Highlights
-
•
Massive mediastinal emphysema is rare signs of colon perforation.
-
•
The diagnosis may be delayed due to the absence of peritoneal irritation.
-
•
Laparotomy should be considered in case of colonic penetration with the mediastinum emphysema.
Keywords: Mediastinal emphysema, Pneumomediastinum, Retroperitoneal emphysema, Subcutaneous emphysema, Colonic perforation, Diverticulitis
Abstract
Introduction
Mediastinal and subcutaneous emphysema usually result from spontaneous rupture of the alveolar wall. We present an extremely rare case of massive mediastinal, retroperitoneal, and subcutaneous emphysema due to the penetration of the colon into the mesentery.
Presentation of case
A 57-year-old man presented to our institution with a history of chest pain. The patient’s medical history included malignant rheumatoid arthritis during the use of steroids and an immunosuppressive agent. The patient had no signs of peritoneal irritation or abdominal pain. A chest radiography revealed subcutaneous emphysema of the neck, mediastinal emphysema, as well as subdiaphragmatic free air. Computed tomography showed extensive retroperitoneal, mediastinal, and mesenteric emphysema of the sigmoid colon without pneumothorax. Diagnostic laparoscopy was performed and revealed perforation into the sigmoid mesentery. Segmental resection of the sigmoid colon and end-colostomy were performed. The diverticulum was communicating with the outside of the mesentery via the mesentery. The mediastinal emphysema disappeared a few days after the surgery.
Discussion
Colonic perforation generally results in free perforation. Colonic gas may spread via various anatomical pathways when perforation of the colon occurs in the retroperitoneum; thus, diverse atypical clinical symptoms may be present. Signs of peritoneal irritation can be hidden in cases of retroperitoneal colonic perforation. The atypical manifestation of a retroperitoneal colonic perforation can cause difficulties in making a diagnosis.
Conclusions
Massive mediastinal and retroperitoneum emphysema are rare signs of colonic perforation. Emergency laparotomy should be considered in colonic penetration of the diverticulitis where the emphysema expands to the mediastinum extensively.
1. Introduction
Mediastinal and subcutaneous emphysema usually result from spontaneous rupture of the alveolar wall [1]. These symptoms, following colonic perforation, are unusual, and massive mediastinal emphysema is extremely rare without a preceding endoscopic procedure [[2], [3], [4], [5]]. Most symptoms of colonic perforation are due to abscesses or peritonitis [6]. However, it is difficult to diagnose retroperitoneal penetration of the colon and rectum because of the lack of typical symptoms [7,8]. Furthermore, delayed diagnosis and treatment could result in high morbidity and mortality [6]. We present a rare case of colonic penetration with massive retroperitoneal, mediastinal, and subcutaneous emphysema. This report has been made according to the SCARE criteria [9].
2. Presentation of case
A 57-year-old man presented to our institution with a history of chest pain of a few days. The patient’s medical history included malignant rheumatoid arthritis while using steroids and an immunosuppressive agent. Because of interstitial pneumonia, he had been inhaling oxygen (3 L/min) at home. One year prior, the patient experienced mediastinal emphysema due to pneumothorax and was cured via nonoperative management. Vital signs were stable. Snowball crepitations were noted on the chest and neck. The abdomen was not distended, and there was no abdominal pain or sign of peritoneal irritation. A recurrence of pneumothorax was suspected, and chest radiography was performed, which revealed subcutaneous emphysema of the neck, mediastinal emphysema, and subdiaphragmatic free air (Fig. 1). Computed tomography (CT) of the neck, thorax, and abdomen was performed to rule out gastrointestinal perforation. This showed extensive retroperitoneal and mediastinal emphysema, including emphysema of the sigmoid colon mesentery (Fig. 2a–d). No evidence of pneumothorax was detected. Laboratory tests revealed increased white blood cell count (11,240/μL) and an elevated C-reactive protein level (17.85 mg/dL). A perforation in the mesentery due to sigmoid colon diverticulitis was strongly suspected. Diagnostic laparoscopy was performed under general anesthesia, and it revealed that the perforation was in the sigmoid mesentery (Fig. 3a–c). Segmental resection of the sigmoid colon and end-colostomy (Hartmann’s procedure) was performed via open laparotomy. Macroscopy of the surgical specimen revealed that the diverticulum was communicating with the outside of the mesentery without signs of malignancy, thus, it was diagnosed as a diverticular penetration (Fig. 4). The subcutaneous and mediastinal emphysema disappeared a few days after the surgery, and the patient was transferred from the intensive care unit to the general ward on the postoperative day 3.
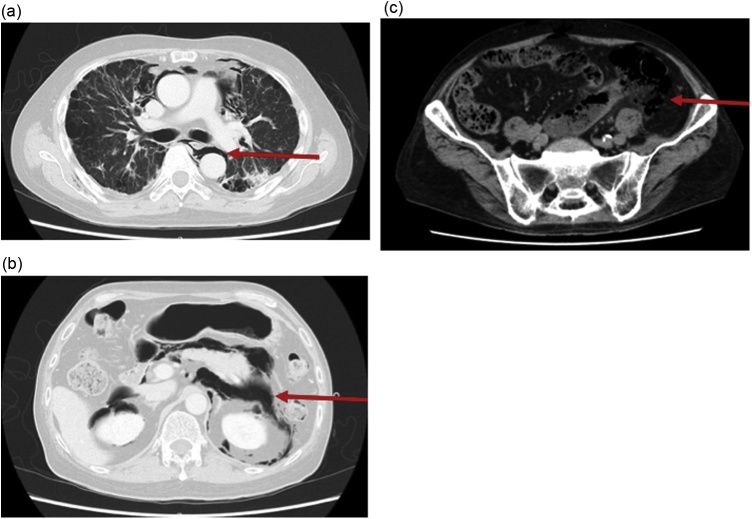
Fig. 1.
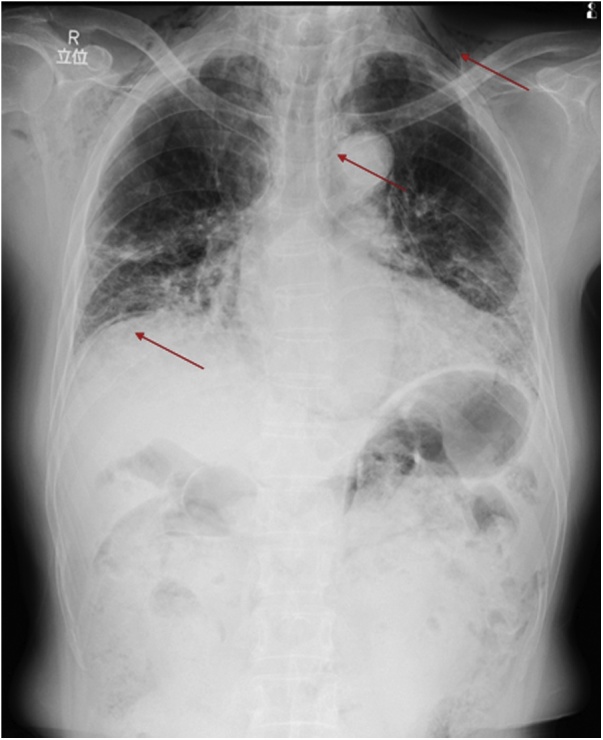
Chest radiography showing subcutaneous emphysema of the neck, mediastinal emphysema, and subdiaphragmatic free air (red arrows).
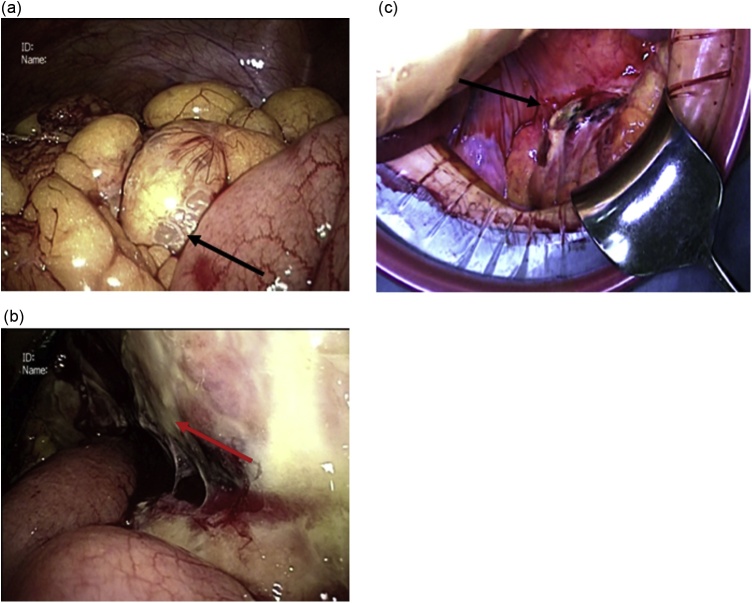
Fig. 2.
Selected images from a computed tomography (CT) scan of the chest, abdomen, and pelvis (a, b, and c: axial images; d: reformatted coronal images). CT demonstrated perforation of the sigmoid colon into the mesentery (c, red arrows). Using lung windowing, gas was found extensively, from the retroperitoneum to the mediastinum (a, b, and d, red arrows).
Fig. 3.
Intraoperative image showing intestinal emphysema (a) and necrotizing and perforating mesentery of the sigmoid colon (b: laparoscopy, c: open laparotomy).
Fig. 4.

In the macroscopic examination of the surgical specimen, the diverticulum communicates with the outside of the mesentery without signs of malignancy (the inserted probe penetrated the lumen).
3. Discussion
Colonic perforation is most often due to diverticulitis, neoplasm, and iatrogenic and traumatic mechanisms. Colonic diverticulosis is common in the developed world, affecting up to 50% of adults in Western countries [10]. Among patients with colonic diverticulosis, approximately 20% may develop diverticulitis due to infection and inflammation of the diverticula [11]. Perforation of diverticulitis is one of the most serious complications and requires an urgent operation. In some previous reports, colonic perforation resulted in a free hole occurring on the opposite side of the mesentery [12,13]. In cases of free perforation, clinical features include massive free air on CT and signs of peritoneal irritation; thus, it is easy to diagnose this early. However, spontaneous mediastinal and subcutaneous emphysema commonly occur when increased intra-alveolar pressure such as from asthma, cough, or mechanical ventilation leads to the rupture of marginal pulmonary alveoli. In particular, massive mediastinal emphysema in colonic perforation is an unusual complication, which is extremely rare without a preceding endoscopic procedure [[2], [3], [4], [5]]. To the best of our knowledge, in the English literature, only 20 cases of mediastinal emphysema following colonic perforation, excluding iatrogenic and traumatic injury, have been reported (Table 1).
Table 1.
Mediastinal emphysema as a rare complication of colon perforation reported in the English literature.
| Case | Year | Author | Age/sex | Cause | Remarks | Presenting symptom | Peritoneal irritation | Time from onset (days) | Site | Surgery | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1968 | Maw | 90/F | Diverticulitis | None | Constipation, Subcutaneous emphysema | None | 3 | Sigmoid colon | NOM | Survived |
| 2 | 1973 | Suros and Lee | 80/F | Diverticulitis | NA | Abdominal pain, fever | NA | 1 | Sigmoid colon | colostomy | Survived |
| 3 | 1973 | Suros and Lee | 63/M | Diverticulitis | NA | Abdominal pain, fever, shortness of breath | NA | 19 | Sigmoid colon | colostomy | Survived |
| 4 | 1973 | Dharia and Shah | 66/M | Diverticulitis | NA | Substernal pain | None | 1 | Sigmoid colon | NOM | Survived |
| 5 | 1980 | Mogan et al. | 22/M | Ulcerative colitis | Steroids and immunosuppressive agent | Abdominal pain, fever, | None | 1 | NA | Subtotal colectomy | Survived |
| 6 | 1980 | Mogan et al. | 16/F | Ulcerative colitis | Steroids | Abdominal pain, fever | None | 10 | NA | Subtotal colectomy | Survived |
| 7 | 1995 | Hur et al. | 67/F | Diverticulitis | Diabetes Mellitus | Neck swelling | None | 7 | Sigmoid colon | Hartmann's procedure | Survived |
| 8 | 2000 | von Oers et al. | 66/M | Diverticulitis | NA | Abdominal pain, fever | NA | NA | Sigmoid colon | Hartmann's procedure | Survived |
| 9 | 2002 | Soliani et al. | 63/M | Diverticulitis | Steroids | Abdominal pain | None | a few days | Sigmoid colon | Hartmann's procedure | Survived |
| 10 | 2004 | Becic et al. | 50/F | Diverticulitis | Steroids and immunosuppressive agent | Neck swelling | None | 3 | Descending colon | Segmental resection and anastomosis | Survived |
| 11 | 2007 | Arana-Arri et al. | 75/F | Stercoroma | Liver cirrhosis | Abdominal distension | NA | 4 | Rectum | Hartmann's procedure | Died |
| 12 | 2008 | Schmidt et al. | 69/M | Diverticulitis | Steroids | Neck swelling, abdominal pain | NA | 1 | Sigmoid colon | Hartmann's procedure | Died |
| 13 | 2009 | Wawrzak et al. | 58/M | Colon cancer | Steroids | Abdominal pain | None | 2 | Descending colon | Hartmann's procedure | Survived |
| 14 | 2009 | Wawrzak et al. | 60/M | Rectal cancer | Radiation and Chemo therapy | Lower limb pain | None | 14 | Rectum | colostomy | Survived |
| 15 | 2010 | Choi et al. | 59/M | Diverticulitis | None | Abdominal pain | None | 30 | Sigmoid colon | Hartmann's procedure | Died |
| 16 | 2012 | Annahazi et al. | 19/M | Ulcerative colitis | Steroids and immunosuppressive agent | Chest pain, shortness of breath | None | 7 | NA | NOM | Survived |
| 17 | 2014 | Wiles et al. | 81/F | Diverticulitis | Steroids and immunosuppressive agent | Abdominal pain | None | NA | Sigmoid colon | NOM | Survived |
| 18 | 2014 | Fosi et al. | 57/M | Diverticulitis | None | Abdominal pain | None | a few days | Sigmoid colon | Hartmann's procedure | Survived |
| 19 | 2015 | Montori et al. | 59/F | NA | None | Abdominal pain | None | NA | Descending colon | colostomy | Survived |
| 20 | 2018 | The present case | 53/M | Diverticulitis | Steroids and immunosuppressive agent | Chest pain | None | 5 | Sigmoid colon | Hartmann's procedure | Survived |
Abbreviations: NA, no available information NOM, non-operative management.
All cases involved perforation into the retroperitoneal or intramesenteric space. The most common cause of subcutaneous and mediastinal emphysema of colonic origin was diverticulitis (13 cases) [[2], [3], [4], [5],7,[14], [15], [16], [17], [18], [19]]. Our case also showed a wide range of emphysema from the mesentery to the retroperitoneum, mediastinum, and subcutaneous tissue. The pressure gradient between the gastrointestinal lumen and the retroperitoneal and subcutaneous tissue is the mechanism by which colonic perforation presents extensive subcutaneous and mediastinal emphysema. The retroperitoneal cavity is divided into three large areas and small parts; the three areas are the anterior pararenal space, the perirenal space, and the posterior pararenal space [20]. The anterior pararenal space is continuous with the mesentery, the small intestine, and the colon, and the head side of the posterior pararenal space is linked to the diaphragm, continuing to the mediastinum [[20], [21], [22]]. Quigley et al. reported that gastrointestinal tract pressure would be as high as 60 mmH2O in its natural state, and that gas would spread from the mesentery to the retroperitoneal space beyond the diaphragm [23]. Depending on the location of the perforation, signs of peritoneal irritation may be evident, but they can be hidden in cases of retroperitoneal colonic perforation. Colonic gas may spread via various anatomical pathways when perforation of the colon occurs in the retroperitoneum; thus, diverse atypical clinical symptoms may be present [24]. The atypical manifestation of a retroperitoneal colonic perforation can cause difficulties in making a diagnosis [[2], [3], [4], [5],24].
Additionally, in patients receiving steroid administration, abdominal signs are generally poor. Particularly, in patients receiving prednisone at 20 mg/day or more, clinical symptoms may not be noticeable even in cases of peritonitis resulting from a perforation and an abscess [25]. Remine et al. reported a colonic perforation due to steroid administration. They found that the mortality rate of patients who were receiving a dose of 20 mg/day or less was 13.3%, while that of those who were receiving a dose of 20 mg/day or more was 85.1% [26]. In our case, high-dose prednisolone therapy had been administered twice to treat malignant rheumatoid arthritis, and an average of 22.5 mg of prednisolone was administered. We carefully conducted a physical examination, but we did not identify any spontaneous pain in the abdomen or symptom of peritoneal irritation. In the 20 cases presented in Table 1 (including our own case), steroids and immunosuppressive agents were administered; symptoms could have been masked. Moreover, the duration from the onset of symptoms to the initiation of therapy was relatively long (Table 1); the emphysema may have widely spread.
Diagnosis in a patient with covert symptoms can be challenging for surgeons; thus, delayed diagnosis may be occurred especially in the absence of peritoneal signs and abdominal pain due to both steroid use and intramesenteric perforation. A CT scan in stable patients can be useful to detect direct evidence of colonic perforation and penetration, such as retroperitoneal and mesenteric emphysema. Finally, we suspected that the retroperitoneal and mediastinal emphysema may be from the thorax. The proportion of retroperitoneal emphysema due to intrathoracic factors was only 3.5%, which is relatively rare. In our case, judging that the mediastinal emphysema was due to the penetration of the colonic diverticulitis might be valid from two standpoints: the colonic penetration was obvious from the CT scan and there was no evidence of pneumothorax. The fact that the emphysema from the colon expanded to the mediastinum is suggestive of mediastinal infection, and delay in surgical treatment should increase the risk of developing mediastinitis. Therefore, laparotomy should be performed immediately in cases of colonic penetration of diverticulitis, where the emphysema expands to the mediastinum extensively.
4. Conclusions
Massive mediastinal and retroperitoneal emphysema may be rare signs of colonic perforation. Despite the presence of colonic penetration, the diagnosis may be delayed due to the absence of peritoneal irritation. Emergency laparotomy, including diagnostic laparoscopy, should be considered in cases of colonic penetration of diverticulitis, where the emphysema expands to the mediastinum extensively.
Conflict of interest
The authors of this paper declare that they have no competing interests regarding the publication of this paper.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This study is exempt from ethical approval in our institution.
Consent
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Author contribution
TM drafted the article. EH, AK, KT, SK, KO, YS, and HW carried out the acquisition of data. HW participated in the critical revision of the manuscript. All authors read and approved the manuscript. TM take responsibility for the paper as a whole.
Registration of research studies
researchregistry4660.
Guarantor
TM take responsibility for the paper as a whole.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Maunder R.J., Pierson D.J., Hudson L.D. Subcutaneous and mediastinal emphysema: pathophysiology, diagnosis, and management. Arch. Intern. Med. 1984;144:1447–1453. [PubMed] [Google Scholar]
- 2.Hur T., Chen Y., Shu G.H., Chang J.M., Cheng K.C. Spontaneous cervical subcutaneous and mediastinal emphysema secondary to occult sigmoid diverticulitis. Eur. Respir. J. 1995;8:2188–2190. doi: 10.1183/09031936.95.0812188. [DOI] [PubMed] [Google Scholar]
- 3.Suros J., Lee R.A. Pneumoretroperitoneum, pneumomediastinum, and subcutaneous emphysema. Complications of acute, perforated diverticulitis. Minn. Med. 1973;56:747–749. [PubMed] [Google Scholar]
- 4.van Oers J.A.H., Ponssen H.H., WLEM Hesp. Pneumopericardium, pneumomediastinum, pericarditis and mediastinal abscess secondary to diverticulitis of the sigmoid. Intensive Care Med. 2000;26:1867–1868. doi: 10.1007/s001340000711. [DOI] [PubMed] [Google Scholar]
- 5.Besic N., Zgajnar J., Kocijancic I. Pneumomediastinum, pneumopericardium, and pneumoperitoneum caused by peridiverticulitis of the colon: report of a case. Dis. Colon Rectum. 2004;47:766–768. doi: 10.1007/s10350-003-0102-x. [DOI] [PubMed] [Google Scholar]
- 6.Onur M.R., Akpinar E., Karaosmanoglu A.D., Isayev C., Karcaaltincaba M. Diverticulitis: a comprehensive review with usual and unusual complications. Insights Imaging. 2017;8:19–27. doi: 10.1007/s13244-016-0532-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi P.W. Pneumomediastinum caused by colonic diverticulitis perforation. J. Korean Surg. Soc. 2011;80(Suppl 1):17–20. doi: 10.4174/jkss.2011.80.Suppl1.S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mogan G.R., Sachar D.B., Bauer J., Salky B., Janowitz H.D. Toxic megacolon in ulcerative colitis complicated by pneumomediastinum: report of two cases. Gastroenterology. 1980;79:559–562. [PubMed] [Google Scholar]
- 9.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Warner E., Crighton E.J., Moineddin R., Mamdani M., Upshur R. Fourteen-year study of hospital admissions for diverticular disease in Ontario. Can. J. Gastroenterol. 2007;21:97–99. doi: 10.1155/2007/943460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bordeianou L., Hodin R. Controversies in the surgical management of sigmoid diverticulitis. J. Gastrointest. Surg. 2007;11:542–548. doi: 10.1007/s11605-007-0126-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bell J.W. Intramesenteric perforation of colon diverticulitis. Arch. Surg. 1971;102:471–473. doi: 10.1001/archsurg.1971.01350050037012. [DOI] [PubMed] [Google Scholar]
- 13.Jensen J.A., Tsang D., Minnis J.F., Ponn T., Merrell R.C. Pneumopylephlebitis and intramesocolic diverticular perforation. Am. J. Surg. 1985;150:284–287. doi: 10.1016/0002-9610(85)90140-0. [DOI] [PubMed] [Google Scholar]
- 14.Maw A. Perforation of the sigmoid colon resulting in subcutaneous emphysema of the head and neck and associated pneumoperitoneum. Br. J. Surg. 1968;55:712–714. [Google Scholar]
- 15.Dharia K.M., Shah I.C. Subcutaneous emphysema of gastrointestinal origin: report of four cases. Dis. Colon Rectum. 1973;16:319–324. doi: 10.1007/BF02587711. [DOI] [PubMed] [Google Scholar]
- 16.Soliani G., Dominici M., Bergossi L., Basaglia E., Pauli S., Carcoforo P. Acute colon diverticulitis in multiple myeloma patient: an unusual presentation of a colonic perforation. Case report. Ann. Ital. Chir. 2002;73:643–646. [PubMed] [Google Scholar]
- 17.Schmidt G.B., Bronkhorst M.W., Hartgrink H.H., Bouwman L.H. Subcutaneous cervical emphysema and pneumomediastinum due to a lower gastrointestinal tract perforation. World J. Gastroenterol. 2008;14:3922. doi: 10.3748/wjg.14.3922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiles T., Mullett R., Chadwick M. Diverticular perforation: an unusual cause of subcutaneous emphysema. Emerg. Med. J. 2014;31:259–260. doi: 10.1136/emermed-2013-202662. [DOI] [PubMed] [Google Scholar]
- 19.Fosi S., Giuricin V., Girardi V., Di Caprera E., Costanzo E., Di Trapano R. Subcutaneous emphysema, pneumomediastinum, pneumoretroperitoneum, and pneumoscrotum: unusual complications of acute perforated diverticulitis. Case Rep. Radiol. 2014;2014 doi: 10.1155/2014/431563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ishikawa K., Idoguchi K., Tanaka H., Tohma Y., Ukai I., Watanabe H. Classification of acute pancreatitis based on retroperitoneal extension: application of the concept of interfascial planes. Eur. J. Radiol. 2006;60:445–452. doi: 10.1016/j.ejrad.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 21.Lai W., Dowell J. Images in clinical medicine. Diffuse subcutaneous air due to a perforated colonic diverticulum. N. Engl. J. Med. 2004;350:e12. doi: 10.1056/ENEJMicm020108. [DOI] [PubMed] [Google Scholar]
- 22.Meyers M.A. Radiological features of the spread and localization of extraperitoneal gas and their relationship to its source. An anatomical approach. Radiology. 1974;111:17–26. doi: 10.1148/111.1.17. [DOI] [PubMed] [Google Scholar]
- 23.Quigley J.P., Brody D.A. A physiologic and clinical consideration of the pressures developed in the digestive tract. Am. J. Med. 1952;13:73–81. doi: 10.1016/0002-9343(52)90082-x. [DOI] [PubMed] [Google Scholar]
- 24.Ravo B., Khan S.A., Ger R., Mishrick A., Soroff H.S. Unusual extraperitoneal presentations of diverticulitis. Am. J. Gastroenterol. 1985;80:346–351. [PubMed] [Google Scholar]
- 25.Marshall L.F., King J., Langfitt T.W. The complications of high-dose corticosteroid therapy in neurosurgical patients: a prospective study. Ann. Neurol. 1977;1:201–203. doi: 10.1002/ana.410010220. [DOI] [PubMed] [Google Scholar]
- 26.ReMine S.G., McIlrath D.C. Bowel perforation in steroid-treated patients. Ann. Surg. 1980;192:581–586. doi: 10.1097/00000658-198010000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]