Abstract
AIM
To investigate the pooled prevalence of diabetic retinopathy (DR), proliferative DR (PDR) and nonproliferative DR (NPDR) in Asian type 2 diabetes mellitus (T2DM) patients.
METHODS
We performed a systematic search online search using PubMed, EMBASE, Web of Science, the Cochrane Library, and China WeiPu Library to identify eligible studies that reported the prevalence of DR, PDR and NPDR in Asian T2DM patients. Effect size (ES) with 95% confidence interval (CI) was used to evaluate the prevalence of DR, PDR and NPDR in Asian T2DM patients, respectively.
RESULTS
There were 41 references and 48 995 T2DM patients involved in this study. The prevalence of DR, PDR, and NPDR was 28%, 6%, and 27% in T2DM patients, respectively; while the prevalence of PDR and NPDR in DR patients was 17% and 83%, respectively. Subgroup analysis showed that prevalence of DR in T2DM patients from Singaporean, Indian, South Korean, Malaysian, Asian, and Chinese was 33%, 42%, 16%, 35%, 21% and 25%, respectively. In T2DM patients with NPDR from Indian, South Korean, Malaysian, Asian, Chinese, higher prevalence was found than that in PDR patients (45% vs 17%, 13% vs 3%, 30% vs 5%, 23% vs 2% and 22% vs 3%), as well as in DR patients (74% vs 26%, 81% vs 19%, 86% vs 14%, 92% vs 8% and 85% vs 15%). The prevalence of PDR in T2DM from India was higher than patients from other locations of Asia, and the same results were also observed in NPDR patients.
CONCLUSION
In either T2DM Asian patients or DR patients, NPDR is more common than PDR. Based on our results, we should pay more attention to NPDR screening and management in T2DM patients, and we also recommend suitable interventions to prevent its progression.
Keywords: prevalence, proliferative diabetic retinopathy, nonproliferative diabetic retinopathy, Asian, type 2 diabetes mellitus
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is now considered as a growing world-wide health concern[1]. Nearly 180 million adults were reported to suffer from diabetes in 1980. The number of T2DM increased to 422 million in 2014[1], which is expected to be more than 552 million in 2030[2]. Several related complications have been observed in T2DM, such as diabetic nephropathy[3], diabetic cardiovascular diseases[4] and diabetic retinopathy (DR)[5]. Among these complications, DR is a common one and is classified as a microvascular damage disease, which includes two subtypes: nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR)[6]. DR is a leading cause of blindness in working-age adults with T2DM. According to statistics, once T2DM patients are diagnosed as DR, it will progress to vision threaten stage in approximately 11% patients every year, making DR a public health challenge[7].
It is believed that optimal screening strategies for DR in T2DM is necessary to public health due to its disastrous outcomes. Therefore, it is crucial to explore the prevalence of DR as well as PDR and NPDR in T2DM patients to provide further evidence for screening strategies. However, the prevalence of DR and PDR in different researches remains controversial. In Huang et al's[8] research, the prevalence of DR in Singaporean, Indian and Chinese populations was 36.88%, 36.47% and 30.30%, respectively, and the prevalence of PDR was 27.72%, 25.82% and 26.57%, respectively, which was inconsistent with Thomas et al's[9] study, who reported that the prevalence of PDR in South Africa was 6.6%. In Stolk et al's[10] study, the prevalence of DR in Caucasian, Chinese and South Asian populations was 31.3%, 49.4% and 46.0% respectively, and the prevalence of PDR in Caucasian, Chinese and South Asian population was 1.2%, 3.5% and 1.7%, respectively.
Previous Meta-analyses have been performed to explore the prevalence of DR, PDR and NPDR in Iran and Chinese populations; however, these results were also conflicting[11]–[12]. Maroufizadeh et al[12] recruited thirty-one studies involving 23 729 patients with type 1 and 2 diabetes. Their results showed that the prevalence of DR, NPDR and PDR in Iranian diabetic patients were 41.9% (95%CI: 35.6–48.2), 32.2% (95%CI: 28.7–35.8), and 13.2% (95%CI: 8.3–18.1), respectively. In Liu et al's[11] study, the prevalence of DR, NPDR and PDR in the pooled general population was 1.3% (95%CI: 0.5%–3.2%), 1.1% (95%CI: 0.6%–2.1%), and 0.1% (95%CI: 0.1%–0.3%), respectively, but was 23% (95%CI: 17.8%–29.2%), 19.1% (95%CI: 13.6%–26.3%), and 2.8% (95%CI: 1.9%–4.2%) in the diabetic group. Due to this conflicting result of Meta-analysis and the fact that no Meta-analysis and sub-analysis has been performed to detect this issue in other Asian countries, we performed this systematic review and Meta-analysis to investigate the pooled prevalence of DR, PDR and NPDR in Asian T2DM patients.
MATERIALS AND METHODS
Literature Search
A systematic online search was conducted to find out all the eligible studies that reported the prevalence of DR, NPDR and PDR in Asian populations. Databases including ‘PubMed’, ‘EMBASE’, ‘Web of Science’, ‘Cochrane Library’ and ‘China WeiPu Library’ were searched. The following search terms were used to identify all the relevant studies: (‘prevalence’ OR ‘incidence’) AND (‘diabetic retinopathy’ OR ‘nonproliferative diabetic retinopathy’ OR ‘proliferative diabetic retinopathy’ OR ‘DR’ OR ‘PDR’ OR ‘NPDR’). Then, studies were screened according to their study populations. There were no language and date restrictions in our searching procedure. The reference lists of the recruited studies, reviews or conference reports were also searched. Furthermore, the reviews and comments were also searched. All the analyses involved in our study were based on previous published studies, thus no ethical approval and patient consent are required.
Inclusion and Exclusion Criteria
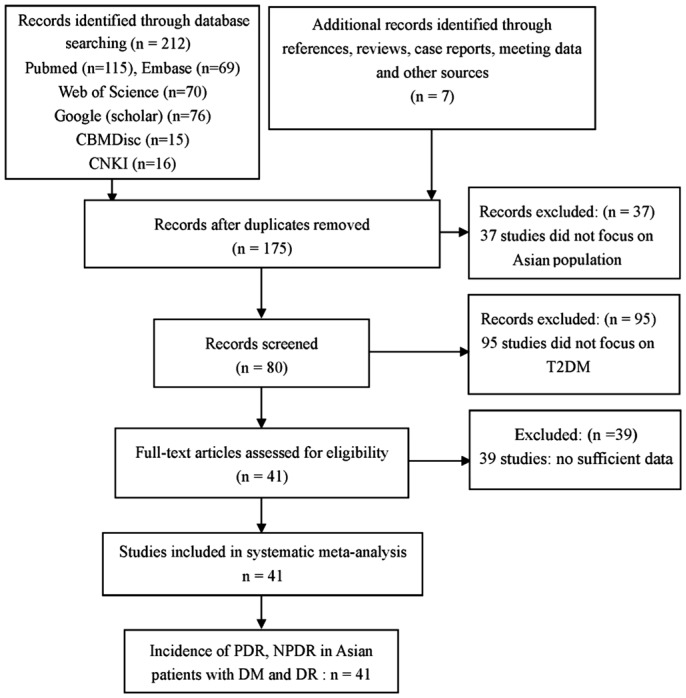
The inclusion criteria were as follows: 1) studies with prevalence estimates of DR, PDR and NPDR, including the numbers of DR, PDR, NPDR and T2DM; 2) study populations in Asian countries. The exclusion criteria were as follows: 1) intervention or treatment studies; 2) no usable data reported; 3) duplicated studies. In addition, studies that reported the prevalence of DR, PDR and NPDR in T1DM were also excluded. The progress for study inclusion is shown in Figure 1.
Figure 1. Flow chart showing the process of selection.
Data Extraction
Two authors extracted the general information and data in each study according to the inclusion and exclusion criteria, and a consensus was reached by discussion. If there was any disagreement, a third author would extract them, which was solved by consensus. Data were extracted using a standard form. The following data were collected: author, publish year, ethnicity, age, number of T2DM, DR, NPDR and PDR, and the total sample size. We also contacted the corresponding authors if there were incomplete data in recruited studies.
Quality Assessment
Newcastle Ottawa Quality Assessment Scale (NOQAS)[13] was used to assess the quality of all studies including non-randomized case controlled studies.
Data Synthesis
Effect size (ES) with 95%CI was assessed to analyze the pooled prevalence of DR, PDR and NPDR in T2DM populations. The prevalence of PDR and NPDR in DR populations were also performed. Subgroup analysis according to the ethnicity of populations was also performed. The heterogeneity of included studies was examined by a Chi-squared-based Q statistical test and quantified by I2 metric value. If I2 value was more than 50% or P<0.10, ES was pooled by the random effect model; otherwise, the fixed effect model was used. Sensitivity analysis was performed to assess the impact of each study on the combined effect of the present Meta-analysis. Stata 12.0 software (StataCorp, College Station, TX, USA) was used, and a P<0.05 was considered as statistically significant.
RESULTS
Study Selection and Characteristics
A total of 41 studies were finally included in our study (Figure 1). Of 6 studies were performed in Asian populations[14]–[19]; 4 studies were conducted in Singaporean group[8],[20]–[23]; 7 studies were conducted in Indian group[23]–[28]; 2 studies were performed in South Korean group[29]–[30]; 2 studies were conducted in Malaysian populations[14],[31] and 20 studies were performed in Chinese group[19],[32]–[50]. And 10 studies reported the numbers of DR and DM[8],[14]–[15],[17],[21]–[23],[35],[46], while 31 studies reported the numbers of DR, PDR, NPDR and DM[10],[16],[19],[24]–[34],[36]–[37],[39]–[45],[47]–[49],[51]–[52]. The general characteristics of included studies were shown in Table 1.
Table 1. The general characteristics of included studies.
| Author | Publish Year | Ethnicity | Age (y) | DM (n) | DR (n) |
Sample (n) | ||
| PDR | NPDR | Total | ||||||
| Wong et al | 2016 | Singaporean | CKD+/−: 57.3/68.3 | 2251 | NR | NR | 453 | 9434 |
| Huang et al | 2015 | Singaporean | 40–80 | 2376 | NR | NR | 805 | 10033 |
| Sabanayagam et al | 2015 | Singaporean | NR | 13170 | NR | NR | 4111 | 13170 |
| Pradeepa et al | 2015 | Indian | >20 | 1723 | 203 | 215 | 418 | 1723 |
| Rooney et al | 2015 | Singaporean | >40 | 2278 | NR | NR | 800 | 2278 |
| Rajalakshmi et al | 2014 | Indian | DR+/−:38.1±9.1/28.0±7.8 | 300 | 14 | 65 | 79 | 300 |
| Cheema et al | 2012 | Indian | NR | 1720 | 582 | 260 | 842 | 1720 |
| Zheng et al | 2012 | Indian | >40 | 1065 | 246 | 819 | 1201 | 3174 |
| Zheng et al | 2012 | Indian | >40 | 610 | 124 | 423 | 547 | 1893 |
| Kim et al | 2011 | South Korean | >40 | 1298 | 17 | 217 | 234 | 1298 |
| Huang et al | 2010 | Malaysian | 40–80 | 768 | NR | NR | 272 | 768 |
| An et al | 2009 | South Korean | 59±10 | 562 | 25 | 56 | 81 | 562 |
| Pan et al | 2008 | Asian | 18–80 | 8561 | NR | NR | 1199 | 8561 |
| Wong et al | 2008 | Malaysian | 40–79 | 757 | 37 | 228 | 265 | 3261 |
| Stolk et al | 2008 | Asian | 65.7±6.1 | 785 | 24 | 358 | 382 | 785 |
| Rema et al | 2004 | Indian | DR+/−: 54±11; 52±11 | 6 | 110 | 116 | 590 | 590 |
| Kumaramanickavel et al | 2001 | Indian | DR+/−: 61; 60 | 34 | 66 | 100 | 207 | 207 |
| Chang et al | 2000 | Chinese | >40 | 67 | 133 | 200 | 1333 | 11478 |
| Dowse et al | 1998 | Asian | DR+/−: 54.6; 51.8 | 2 | 108 | 110 | 746 | 746 |
| Das et al | 1994 | Asian | >40 | 22 | NR | NR | 5 | 165 |
| Hu et al | 1991 | Chinese | 25–74 | 423 | 10 | 119 | 129 | 110660 |
| He et al | 1997 | Chinese | >30 | 534 | 2 | 88 | 90 | 29938 |
| Li et al | 1998 | Chinese | >15 | 216 | NR | NR | 67 | 11618 |
| Wang et al | 2001 | Chinese | ≥25 | 326 | 7 | 30 | 37 | 1438 |
| Zhou et al | 2006 | Chinese | 44–87 | 535 | 23 | 123 | 146 | 43762 |
| Liang et al | 2006 | Chinese | >18 | 356 | 38 | NR | NR | 10723 |
| Xie et al | 2009 | Chinese | >40 | 434 | 12 | 273 | 285 | 4391 |
| Liu et al | 2009 | Chinese | 14–82 | 137 | 0 | 17 | 17 | 1534 |
| Shu et al | 2010 | Chinese | ≥25 | 689 | 74 | 107 | 181 | 16330 |
| Xin et al | 2010 | Chinese | >35 | 114 | 2 | 25 | 27 | 1293 |
| Teng et al | 2010 | Chinese | >50 | NR | 7 | 49 | 56 | 5053 |
| Dong et al | 2010 | Chinese | >18 | 554 | 18 | 76 | 94 | 5753 |
| Ynag et al | 2010 | Chinese | 35–80 | 381 | 18 | 69 | 87 | 3381 |
| Wang et al | 2010 | Chinese | >15 | 2632 | NR | NR | 986 | 57500 |
| Ye et al | 2010 | Chinese | >20 | 1046 | 30 | 71 | 101 | 11723 |
| Wang et al | 2011 | Chinese | >30 | 368 | 20 | 145 | 165 | 6830 |
| Li et al | 2011 | Chinese | ≥40 | 445 | 6 | 124 | 130 | 4167 |
| Pang et al | 2011 | Chinese | >15 | 799 | 1 | 74 | 75 | 3259 |
| Das et al | 1994 | Asian | ≥40 | 173 | NR | NR | 23 | 173 |
| Raymond et al | 2009 | Asian | ≥30 | 421 | 12 | 33 | 45 | 421 |
| Dowse et al | 1998 | Chinese | DR+/−: 54.6; 51.8 | 57 | 2 | 23 | 25 | 57 |
PDR: Proliferative diabetic retinopathy; NPDR: Nonproliferative diabetic retinopathy; DR: Diabetic retinopathy; DM: Diabetes mellitus; CKD+/−: Patients with/without CKD; DR+/−: Patients with/without DR.
Quality Assessment
The quality assessments of studies are shown in Table 2, and we considered that the quality of each study was relatively high. In our study, 5 researches scored 9 points[7],[19],[24],[30],[43]; 27 studies scored 8points[8],[10],[14],[16]–[19],[22]–[23],[25]–[26],[28],[31]–[35],[37],[40]–[43],[46],[48]–[49]; 9 researches scored 7 points[15],[17],[28]–[29],[36],[38]–[39],[45],[51].
Table 2. The quality assessment according to the Newcastle Ottawa Quality Assessment Scale (NOQAS) of each study.
| Study | Year | Selection | Comparability | Exposure | Total score |
| Wong et al | 2016 | 4 | 2 | 3 | 9 |
| Huang et al | 2015 | 3 | 2 | 3 | 8 |
| Sabanayagam et al | 2015 | 3 | 2 | 3 | 8 |
| Pradeepa et al | 2015 | 4 | 2 | 3 | 9 |
| Rooney et al | 2015 | 3 | 2 | 3 | 8 |
| Rajalakshmi et al | 2014 | 3 | 2 | 3 | 8 |
| Cheema et al | 2012 | 3 | 2 | 3 | 8 |
| Zheng et al | 2012 | 3 | 2 | 3 | 8 |
| Zheng et al | 2012 | 3 | 2 | 2 | 7 |
| Kim et al | 2011 | 3 | 2 | 2 | 7 |
| Huang et al | 2010 | 3 | 2 | 3 | 8 |
| An et al | 2009 | 4 | 2 | 3 | 9 |
| Pan et al | 2008 | 3 | 2 | 2 | 7 |
| Wong et al | 2008 | 3 | 2 | 3 | 8 |
| Stolk et al | 2008 | 3 | 2 | 3 | 8 |
| Rema et al | 2004 | 3 | 2 | 2 | 7 |
| Kumaramanickavel et al | 2001 | 3 | 2 | 3 | 8 |
| Chang et al | 2000 | 3 | 2 | 3 | 8 |
| Dowse et al | 1998 | 3 | 2 | 3 | 8 |
| Das et al | 1994 | 3 | 2 | 2 | 7 |
| Hu et al | 1991 | 3 | 2 | 3 | 8 |
| He et al | 1997 | 3 | 2 | 3 | 8 |
| Li et al | 1998 | 3 | 2 | 3 | 8 |
| Wang et al | 2001 | 3 | 2 | 2 | 7 |
| Zhou et al | 2006 | 3 | 2 | 3 | 8 |
| Liang et al | 2006 | 3 | 2 | 2 | 7 |
| Xie et al | 2009 | 3 | 2 | 2 | 7 |
| Liu et al | 2009 | 3 | 2 | 3 | 8 |
| Shu et al | 2010 | 3 | 2 | 3 | 8 |
| Xin et al | 2010 | 4 | 2 | 2 | 8 |
| Teng et al | 2010 | 4 | 2 | 3 | 9 |
| Dong et al | 2010 | 4 | 2 | 2 | 8 |
| Ynag et al | 2010 | 3 | 2 | 3 | 7 |
| Wang et al | 2010 | 3 | 2 | 3 | 8 |
| Ye et al | 2010 | 3 | 2 | 3 | 8 |
| Wang et al | 2011 | 4 | 2 | 2 | 8 |
| Li et al | 2011 | 3 | 2 | 3 | 8 |
| Pang et al | 2011 | 4 | 2 | 2 | 8 |
| Das et al | 1994 | 3 | 2 | 3 | 8 |
| Raymond et al | 2009 | 4 | 2 | 2 | 8 |
| Dowse et al | 1998 | 4 | 2 | 3 | 9 |
Meta-analysis Results
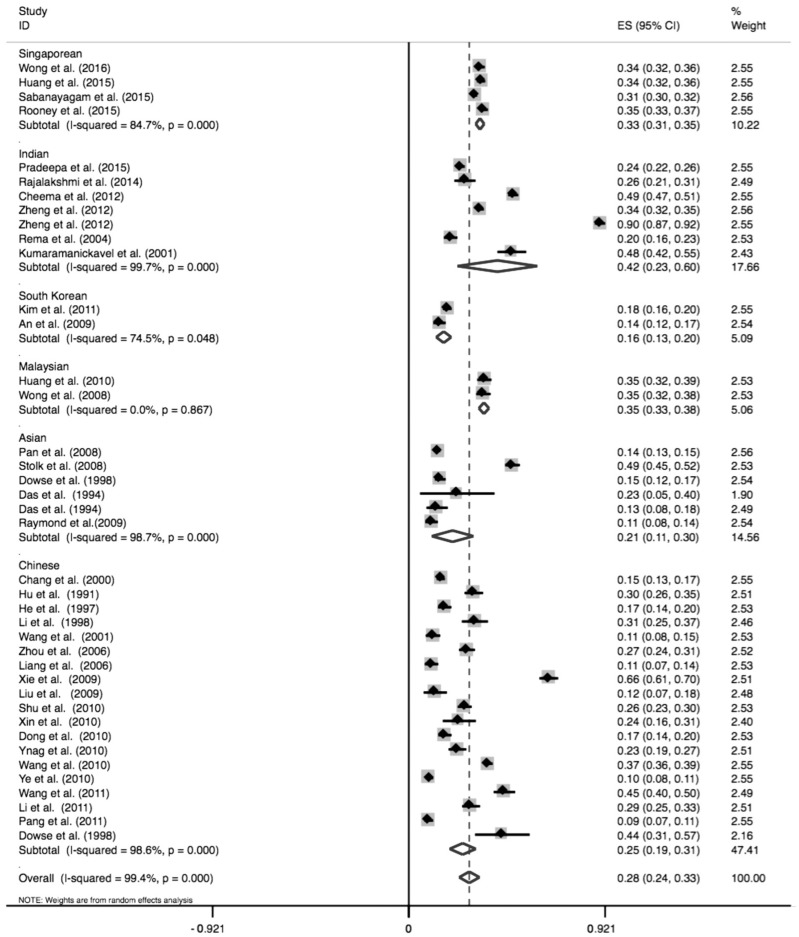
Overall, the prevalence of DR in Asian T2DM patients was 28% (95%CI: 24%–33%). Subgroup analysis showed that the prevalence of DR in Singaporean, Indian, South Korean, Malaysian, Asian and Chinese populations was 33% (95%CI: 31%–35%), 42% (95%CI: 23%–60%), 16% (95%CI: 13%–20%), 35% (95%CI: 33%–38%), 21% (95%CI: 11%–30%), and 25% (95%CI: 19%–31%), respectively, as indicated in Table 3 and Figure 2.
Table 3. The pooled results of prevalence of DR, PDR and NPDR in patients with DM.
| Variables | Prevalence (ES) | 95% CI | P value of ES | I2 (%) | P value of heterogeneity |
| Prevalence of DR in DM populations | |||||
| Overall populations | 28% (0.28) | 0.24–0.33 | <0.001 | 99.4 | <0.001 |
| Singaporean | 33% (0.33) | 0.31–0.35 | <0.001 | 84.7 | <0.001 |
| Indian | 42% (0.42) | 0.23–0.60 | <0.001 | 99.7 | <0.001 |
| South Korean | 16% (0.16) | 0.13–0.20 | <0.001 | 74.5 | 0.048 |
| Malaysian | 35% (0.35) | 0.33–0.38 | <0.001 | 0.0 | 0.867 |
| Asian | 21% (0.21) | 0.11–0.30 | <0.001 | 98.7 | <0.001 |
| Chinese | 25% (0.25) | 0.19–0.31 | <0.001 | 98.6 | <0.001 |
| Prevalence of PDR in DM populations | |||||
| Overall populations | 6% (0.06) | 0.05–0.07 | <0.001 | 98.1 | <0.001 |
| Indian | 17% (0.17) | 0.08–0.26 | <0.001 | 99.2 | <0.001 |
| South Korean | 3% (0.03) | 0.00–0.06 | 0.076 | 91.3 | 0.001 |
| Malaysian | 5% (0.05) | 0.03–0.06 | <0.001 | – | – |
| Asian | 2% (0.02) | 0.00–0.04 | 0.072 | 92.5 | <0.001 |
| Chinese | 3% (0.03) | 0.02–0.04 | <0.001 | 98.1 | <0.001 |
| Prevalence of NPDR in DM populations | |||||
| Overall populations | 27% (0.27) | 0.17–0.38 | <0.001 | 99.8 | <0.001 |
| Indian | 45% (0.45) | 0.13–0.78 | 0.006 | 99.9 | <0.001 |
| South Korean | 13% (0.13) | 0.07–0.20 | <0.001 | 94.1 | <0.001 |
| Malaysian | 30% (0.30) | 0.27–0.33 | <0.001 | – | – |
| Asian | 23% (0.23) | 0.02–0.43 | 0.028 | 99.4 | <0.001 |
| Chinese | 22% (0.22) | 0.16–0.27 | <0.001 | 99.8 | <0.001 |
| Prevalence of PDR in DR populations | |||||
| Overall populations | 17% (0.17) | 0.13–0.22 | <0.001 | 97.1 | <0.001 |
| Indian | 26% (0.26) | 0.17–0.36 | <0.001 | 97.4 | <0.001 |
| South Korean | 19% (0.19) | 0.05–0.42 | 0.115 | 94.8 | <0.001 |
| Malaysian | 14% (0.14) | 0.10–0.18 | <0.001 | – | – |
| Asian | 8% (0.08) | 0.01–0.14 | 0.019 | 88.8 | <0.001 |
| Chinese | 15% (0.15) | 0.10–0.20 | <0.001 | 93.8 | <0.001 |
| Prevalence of NPDR in DR populations | |||||
| Overall populations | 83% (0.83) | 0.78–0.87 | <0.001 | 97.1 | <0.001 |
| Indian | 74% (0.74) | 0.64–0.83 | <0.001 | 97.4 | <0.001 |
| South Korean | 81% (0.81) | 0.58–1.05 | <0.001 | 94.8 | <0.001 |
| Malaysian | 86% (0.86) | 0.82–0.90 | <0.001 | – | – |
| Asian | 92% (0.92) | 0.86–0.99 | <0.001 | 88.8 | <0.001 |
| Chinese | 85% (0.85) | 0.80–0.90 | <0.001 | 93.8 | <0.001 |
PDR: Proliferative diabetic retinopathy; NPDR: Nonproliferative diabetic retinopathy; DR: Diabetic retinopathy; DM: Diabetes mellitus; T2DM: Type 2 diabetes mellitus. Effect size with 95%CI was assessed to analyze the pooled prevalence of DR, PDR and NPDR in T2DM populations. P<0.05 was considered as statistically significant.
Figure 2. Forest plot of prevalence of DR in Singaporean, Indian, South Korean, Malaysian, Asian and Chinese populations.
In the overall Asian populations, the prevalence of PDR in DM patients was 6% (95%CI: 5%–7%). Our results also showed that the prevalence of PDR in Indian, South Korean, Malaysian, Asian and Chinese populations was 17% (95%CI: 8%–26%), 3% (95%CI: 0–6%), 5% (95%CI: 3%–6%), 2% (95%CI: 0–4%) and 3% (95%CI: 2%–4%), respectively (Table 3).
The prevalence of NPDR in Asian T2DM patients was 27% (95%CI: 17%–38%). As to the prevalence of NPDR in various regions, our study showed that the prevalence of NPDR in Indian, South Korean, Malaysian, Asian and Chinese populations was 45% (95%CI: 13%–78%), 13% (95%CI: 7%–20%), 30% (95%CI: 27%–33%), 23% (95%CI: 2%–43%), 22% (95%CI: 16%–27%), respectively, as shown in Table 3.
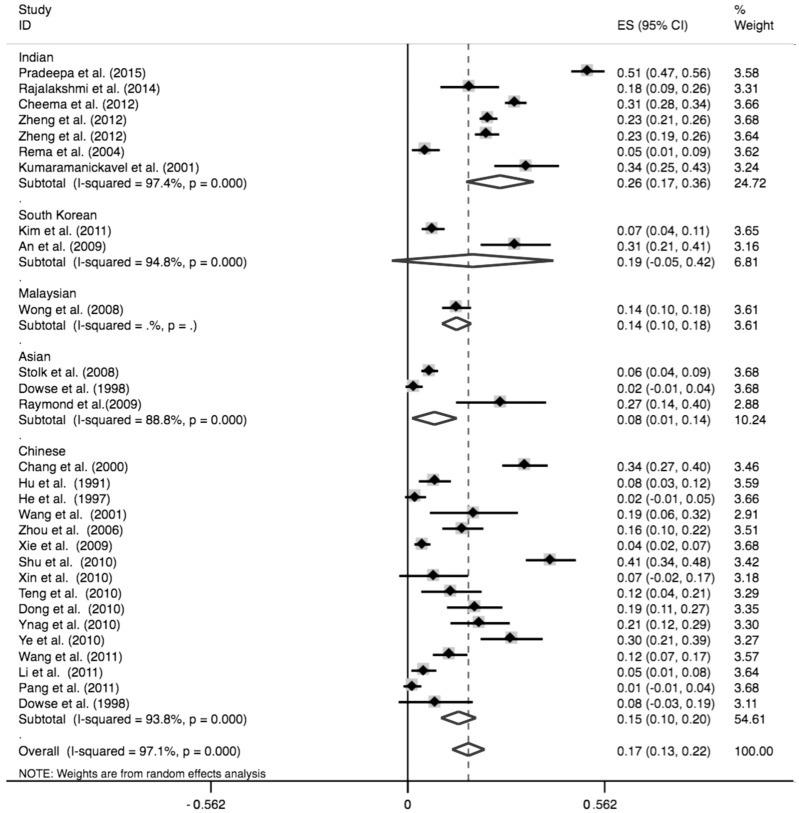
Regarding to the prevalence of PDR in DR patients, our study indicated that the prevalence of PDR overall Asian DR patients, Indian, South Korean, Malaysian, Asian and Chinese populations was 17% (95%CI: 13%–22%), 26% (95%CI: 17%–36%), 19% (95%CI: −5%–42%), 14% (95%CI: 10%–18%), 8% (95%CI: 1%–14%), and 15% (95%CI: 10%–20%), respectively (Table 3 and Figure 3).
Figure 3. Forest plot of prevalence of PDR in Indian, South Korean, Malaysian, Asian and Chinese populations.
Furthermore, NPDR was more common than PDR in either overall Asian DR patients, Indian, South Korean, Malaysian, Asian or Chinese populations as our pooled analysis and subgroup analysis showed that the prevalence of NPDR was 83% (95%CI: 78%–87%), 74% (95%CI: 64%–83%), 81% (95%CI: 58%–105%), 86% (95%CI: 82%–90%), 92% (95%CI: 86%–99%), 85% (95%CI: 80%–90%), respectively.
Sensitivity Analysis and Publication Bias
In addition, we performed the sensitivity analysis. The previous results were not affected by omission of any studies, suggesting that the results were relatively stable. Otherwise, we did not perform the publication bias due to the insufficient data.
DISCUSSION
DR is a leading complication of diabetes mellitus (DM), affecting over 130 million people worldwide[53]. Therefore, how to prevent the progression of DR and treat this devastating complication remains a challenge for ophthalmologists[54]. DR is considered as an indicator of systemic diabetic microvascular complications, and also a crucial indicator of the impact of diabetes on patients[12]. It is well acknowledged that accurate prevalence of DR including PDR and NPDR in T2DM patients could be used for guiding public health education and managing the clinical aspects of this disease in a favorable way[55]. However, the prevalence of DR, PDR and NPDR in T2DM patients from various regions reported in several studies remains conflicting[16],[21],[26]. In addition, results from two previous Meta-analyses[11]–[12] were also controversial, suggesting that an updated Meta-analysis is necessary to provide ophthalmologists with more evidence to treat this disease. To the best of our knowledges, this systematic review and Meta-analysis was the first study that investigated the prevalence of DR, PDR and NPDR in the Asian T2DM patients.
In our study, a total of 41 studies were finally included according to our inclusion and exclusion criteria. Our results showed that pooled prevalence of DR in Asian T2DM patients was 28%, which was consistent with several studies[22],[24],[56]. In Tan et al's study[56], they recruited 2877 DM patients of Malay, Indian, and Chinese ethnicity aged 40 years older, living in Singapore. Their results indicated that the overall age-standardized prevalence (95%CI) was 28.2% (25.9%–30.6%) for any DR, which was consistent with our study, further suggesting that DR was a common complication among DM patients. Besides, according to our and Tan et al's study[56], more attention should be paid to DR prevention in the follow-up time if the patient was diagnosed as DM. However, controversial results were observed in other studies[15],[26],[30]. In An et al[30] and Pan et al[15]'s study, the prevalence of DR in T2DM was smaller than that in our study; while Cheema et al[26] reported that almost 49% of T2DM patients suffered from DR. In our opinion, several factors might be contributed to this difference. First, different sample size might be a primary contributor. Our study included 41 studies involving 17 336 DR and 48 995 DM individuals, which made our results more credible than these studies. Second, we conducted this pooled analysis, in which data in various studies were used, which might lead to the change of distribution of DR in T2DM patients. Besides, different follow-up time, various inclusion and exclusion criteria and measurement errors could also explain the difference between our results and An et al[30], Pan et al[15] and Cheema et al[26]'s study. Furthermore, our results were also different from Maroufizadeh et al[12] and Liu et al[11]'s Meta-analysis. In their study, the prevalence of DR in DM patients was 41.9% and 23%, respectively. In Maroufizadeh et al's study[12], thirty-one studies involving 23 729 patients with type 1 and 2 diabetes were included; and Liu et al[11] only recruited nineteen studies. Therefore, the numbers of included studies and the total sample size might be the most important factor for the difference between our results and theirs. Besides, Maroufizadeh et al[12] reported the prevalence of DR in both type 1 and 2 diabetes patients; therefore, it is easy for us to understand this discrepancy. Therefore, our results were more credible than previous single-center studies and Meta-analysis, which could be used for guiding public health education and managing the clinical aspects of this disease in a favorable way.
Regarding prevalence of PDR and NPDR, our Meta-analysis showed the prevalence of PDR and NPDR was 6% and 27% in Asian T2DM, and 17% and 83% in DR patients, respectively. Our results indicated that NPDR was more common than PDR in both T2DM and DR populations, suggesting that NPDR screening should be paid more attention compared with PDR screening. In addition, our results also verified that NPDR was the early stage in DR progression. NPDR screening and suitable intervention should be applied if possible in T2DM patients[57]. Furthermore, our results were also consistent with two previous studies with numerous sample size[31],[56]. Tan et al[56] conducted a survey recruiting 2877 individuals, which showed prevalence of PDR and NPDR was 3.75% and 24.41%, respectively, further verifying the importance of NPDR screening in T2DM patients. Besides, different prevalence of PDR and NPDR in T2DM were reported in some other studies, though their study also indicated higher prevalence of NPDR in T2DM[24],[26]. Dissimilarity of ophthalmologic definitions, examination methodologies and specific population might contribute to this difference. Our study was more credible than Cheema et al[26] and Pradeepa et al[24]'s study as they only performed the analysis in Indian populations; while our study was multi-ethnic. Furthermore, although two previous Meta-analyses[11]–[12] showed the same results as ours, their studies only focus on the prevalence PDR and NPDR in T2DM patients, while we performed analyses in both T2DM and DR patients. Therefore, based on our results and previous studies, we recommend that NPDR screening is essential in T2DM to prevent its progression into severe stage (PDR)[57].
We also performed a subgroup analysis to explore whether the prevalence of DR, PDR and NPDR in T2DM is different among various origins. Our subgroup analysis showed that the prevalence of PDR in Indian patients with T2DM and DR was the highest compared with that in Southern Korean, Malaysian, Asian and Chinese populations. Meanwhile, some researchers held the views that Indian ethnicity was an independent risk factor for DR[56], further verifying our results. Therefore, as to Indian ophthalmologists, more focus should be paid on Indian T2DM patients than ophthalmologists from other origins. In our views, the different prevalence in various origins might be resulted from obesity, urbanization, changes in diet, education level of the involved region, increasingly sedentary lifestyles and so on[58]. In addition, the characteristics of studies, such as different inclusion and exclusion criteria, measurement errors and sample size might also contribute to the discrepancy of prevalence between different origins. Therefore, improvement of education, diet and other factors should also gain enough attentions other than regular examinations in T2DM to prevent the occurrence of this complication.
Our study is the first systematic review and Meta-analysis that investigated the prevalence of DR, PDR and NPDR in T2DM patients in various Asian countries. Although our study provided basic evidence for ophthalmologists in DR screening, some limitations should be addressed. First, our study only focused on the prevalence in Asian DM patients due to the insufficient data in other ethnicities. Therefore, whether the prevalence of DR, PDR and NPDR in Caucasian populations was as high as that in Asian populations remains further investigated. Second, the prevalence might be affected by other risk factors, such as diet and environment. Due to the insufficient data, we could not perform adjusted analysis in our study, which is also a limitation. Third, sample size in some studies was relatively small, which might also have impacts on our pooled results. Therefore, studies with large sample size in different ethnicities should be performed to determinate the accurate prevalence of DR, PDR and NPDR to provide more knowledges to ophthalmologists when they treat T2DM patients diagnosed as DR.
In either T2DM Asian patients or DR patients, NPDR was more common than PDR. Based on our results, we should pay more attention to NPDR screening and management in T2DM patients, and we also recommend suitable interventions to prevent its progression. In addition, other factors, such as diet and environment should also not be ignored.
Acknowledgments
Conflicts of Interest: Yang QH, None; Zhang Y, None; Zhang XM, None; Li XR, None.
REFERENCES
- 1.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hod M, Kapur A, Sacks DA, Hadar E, Agarwal M, di Renzo GC, Roura LC, McIntyre HD, Morris JL, Divakar H. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on gestational diabetes mellitus: a pragmatic guide for diagnosis, management, and care. Int J Gynaecol Obstet. 2015;131:S173–S211. doi: 10.1016/S0020-7292(15)30033-3. [DOI] [PubMed] [Google Scholar]
- 3.Vinik AI, Nevoret ML, Casellini C, Parson H. Diabetic neuropathy. Endocrinol Metab Clin North Am. 2013;42(4):747–787. doi: 10.1016/j.ecl.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 4.Kayama Y, Raaz U, Jagger A, Adam M, Schellinger IN, Sakamoto M, Suzuki H, Toyama K, Spin JM, Tsao PS. Diabetic cardiovascular disease induced by oxidative stress. Int J Mol Sci. 2015;16(10):25234–25263. doi: 10.3390/ijms161025234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yamagishi S, Imaizumi T. Diabetic vascular complications: pathophysiology, biochemical basis and potential therapeutic strategy. Curr Pharm Des. 2005;11(18):2279–2299. doi: 10.2174/1381612054367300. [DOI] [PubMed] [Google Scholar]
- 6.Hammes HP. Diabetic retinopathy: hyperglycaemia, oxidative stress and beyond. Diabetologia. 2018;61(1):29–38. doi: 10.1007/s00125-017-4435-8. [DOI] [PubMed] [Google Scholar]
- 7.Wang LZ, Cheung CY, Tapp RJ, Hamzah H, Tan G, Ting D, Lamoureux E, Wong TY. Availability and variability in guidelines on diabetic retinopathy screening in Asian countries. Br J Ophthalmol. 2017;101(10):1352–1360. doi: 10.1136/bjophthalmol-2016-310002. [DOI] [PubMed] [Google Scholar]
- 8.Huang OS, Tay WT, Ong PG, Sabanayagam C, Cheng CY, Tan GS, Cheung GC, Lamoureux EL, Wong TY. Prevalence and determinants of undiagnosed diabetic retinopathy and vision-threatening retinopathy in a multiethnic Asian cohort: the Singapore Epidemiology of Eye Diseases (SEED) study. Br J Ophthalmol. 2015;99(12):1614–1621. doi: 10.1136/bjophthalmol-2014-306492. [DOI] [PubMed] [Google Scholar]
- 9.Thomas RL, Distiller L, Luzio SD, Chowdhury SR, Melville VJ, Kramer B, Owens DR. Ethnic differences in the prevalence of diabetic retinopathy in persons with diabetes when first presenting at a diabetes clinic in South Africa. Diabetes Care. 2013;36(2):336–341. doi: 10.2337/dc12-0683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stolk RP, van Schooneveld MJ, Cruickshank JK, Hughes AD, Stanton A, Lu JM, Patel A, Thom SA, Grobbee DE, Vingerling JR, AdRem Project Team and ADVANCE Management Committee Retinal vascular lesions in patients of Caucasian and Asian origin with type 2 diabetes: baseline results from the ADVANCE Retinal Measurements (AdRem) study. Diabetes Care. 2008;31(4):708–713. doi: 10.2337/dc07-1657. [DOI] [PubMed] [Google Scholar]
- 11.Liu L, Wu XM, Liu LM, Geng J, Yuan Z, Shan ZY, Chen L. Prevalence of diabetic retinopathy in mainland China: a meta-analysis. PLoS One. 2012;7(9):e45264. doi: 10.1371/journal.pone.0045264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maroufizadeh S, Almasi-Hashiani A, Hosseini M, Sepidarkish M, Omani Samani R. Prevalence of diabetic retinopathy in Iran: a systematic review and Meta-analysis. Int J Ophthalmol. 2017;10(5):782–789. doi: 10.18240/ijo.2017.05.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 14.Huang OS, Lamoureux EL, Tay WT, Tai ES, Wang JJ, Wong TY. Glycemic and blood pressure control in an Asian malay population with diabetes and diabetic retinopathy. Arch Ophthalmol. 2010;128(9):1185–1190. doi: 10.1001/archophthalmol.2010.168. [DOI] [PubMed] [Google Scholar]
- 15.Pan CY, Ho LT, Soegondo S, Prodjosudjadi W, Suwanwalaikorn S, Lim SC, Chan TM, Chow KW, Thoenes M, Choi DS, DEMAND Study Investigators Prevalence of albuminuria and cardiovascular risk profile in a referred cohort of patients with type 2 diabetes: an Asian perspective. Diabetes Technol Ther. 2008;10(5):397–403. doi: 10.1089/dia.2007.0296. [DOI] [PubMed] [Google Scholar]
- 16.Kumaramanickavel G, Sripriya S, Vellanki RN, Upadyay NK, Badrinath SS, Arokiasamy T, Sukumar B, Vidhya A, Joseph B, Sharma T, Gopal L. Tumor necrosis factor allelic polymorphism with diabetic retinopathy in India. Diabetes Res Clin Pract. 2001;54(2):89–94. doi: 10.1016/s0168-8227(01)00269-8. [DOI] [PubMed] [Google Scholar]
- 17.Das BN, Thompson JR, Patel R, Rosenthal AR. The prevalence of eye disease in Leicester: a comparison of adults of Asian and European descent. J R Soc Med. 1994;87(4):219–222. [PMC free article] [PubMed] [Google Scholar]
- 18.Raymond NT, Varadhan L, Reynold DR, Bush K, Sankaranarayanan S, Bellary S, Barnett AH, Kumar S, O'Hare JP, UK Asian Diabetes Study Retinopathy Study Group Higher prevalence of retinopathy in diabetic patients of South Asian ethnicity compared with white Europeans in the community: a cross-sectional study. Diabetes Care. 2009;32(3):410–415. doi: 10.2337/dc08-1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dowse GK, Humphrey AR, Collins VR, Plehwe W, Gareeboo H, Fareed D, Hemraj F, Taylor HR, Tuomilehto J, Alberti KG, Zimmet PZ. Prevalence and risk factors for diabetic retinopathy in the multiethnic population of Mauritius. Am J Epidemiol. 1998;147(5):448–457. doi: 10.1093/oxfordjournals.aje.a009470. [DOI] [PubMed] [Google Scholar]
- 20.Cheung CY, Sabanayagam C, Law AK, Kumari N, Ting DS, Tan G, Mitchell P, Cheng CY, Wong TY. Retinal vascular geometry and 6 year incidence and progression of diabetic retinopathy. Diabetologia. 2017;60(9):1770–1781. doi: 10.1007/s00125-017-4333-0. [DOI] [PubMed] [Google Scholar]
- 21.Wong CW, Lamoureux EL, Cheng CY, Cheung GC, Tai ES, Wong TY, Sabanayagam C. Increased burden of vision impairment and eye diseases in persons with chronic kidney disease - a population-based study. EBioMedicine. 2016;5:193–197. doi: 10.1016/j.ebiom.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sabanayagam C, Khoo EY, Lye WK, Ikram MK, Lamoureux EL, Cheng CY, Tan ML, Salim A, Lee J, Lim SC, Tavintharan S, Thai AC, Heng D, Ma S, Tai ES, Wong TY. Diagnosis of diabetes mellitus using HbA1c in Asians: relationship between HbA1c and retinopathy in a multiethnic Asian population. J Clin Endocrinol Metab. 2015;100(2):689–696. doi: 10.1210/jc.2014-2498. [DOI] [PubMed] [Google Scholar]
- 23.Rooney D, Lye WK, Tan G, Lamoureux EL, Ikram MK, Cheng CY, Kumari N, Zheng YF, Mitchell P, Wang JJ, Wong TY, Sabanayagam C. Body mass index and retinopathy in Asian populations with diabetes mellitus. Acta Diabetol. 2015;52(1):73–80. doi: 10.1007/s00592-014-0602-2. [DOI] [PubMed] [Google Scholar]
- 24.Pradeepa R, Surendar J, Indulekha K, Chella S, Anjana RM, Mohan V. Relationship of diabetic retinopathy with coronary artery disease in Asian Indians with type 2 diabetes: the Chennai Urban Rural Epidemiology Study (CURES) Eye Study: 3. Diabetes Technol Ther. 2015;17(2):112–118. doi: 10.1089/dia.2014.0141. [DOI] [PubMed] [Google Scholar]
- 25.Rajalakshmi R, Amutha A, Ranjani H, Ali MK, Unnikrishnan R, Anjana RM, Narayan KM, Mohan V. Prevalence and risk factors for diabetic retinopathy in Asian Indians with young onset type 1 and type 2 diabetes. J Diabetes Complicat. 2014;28(3):291–297. doi: 10.1016/j.jdiacomp.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 26.Cheema BS, kohli HS, Sharma R, Bhansali A, Khullar M. Endothelial nitric oxide synthase gene polymorphism and type 2 diabetic retinopathy among Asian Indians. Acta Diabetol. 2012;49(6):481–488. doi: 10.1007/s00592-012-0437-7. [DOI] [PubMed] [Google Scholar]
- 27.Zheng YF, Lamoureux EL, Ikram MK, Mitchell P, Wang JJ, Younan C, Anuar AR, Tai ES, Wong TY. Impact of migration and acculturation on prevalence of type 2 diabetes and related eye complications in Indians living in a newly urbanised society. PLoS One. 2012;7(4):e34829. doi: 10.1371/journal.pone.0034829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zheng YF, Lamoureux EL, Chiang PC, Anuar AR, Ding J, Wang JJ, Mitchell P, Tai ES, Wong TY. Language barrier and its relationship to diabetes and diabetic retinopathy. BMC Public Health. 2012;12:781. doi: 10.1186/1471-2458-12-781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim JH, Kwon HS, Park YM, Lee JH, Kim MS, Yoon KH, Lee WC, Cha BY, Son HY. Prevalence and associated factors of diabetic retinopathy in rural Korea: the Chungju metabolic disease cohort study. J Korean Med Sci. 2011;26(8):1068–1073. doi: 10.3346/jkms.2011.26.8.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.An JH, Cho YM, Yu HG, Jang HC, Park KS, Kim SY, Lee HK. The clinical characteristics of normoalbuminuric renal insufficiency in Korean type 2 diabetic patients: a possible early stage renal complication. J Korean Med Sci. 2009;24(Suppl):S75–S81. doi: 10.3346/jkms.2009.24.S1.S75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong TY, Cheung N, Tay WT, Wang JJ, Aung T, Saw SM, Lim SC, Tai ES, Mitchell P. Prevalence and risk factors for diabetic retinopathy: the Singapore Malay Eye Study. Ophthalmology. 2008;115(11):1869–1875. doi: 10.1016/j.ophtha.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 32.Chang C, Lu F, Yang YC, Wu JS, Wu TJ, Chen MS, Chuang LM, Tai TY. Epidemiologic study of type 2 diabetes in Taiwan. Diabetes Res Clin Pract. 2000;50(Suppl 2):S49–S59. doi: 10.1016/s0168-8227(00)00179-0. [DOI] [PubMed] [Google Scholar]
- 33.Hu YH, Pan XR, Liu PA, Li GW, Howard BV, Bennett PH. Coronary heart disease and diabetic retinopathy in newly diagnosed diabetes in Da Qing, China: the Da Qing IGT and Diabetes Study. Acta Diabetol. 1991;28(2):169–173. doi: 10.1007/BF00579721. [DOI] [PubMed] [Google Scholar]
- 34.He S, Guo Y, Li Z. Epidemiologic study of diabetic retinopathy in Capital Steel Company. Zhonghua Yan Ke Za Zhi. 1997;33(5):381–383. [PubMed] [Google Scholar]
- 35.Li SL, Zhou YF, Chen D, Yang MG, Zhu ML. Epidemiological investigation of diabetic retinopathy risk factors. Chin J Ocul Fundus Dis. 1998;14:119–121. [Google Scholar]
- 36.Wang GL, Zhang F, Yuan SY, et al. et al. A screening survey of diabetic retinopathy and other chronic complications in beijing district. Ophthalmology In China. 2001;10:180–182. [Google Scholar]
- 37.Zou HD, Zhang X, Zhu JF, et al. et al. Epidemiological investigation of diabetic retinopathy in Beixinjing blocks, Shanghai. Chin J Ocul Fundus Dis. 2006;22:31–34. [Google Scholar]
- 38.Liang XJ, Lin JJ, Huang Z, Li GP, Wu XY. Prevalence and risk factors of diabetic retinopathy in foshan city. Guangdong Medical Journal. 2006;27:1552–1553. [Google Scholar]
- 39.Xie XW, Xu L, Yang H, Wang S, Jonas JB. Frequency of diabetic retinopathy in the adult population in China: the Beijing Eye Study 2001. Int Ophthalmol. 2009;29(6):485–493. doi: 10.1007/s10792-008-9272-9. [DOI] [PubMed] [Google Scholar]
- 40.Liu L, Chen L, Hu YD, Liu LM. Analysis risk factors for diabetic retinopathy. Shandong Medical Journal. 2009;49:52–53. [Google Scholar]
- 41.Shu XW, Wang Y, Fan CF, Sheng YJ, Zhang H, Wu CL. Epidemiology study on the prevalence rate and risk factors of diabetic retinopathy in rural residents in shandong. Chin J Ocul Fundus Dis. 2010;26:113–115. [Google Scholar]
- 42.Ye XQ. The analysis about epidemiological survey of diabetic retinopathy in huizhou city. Guide of China Medicine. 2010;8:27–28. [Google Scholar]
- 43.Teng Y, Cui H, Zhang QS, Teng YF, Su Y, Yang MM, Yu XH. Prevalence of diabetic retinopathy among the elderly in rural southern Shuangcheng City, Heilongjiang Province. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31(8):856–859. [PubMed] [Google Scholar]
- 44.Dong HL. Screening procession for diabetic retinopathy for Shunyi district Houshayu valley residents. Medical Information. 2010;10:2701–2702. [Google Scholar]
- 45.Yang MZ, Wei SQ. Early detection for diabetic retinopathy in grassroots community and results analysis. Hebei Medical Journal. 2010;32:844–845. [Google Scholar]
- 46.Wang HB, Sun FX, Zhang Q, Zhai M, Wang SF, Lu H. Epidemiologic study on the prevalence rate and risk factors of diabetic retinopathy in eastern countryside of Changzhi. Chin J Ocul Fundus Dis. 2010;26:109–112. [Google Scholar]
- 47.Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, Chen SJ, Dekker JM, Fletcher A, Grauslund J, Haffner S, Hamman RF, Ikram MK, Kayama T, Klein BE, Klein R, Krishnaiah S, Mayurasakorn K, O'Hare JP, Orchard TJ, Porta M, Rema MH, Roy MS, Sharma T, Shaw J, Taylor H, Tielsch JM, Varma R, Wang JJ, Wang NL, West S, Xu L, Yasuda M, Zhang XZ, Mitchell P, Wong TY, Meta-Analysis for Eye Disease (META-EYE) Study Group Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–564. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang FH, Liang YB, Peng XY, Wang JJ, Zhang F, Wei WB, Sun LP, Friedman DS, Wang NL, Wong TY, Handan Eye Study Group Risk factors for diabetic retinopathy in a rural Chinese population with type 2 diabetes: the Handan Eye Study. Acta Ophthalmol. 2011;89(4):e336–e343. doi: 10.1111/j.1755-3768.2010.02062.x. [DOI] [PubMed] [Google Scholar]
- 49.Li BZ, Liu YL, Han L, et al. et al. Epidemiological survey of diabetic retinopathy in shunyi district of beijing. Chin J Exp Ophthalmol. 2011;29:747–752. [Google Scholar]
- 50.Pang C, Jia LL, Jiang SF, Liu W, Hou XH, Zuo YH, Gu HL, Bao YQ, Wu Q, Xiang KS, Gao X, Jia WP. Determination of diabetic retinopathy prevalence and associated risk factors in Chinese diabetic and pre-diabetic subjects: Shanghai diabetic complications study. Diabetes Metab Res Rev. 2012;28(3):276–283. doi: 10.1002/dmrr.1307. [DOI] [PubMed] [Google Scholar]
- 51.Rema MH, Mohan V, Deepa R, Ravikumar R, Chennai Urban Rural Epidemiology Study-2 Association of carotid intima-media thickness and arterial stiffness with diabetic retinopathy: the Chennai Urban Rural Epidemiology Study (CURES-2) Diabetes Care. 2004;27(8):1962–1967. doi: 10.2337/diacare.27.8.1962. [DOI] [PubMed] [Google Scholar]
- 52.Pang C, Jia LL, Jiang SF, Liu W, Hou XH, Zuo YH, Gu HL, Bao YQ, Wu Q, Xiang KS, Gao X, Jia WP. Determination of diabetic retinopathy prevalence and associated risk factors in Chinese diabetic and pre-diabetic subjects: Shanghai diabetic complications study. Diabetes Metab Res Rev. 2012;28(3):276–283. doi: 10.1002/dmrr.1307. [DOI] [PubMed] [Google Scholar]
- 53.Zaghloul H, Pallayova M, Al-Nuaimi O, Hovis KR, Taheri S. Association between diabetes mellitus and olfactory dysfunction: current perspectives and future directions. Diabet Med. 2018;35(1):41–52. doi: 10.1111/dme.13542. [DOI] [PubMed] [Google Scholar]
- 54.Jin PY, Peng JJ, Zou HD, Wang WW, Fu J, Shen BJ, Bai XL, Xu X, Zhang X. A five-year prospective study of diabetic retinopathy progression in Chinese type 2 diabetes patients with “well-controlled” blood glucose. PLoS One. 2015;10(4):e0123449. doi: 10.1371/journal.pone.0123449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Askew DA, Crossland L, Ware RS, Begg S, Cranstoun P, Mitchell P, Jackson CL. Diabetic retinopathy screening and monitoring of early stage disease in general practice: design and methods. Contemp Clin Trials. 2012;33(5):969–975. doi: 10.1016/j.cct.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 56.Tan GS, Gan A, Sabanayagam C, Tham YC, Neelam K, Mitchell P, Wang JJ, Lamoureux EL, Cheng CY, Wong TY. Ethnic differences in the prevalence and risk factors of diabetic retinopathy: the singapore epidemiology of eye diseases study. Ophthalmology. 2018;125(4):529–536. doi: 10.1016/j.ophtha.2017.10.026. [DOI] [PubMed] [Google Scholar]
- 57.Panagiotoglou T, Tsilimbaris M, Ginis H, Karyotakis N, Georgiou V, Koutentakis P, Pallikaris I. Ocular rigidity and outflow facility in nonproliferative diabetic retinopathy. J Diabetes Res. 2015;2015:141598. doi: 10.1155/2015/141598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sivaprasad S, Gupta B, Crosby-Nwaobi R, Evans J. Prevalence of diabetic retinopathy in various ethnic groups: a worldwide perspective. Surv Ophthalmol. 2012;57(4):347–370. doi: 10.1016/j.survophthal.2012.01.004. [DOI] [PubMed] [Google Scholar]