-Laencina PJ, Sancho-Gómez J-L, Figueiras-Vidal AR. Pattern classification with missing data: a review. Neural Computing and Applications. 2010;19:263–282. doi: 10.1007/s00521-009-0295-6. [DOI] [Google Scholar]
- 23.Ennett CM, Frize M, Walker CR. Influence of missing values on artificial neural network performance. Stud Health Technol Inform. 2001;84:449–453. [PubMed] [Google Scholar]
- 24.Chen H, Grant-Muller S, Mussone L, Montgomery F. A study of hybrid neural network approaches and the effects of missing data on traffic forecasting. Neural Computing & Applications. 2001;10:277–286. doi: 10.1007/s521-001-8054-3. [DOI] [Google Scholar]
- 25.Gevrey M, Dimopoulos I, Lek S. Review and comparison of methods to study the contribution of variables in artificial neural network models. Ecological modelling. 2003;160:249–264. doi: 10.1016/S0304-3800(02)00257-0. [DOI] [Google Scholar]
- 26.Batista GE, Monard MC. A Study of K-Nearest Neighbour as an Imputation Method. HIS. 2002;87:251–260. [Google Scholar]
- 27.Martina, R., Teti, R., D’Addona, D. & Iodice, G. Neural network based system for decision making support in orthodontic extractions. Intelligent Production Machines and Systems, 235–240 (2006).
- 28.Dedecker AP, et al. Application of artificial neural network models to analyse the relationships between Gammarus pulex L. (Crustacea, Amphipoda) and river characteristics. Environmental monitoring and assessment. 2005;111:223–241. doi: 10.1007/s10661-005-8221-6. [DOI] [PubMed] [Google Scholar]
- 29.Graber, L. W., Vanarsdall, R. L., Vig, K. W. & Huang, G. J. Orthodontics: Current Principles and Techniques. (Elsevier Health Sciences, 2016).
- 30.Guyon, I. A scaling law for the validation-set training-set size ratio. AT&T Bell Laboratories, 1–11 (1997).
- 31.Mavani, V., Raman, S. & Miyapuram, K. P. In Computer Vision Workshop (ICCVW), 2017 IEEE International Conference on. 2783–2788 (IEEE).
- 32.Yang, J. B., Nguyen, M. N., San, P. P., Li, X. L. & Krishnaswamy, S. In 2015 International Conference onArtificial Intelligence (Ijcai). 3995–4001.
- 33.Kshirsagar A, Seftel A, Ross L, Mohamed M, Niederberger C. Predicting hypogonadism in men based upon age, presence of erectile dysfunction, and depression. International journal of impotence research. 2006;18:47. doi: 10.1038/sj.ijir.3901369. [DOI] [PubMed] [Google Scholar]
- 34.Boixo S, et al. Characterizing quantum supremacy in near-term devices. Nature Physics. 2018;14:595. doi: 10.1038/s41567-018-0124-x. [DOI] [Google Scholar]
- 35.Møller MF. A scaled conjugate gradient algorithm for fast supervised learning. Neural networks. 1993;6:525–533. doi: 10.1016/S0893-6080(05)80056-5. [DOI] [Google Scholar]
- 36.Srivastava N, Hinton G, Krizhevsky A, Sutskever I, Salakhutdinov R. Dropout: a simple way to prevent neural networks from overfitting. The Journal of Machine Learning Research. 2014;15:1929–1958. [Google Scholar]
- 37.Hinton, G. E., Srivastava, N., Krizhevsky, A., Sutskever, I. & Salakhutdinov, R. R. Improving neural networks by preventing co-adaptation of feature detectors. arXiv preprint arXiv:1207.0580 (2012).
- 38.Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–35. doi: 10.1002/1097-0142(1950)3:1<32::AID-CNCR2820030106>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 39.Altman NS. An introduction to kernel and nearest-neighbor nonparametric regression. The American Statistician. 1992;46:175–185. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The present neural network models, medical data of example patients, features descriptions and training setting are provided in the Supplementary Information.