WHY DON’T PAEDIATRICIANS AND FAMILY DOCTORS SCREEN FOR ADVERSE CHILDHOOD EXPERIENCES?
The adverse childhood experiences (ACEs) screening instrument is a validated, accessible screening tool that can be used for early detection of common childhood traumas. Modifications to the original adult questionnaire have been made in paediatric practices so that the questions are appropriately phrased for asking children and youth directly about their experiences (1,2) (Figure 1), but the 10 specific ACE exposures remain the same in the adult and child questionnaires. As Jacob et al. note, ACEs are common and toxic to children, with lifelong impacts on their neuroendocrine, inflammatory, immune, metabolic, and other physiologic systems (3). ACEs meet evidence-based criteria for screening: they are prevalent, detectible, and their associated conditions have evidence-based early interventions. However, most paediatricians and family doctors do not routinely screen for ACEs. This is termed a ‘knowledge-to-action gap’, where the research evidence has not yet changed standard clinical practice. This is due in part to perceived barriers that doctors may have regarding ACEs. For example, paediatricians and family physicians may view ACEs as psycho-social, or strictly in the domain of mental health, and thus outside of their expertise. They may also feel under-prepared to address possible traumas, or concerned that there is no effective response to the clinical ‘can of worms’ they’ve opened by screening for ACEs (4).
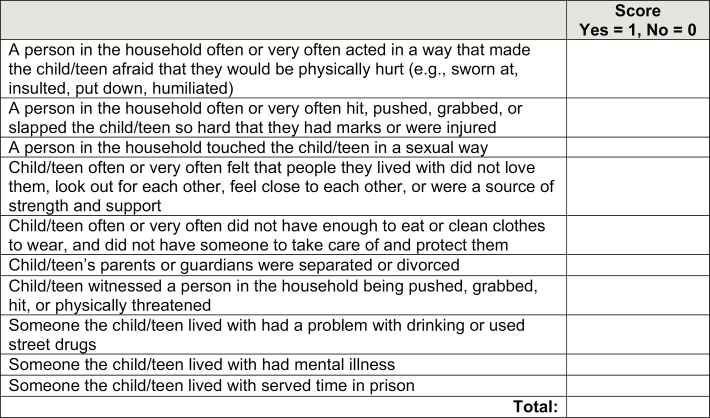
Figure 1.
ACE Questionnaire, adapted for use in paediatric practice (1,2). Sources: Center for Youth Wellness, ACEs Too High (https://acestoohigh.com/got-your-ace-score/).
Reassuringly, the emerging literature on ACEs screening tells us that it is not a time-consuming process and does not require extensive mental health training. Sensitive and effective screening can be integrated into a routine clinical appointment in approximately 10 minutes. Parents report that ACEs screening is acceptable and helpful to their children’s care (5), and addressing ACEs in standard paediatric care affords an opportunity to improve health outcomes for children (6). Therefore, despite perceived barriers, paediatricians and family doctors are well-positioned to screen for ACEs, just as they screen for other childhood health concerns (7).
How to screen
Screening for ACEs involves asking children and their caregivers about exposures to the emotional stresses known to impact their health. Screening with these 10 yes/no questions generates the child’s ‘ACE Score’, by giving one point for each ‘yes’ answer. This ACE score then informs treatment planning for child and family, as follows:
- Parent and child answer the ACE questions.
- Explain the rationale for the questionnaire and limits of confidentiality: Physicians can explain that certain stresses are known to increase children’s risk for illness across their lives. Note that these questions are now being asked of all patients to identify these stresses early and help reduce them. Explain that their answers are confidential, except in those cases where the child is at risk of serious harm from abuse or neglect.
- Complete the questionnaire: This can be done by the parent and child/youth each filling out the ACE 10-item questionnaire with their physician, or answering verbally in the clinical meeting. Both children and their parents should be asked about the child’s ACEs separately. For clarity and accuracy, children under the age of 12 can answer the questions verbally, asked by their doctor. Differences in how parents and children answer the questions can be addressed in the meeting, as parents may not be aware of their child’s perceptions, or one or the other may under-report the stresses present in the family. For instructional videos on quick ACEs screening with parent and child, see: www.porticonetwork.ca/web/childhood-trauma-toolkit/developmental-trauma/how-does-it-present
-
Discuss the results. Reviewing and explaining the significance of the ACE score is an essential part of the process. Engaging nonjudgmentally with parent and child is important to maintaining your treatment alliance, and taking a stance that emphasizes collaboration and support is central to trauma-informed care. Physicians should explain to parents that early intervention can reduce these ACE stresses. Describing the intervention as an investment in the child’s lifelong physical and mental health may help reduce perceived stigma around the results of the screen, and increase engagement (5). Link the ACE score to any health concerns the child may currently have, emphasizing that addressing ACEs will help regulate the child’s health by lowering stress hormones, and could therefore improve health and learning (2). If Child Protective Services must be notified, discuss this with the parent as an effort to assist the family and ensure the long-term health of the child.
Sample scripts for how to discuss the ACE score can be found at: centerforyouthwellness.org/advancing-clinical-practice/
Collaborate on treatment planning. As part of the discussion with parent and child, physicians can tailor their recommendations to the child’s specific ACE score, for example recommending that a parent obtain treatment for their own mental health or substance use, or referring for family therapy. Paediatricians and family physicians might not conduct the treatment interventions themselves, but in their roles as service gate-keepers and treatment-planners, they can use the ACEs data to make appropriate referrals. Evidence-based interventions to address ACEs include parenting therapy, individual psychotherapies, and treatment of parental mental health and substance use concerns, among others.
Revisit the ACE score. Periodically redoing the ACE questionnaire with parents and children will assist in monitoring the effectiveness of treatment interventions and ensuring that risk factors are being addressed.
Financial disclosure: There are no financial relationships relevant to this paper.
Potential Conflicts of Interest
All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. The Childhood Trauma Toolkit. Year accessed 2018. <https://www.porticonetwork.ca/web/childhood-trauma-toolkit/tools>.
- 2. Centre for Youth Wellness. Year accessed 2018. <https://centerforyouthwellness.org/cyw-aceq/> (sign up required to access resource).
- 3. Jacob G, Heuvel Mvd, Jama N, Moore AM, Ford-Jones L, Wong PD. Adverse childhood experiences: Basics for the paediatrician. Paediatr Child Health. <https://academic.oup.com/pch/advance-article-abstract/doi/10.1093/pch/pxy043/4961508?redirectedFrom=fulltext> [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kerker BD, Storfer-Isser A, Szilagyi M, et al. . Do pediatricians ask about adverse childhood experiences in pediatric primary care?Acad Pediatr 2016;16(2):154–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gillespie RJ, Folger AT. Feasibility of assessing parental ACEs in pediatric primary care: Implications for practice-based implementation. J Child Adolesc Trauma 2017;10(3):249–256. [Google Scholar]
- 6. Kerker BD, Zhang J, Nadeem E, et al. . Adverse childhood experiences and mental health, chronic medical conditions, and development in young children. Acad Pediatr 2015;15(5):510–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Johnson SB, Riley AW, Granger DA, Riis J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics 2013;131(2):319–27. [DOI] [PMC free article] [PubMed] [Google Scholar]