Abstract
Objective
To compare characteristics associated with backyard trampoline injuries (BTI) and trampoline park injuries (TPI) using records from the electronic Canadian Hospitals Injury Reporting and Prevention Program (eCHIRPP).
Methods
eCHIRPP records for trampoline injuries (2012 to 2016) were extracted using variable codes and narratives, and injuries were examined among individuals 17 years and younger. Descriptive estimates for BTI and TPI, as well as age and sex adjusted odds ratios (OR) for the mechanism, source, body part and type of injury associated with TPIs relative to BTIs, are presented.
Results
Trampoline injuries are increasing in Canada (P<0.01). Patients with TPIs were older than those with BTIs. Relative to BTIs, TPIs were more associated with impact as the mechanism (OR 2.6, 95% CI: 2.2 to 3.1), trampoline beds as the source (OR 1.7, 95% CI: 1.4 to 2.1), lower extremity as the body part (OR 3.7, 95% CI: 3.0 to 4.4) and sprains as the type of injury (OR 2.0, 95% CI: 1.6 to 2.4). In contrast, another jumper (OR 0.5, 95% CI: 0.4 to 0.6) or fall (OR 0.4, 95% CI: 0.4 to 0.6) as the mechanism, surface (OR 0.7, 95% CI: 0.5 to 0.9) or another jumper (OR 0.5, 95% CI: 0.4 to 0.7) as the source, face or neck (OR 0.6, 95% CI: 0.4 to 0.7) as the body part, and lacerations (OR 0.6, 95% CI: 0.3 to 0.9) or soft tissue injury (OR 0.7, 95% CI: 0.6 to 0.9) as the type of injury were more associated with BTIs relative to TPIs.
Conclusion
Trampoline parks result in injuries different than those from backyard trampolines. This examination into the distinct injury characteristics can help to inform future prevention measures.
Keywords: Trampoline, Injury
Trampoline use has become a popular source of entertainment for children, but this pastime has also been associated with significant risk of injury (1–3). Recreational use of backyard trampolines can result in injuries such as forearm and spinal fractures requiring hospitalization and surgery (4,5). Trampoline parks, which were introduced to the Canadian market in 2011 (6), have been similarly associated with injury. Due to these and other risks, the Canadian Paediatric Society (1) and American Academy of Pediatrics (2,3) have each recommended against recreational backyard trampoline use. Current position statements do not include consideration of trampoline park injuries (TPI), likely due to the limited number of studies focused on this setting (5,7).
In response to the variety of injuries associated with recreational trampoline use, voluntary industry standards have been developed. For instance, trampoline parks are fitted with padded surfaces and walls to protect people from impact injuries, as well as foam pits, where individuals can perform stunts such as somersaults (7,8). New springfree trampolines were developed to reduce injuries previously seen due to exposed trampoline springs (9). Similarly, safety nets have been recommended for backyard trampolines to prevent falls from the trampoline and subsequent injury (8). In spite of these changes, trampoline injuries persist. Backyard trampoline injuries (BTI) have been previously described using data from the electronic Canadian Hospitals Injury Reporting and Prevention Program (eCHIRPP) (10). The present study examines trends in trampoline injuries since the introduction of trampoline parks in Canada, and to compare characteristics of BTIs and TPIs.
METHODS
Data
The eCHIRPP (11,12) is a sentinel injury surveillance system established in 1990 by the Public Health Agency of Canada that currently operates in 11 paediatric and 7 general hospitals across the country. It has since accumulated more than three million records, of which roughly 80% are paediatric (12). Patients’ (or caregivers’) accounts of pre-event injury circumstances (narratives of ‘what went wrong’) are collected using the Injury Reporting form (12). All records between January 1, 2012 and August 24, 2016 for individuals ages 17 years old and younger were used in the present analysis (N=478,717).
Variables
Records that included English or French narrative terms ‘trampoline’, ‘jump’ or ‘saut’ or that indicated trampolining (S1180) as the sport were selected for initial screening. Where location information was available, cases identified to be backyard trampoline cases were selected through location codes for own home (11L to 19L) or other home (21L to 29L), while those for trampoline parks were selected using location codes for relevant sport and recreation facilities (61L, 66L, 68L and 79L). Further refinement of cases to the final two groups (TPI versus BTI) was done using iterative text mining techniques, including for those cases where location or place of injury codes were not informative. For instance, cases that occurred at venues other than those of interest (e.g., day care or zoo) were excluded. Similarly, cases that included names of known trampoline parks as the place of injury were categorized as related to TPIs.
Existing eCHIRPP codes for age in months was rounded so as to describe age in years. Existing CHIRPP variable codes were also used to identify the body part injured: face or neck (including head injury), skull (including scalp), spine (spine and/or spinal cord including discs and spinal nerves), trunk, upper extremity (UE) or lower extremity (LE). Mechanisms of injury were identified based on a combination of external cause variable codes and narrative text: impact with trampoline bed, fall, stunts or flips, another jumper, impact with horizontal surface, injury to self, impact with wall or cut or pierced. Sources (i.e., direct cause) of injury include the trampoline, the frame, springs, an external surface (e.g., cement floor), the patient (e.g., kneeing themselves), another jumper and other (e.g., a pole, a fence or furniture). Type of injury was ascertained from nature of injury variable codes: fracture, traumatic brain injuries (TBI, includes minor closed head injury, concussion and intracranial injury), dislocation, dental and injury to nerve. Patient disposition was identified through treatment variable codes, and admission to hospital was used as a proxy for injury severity.
Analysis
Data mining syntax (PERL regular expressions) (13) was used to analyse narrative text to identify cases. Statistical analyses were conducted using SAS Enterprise Guide version 5.1 (SAS Institute Inc., Cary, NC, USA). Frequency estimates are presented using proportions relative to the total number of records in the database (proportion = [injury N/total eCHIRPP N] × 100,000; presented as the number per 100,000 eCHIRPP cases). Chi-square tests were used to examine significance between groups. Logistic regression models were used to compare the odds of body part injured, type and mechanism of injury among TPI cases relative to BTI ones. These models were adjusted for age and sex, and adjusted odds ratios (OR) and 95% confidence intervals (CI) are presented.
RESULTS
Backyard versus trampoline park
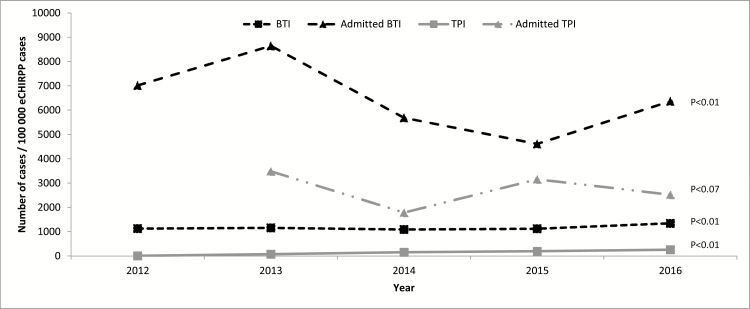
A total of 5481 cases of BTI and 563 cases of TPI were identified, representing a frequency of 968 and 101 cases per 100,000 eCHIRPP cases, respectively. Examining time trends over the past 5.5 years, the proportion of trampoline injury cases has been rising for both TPIs and BTIs (P<0.01). Furthermore, hospital admission for trampoline injuries relative to all other injuries resulting in a hospital admission have also increased significantly for BTI cases (P<0.01), but not for TPIs (P=0.07) (Figure 1).
Figure 1.
Backyard trampoline and trampoline park injury time trends, eCHIRPP, 2012–2016. Proportions of BTI and TPI cases are presented relative to other non-trampoline injuries. Proportions of admitted BTI and TPI cases are presented relative to other hospital admitted nontrampoline injuries. Records entered on or before August 24, 2016. BTI Backyard trampoline injury; TPI Trampoline park injury.
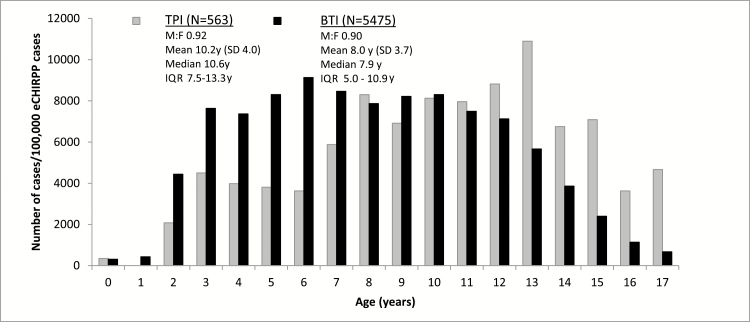
The distribution of cases among BTIs is skewed younger than for TPIs, with the proportion of cases overall being more frequent among females (Figure 2). The average age of injury was higher for TPIs at 10.2 years old, versus 8.0 years old for BTIs.
Figure 2.
Age and sex characteristics of backyard trampoline and trampoline park injury, eCHIRPP, 2012–2016. Records entered on or before August 24, 2016. BTI Backyard trampoline injury; IQR Interquartile range; ‘M:F’ Ratio of male to female cases; TPI Trampoline park injury.
Mechanism of injury
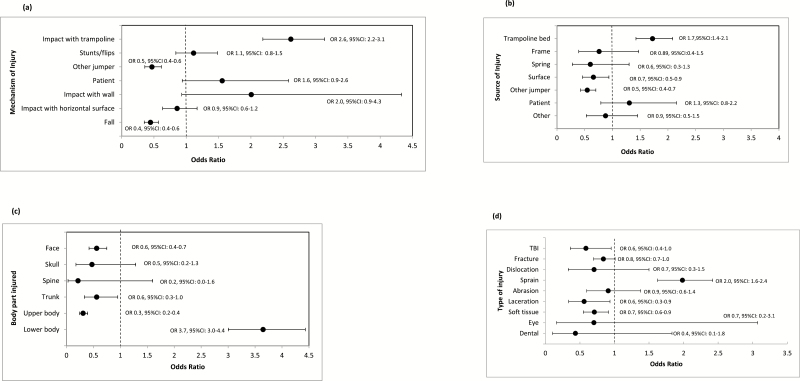
Impact with the trampoline bed, such as through a bad landing, was the most common mechanism of injury for TPIs and the second most common for BTIs (46.9% and 26.0%, respectively, P<0.01). Relative to BTIs, there were significantly more stunt-based injuries (13.5% for TPIs and 8.1% for BTIs, P<0.01) and a high proportion of patient-to-self injuries for TPIs (3.6% for TPIs and 2.3% for BTIs, P=0.06). Among BTI cases, impact with another jumper (11.4% for TPIs and 23.4% for BTIs, P<0.01) and falls (14.6% for TPIs and 27.6% for BTIs, P<0.01) were significantly more common, with no observed differences for other mechanisms of injury (impact with horizontal surface: 8.7% for TPIs and 11.0% for BTIs, P=0.10 and impact with wall: 1.4% for TPIs and 0.8% for BTIs, P=0.10). Furthermore, reports of injuries due to a cut were only observed for BTIs (n=52, 1.0%), and not for TPIs. Age and sex adjusted models examining the odds of each mechanism of injury among TPI relative to BTI follow a similar pattern, with significant differences observed for impacts with other jumper and falls for BTIs and impact with trampoline for TPIs (Figure 3a). Interestingly, the second most common mechanism of injury (after impact with trampoline bed) in infants younger than 1-year old involved circumstances where the infant was on the trampoline with another jumper (data not shown).
Figure 3.
Adjusted odds ratios of injury characteristics among trampoline park injuries, relative to backyard trampoline injuries, eCHIRPP, 2012–2016. (a) Mechanism of injury. (b) Source of injury. (c) Body part injured. (d) Type of injury. Models are adjusted for age and sex. Error bars (horizontal lines) represent 95% confidence intervals. Records entered on or before August 24, 2016.
Source of injury
Trampoline parks resulted in significantly more trampoline bed-based injuries (70.2% for TPIs and 55.9% for BTIs, P<0.01), while backyard trampolines resulted in more surface-based (6.4% for TPIs and 10.0% for BTIs, P<0.01) and other jumper-based injuries (13.7% for TPIs and 24.6% for BTIs, P<0.01). Patient, spring and frame did not appear more likely as a source of injury among either type of trampoline (Figure 3b).
Body part injured
LE injuries were more common for TPIs and while LE injuries were still the main body region for BTI injuries (71.1% for TPIs and 43.2% for BTIs), UE injuries were more common for BTIs than TPIs (35.6% and 14.7%, respectively). Face/neck injuries were more frequent among BTIs (10.0% for TPIs and 14.9% for BTIs, P<0.01). No differences were observed for other body parts (skull: 0.7% for TPI and 1.6% for BTIs, P=0.09; spine: 0.2% for TPIs and 0.6% for BTIs, P=0.23; trunk 2.8% for TPIs and 3.8% for BTIs, P=027) (Figure 3c). One case of TPI related to an UE injury, and one BTI case related to a spinal injury, were listed as involving injury to a nerve. Where information was available regarding the vertebrae affected (N=28), 53.6% involved the cervical, 21.4% the sacrum/coccyx, 17.9% the thoracic and 7.1% the lumbar vertebrae.
The mechanism of injury for each body part (by type of trampoline) is described in Table 1. The sole TPI spinal injury case involved an individual landing on their neck, while BTI spinal injuries occurred due to a variety of mechanisms and resulted in injuries ranging from soft tissue injury to nerve damage and dislocation.
Table 1.
Injury characteristics of backyard trampoline and trampoline park injury cases, eCHIRPP, 2012–2016
| Backyard trampoline injuries | Trampoline park injuries | ||||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Leading mechanism of injury based on body part | |||||
| Face/Neck | |||||
| Stunts/flips | 105 | 12.9 | 20 | 35.7 | |
| Fall | 305 | 37.3 | 17 | 30.4 | |
| Other jumper | 218 | 26.7 | 6 | 10.7 | |
| Other mechanism | 189 | 23.1 | 13 | 23.2 | |
| Skull | |||||
| Other jumper | 29 | 32.6 | 3 | 75.0 | |
| Stunts/flips | 5 | 5.6 | 1 | 25.0 | |
| Fall | 31 | 34.8 | - | - | |
| Other mechanism | 24 | 27.0 | |||
| Spine | |||||
| Fall | 11 | 35.5 | 1 | 100.0 | |
| Stunts/flips | 8 | 25.8 | - | - | |
| Impact with horizontal surface | 6 | 19.4 | - | - | |
| Other mechanism | 6 | 19.4 | - | - | |
| Trunk | |||||
| Fall | 99 | 48.1 | 9 | 56.3 | |
| Other jumper | 42 | 20.4 | 1 | 6.3 | |
| Stunts/flips | 35 | 17.0 | 4 | 25.0 | |
| Other mechanism | 30 | 14.6 | 2 | 12.5 | |
| Upper extremity | |||||
| Fall | 1034 | 53.0 | 47 | 56.6 | |
| Other jumper | 403 | 20.7 | 3 | 3.6 | |
| Impact with horizontal surface | 321 | 16.5 | 8 | 9.6 | |
| Other mechanism | 192 | 9.8 | 25 | 30.1 | |
| Lower extremity | |||||
| Impact with trampoline | 1409 | 59.5 | 262 | 65.5 | |
| Other jumper | 580 | 24.5 | 51 | 12.8 | |
| Stunts/flips | 120 | 5.1 | 29 | 7.3 | |
| Other mechanism | 260 | 11.0 | 58 | 14.5 | |
| Emergency department disposition | |||||
| Left without being seen by physician | 92 | 1.7 | 14 | 2.5 | |
| Advice only, diagnostic testing, referred to GP | 1408 | 25.7 | 140 | 25.0 | |
| Observation in ED, follow-up PRN | 69 | 1.3 | 7 | 1.3 | |
| Observation in ED, follow-up required | 84 | 1.5 | 21 | 3.7 | |
| Treated in ED, with follow-up PRN | 1410 | 25.8 | 167 | 29.8 | |
| Treated in ED, with follow-up required | 2050 | 37.5 | 195 | 34.8 | |
| Admitted to hospital | 357 | 6.5 | 17 | 3.0 | |
| Admitted primarily for reason other than injury treatment | 3 | 0.1 | - | ||
| Admitted cases | |||||
| Fractures | 326 | 90.6 | 11 | 64.7 | |
| Dislocation | 10 | 2.8 | 2 | 11.8 | |
| Injury to internal organs | - | - | 3 | 17.7 | |
| Soft tissue damage | 7 | 1.9 | - | - | |
| Traumatic brain injury | 5 | 1.4 | 1 | 5.9 | |
| Sprain | 4 | 1.1 | - | - | |
| Abrasion | 2 | 0.6 | - | - | |
| Laceration | 1 | 0.3 | - | - | |
| Eye injury | 1 | 0.3 | - | - | |
| Injury to nerve | 1 | 0.3 | - | - | |
| Other or none detected | 3 | 0.8 | - | - | |
Ages 17 years old and younger.
Disposition information missing for eight BTI cases and two TPI cases.
The three leading mechanisms were selected to report for each body part, information regarding additional mechanisms was collapsed into the ‘other mechanism’ category.
BTI Backyard trampoline injury; ED emergency department; GP General practitioner; PRN pro re nata or as needed; TPI Trampoline park injury.
Records entered on or before August 24, 2016.
Type of injury
The type of injury varied based on the type of trampoline. Sprains were more common on TPIs (32.9% in TPIs and 16.8% for BTIs, P<0.01), while traumatic brain injuries (TBI) (3.2% for TPI and 5.2% for BTIs, P=0.04), fractures (35.5% for TPIs and 43.7% for BTIs, P<0.01), soft tissue injury and lacerations (2.8% for TPIs and 5.1% for BTIs, P=0.02,) were more frequent with BTIs. There was no significant difference in the occurrence of dental and eye injuries (dental: n=2 for TPI and n=45 for BTI, P=0.73, eye: n=2 for TPI and N=25 for BTI, P=0.23). Dislocations and abrasions were not significantly associated with either type of trampoline. Figure 3d shows the age- and sex-adjusted odds of each type of injury among TPIs relative to BTIs. All but one case of intracranial injury occurred among BTIs (n=2 for BTI and n=1 for TPI), with two of the three occurring due to contact of the head with a knee (data not shown). Among spinal fracture cases (n=7 for BTI and n=1 for TPI), two cases were severe enough to require hospital admission, while for intracranial injury, one case required admission.
Disposition
BTIs resulted in more hospital admissions than TPIs (6.6%, n=360 for BTI and 3.0%, n=17 for TPI, P<0.01), with fractures accounting for the majority of admissions (64.7% for TPIs and 90.6% for BTIs). Other types of injuries that resulted in hospital admission include dislocation (11.8% for TPIs and 2.8% for BTIs), injury to internal organ (17.7% for TPI), soft tissue damage (1.9% for BTI) and TBIs (5.9% for TPIs and 1.4% for BTIs).
DISCUSSION
Trampoline injuries continue to increase in Canada (4,10) in spite of the introduction of new measures, such as springfree trampolines and recommendations for the use of safety nets. The age distribution of trampoline injuries highlights the paediatric nature of this type of unintentional injury (1,2). While the difference is modest, it appears that injuries occur more frequently among females for both types of trampoline (BTIs and TPIs), as is similar in Ireland (14), in contrast to reports from the USA (5), Norway (15) and Australia (16). Falls and injuries involving contact with another jumper or surface were more frequent among BTIs, while injuries related to impact with the trampoline bed were more frequent with TPIs. LE injuries were more common among TPIs relative to BTIs, while UE, trunk and facial injuries were more common among BTIs. Finally, sprains were the type of injury more frequently associated with TPIs, while lacerations and soft tissue injuries were more frequent among BTIs. Although cases admitted to the hospital are increasing regardless of trampoline type, it is noteworthy that this tendency is higher for BTI cases.
Historically (17), trampoline injuries often related to an individual falling off a trampoline or making contact with exterior surfaces. The frequency of such injuries resulted in the development of voluntary standards to include safety enclosures for backyard trampolines (8) and in the adoption of the new springfree or soft-edge trampoline formats (9), which are most frequently seen in trampoline parks. Nevertheless, trampoline injuries persist. The various characteristics of trampoline injury described in this study can be associated with some of the same concerns that existed prior to the introduction of these newer safety measures, but others have been shown to relate to newer iterations of trampoline design and low adoption of safety recommendations.
Examining LE injuries, for instance, there is a clear likelihood of such injuries occurring at trampoline parks relative to backyard trampolines. This can be partially explained by the structural differences between the two settings. Backyard trampolines are fitted with beds with lower tensile strength, producing a softer bounce and less pressure on an individual’s joints, while trampoline parks use springfree formats, which use beds with higher tension. The benefit of the latter includes that it does away with exposed springs, which were previously a source of lacerations. However, an explanation for the higher observed frequency (5,7) of LE TPIs is the tensile strength of their trampoline beds (5,7). They are thought to result in a more jarring stop, thereby increasing the load on an individual’s joints (18). By contrast, it appears that spring-based trampolines continue to cause laceration injuries; springfree trampolines are more common in trampoline parks, so the higher likelihood of lacerations with BTIs relative to TPIs may be due to exposed springs or surfaces proximal to such trampolines. UE injuries were more frequent among BTIs, which may be associated with the fact that despite conflicting reports on the effectiveness of safety nets, their use is not always adhered to (9,16). The absence, or faulty functioning, of a safety net on a backyard trampoline can result in cases where an individual falls off of the trampoline onto surfaces like cement (8). By comparison, trampoline parks use wall-to-wall trampolines and padding so as to reduce the number of similar falls from the trampoline or impact injuries.
Position statements regarding the safe use of trampolines (1,2) caution against risky behaviours that could result in injury, such as with having multiple people on the trampoline, trying stunts or not having adequate supervision (19). Our findings demonstrate that these issues persist. When performing stunts such as a somersault, for instance, hyperflexion injuries leading to cervical spine injury are a possibility (20) and can result in neurological consequences (14,20). Having more than one individual on a trampoline can result in injuries via making contact with another individual or through energy transferred from a ‘double bounce’ (i.e., the energy transferred between two or more jumpers, resulting in a higher load on their bones and ligaments) (21). One study estimated that a lighter child has a 14-fold increased risk of being injured when on a trampoline with a heavier child (14).
While severe trampoline injuries are rare, severe cases can be detrimental. For example, cervical spine injuries hold a high risk of severe outcomes, and they made up the largest proportion of spinal injuries observed in our study. Paraplegia, quadriplegia and even death are possible, although rare, outcomes of such trampoline injuries (22). While similar estimates were not available for Canada, trampolines were responsible for more than 6500 paediatric cervical spine injuries in 1998 in the USA (22).
Limitations
The injuries described in our study are not representative of all injuries in Canada, only to those presenting to participating emergency departments. However, eCHIRPP includes all Canadian paediatric EDs, and some general EDs, and should therefore provide good coverage of paediatric injury. A number of studies have indicated that patterns observed in studies using CHIRPP are representative of the Canadian context (23,24).
In addition to older teens, Aboriginal persons, people who live in rural areas and fatal cases are under-represented in eCHIRPP.
CONCLUSION
In spite of statements regarding the safe use of trampolines, injuries continue to rise in Canada. Trampoline parks present a similar risk of injury as backyard trampolines, but the mechanism and location of injury varies. Based on a comparison of TPIs with BTIs, the former appears to be confounded by harder mats while the latter is confounded by factors such as surrounding surfaces or additional jumpers. As this recreational activity grows in popularity, and broadens its venues for activity, ongoing surveillance will help to inform our understanding of potential risks and assist with injury prevention efforts.
References
- 1. Canadian Paediatric Society. Trampoline use in homes and playgrounds. Paediatr Child Health 2007;12:501–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Briskin S, LaBotz M; Council on Sports Medicine and Fitness, American Academy of Pediatrics Trampoline safety in childhood and adolescence. Pediatrics 2012;4:775–9. [DOI] [PubMed] [Google Scholar]
- 3. Briskin S, LaBotz M; Council on Sports Medicine and Fitness, American Academy of Pediatrics Trampoline safety in childhood and adolescence - reaffirmed. Pediatrics 2015; (5):136. [DOI] [PubMed] [Google Scholar]
- 4. McFaull S. Injuries associated with backyard trampoline use, Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP), 1999–2003. Paediatr Child Health 2007;12 (Suppl A):55A. [Google Scholar]
- 5. Kasmire KE, Rogers SC, Sturm JJ. Trampoline park and home trampoline injuries. Pediatrics 2016; 138(3). [DOI] [PubMed] [Google Scholar]
- 6. Saunders P. Launching Sky Zone Indoor Trampoline Park http://www.franchiseinfo.ca/features/launching-sky-zone-indoor-trampoline-park/ (Accessed August 27, 2016).
- 7. Mulligan CS, Adams S, Brown J. Paediatric injury from indoor trampoline centres. Inj Prev 2017;23(5):352–4. [DOI] [PubMed] [Google Scholar]
- 8. Alexander K, Eager D, Scarrott C, Sushinsky G. Effectiveness of pads and enclosures as safety interventions on consumer trampolines. Inj Prev 2010;16(3):185–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eager DB, Scarrott C, Nixon J, Alexander K. Injury survey of a non-traditional ‘soft-edged’ trampoline designed to lower equipment hazards. Int J Inj Contr Saf Promot 2013;20(1):42–9. [DOI] [PubMed] [Google Scholar]
- 10. Health Surveillance and Epidemiology Division, Public Health Agency of Canada. Injuries associated with Backyard Trampolines: Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP) database 1999–2003 (cumulative to February 2006). All ages, 2,705 records. Update 2004–2006, 1749 cases http://www.phac-aspc.gc.ca/injury-bles/chirpp/injrep-rapbles/pdf/trampolines-eng.pdf (Accessed August 29, 2016).
- 11. Mackenzie SG, Pless IB. CHIRPP: Canada’s principal injury surveillance program. Canadian hospitals injury reporting and prevention program. Inj Prev 1999;5(3):208–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Crain J, McFaull S, Thompson W, et al. . Status report - the Canadian hospitals injury reporting and prevention program: A dynamic and innovative injury surveillance system. Health Promot Chronic Dis Prev Can 2016;36(6):112–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhang Y. Perl regular expression in SAS macro programming. SAS Global Forum 2011;159–2011:1–7. [Google Scholar]
- 14. Hurson C, Browne K, Callender O, et al. . Pediatric trampoline injuries. J Pediatr Orthop 2007;27(7):729–32. [DOI] [PubMed] [Google Scholar]
- 15. Nysted M, Drogset JO. Trampoline injuries. Br J Sports Med 2006;40(12):984–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ashby K, Pointer S, Eager D, Day L. Australian trampoline injury patterns and trends. Aust N Z J Public Health 2015;39(5):491–4. [DOI] [PubMed] [Google Scholar]
- 17. McFaull S, Subaskaran J, Branchard B, Thompson W. Emergency department surveillance of injuries and head injuries associated with baseball, football, soccer and ice hockey, children and youth, ages 5 to 18 years, 2004 to 2014. Health Promot Chronic Dis Prev Can 2016;36(1):13–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Springfree. Towards trampolines without injury. SpringFree Trampoline White Paper 2005; v 1.02 http://www.springfreetrampoline.com/sites/springfreetrampoline.com/files/files/pdf/whitepaper_springfree_2007.pdf [Google Scholar]
- 19. Wootton M, Harris D. Trampolining injuries presenting to a children’s emergency department. Emerg Med J 2009;26(10):728–31. [DOI] [PubMed] [Google Scholar]
- 20. Leonard H, Joffe AR. Children presenting to a Canadian hospital with trampoline-related cervical spine injuries. Paediatr Child Health 2009;14(2):84–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Menelaws S, Bogacz AR, Drew T, Paterson BC. Trampoline-related injuries in children: A preliminary biomechanical model of multiple users. Emerg Med J 2011;28(7):594–8. [DOI] [PubMed] [Google Scholar]
- 22. Brown PG, Lee M. Trampoline injuries of the cervical spine. Pediatr Neurosurg 2000;32(4):170–5. [DOI] [PubMed] [Google Scholar]
- 23. Kang J, Hagel B, Emery CA, Senger T, Meeuwisse W. Assessing the representativeness of Canadian hospitals injury reporting and prevention programme (CHIRPP) sport and recreational injury data in Calgary, Canada. Int J Inj Contr Saf Promot 2013;20(1):19–26. [DOI] [PubMed] [Google Scholar]
- 24. Pickett W, Brison RJ, Mackenzie SG, et al. . Youth injury data in the Canadian hospitals injury reporting and prevention program: Do they represent the Canadian experience?Inj Prev 2000;6(1):9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]