Version Changes
Revised. Amendments from Version 1
A number of specific edits have been made following the suggestions of the reviewers (detailed in the response to reviewers section). In addition, we have added a new paragraphs detailing:
Further information on the data sources used to calculate peak HIV prevalence
How the network-connectivity theory conceptualizes the relationship between race, ethnicity and STIs.
Additional limitations of the paper relating to how we mention the importance of, but do not go into detail as to the importance of upstream determinants of STI transmission
The legend for Figure 2 has been expanded
Abstract
There is little consensus as to why sexually transmitted infections (STIs), including HIV and bacterial vaginosis (BV) are more prevalent in some populations than others. Using a broad definition of sexual network connectivity that includes both structural and conductivity-related factors, we argue that the available evidence suggests that high prevalence of traditional STIs, HIV and BV can be parsimoniously explained by these populations having more connected sexual networks. Positive feedback, whereby BV and various STIs enhance the spread of other STIs, then further accentuates the spread of BV, HIV and other STIs. We review evidence that support this hypothesis and end by suggesting study designs that could further evaluate the hypothesis, as well as implications of this hypothesis for the prevention and management of STIs.
Keywords: HIV, STI, bacterial vaginosis, sexual network connectivity, concurrency
Introduction
There is little consensus as to why the prevalence of bacterial vaginosis (BV), HIV and other sexually transmitted infections (STIs) varies so dramatically around the world. A range of explanations have been put forward, including variation in circumcision prevalence 1, STI treatment efficacy 2, poverty 2– 4, socioeconomic inequality 5, gender inequality 6, migration intensity 7, hormonal contraception 8, vaginal microbiome 9, host genetic susceptibility 10 and sexual behavior 11, 12. We do not dispute that each of these can play a role in differential STI spread. Rather we argue that differential connectivity of sexual networks emerges as a parsimonious dominant explanation for the global variation in STI prevalence, taking a central position in the causal pathway that links all of the above-mentioned risk factors for STI infection ( Figure 1).
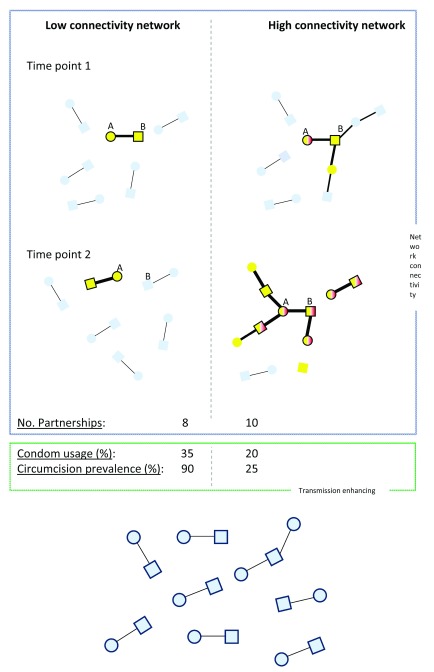
Figure 1. Schematic comparison of STI spread in a low (left) and high (right) sexual network connectivity populations soon after sexual debut.
In both populations, STI acquisition commences when ‘A’ has sex with an older man and acquires BV-associated bacteria (yellow) and HSV-2 (black border around each node). In the high connectivity population ‘A’ also acquires T. vaginalis (TV; red) from this relationship. The major determinant of the difference in network connectivity is that more relationships run concurrently in the high connectivity population. This facilitates STI spread by: i) Creating a larger reachable path for STIs 13, ii) Removing the benefits of partner sequencing seen in serial monogamy (for details see 21), iii) Reducing the time between STI transmissions since infections are not trapped in dyads 21 and iv) Bypassing the rapid-clearance-in-males-buffer 31, 32. This is the buffer that reduces STI spread in serial monogamous networks where the gap between partnerships (time points 1 and 2) is longer than the duration of colonization of TV and BV-associated bacteria in men. This gap protects the women at time point 2 in the serial monogamy/low connectivity population (represented by the partner of B at time point 2) but not in the high connectivity population from BV and TV acquisition. Various STIs, including HSV-2, BV and TV enhance the susceptibility/infectiousness of other STIs, leading to positive feedback loops. This is conveyed via the transmission probabilities being depicted as proportional to edge width. The high connectivity network also has a low prevalence of circumcision and condom usage which further increase STI transmission probabilities in this population. The combination of high network connectivity, low circumcision/condom-use lead to a rapid spread of multiple STIs in the high- but not the low-connectivity network (blue nodes, no STIs; squares, men; circles, women).
Outline and origins of the network connectivity theory
STIs are transmitted along sexual networks and, as a result, the structural characteristics of these networks determine the speed and extent of STI spread 13– 15. These structural characteristics include summary measures of the number of partners per unit time, coital frequency, prevalence of concurrent partnering (having two or more partners at the same time), size of core groups (and their connections with non-core populations), type of sex, size of sexual network, length of gaps between partnerships and degree/type of homophily 13, 15– 20 (reviewed in 21). These structural factors determine the forward reachable path of a network, which is defined as the cumulative set of individuals in a population that can be infected with an STI from an initial seed via a path of temporally ordered partnerships 22. Two particularly important determinants of the forward reachable path are the prevalence of concurrency and the number of partners per unit time 22.
STI transmission can also be enhanced through a sexual network by factors that enhance the conductivity or probability of STI transmission per sex act. These factors include a low prevalence of circumcision, pre-exposure prophylaxis (PrEP) and condom usage ( Figure 1 and Figure 2). Enhanced screening/early and effective treatment of STIs could reduce spread of STIs via reducing the duration of infectivity. Because numerous STIs enhance the transmission/acquisition of other STIs 23, effective STI control could then also reduce the conductivity of a network. We use a broad definition of network connectivity in this paper that includes both these structural and conductivity-related factors.
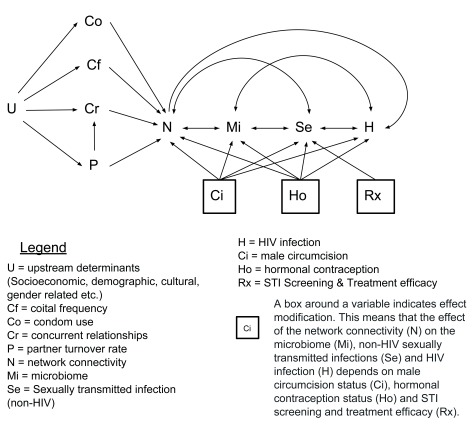
Figure 2. Conceptual framework for the understanding the genesis of differences in STI prevalence between populations.
Note that we use directed cyclic graphs as short-hand notation for an infinite acyclic directed graph containing variables indexed by time. Our definition of network connectivity is broad: in addition to considering the sexual links between individuals, it takes into account the “conductivity” and timing of these links.
The origins of this network connectivity theory lie in the STI modeling field. Previous modelling studies from the 1970s established the importance of the rate of partner change and mixing between core and non-core groups to STI spread 24, 25. Seminal modelling papers by Morris et al. 13 and Watts et al. 15 in the 1990s built on these findings by revealing that the prevalence of sexual partner concurrency may be a particularly important determinant of network connectivity. Their analyses found that relatively small increases in concurrency could lead to dramatic increases in network connectivity and as a result, HIV spread 13. The main mechanisms whereby concurrency promotes STI spread are illustrated in Figure 1. A number of empirical studies have subsequently established that markers of network connectivity such as concurrency and rate of partner change are correlated with the prevalence of all major STIs ( Table 1). In this paper, we review some of the cross sectional and longitudinal evidence that two components of network connectivity (concurrency and rate of partner change) are associated with STI prevalence. We then summarize evidence that network connectivity influences the prevalence of BV and end by noting the potential for positive feedback loops between various STIs being underpinned by network connectivity.
Table 1. A non-exhaustive tabulation of studies that have found number of partners and partner concurrency to be positively associated with various sexually transmitted infections (STIs).
Studies that found no association are not included.
| STI | No. sex partners | Concurrency prevalence | ||
|---|---|---|---|---|
| Individual level | Population level | Individual level | Population level | |
| BV | [ 33] | NA | [ 31] | [ 34] |
| Chlamydia | [ 35, 36] | [ 35] | [ 18, 36, 37] | NA |
| Gonorrhoea | [ 38] | NA | [ 39] | NA |
| HIV | [ 40, 41] | [ 42– 44] | [ 45– 47] | [ 48– 50] |
| HSV-2 | [ 51, 52] | NA | [ 52] | [ 53] |
| HPV | [ 54, 55] | NA | [ 56] | NA |
| Syphilis | [ 35] | NA | [ 57] | [ 58] |
| Trichomoniasis | [ 37, 59] | NA | [ 32, 37] | [ 60] |
No. of sex partners refers to number of partners over lifetime or over past year. Concurrency refers to the prevalence of concurrency (male, female or combined) for the population level studies and partner concurrency in the individual level studies. NA, not available/no studies found that evaluated this association.
Markers of network connectivity are correlated with the prevalence of STIs: cross-sectional evidence
a. Ethnic group comparative analyses
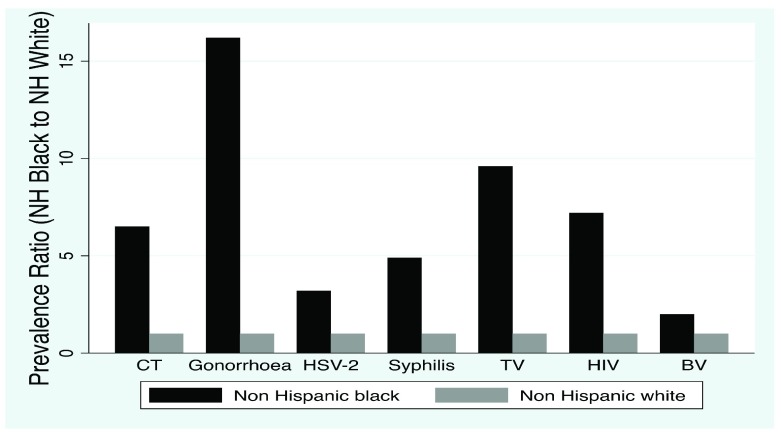
USA: In the United States the prevalence of BV, HIV and most STIs for non-Hispanic blacks in the 1990s was considerably higher than in non-Hispanic whites ( Figure 3). Historical data is limited but the available data demonstrates that these divergences in prevalence extend back to the 1930s for syphilis 26, 27 and the 1970s for HSV-2 28. Morris et al. used five large national behavioural surveys to investigate which possible risk factors could underpin these differences in HIV prevalence, and found that the prevalence of concurrency was on average 3.5 and 2.1 times higher in non-Hispanic black men and women, respectively. In their modelling analysis, they found that these differences in concurrency prevalence between these groups translated into 2.6-fold differences in HIV prevalence. They did not, however, model the enhanced transmission probability that is associated with acute HIV which subsequent analyses have shown to have a synergistic effect with concurrency on HIV transmission 29. Subsequent studies have demonstrated that concurrency plays an important role in the spread of the other STIs and thus the differential concurrency prevalence they found could represent a parsimonious explanation for the differences in the range of STI prevalence demonstrated in Figure 3.
Figure 3. Estimated prevalence ratio of HIV and other sexually transmitted infections in non-Hispanic Blacks versus non-Hispanic Whites in the United States National Health and Nutrition Examination Survey 2003–2004.
Southern Africa: The HIV prevalence varies 40-fold between ethnic groups in South Africa 30. Analyses from 5 nationally representative behavioural surveys revealed that the most plausible risk factors that could explain this were the 5- to 17-fold higher prevalence of male concurrency and the higher number of partners per year in the highest compared to the lowest HIV prevalence ethnic group 30. A modelling study likewise demonstrated that the combination of concurrency and rate of partner change was responsible for approximately 75% of the HIV infections in the 1990s when antenatal HIV prevalence increased from 0.7% to 24.5% 62. In a similar vein, modelling studies from Zimbabwe found that both the observed high prevalence of concurrency and the increased transmission probability associated with acute HIV were needed to replicate Zimbabwe's explosive HIV epidemic curve 29.
Elsewhere: The prevalence of concurrency and/or number of partners have also been found to be associated with variations in HIV prevalence by ethnic group in Ethiopia 43, Honduras 63, Kenya 64, Uganda 65 and the United Kingdom 66– 68. Although no published study has assessed how generalizable these findings are globally, one study attempted to do this within sub-Saharan African countries. This study used demographic and health surveys to systematically assess the behavioural correlates of HIV prevalence by region (as a proxy for ethnic group) in 47 surveys from 27 African countries where HIV prevalence varied by at least two-fold between regions. It found that the lifetime number of partners reported by men and women was positively correlated with HIV prevalence in 23 and 18 out of 36 surveys, respectively. Likewise, reporting sex with a non-marital, non-cohabiting partner by men and women was positively correlated with HIV prevalence in 38 and 39 out of 47 surveys, respectively 69.
The relationship between ethnicity, race and STI prevalence
It is of paramount importance to emphasize that our hypothesis makes no reference to race. The hypothesis proposes that there are differences in sexual behavior between different groups of people which translate into differences in network connectivity and as a result differential STI prevalence. These groups can be defined by sexual orientation, ethnicity, social class, caste or whatever categories meaningfully segregate sexual networks. These categories are social constructs and thus vary considerably across time and place. It is our considered opinion that investigators who conduct investigations into STI epidemiology usingthese categories do so with sufficient sensitivity to the concerns as to how these categories are and have been used and abused.
Other authors have hypothesized that biological differences between racial groups play an important role in STI epidemiology. A recent form of this argument is that ‘black populations’ are innately more likely to have bacterial-vaginosis-type vaginal microbiomes which in turn facilitates the transmission of various STIs in this population 9. We and others have argued that the evidence does not support this, and other race-based explanations of differential STI spread 70, 71. As an example, we noted that ‘black populations’ with evidence of low sexual network connectivity have a very low prevalence of BV and conversely ‘white populations’ with high connectivity had a high BV prevalence 70, 71.
b. Country level comparisons
In the country level analysis we focus on studies that investigate the correlates of country level peak HIV prevalence. Peak HIV prevalence, which represents the maximal HIV prevalence that countries obtained prior to the widespread availability of antiretroviral therapy is a useful composite measure of the factors that enabled the rapid spread of HIV 72. Peak HIV prevalence is based on generally high quality data on HIV prevalence around the world. National HIV prevalence estimates are frequently based on nationally representative serosurveys and other sources such as antenatal surveys that involve sample sizes of up to 216,703 individuals 73– 75. Nationally representative, HIV serolinked, demographic health surveys are one example of this. MeasureDHS provides open-access to 72 such surveys from 37 countries ( https://dhsprogramme.com). As such, peak HIV prevalence offers a useful outcome measure to assess what the correlates of rapid and extensive HIV transmission are 72. Studies have shown that peak HIV prevalence is not associated with a number of risk factors widely believed to be important for HIV spread: poverty, socioeconomic inequality, gender inequality, prevalence of migration and STI treatment efficacy 6, 11, 76, 77. These findings are of considerable consequence. Many authors have claimed that STIs are diseases of poverty 2– 4. Studies from Africa and elsewhere suggest that this is far from universally the case. Using HIV-serolinked and nationally representative survey data from eight countries in sub-Saharan Africa, Mishra et al., for example, established that HIV prevalence increased monotonically with wealth quintile for both men and women 78. This finding has since been confirmed in 19 other countries 40.
Only two risk factors have been consistently found to be associated with peak HIV prevalence: circumcision and the prevalence of concurrency.
i. Circumcision: There is a strong negative association between circumcision and peak HIV prevalence within sub-Saharan Africa, but not globally 11, 77. This is unsurprising since sub-Saharan Africa has the highest prevalence of HIV and the second highest prevalence of circumcision in the world 77, 79. The vast majority of the world’s population lives in countries with both low HIV and low circumcision prevalence 11. Various lines of evidence suggest that something else is driving the spread of HIV in sub-Saharan Africa and that circumcision is then moderating this risk 77, 80.
ii. Concurrency prevalence: The prevalence of male concurrency has been found to be associated with peak HIV prevalence in a cross country study 48. Other studies have however failed to find this association 81, 82 but serious methodological questions have been raised pertaining to these studies including the fact one of these studies compared 5 year cumulative concurrency rates from European countries with point prevalence of concurrency in African countries 48, 81, 83. A further problem related to these cross-national comparisons is that national populations are frequently composed of multiple subpopulations that may have large differences in HIV prevalence. In 29 sub-Saharan countries with available data, for example, HIV prevalence was found to vary by a median of 3.7-fold (IQR 2.9-7.9) between regions within countries 69. As argued above, more fine-grained studies investigating the correlates of HIV prevalence by ethnic group or region within these and other countries have found a range of markers of network connectivity (such as partner number and concurrency) and other risk factors to be associated with HIV prevalence 12, 43, 65, 66.
c. Men who have sex with men (MSM) vs. heterosexual comparison
A number of high-income countries are experiencing epidemics of a range of STIs that are disproportionately affecting MSM 84. In the year 2014 in London, for example, MSM who comprised only 2% of the population, contributed a disproportionate number of diagnoses of STIs (23%/63%/69%/90% of all new chlamydia/HIV/gonorrhoea/syphilis, respectively) 85. Lymphogranuloma venereum (LGV) and sexually transmitted hepatitis C have also been noted to disproportionately affect MSM in contemporary outbreaks in high-income countries 84, 86. A parsimonious explanation for this clustering of STIs in MSM is a combination of behavioural factors including number of sex partners and partner concurrency 86, 87. In the United Kingdom, MSM in 2012 reported a median (interquartile range) of 5 (2–30) partners in the past 5 years versus 1 (1–3) reported by heterosexual men 88; likewise, the proportions reporting concurrency in the prior 5 years were 52% and 15% for these two groups, respectively 88.
Markers of network connectivity are correlated with the incidence of STIs: longitudinal evidence
In this section, we consider two (of many possible) examples where large changes in STI incidence are preceded by corresponding changes in network connectivity.
a) Incidence of primary/secondary syphilis in MSM in the USA 1963 to 2013.
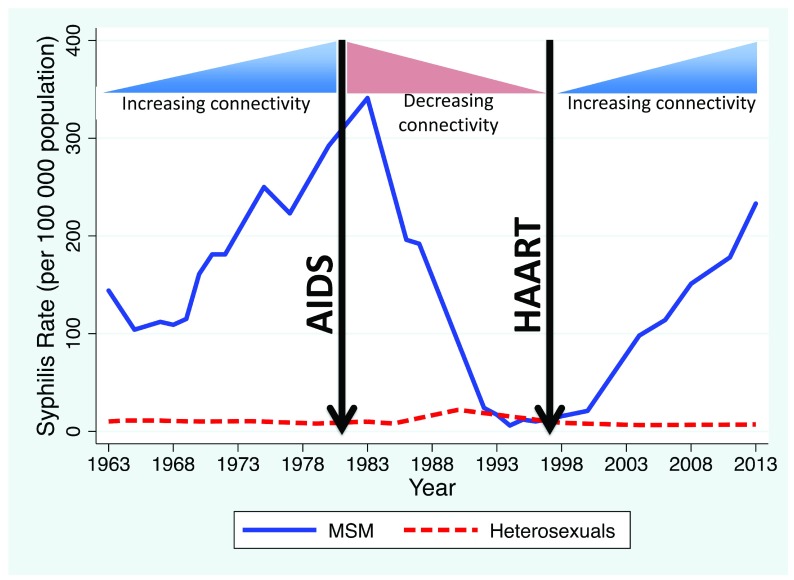
In their review of syphilis epidemiology in the United States 1963 to 2013, Peterman et al., found evidence of an initial dramatic increase in primary/secondary syphilis in MSM between 1963 and 1982 followed by a steep decline to close to zero cases in 1994 and a subsequent increase to 228/100,000 in 2013 ( Figure 4) 89. Increases in multiple partnering were thought to underpin the initial increase 89– 92. The AIDS epidemic in the 1980s led to reductions in network connectivity via both behaviour change and deaths of individuals (from AIDS) centrally placed in sexual networks 89, 93. The arrival of effective antiretroviral therapy from 1996 onwards played an important role in the increases in rates of partner change and reductions in condom usage 89, 94 noted during the ongoing epidemic of syphilis in this population. Although this evidence is indirect and susceptible to confounding, it is at least suggestive that the two large increases and one precipitous decline in syphilis incidence were determined to some extent by corresponding changes in network connectivity. Of note, this epidemic trajectory of syphilis in MSM in the United States was similar to that of a range of other STIs such as LGV and gonorrhoea in this same population and in MSM in other high income countries 84. In a range of European countries where MSM were similarly affected by the AIDS epidemic, the incidence of STIs such as syphilis, LGV and gonorrhoea declined to very low rates in the post AIDS period before large increases in the late 1990s onwards corresponding to increases in partner number and declines in condom usage 84.
Figure 4. Fluctuations in estimated annual rate of primary/secondary syphilis among men who have sex with men (MSM) and men who have sex with women only (MSW) in the USA, 1963–2013 (Modified from 89).
Also shown is how these were temporally associated with changes in network connectivity represented schematically.
b) Southern and Eastern Africa
A number of studies from general populations in Southern and Eastern Africa have concluded that reductions in partner number and concurrency played an important role in the impressive declines in HIV incidence in Uganda, Zimbabwe and other countries in the region 95– 100. Delayed sexual debut, increased condom usage, enhanced antiretroviral therapy coverage and AIDS mortality (via reduced network connectivity) also played an important role in this regard 96, 100, 101.
Clustering of STIs includes incurable STIs and network connectivity is the most parsimonious way to explain this clustering
We have already noted the striking clustering of STIs within certain ethnic groups and sexual orientations in a number of countries. Strong evidence of clustering of STIs has also been found at WHO world regional 102 and country levels. At a country level, the peak HIV prevalence has been found to be associated with the prevalence of a range of STIs before/early in the HIV epidemics: syphilis 103, gonorrhoea 104, HSV-2 103 and trichomoniasis 104 and BV 104.
This clustering of STIs is important for two reasons. Firstly, it suggests that one or more common risk factors could underpin variations in all these STIs. Secondly, the treatable but incurable STI, HSV-2 is correlated with both peak HIV prevalence 103 and antenatal syphilis prevalence from the pre-HIV period 66. This is relevant because differential STI treatment efficacy can explain differences in the prevalence of treatable STIs such as syphilis but not HSV-2. Differential network connectivity, which can explain the differential spread of all STIs, is thus a more parsimonious way to explain the clustering of STIs.
Network connectivity is also a risk factor for BV
Recent couple studies have demonstrated that the consortia of bacteria that constitute the dysbiosis, BV are sexually transmitted 105– 111. BV is strongly associated with number of sexual partners and reporting partner concurrency at an individual level 31, 33, 112, 113. An ecological study found associations at the level of countries between the prevalence of male concurrency and the prevalence of BV 34. The same association was also found at the level of ethnic groups within countries 34.
Populations with high network connectivity are thus likely to have a high prevalence of BV which in addition to the adverse clinical effects of BV 114, is important because of the positive feedback cycles between BV and the traditional STIs. BV for example has been shown to enhance susceptibility to chlamydia 115, 116, gonorrhoea 115, HIV 117, 118, HSV-2 119, 120 and TV 115, 116, 121. HSV-2 and TV have in turn been shown to increase the risk for acquisition of BV and other STIs 115– 117, 122. A more detailed review of the evidence linking BV prevalence to network connectivity is provided in 71.
Previous modelling studies have found that relatively small increases in parameters of network connectivity can lead to non-linear increases in HIV/STI spread 13. If this applies to BV as well, then more connected sexual networks would be expected to facilitate the rapid spread of BV and the various STIs soon after sexual debut. These would then increase susceptibility and transmission of other STIs, adding a further means by which enhanced network connectivity could lead to increases in STI spread. Network connectivity would thus indirectly enhance probability of transmission per sex act for different STIs ( Figure 1).
Limitations
It should be emphasized that this paper presents a narrative, non-systematic review of evidence for network connectivity as a parsimonious explanation of variations in genital microbiomes and STI prevalence. As such, our sampling of evidence is likely biased. We acknowledge that we have picked evidence that is supportive of our hypothesis. Our definition of network connectivity could also be criticized as being impractical because it includes such a breadth of structural and conductivity variables. Consequently, in our conceptual framework of network connectivity, different combinations of these variables could yield the same STI prevalence.
Considerable further work is necessary to construct formulae of the determinants of network connectivity and then establish how these relate to empirical estimates of STI prevalence around the world. A global study that uses a standardized methodology ( Table 2) to map the variations in STI prevalence and associated risk factors by ethnic group/region within all relevant countries could provide valuable further information. So too, longitudinal studies that follow up populations from high and low STI prevalence populations from the time of sexual debut would be useful. These should accurately map the timing and correlates of STI spread including alterations of vaginal and penile microbiomes and allow more precise quantitation of which risk factors are most important for STI spread. These studies should enable the construction of more accurate models of STI spread that can be used to predict STI prevalence for specific populations under various counterfactual scenarios such as reductions in the prevalence of concurrent partnering.
Table 2. Suggested standardized methodology for mapping variations in sexually transmitted infection (STI) prevalence and associated risk factors by ethnic group/region in all relevant countries.
| No. | Methodology |
|---|---|
| 1 | Relevant countries are those where STI/HIV prevalence varies by 2-fold between ethnic groups/regions |
| 2 | Assess if analysis is more appropriately broken down by ethnic group or region based on:
1. HIV prevalence differential greater by region or by ethnicity 2. Degree of homophily by ethnicity in partner choice |
| 3 | Use hierarchy of survey designs for data analysis, with HIV and other STI serolinked, nationally, regionally and ethnic group
representative sampling as the gold standard |
| 4 | Use standardized definitions of variables such all 15–49 year olds and all 15–24 year olds regardless of if ever had sex or not |
| 5 | Standardized methodology for data analysis and visualization |
Our theory includes mention of the wide array of upstream socioeconomic and political factors that have been shown to influence the spread of STIs 123. We argue that the pathways through which these factors facilitate STI transmission is to a large extent mediated via alterations in network connectivity 124. We have not, however, gone into any detail into reviewing the evidence on which this view is based 123, 125, 126. Furthermore, our focus on the more downstream factors responsible for STI transmission should not detract from efforts to target the upstream determinants of enhanced STI transmission.
Implications of network connectivity: Know Your Network, Determine Your Prevalence
If confirmed by further experimental data, the network connectivity approach would generate new opportunities for STI prevention interventions. Whilst individual level biomedical STI control interventions have delivered considerable successes, they do not address the root cause of high STI prevalence and are therefore unlikely to accomplish radical prevention 126, 127. HIV pre-exposure prophylaxis and treatment as prevention, for example, may reduce HIV transmission but will not reduce the transmission of other STIs. If differential network connectivity is a fundamental determinant of STI and BV prevalence then this could be communicated to affected populations as an opportunity to effect radical prevention. Along these lines, a ‘Know your Network’ intervention has been successfully piloted in Kenya 128. During a community meeting, the community's sexual network was computed by fitting a dynamic network model to data from individual sexual diaries, and a graphical representation of the network was fed back to the community. Participants reported the intervention to be transformative but formal trials are required to assess the efficacy on STI incidence of this type of intervention 128. Uganda’s ‘Zero Grazing’ campaign 129 and similar processes elsewhere in Africa 100, 130 which resulted in dramatic declines in side-partners and HIV incidence, could be viewed as providing both guidance and evidence for this approach.
Data availability
No data are associated with this article.
Acknowledgements
We would like to thank Leigh Johnson for helpful comments on an earlier draft of the paper and discussants at a South African Centre for Epidemiological Modelling and Analysis seminar where this hypothesis was presented.
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 2; referees: 2 approved]
References
- 1. Gray R, Kigozi G, Kong X, et al. : The effectiveness of male circumcision for HIV prevention and effects on risk behaviors in a posttrial follow-up study. AIDS. 2012;26(5):609–15. 10.1097/QAD.0b013e3283504a3f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chesson HW, Mayaud P, Aral SO, et al. : Sexually Transmitted Infections: Impact and Cost-Effectiveness of Prevention. Disease Control Priorities. 2017;6:203–232. 10.1596/978-1-4648-0524-0_ch10 [DOI] [PubMed] [Google Scholar]
- 3. Dallabetta G, Wi T, Nielsen G, et al. : Prevention and control of STD and HIV infection in developing countries.Sexually transmitted diseases 4th edn New York, NY: McGraw-Hill.2008. [Google Scholar]
- 4. Gewirtzman A, Bobrick L, Conner K, et al. : Epidemiology of Sexually Transmitted Infections.In: Gross G, Tyring SK, editors. Sexually transmitted infections and sexually transmitted diseases.Heidelbergh: Springer Verlag.2011;13–34. 10.1007/978-3-642-14663-3_2 [DOI] [Google Scholar]
- 5. Holmqvist G: HIV and Income Inequality: If there is a link, what does it tell us?Working Paper, International Policy Centre for Inclusive Growth,2009. Reference Source [Google Scholar]
- 6. Kenyon CR, Buyze J: No association between gender inequality and peak HIV prevalence in developing countries - an ecological study. AIDS Care. 2015;27(2):150–9. 10.1080/09540121.2014.963011 [DOI] [PubMed] [Google Scholar]
- 7. Voeten HA, Vissers DC, Gregson S, et al. : Strong association between in-migration and HIV prevalence in urban sub-Saharan Africa. Sex Transm Dis. 2010;37(4):240–3. 10.1097/OLQ.0b013e3181c3f2d0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Morrison CS, Chen PL, Kwok C, et al. : Hormonal contraception and the risk of HIV acquisition: an individual participant data meta-analysis. PLoS Med. 2015;12(1):e1001778. 10.1371/journal.pmed.1001778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buve A, Jespers V, Crucitti T, et al. : The vaginal microbiota and susceptibility to HIV. AIDS. 2014;28(16):2333–44. 10.1097/QAD.0000000000000432 [DOI] [PubMed] [Google Scholar]
- 10. Kaul R, Cohen CR, Chege D, et al. : Biological factors that may contribute to regional and racial disparities in HIV prevalence. Am J Reprod Immunol. 2011;65(3):317–24. 10.1111/j.1600-0897.2010.00962.x [DOI] [PubMed] [Google Scholar]
- 11. Drain PK, Smith JS, Hughes JP, et al. : Correlates of national HIV seroprevalence: an ecologic analysis of 122 developing countries. J Acquir Immune Defic Syndr. 2004;35(4):407–20. 10.1097/00126334-200404010-00011 [DOI] [PubMed] [Google Scholar]
- 12. Morris M, Kurth AE, Hamilton DT, et al. : Concurrent partnerships and HIV prevalence disparities by race: linking science and public health practice. Am J Public Health. 2009;99(6):1023–31. 10.2105/AJPH.2008.147835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Morris M, Kretzschmar M: Concurrent partnerships and the spread of HIV. AIDS. 1997;11(5):641–8. 10.1097/00002030-199705000-00012 [DOI] [PubMed] [Google Scholar]
- 14. Keeling MJ, Eames KT: Networks and epidemic models. J R Soc Interface. 2005;2(4):295–307. 10.1098/rsif.2005.0051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Watts CH, May RM: The influence of concurrent partnerships on the dynamics of HIV/AIDS. Math Biosci. 1992;108(1):89–104. 10.1016/0025-5564(92)90006-I [DOI] [PubMed] [Google Scholar]
- 16. Jolly AM, Muth SQ, Wylie JL, et al. : Sexual networks and sexually transmitted infections: a tale of two cities. J Urban Health. 2001;78(3):433–445. 10.1093/jurban/78.3.433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jolly AM, Wylie JL: Sexual Networks and Sexually Transmitted Infections; “The Strength of Weak (Long Distance) Ties”. In: The New Public Health and STD/HIV Prevention.Springer;2013:77–109. 10.1007/978-1-4614-4526-5_5 [DOI] [Google Scholar]
- 18. Potterat JJ, Zimmerman-Rogers H, Muth SQ, et al. : Chlamydia transmission: concurrency, reproduction number, and the epidemic trajectory. Am J Epidemiol. 1999;150(12):1331–9. 10.1093/oxfordjournals.aje.a009965 [DOI] [PubMed] [Google Scholar]
- 19. Laumann EO, Youm Y: Racial/ethnic group differences in the prevalence of sexually transmitted diseases in the United States: a network explanation. Sex Transm Dis. 1999;26(5):250–61. 10.1097/00007435-199905000-00003 [DOI] [PubMed] [Google Scholar]
- 20. Kraut-Becher J, Eisenberg M, Voytek C, et al. : Examining racial disparities in HIV: lessons from sexually transmitted infections research. J Acquir Immune Defic Syndr. 2008;47 Suppl 1:S20–7. [DOI] [PubMed] [Google Scholar]
- 21. Morris M, Goodreau S, Moody J: Sexual networks, concurrency and STD/HIV.In: Holmes KK, editor. Sexually transmitted diseases 4th ed. New York: McGraw-Hill Medical;2008;2166. [Google Scholar]
- 22. Armbruster B, Wang L, Morris M: Forward reachable sets: Analytically derived properties of connected components for dynamic networks. Netw Sci. 2017;5(3):328–54. 10.1017/nws.2017.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wasserheit JN: Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis. 1992;19(2):61–77. [PubMed] [Google Scholar]
- 24. Hethcote HW, Yorke JA: Lecture notes in biomathematics: gonorrhea transmission and control.Levin S, editor. Berlin: Springer-Verlag;1984. [Google Scholar]
- 25. Yorke JA, Hethcote HW, Nold A: Dynamics and control of the transmission of gonorrhea. Sex Transm Dis. 1978;5(2):51–6. 10.1097/00007435-197804000-00003 [DOI] [PubMed] [Google Scholar]
- 26. Leiby GM, Turner TB, Clark GE, et al. : Studies on syphilis in the Eastern Health District of Baltimore city; syphilis among parturient women as an index of the trend of syphilis in the community. Am J Hyg. 1947;46(2):260–7. 10.1093/oxfordjournals.aje.a119167 [DOI] [PubMed] [Google Scholar]
- 27. Kenyon CR, Osbak K, Tsoumanis A: The Global Epidemiology of Syphilis in the Past Century - A Systematic Review Based on Antenatal Syphilis Prevalence. PLoS Negl Trop Dis. 2016;10(5):e0004711. 10.1371/journal.pntd.0004711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fleming DT, McQuillan GM, Johnson RE, et al. : Herpes simplex virus type 2 in the United States, 1976 to 1994. N Engl J Med. 1997;337(16):1105–11. 10.1056/NEJM199710163371601 [DOI] [PubMed] [Google Scholar]
- 29. Goodreau SM, Cassels S, Kasprzyk D, et al. : Concurrent partnerships, acute infection and HIV epidemic dynamics among young adults in Zimbabwe. AIDS Behav. 2012;16(2):312–22. 10.1007/s10461-010-9858-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kenyon C, Buyze J, Colebunders R: HIV prevalence by race co-varies closely with concurrency and number of sex partners in South Africa. PLoS One. 2013;8(5):e64080. 10.1371/journal.pone.0064080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kenyon CR, Buyze J, Klebanoff M, et al. : Association between bacterial vaginosis and partner concurrency: a longitudinal study. Sex Transm Infect. 2018;94(1):75–77. 10.1136/sextrans-2016-052652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kenyon CR, Buyze J, Klebanoff M, et al. : Incident Trichomonas vaginalis Is Associated With Partnership Concurrency: A Longitudinal Cohort Study. Sex Transm Dis. 2017;44(11):695–9. 10.1097/OLQ.0000000000000668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Koumans EH, Sternberg M, Bruce C, et al. : The prevalence of bacterial vaginosis in the United States, 2001-2004; associations with symptoms, sexual behaviors, and reproductive health. Sex Transm Dis. 2007;34(11):864–9. 10.1097/OLQ.0b013e318074e565 [DOI] [PubMed] [Google Scholar]
- 34. Kenyon CR, Colebunders R: Strong association between the prevalence of bacterial vaginosis and male point-concurrency. Eur J Obstet Gynecol Reprod Biol. 2014;172:93–6. 10.1016/j.ejogrb.2013.10.011 [DOI] [PubMed] [Google Scholar]
- 35. Buvé A, Weiss HA, Laga M, et al. : The epidemiology of gonorrhoea, chlamydial infection and syphilis in four African cities. AIDS. 2001;15 Suppl 4:S79–88. 10.1097/00002030-200108004-00009 [DOI] [PubMed] [Google Scholar]
- 36. Fenton KA, Korovessis C, Johnson AM, et al. : Sexual behaviour in Britain: reported sexually transmitted infections and prevalent genital Chlamydia trachomatis infection. Lancet. 2001;358(9296):1851–4. 10.1016/S0140-6736(01)06886-6 [DOI] [PubMed] [Google Scholar]
- 37. Canchihuaman FA, Carcamo CP, Garcia PJ, et al. : Non-monogamy and risk of infection with Chlamydia trachomatis and Trichomonas vaginalis among young adults and their cohabiting partners in Peru. Sex Transm Dis. 2010;86 Suppl 3:iii37–iii44. 10.1136/sti.2010.045310 [DOI] [PubMed] [Google Scholar]
- 38. Garnett GP, Mertz KJ, Finelli L, et al. : The transmission dynamics of gonorrhoea: modelling the reported behaviour of infected patients from Newark, New Jersey. Philos Trans R Soc Lond B Biol Sci. 1999;354(1384):787–97. 10.1098/rstb.1999.0431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ghani AC, Swinton J, Garnett GP: The role of sexual partnership networks in the epidemiology of gonorrhea. Sex Transm Dis. 1997;24(1):45–56. 10.1097/00007435-199701000-00009 [DOI] [PubMed] [Google Scholar]
- 40. Mishra V, Medley A, Hong R, et al. : Levels and spread of HIV seroprevalence and associated factors: evidence from national household surveys.2009. Reference Source [Google Scholar]
- 41. Auvert B, Buvé A, Ferry B, et al. : Ecological and individual level analysis of risk factors for HIV infection in four urban populations in sub-Saharan Africa with different levels of HIV infection. AIDS. 2001;15 Suppl 4:S15–30. 10.1097/00002030-200108004-00003 [DOI] [PubMed] [Google Scholar]
- 42. Kenyon C: HIV prevalence correlated with circumcision prevalence and high-risk sexual behavior in India's states: an ecological study [version 1; referees: awaiting peer review]. F1000Res. 2019;8:60 10.12688/f1000research.17807.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kenyon CR, Tsoumanis A, Schwartz IS: HIV Prevalence Correlates with High-Risk Sexual Behavior in Ethiopia's Regions. PLoS One. 2015;10(10):e0140835. 10.1371/journal.pone.0140835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kenyon CR, Tsoumanis A, Schwartz IS: A population's higher-risk sexual behaviour is associated with its average sexual behaviour-An ecological analysis of subpopulations in Ethiopia, Kenya, South Africa, Uganda and the United States. Epidemics. 2016;15:56–65. 10.1016/j.epidem.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 45. Helleringer S, Kohler HP, Kalilani-Phiri L: The association of HIV serodiscordance and partnership concurrency in Likoma Island (Malawi). AIDS. 2009;23(10):1285–7. 10.1097/QAD.0b013e32832aa85c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kenyon CR, Tsoumanis A, Schwartz IS, et al. : Partner concurrency and HIV infection risk in South Africa. Int J Infect Dis. 2016;45:81–7. 10.1016/j.ijid.2016.03.001 [DOI] [PubMed] [Google Scholar]
- 47. Adimora AA, Schoenbach VJ, Martinson FE, et al. : Heterosexually transmitted HIV infection among African Americans in North Carolina. J Acquir Immune Defic Syndr. 2006;41(5):616–23. 10.1097/01.qai.0000191382.62070.a5 [DOI] [PubMed] [Google Scholar]
- 48. Kenyon C, Colebunders R: Strong association between point-concurrency and national peak HIV prevalence. Int J Infect Dis. 2012;16(11):e826–7. 10.1016/j.ijid.2012.05.008 [DOI] [PubMed] [Google Scholar]
- 49. Bohl DD, Raymond HF, Arnold M, et al. : Concurrent sexual partnerships and racial disparities in HIV infection among men who have sex with men. Sex Transm Infect. 2009;85(5):367–9. 10.1136/sti.2009.036723 [DOI] [PubMed] [Google Scholar]
- 50. Adimora AA, Schoenbach VJ, Bonas DM, et al. : Concurrent sexual partnerships among women in the United States. Epidemiology. 2002;13(3):320–7. 10.1097/00001648-200205000-00013 [DOI] [PubMed] [Google Scholar]
- 51. Xu F, Sternberg MR, Kottiri BJ, et al. : Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States. JAMA. 2006;296(8):964–73. 10.1001/jama.296.8.964 [DOI] [PubMed] [Google Scholar]
- 52. Kenyon C, Colebunders R, Buve A, et al. : Partner-concurrency associated with herpes simplex virus 2 infection in young South Africans. Int J STD AIDS. 2013;24(10):804–12. 10.1177/0956462413482810 [DOI] [PubMed] [Google Scholar]
- 53. Kenyon C, Colebunders R, Hens N: Determinants of generalized herpes simplex virus-2 epidemics: the role of sexual partner concurrency. Int J STD AIDS. 2013;24(5):375–82. 10.1177/0956462412472816 [DOI] [PubMed] [Google Scholar]
- 54. Shi R, Devarakonda S, Liu L, et al. : Factors associated with genital human papillomavirus infection among adult females in the United States, NHANES 2007-2010. BMC Res Notes. 2014;7:544. 10.1186/1756-0500-7-544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sonnenberg P, Clifton S, Beddows S, et al. : Prevalence, risk factors, and uptake of interventions for sexually transmitted infections in Britain: findings from the National Surveys of Sexual Attitudes and Lifestyles (Natsal). Lancet. 2013;382(9907):1795–806. 10.1016/S0140-6736(13)61947-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Javanbakht M, Gorbach PM, Amani B, et al. : Concurrency, sex partner risk, and high-risk human papillomavirus infection among African American, Asian, and Hispanic women. Sex Transm Dis. 2010;37(2):68–74. 10.1097/OLQ.0b013e3181bcd3e7 [DOI] [PubMed] [Google Scholar]
- 57. Koumans EH, Farley TA, Gibson JJ, et al. : Characteristics of persons with syphilis in areas of persisting syphilis in the United States: sustained transmission associated with concurrent partnerships. Sex Transm Dis. 2001;28(9):497–503. 10.1097/00007435-200109000-00004 [DOI] [PubMed] [Google Scholar]
- 58. Kenyon CR, Osbak K: The Prevalence of Syphilis Is Associated with the Prevalence of Male Point-Concurrency: An Ecological Analysis. World J AIDS. 2015;5(02): 57363. 10.4236/wja.2015.52016 [DOI] [Google Scholar]
- 59. Rogers SM, Turner CF, Hobbs M, et al. : Epidemiology of undiagnosed trichomoniasis in a probability sample of urban young adults. PLoS One. 2014;9(3):e90548. 10.1371/journal.pone.0090548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kenyon CR, Hamilton DT: Correlation between Trichomonas vaginalis and Concurrency: An Ecological Study. Interdiscip Perspect Infect Dis. 2016;2016:5052802. 10.1155/2016/5052802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Koumans EH, Sternberg M, Bruce C, et al. : The prevalence of bacterial vaginosis in the United States, 2001-2004; associations with symptoms, sexual behaviors, and reproductive health. Sex Transm Dis. 2007;34(11):864–9. 10.1097/OLQ.0b013e318074e565 [DOI] [PubMed] [Google Scholar]
- 62. Johnson LF, Dorrington RE, Bradshaw D, et al. : Sexual behaviour patterns in South Africa and their association with the spread of HIV: insights from a mathematical model. Demogr Res. 2009;21:289–340. 10.4054/DemRes.2009.21.11 [DOI] [Google Scholar]
- 63. Paz-Bailey G, Morales-Miranda S, Jacobson JO, et al. : High rates of STD and sexual risk behaviors among Garífunas in Honduras. J Acquir Immune Defic Syndr. 2009;51 Suppl 1:S26–34. 10.1097/QAI.0b013e3181a2647b [DOI] [PubMed] [Google Scholar]
- 64. Kenyon CR, Vu L, Menten J, et al. : Male circumcision and sexual risk behaviors may contribute to considerable ethnic disparities in HIV prevalence in Kenya: an ecological analysis. PLoS One. 2014;9(8):e106230. 10.1371/journal.pone.0106230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kenyon CR: HIV prevalence by ethnic group covaries with prevalence of herpes simplex virus-2 and high-risk sex in Uganda: An ecological study. PLoS One. 2018;13(4):e0195431. 10.1371/journal.pone.0195431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Kenyon CR, Osbak K, Buyze J: The prevalence of HIV by ethnic group is correlated with HSV-2 and syphilis prevalence in Kenya, South Africa, the United Kingdom and the United States. Interdiscip Perspect Infect Dis 2014:2014:284317. 10.1155/2014/284317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Fenton KA, Mercer CH, McManus S, et al. : Ethnic variations in sexual behaviour in Great Britain and risk of sexually transmitted infections: a probability survey. Lancet. 2005;365(9466):1246–55. 10.1016/S0140-6736(05)74813-3 [DOI] [PubMed] [Google Scholar]
- 68. Turner KM, Garnett GP, Ghani AC, et al. : Investigating ethnic inequalities in the incidence of sexually transmitted infections: mathematical modelling study. Sex Transm Infect. 2004;80(5):379–85. 10.1136/sti.2003.007575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kenyon C, Buyze J, Schwartz IS: Strong association between higher-risk sex and HIV prevalence at the regional level: an ecological study of 27 sub-Saharan African countries [version 1; referees: 1 approved]. F1000Res. 2018;7:1879 10.12688/f1000research.17108.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Kenyon C, Osbak K: Sexual networks, HIV, race and bacterial vaginosis. AIDS. 2015;29(5):641–642. 10.1097/QAD.0000000000000566 [DOI] [PubMed] [Google Scholar]
- 71. Kenyon CR, Delva W, Brotman RM: Differential sexual network connectivity offers a parsimonious explanation for population-level variations in the prevalence of bacterial vaginosis: a data-driven, model-supported hypothesis. BMC Womens Health. 2019;19(1):8. 10.1186/s12905-018-0703-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Kenyon C, Colebunders R, Voeten H, et al. : Peak HIV prevalence: a useful outcome variable for ecological studies. Int J Infect Dis. 2013;17(5):e286–8. 10.1016/j.ijid.2012.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Gouws E, Mishra V, Fowler TB: Comparison of adult HIV prevalence from national population-based surveys and antenatal clinic surveillance in countries with generalised epidemics: implications for calibrating surveillance data. Sex Transm Infect. 2008;84 Suppl 1:i17–i23. 10.1136/sti.2008.030452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. UNAIDS/WHO: Estimating National Adult Prevalence of HIV-1 in Generalized Epidemics. Geneva: UNAIDS/WHO, 2009. [Google Scholar]
- 75. WHO: Surveillance of the HIV/AIDS epidemic: 2013 comprehensive package. Geneva: WHO.2013. Reference Source [Google Scholar]
- 76. Kenyon C, Colebunders R, Voeten H, et al. : Migration intensity has no effect on peak HIV prevalence: an ecological study. BMC Infect Dis. 2014;14(1):350. 10.1186/1471-2334-14-350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Kenyon C, Buyze J: Correlation between National Peak HIV Prevalence and Concurrency, STI Treatment Capability, Condom Use and Circumcision: An Ecological Study. World J AIDS. 2014;4(2): 47249. 10.4236/wja.2014.42030 [DOI] [Google Scholar]
- 78. Mishra V, Assche SB, Greener R, et al. : HIV infection does not disproportionately affect the poorer in sub-Saharan Africa. AIDS. 2007;21 Suppl 7:S17–28. 10.1097/01.aids.0000300532.51860.2a [DOI] [PubMed] [Google Scholar]
- 79. Drain PK, Halperin DT, Hughes JP, et al. : Male circumcision, religion, and infectious diseases: an ecologic analysis of 118 developing countries. BMC Infect Dis. 2006;6:172. 10.1186/1471-2334-6-172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Kenyon C: Ecological association between HIV and concurrency point-prevalence in South Africa's ethnic groups. Afr J AIDS Res. 2013;12(2):79–84. 10.2989/16085906.2013.851717 [DOI] [PubMed] [Google Scholar]
- 81. Sawers L, Stillwaggon E: Concurrent sexual partnerships do not explain the HIV epidemics in Africa: a systematic review of the evidence. J Int AIDS Soc. 2010;13:34. 10.1186/1758-2652-13-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Lagarde E, Auvert B, Caraël M, et al. : Concurrent sexual partnerships and HIV prevalence in five urban communities of sub-Saharan Africa. AIDS. 2001;15(7):877–84. 10.1097/00002030-200105040-00008 [DOI] [PubMed] [Google Scholar]
- 83. Morris M: Barking up the wrong evidence tree. Comment on Lurie & Rosenthal, "Concurrent partnerships as a driver of the HIV epidemic in sub-Saharan Africa? The evidence is limited". AIDS Behav. 2010;14(1):31–3; discussion 34–7. 10.1007/s10461-009-9639-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Fenton KA, Imrie J: Increasing rates of sexually transmitted diseases in homosexual men in Western europe and the United States: why? Infect Dis Clin North Am. 2005;19(2):311–31. 10.1016/j.idc.2005.04.004 [DOI] [PubMed] [Google Scholar]
- 85. Public Health England: Inequalities in sexual health: Update on HIV and STIs in men who have sex with men in London.London:2016. Reference Source [Google Scholar]
- 86. Fenton KA, Wasserheit JN: The courage to learn from our failures: syphilis control in men who have sex with men. Sex Transm Dis. 2007;34(3):162–5. 10.1097/01.olq.0000259398.70789.c6 [DOI] [PubMed] [Google Scholar]
- 87. Kenyon C, Osbak K: Certain attributes of the sexual ecosystem of high-risk MSM have resulted in an altered microbiome with an enhanced propensity to generate and transmit antibiotic resistance. Med Hypotheses. 2014;83(2):196–202. 10.1016/j.mehy.2014.04.030 [DOI] [PubMed] [Google Scholar]
- 88. Mercer CH, Prah P, Field N, et al. : The health and well-being of men who have sex with men (MSM) in Britain: Evidence from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). BMC Public Health. 2016;16:525. 10.1186/s12889-016-3149-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Peterman TA, Su J, Bernstein KT, et al. : Syphilis in the United States: on the rise? Expert Rev Anti Infect Ther. 2015;13(2):161–8. 10.1586/14787210.2015.990384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Stenger MR, Baral S, Stahlman S, et al. : As through a glass, darkly: the future of sexually transmissible infections among gay, bisexual and other men who have sex with men. Sex Health. 2017;14(1):18–27. 10.1071/SH16104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Aral SO, Fenton KA, Holmes KK: Sexually transmitted diseases in the USA: temporal trends. Sex Transm Infect. 2007;83(4):257–66. 10.1136/sti.2007.026245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Sandholzer TA: Factors Affecting the Incidence and Management of Sexually Transmitted Diseases in Homosexual Men. Sexually Transmitted Diseases in Homosexual Men: Springer;1983;3– 12 10.1007/978-1-4684-1164-5_1 [DOI] [Google Scholar]
- 93. Chesson HW, Dee TS, Aral SO: AIDS mortality may have contributed to the decline in syphilis rates in the United States in the 1990s. Sex Transm Dis. 2003;30(5):419–24. 10.1097/00007435-200305000-00008 [DOI] [PubMed] [Google Scholar]
- 94. Crepaz N, Hart TA, Marks G: Highly active antiretroviral therapy and sexual risk behavior: a meta-analytic review. JAMA. 2004;292(2):224–36. 10.1001/jama.292.2.224 [DOI] [PubMed] [Google Scholar]
- 95. Stoneburner RL, Low-Beer D: Sexual partner reductions explain human immunodeficiency virus declines in Uganda: comparative analyses of HIV and behavioural data in Uganda, Kenya, Malawi, and Zambia. Int J Epidemiol. 2004;33(3):624. 10.1093/ije/dyh141 [DOI] [PubMed] [Google Scholar]
- 96. Gregson S, Garnett GP, Nyamukapa CA, et al. : HIV decline associated with behavior change in eastern Zimbabwe. Science. 2006;311(5761):664–6. 10.1126/science.1121054 [DOI] [PubMed] [Google Scholar]
- 97. Stoneburner RL, Low-Beer D: Population-level HIV declines and behavioral risk avoidance in Uganda. Science. 2004;304(5671):714–8. 10.1126/science.1093166 [DOI] [PubMed] [Google Scholar]
- 98. Cheluget B, Baltazar G, Orege P, et al. : Evidence for population level declines in adult HIV prevalence in Kenya. Sex Transm Infect. 2006;82 Suppl 1:i21–6. 10.1136/sti.2005.015990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Eaton JW, Takavarasha FR, Schumacher CM, et al. : Trends in concurrency, polygyny, and multiple sex partnerships during a decade of declining HIV prevalence in eastern Zimbabwe. J Infect Dis. 2014;210 Suppl 2:S562–8. 10.1093/infdis/jiu415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Halperin DT, Mugurungi O, Hallett TB, et al. : A surprising prevention success: why did the HIV epidemic decline in Zimbabwe? PLoS Med. 2011;8(2):e1000414. 10.1371/journal.pmed.1000414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Johnson LF, Dorrington RE, Bradshaw D, et al. : The effect of syndromic management interventions on the prevalence of sexually transmitted infections in South Africa. Sex Reprod Healthc. 2011;2(1):13–20. 10.1016/j.srhc.2010.08.006 [DOI] [PubMed] [Google Scholar]
- 102. Kenyon C, Buyze J, Colebunders R: Classification of incidence and prevalence of certain sexually transmitted infections by world regions. Int J of Infec Dis. 2014;18:73–80. 10.1016/j.ijid.2013.09.014 [DOI] [PubMed] [Google Scholar]
- 103. Osbak KK, Rowley JT, Kassebaum NJ, et al. : The Prevalence of Syphilis from the Early HIV Period is Correlated With Peak HIV Prevalence at a Country Level. Sex Transm Dis. 2016;43(4):255–7. 10.1097/OLQ.0000000000000422 [DOI] [PubMed] [Google Scholar]
- 104. Kenyon C: Strong associations between national prevalence of various STIs suggests sexual network connectivity is a common underpinning risk factor. BMC Infect Dis. 2017;17(1):682. 10.1186/s12879-017-2794-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Liu CM, Hungate BA, Tobian AA, et al. : Penile Microbiota and Female Partner Bacterial Vaginosis in Rakai, Uganda. mBio. 2015;6(3):e00589. 10.1128/mBio.00589-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Balashov SV, Mordechai E, Adelson ME, et al. : Identification, quantification and subtyping of Gardnerella vaginalis in noncultured clinical vaginal samples by quantitative PCR. J Med Microbiol. 2014;63(Pt 2):162–75. 10.1099/jmm.0.066407-0 [DOI] [PubMed] [Google Scholar]
- 107. Swidsinski A, Doerffel Y, Loening-Baucke V, et al. : Gardnerella biofilm involves females and males and is transmitted sexually. Gynecol Obstet Invest. 2010;70(4):256–63. 10.1159/000314015 [DOI] [PubMed] [Google Scholar]
- 108. Gardner HL, Dukes CD: Haemophilus vaginalis vaginitis: a newly defined specific infection previously classified non-specific vaginitis. Am J Obstet Gynecol. 1955;69(5):962–76. 10.1016/0002-9378(55)90095-8 [DOI] [PubMed] [Google Scholar]
- 109. Zozaya M, Ferris MJ, Siren JD, et al. : Bacterial communities in penile skin, male urethra, and vaginas of heterosexual couples with and without bacterial vaginosis. Microbiome. 2016;4:16. 10.1186/s40168-016-0161-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Nelson DE, Dong Q, Van der Pol B, et al. : Bacterial communities of the coronal sulcus and distal urethra of adolescent males. PLoS One. 2012;7(5):e36298. 10.1371/journal.pone.0036298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Nelson DE, Van Der Pol B, Dong Q, et al. : Characteristic male urine microbiomes associate with asymptomatic sexually transmitted infection. PLoS One. 2010;5(11):e14116. 10.1371/journal.pone.0014116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Fethers KA, Fairley CK, Hocking JS, et al. : Sexual risk factors and bacterial vaginosis: a systematic review and meta-analysis. Clin Infect Dis. 2008;47(11):1426–35. 10.1086/592974 [DOI] [PubMed] [Google Scholar]
- 113. Fethers KA, Fairley CK, Morton A, et al. : Early sexual experiences and risk factors for bacterial vaginosis. J Infect Dis. 2009;200(11):1662–70. 10.1086/648092 [DOI] [PubMed] [Google Scholar]
- 114. Bautista CT, Wurapa E, Sateren WB, et al. : Bacterial vaginosis: a synthesis of the literature on etiology, prevalence, risk factors, and relationship with chlamydia and gonorrhea infections. Mil Med Res. 2016;3:4. 10.1186/s40779-016-0074-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Brotman RM, Klebanoff MA, Nansel TR, et al. : Bacterial vaginosis assessed by gram stain and diminished colonization resistance to incident gonococcal, chlamydial, and trichomonal genital infection. J Infect Dis. 2010;202(12):1907–15. 10.1086/657320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Kaul R, Nagelkerke NJ, Kimani J, et al. : Prevalent herpes simplex virus type 2 infection is associated with altered vaginal flora and an increased susceptibility to multiple sexually transmitted infections. J Infect Dis. 2007;196(11):1692–7. 10.1086/522006 [DOI] [PubMed] [Google Scholar]
- 117. Rottingen JA, Cameron DW, Garnett GP: A systematic review of the epidemiologic interactions between classic sexually transmitted diseases and HIV: how much really is known? Sex Transm Dis. 2001;28(10):579–97. 10.1097/00007435-200110000-00005 [DOI] [PubMed] [Google Scholar]
- 118. Ward H, Ronn M: Contribution of sexually transmitted infections to the sexual transmission of HIV. Curr Opin HIV AIDS. 2010;5(4):305–10. 10.1097/COH.0b013e32833a8844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Cherpes TL, Meyn LA, Krohn MA, et al. : Risk factors for infection with herpes simplex virus type 2: role of smoking, douching, uncircumcised males, and vaginal flora. Sex Transm Dis. 2003;30(5):405–10. 10.1097/00007435-200305000-00006 [DOI] [PubMed] [Google Scholar]
- 120. Cherpes TL, Meyn LA, Krohn MA, et al. : Association between acquisition of herpes simplex virus type 2 in women and bacterial vaginosis. Clin Infect Dis. 2003;37(3):319–25. 10.1086/375819 [DOI] [PubMed] [Google Scholar]
- 121. Rathod SD, Krupp K, Klausner JD, et al. : Bacterial vaginosis and risk for Trichomonas vaginalis infection: a longitudinal analysis. Sex Transm Dis. 2011;38(9):882–6. 10.1097/OLQ.0b013e31821f91a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Esber A, Vicetti Miguel RD, Cherpes TL, et al. : Risk of Bacterial Vaginosis Among Women With Herpes Simplex Virus Type 2 Infection: A Systematic Review and Meta-analysis. J Infect Dis. 2015;212(1):8–17. 10.1093/infdis/jiv017 [DOI] [PubMed] [Google Scholar]
- 123. Aral SO: Determinants of STD epidemics: implications for phase appropriate intervention strategies. Sex Transm Infect. 2002;78 Suppl 1:i3–13. 10.1136/sti.78.suppl_1.i3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Gorbach PM, Stoner BP, Aral SO, et al. : "It takes a village": understanding concurrent sexual partnerships in Seattle, Washington. Sex Transm Dis. 2002;29(8):453–462. 10.1097/00007435-200208000-00004 [DOI] [PubMed] [Google Scholar]
- 125. Aral SO, Leichliter JS: Non-monogamy: risk factor for STI transmission and acquisition and determinant of STI spread in populations. Sex Transm Infect. 2010;86 Suppl 3:iii29–36. 10.1136/sti.2010.044149 [DOI] [PubMed] [Google Scholar]
- 126. Aral SO, Leichliter JS, Blanchard JF: Overview: the role of emergent properties of complex systems in the epidemiology and prevention of sexually transmitted infections including HIV infection. Sex Transm Infect. 2010;86 Suppl 3:iii1–3. 10.1136/sti.2010.047373 [DOI] [PubMed] [Google Scholar]
- 127. Rose G, Day S: The population mean predicts the number of deviant individuals. BMJ. 1990;301(6759):1031–4. 10.1136/bmj.301.6759.1031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Knopf A, Agot K, Sidle J, et al. : "This is the medicine:" A Kenyan community responds to a sexual concurrency reduction intervention. Soc Sci Med. 2014;108:175–84. 10.1016/J.Socscimed.2014.01.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Kirby D: Changes in sexual behaviour leading to the decline in the prevalence of HIV in Uganda: confirmation from multiple sources of evidence. Sex Transm Infect. 2008;84 Suppl 2:ii35–ii41. 10.1136/sti.2008.029892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Shisana O, Rehle, T, Simbayi LC, et al. : South African National HIV Prevalence, Incidence and Behaviour Survey, 2012.Cape Town: HSRC Press;2014. Reference Source [Google Scholar]