Abstract
Purpose
When using tension band plates for angular deformity correction, the literature is unclear regarding the most effective screw insertion angle to use. This study evaluates the correlation between initial screw angle and the average rate of correction during hemiepiphysiodesis using tension band plates
Methods
This retrospective study includes 35 patients (47 physes) with genu valgum deformity (17 idiopathic and 18 fibular hemimelia) who underwent insertion of Eight-Plates between 2010 and 2015. Initial screw angle was determined from the intraoperative fluoroscopic images. Radiographs were obtained within three months of surgery, and follow-up films were obtained every three to six months. Change in mechanical lateral distal femoral angle, medial proximal tibial angle and screw angle was obtained from each follow-up radiograph. Initial screw angle was correlated with the average rate of correction during the entire treatment period. The average rate of angular correction during first and last follow-up periods was also compared.
Results
The relationship between the initial screw angle and the mean rate of angular correction was not statistically significant (p = 0.2). The rate of angular correction during the first follow-up period (mean of 4.7 months) was 0.86° per month compared with 0.71° per month during the last follow-up period (mean of 5.1 months).
Conclusion
Application of a tension band plate with a divergence angle ranging from 0° to 30° results in similar rates of angular correction. For surgeons inserting screw-plate tension band devices, there does not seem to be any necessity to make the screws parallel or divergent. We recommend that screw placement be anatomically correct, i.e. not impinging on the physis, rather than favouring any particular divergence angle.
Level of evidence
IV
Keywords: tension band plate, rate of correction, screw angle, initial screw angle, growth modulation, guided growth
Introduction
Hemiepiphysiodesis is widely used as a method for gradual correction of angular deformities in skeletally immature patients.1-9 The rate of angular correction with hemiepiphysiodesis is an area of interest for many researchers.10-15 Because clinicians are often faced with angular deformity patients who are approaching skeletal maturity, it may be important to know which technique provides the most effective correction in the shortest amount of time. Stevens (2007)3 reported a 30% faster rate of correction using the Eight-Plate (Orthofix, Lewisville, Texas) compared with Blount staples (Stryker Howmedica, Kiel, Germany). This was confirmed in an experimental study on pigs.14 However, other studies observed a faster correction using Blount staples,15,16 suggesting that Blount staples cause immediate tethering, while the Eight-Plate only becomes effective a few months after insertion. Burghardt et al17 hypothesized in 2011 that the slower rate using the Eight-Plate could be explained by the time taken for the screws to diverge with growth until full engagement with the plate, after which the device behaves more like a rigid fixed angle device similar to a staple. They suggest that the rate of correction starts slowly due to the slack in the system until the screws diverge and engage the plate. Based on this hypothesis, a faster correction should be expected when the tension band plate screws are prepositioned in divergence. In a biomechanical study by Schoenleber et al,18 parallel screws achieved faster correction compared with divergent screws, seemingly contradicting the hypothesis suggested in the Burghardt et al.17 study.
Due to the conflicting findings in the literature, the aim of this retrospective study is to investigate in a clinical series the correlation between the initial screw angle and the rate of correction in patients with genu valgum. To our knowledge, this is the first clinical study to evaluate this correlation.
Materials and methods
This retrospective study included 47 physes treated with Eight-Plates in 35 patients between 2010 and 2015. To reduce sample bias, only genu valgum deformities were chosen for the study. Patients with sagittal plane deformities or who had concomitant osteotomies for acute or gradual correction using external or internal fixation were also excluded. All patients had a preoperative radiograph within three months after surgery and had follow-up films every three to six months. In all, 17 patients (28 physes) had idiopathic genu valgum and another 18 patients (19 physes) had genu valgum associated with fibular hemimelia.
From the preoperative radiograph, the mechanical lateral distal femoral angle (mLDFA) and the medial proximal tibial angle (MPTA) were noted. The initial screw angle was noted from the fluoroscopy image taken during surgery. The mLDFA, MPTA and screw angle were noted in each follow-up radiograph.
The rate of correction was calculated at the first follow-up period (change in angular correction (°)/first follow-up period (months)) and the last follow-up period (change in angular correction at last follow-up (°)/last follow-up period (months)). The follow-up periods were typically from three to six months.
A regression analysis and a correlation graph were drawn using IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, New York).
Results
The mean total follow-up period was 12.2 months (7 to 25). The mean age at the time of surgery was 11 years (3 to 15), and the initial screw angle ranged from 0° to 30°. In all, 25 physes were in female patients and 22 were in male patients. A total of 39 had medial distal femoral hemiepiphysiodesis and eight were treated with medial proximal tibial hemiepiphysiodesis. In the idiopathic group, medial distal femoral hemiepiphysiodesis was done for 21 physes while medial proximal tibial was done for seven physes. In the fibular hemimelia group, medial distal femoral hemiepiphysiodesis was done in 18 physes and medial proximal tibial was done for a single case.
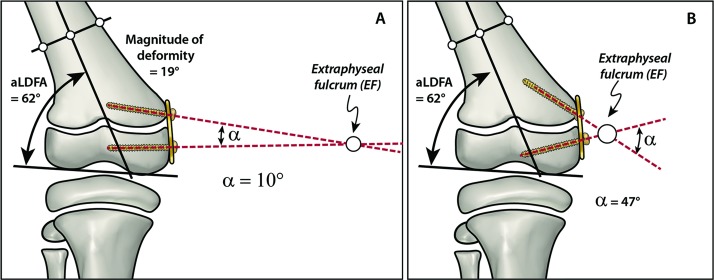
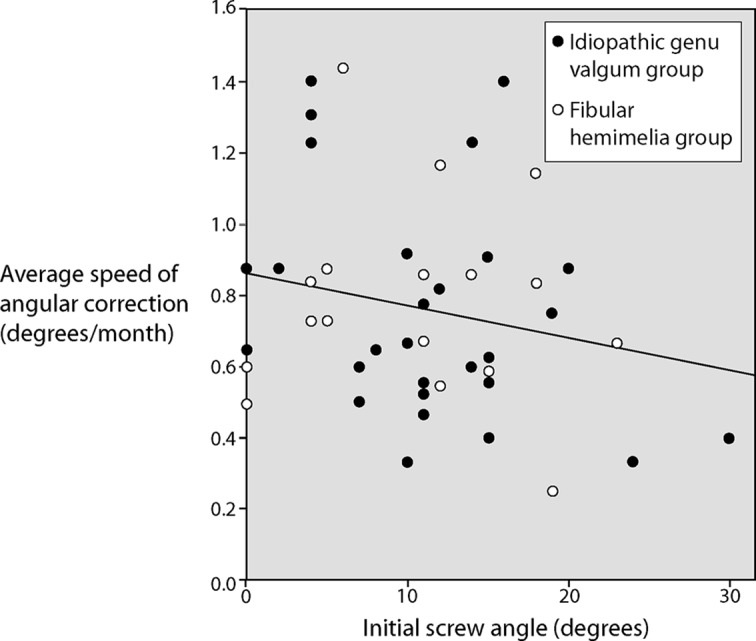
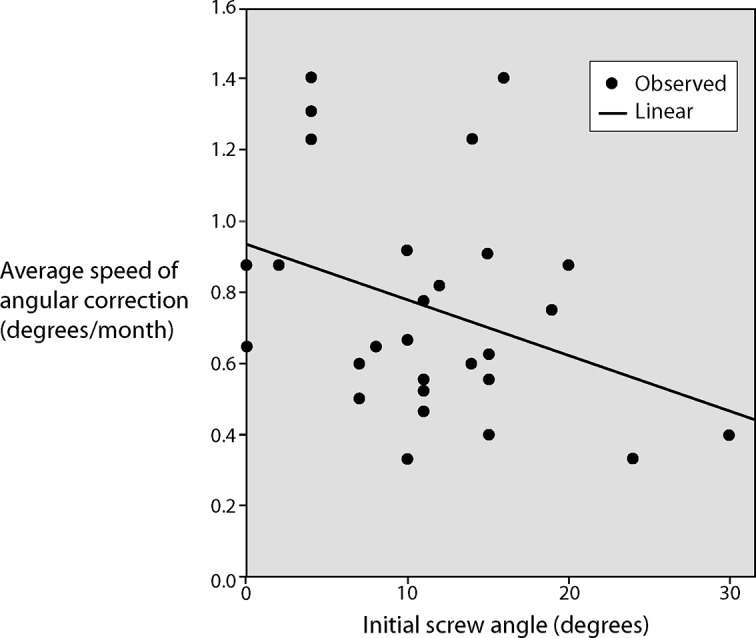
The results showed a trend towards a negative correlation between the initial screw angle and the rate of correction with a p-value of 0.2 (Fig. 1). To eliminate confounding bias, the correlation was again repeated for the idiopathic genu valgum group (Fig. 2) and the fibular hemimelia group (Fig. 3). The idiopathic group showed negative correlation, while the fibular hemimelia group showed almost no correlation. While the negative correlation suggests that a greater initial screw angle gives a slower correction, the results were neither clinically nor statistically significant. The mean rate of angular correction (change in correction/month) was 0.74° per month (0.3° to 1.4°; sd 0.31°).
Fig. 1.
Correlation between initial screw angle and mean rate of angular correction shows a non-significant negative correlation: p = 0.2; R square = 0.044. (Copyright 2019, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)
Fig. 2.
Correlation between initial screw angle and mean rate of angular correction in the idiopathic genu valgum group shows a non-significant negative correlation: p = 0.81; R square = 0.112. (Copyright 2019, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)
Fig. 3.
Correlation between initial screw angle and mean rate of angular correction in the fibular hemimelia group shows a non-significant negative correlation: p = 0.97; R square = 0.00. (Copyright 2019, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)
The mean rate of correction for the first follow-up period, with a mean follow-up of 4.7 months (2.8 to 5.9), was 0.86° per month (0° to 2.3°; sd 0.45), while the mean rate of correction during the last follow-up period, with a mean follow-up of 5.1 months (3.1 to 6.7), was 0.71° per month (0.3° to 1.7°; sd 0.33). There was no statistical significance between these results (p = 0.18).
Discussion
Although we hypothesized that using a wider initial screw angle would result in faster angular correction, this was generally not seen. It has previously been suggested that divergent screws engage the plate more rigidly, thus tethering the physis more efficiently. However, the results of this study showed a negative correlation between initial screw angle and rate of correction. In other words, tension band plates with a narrow initial screw angle corrected faster.
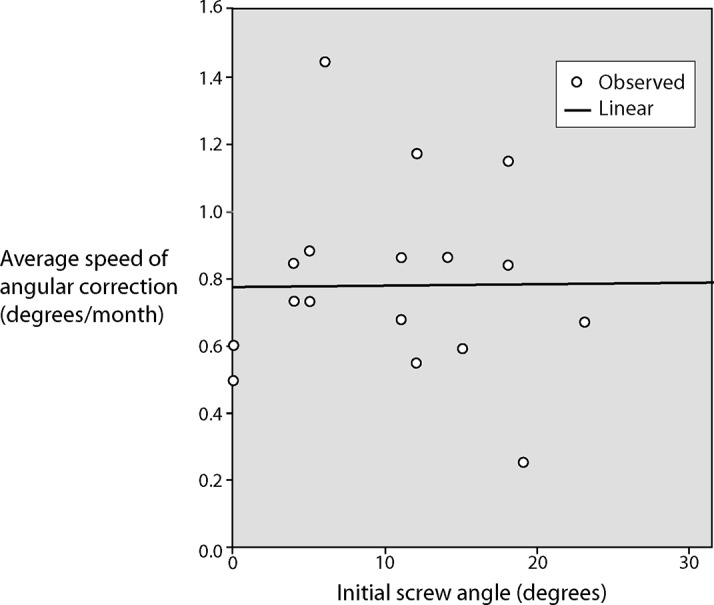
A possible explanation for this finding could be Steven’s theory that the tension band plate creates an extra-physeal fulcrum.3 Figure 4 illustrates the extra-articular fulcrum (marked in the figures with a small white circle) created by a narrow screw angle (Fig.4a) versus a wide screw angle (Fig. 4b). The fulcrum that is closer to the growth plate would seem to correct faster, but our data did not bear this out.
Fig. 4.
The two main scenarios for angular correction: (A) narrow screw angle shows that the two lines from the screws along their axis creates an extraphyseal fulcrum far from the physis; (B) wide screw angle shows that the extension of lines from the screws creates an extraphyseal fulcrum closer to the physis. aLDFA, anatomic lateral distal femoral angle. (Copyright 2019, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)
The biomechanical study by Schoenleber et al18 investigated the influence of screw configuration on angular correction. The authors used a plastic bone model of angular correction using an Eight-Plate with different screw angles: parallel, divergent and hyper divergent screws. An osteotomy was performed at the physis and a monorail fixator was mounted posteriorly in the sagittal plane using two half-pins in the shaft and one half-pin in the epiphysis. According to the authors’ protocol, care was taken to place the half-pin in the centre of the epiphysis. The angular correction was measured at 5 mm, 10 mm and 15 mm of distractions. The study showed more statistically significant angular correction in the models with parallel screws compared with the models with divergent screws. Comparisons with hyper divergent screws were statistically insignificant.
Other studies demonstrated slow early correction using Eight-Plate.17 There may be a brief lag for physes with parallel screws. When the screws first begin diverging, an extraphyseal fulcrum is formed and the maximum rate of correction begins. Alternatively, there may be ‘slack’ in the screw-plate mechanism that needs to be taken up before correction can commence.
We initially thought that the latency sometimes observed with tension band plates is due to the time it takes for the screws to diverge and engage the plate. In addition, a study by Ballal et al,4 indicates that due to its inherent flexibility, the plate seems to bend even before the screws reach maximum divergence.
The results of this clinical study illustrate that the proposed theory of an imaginary extraphyseal fulcrum changing the rate of correction may not necessarily be valid. As angular correction proceeds, the tension band plate screws continue to diverge, moving the imaginary extraphyseal fulcrum closer to the bone. The mean rate of angular correction calculated for the first follow-up period was 0.86° per month compared with the mean rate calculated for the last follow-up, which was 0.71° per month. This difference in rate, however, was not significant (p = 0.18). The change in the rate of correction was probably not related to any decrease in the patient’s growth rate since the mean follow-up was only 12.2 months and the study included patients as young as age three years.
There are certain limitations in this study. The number of cases may be insufficient to unveil the difference between different screw divergences. Furthermore, it is known that the rate of growth in children approaching adolescence changes. Top rates of growth around the knee occur in boys age 13 years and girls age 11 years, and slow down after that.19 Other factors may come into play, including the distance between the holes in the Eight-Plate (12 mm versus 16 mm) and the different screw lengths available for use. Perhaps this could be a topic for finite element analysis to further investigate the effects of screw and plate geometry and size on rate of correction.
Conclusion
The initial screw angle (0° to 30°) does not appear to significantly influence the rate of correction in hemiepiphysiodesis when using tension band plates. We recommend that surgeons insert the screws in such devices according to anatomic restrictions, to avoid the growth plate, rather than favouring parallel, divergent or widely divergent configurations.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: In this retrospective study, medical records of human patients were reviewed after approval was obtained from the institutional review board.
Informed consent: For this type of study, formal consent is not required
ICMJE Conflict of interest statement
JEH is a paid consultant for OrthoPediatrics, Orthofix, NuVasive Specialized Orthopedics, Smith & Nephew and Wishbone Medical.
CAI is a paid consultant for Orthofix, NuVasive Specialized Orthopedics and Smith & Nephew.
HHE has nothing to disclose.
Author Contributions
HHE: Collected the data, analysed and interpreted the data, wrote the manuscript.
CAI: Analysed and interpreted the data, reviewed and edited the manuscript.
JEH: Designed the study, analysed and interpreted the data, reviewed and edited the manuscript.
References
- 1.Burghardt RD, Herzenberg JE, Standard SC, Paley D. Temporary hemiepiphyseal arrest using a screw and plate device to treat knee and ankle deformities in children: a preliminary report. J Child Orthop 2008;2:187-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shabtai L, Herzenberg JE. Limits of growth modulation using tension band plates in the lower extremities. J Am Acad Orthop Surg 2016;24:691-701. [DOI] [PubMed] [Google Scholar]
- 3.Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop 2007;27:253-259. [DOI] [PubMed] [Google Scholar]
- 4.Ballal MS, Bruce CE, Nayagam S. Correcting genu varum and genu valgum in children by guided growth: temporary hemiepiphysiodesis using tension band plates. J Bone Joint Surg [Br] 2010;92-B:273-276. [DOI] [PubMed] [Google Scholar]
- 5.Bowen JR, Leahey JL, Zhang ZH, MacEwen GD. Partial epiphysiodesis at the knee to correct angular deformity. Clin Orthop Relat Res 1985;198:184-190. [PubMed] [Google Scholar]
- 6.Danino B, Rödl R, Herzenberg JE, et al. . Guided growth: preliminary results of a multinational study of 967 physes in 537 patients. J Child Orthop 2018;12:91-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stevens PM, Klatt JB. Guided growth for pathological physes: radiographic improvement during realignment. J Pediatr Orthop 2008;28:632-639. [DOI] [PubMed] [Google Scholar]
- 8.Blount WP, Clarke GR. Control of bone growth by epiphyseal stapling; a preliminary report. J Bone Joint Surg [Am] 1949;31-A:464-478. [PubMed] [Google Scholar]
- 9.Marangoz S, Buyukdogan K, Karahan S. Is there a correlation between the change in the interscrew angle of the eight-plate and the delta joint orientation angles? Acta Orthop Traumatol Turc 2017;51:39-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar A, Gaba S, Sud A, et al. . Comparative study between staples and eight plate in the management of coronal plane deformities of the knee in skeletally immature children. J Child Orthop 2016;10:429-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gottliebsen M, Rahbek O, Hvid I, et al. . Hemiepiphysiodesis: similar treatment time for tension-band plating and for stapling: a randomized clinical trial on guided growth for idiopathic genu valgum. Acta Orthop 2013;84:202-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wiemann JM IV, Tryon C, Szalay EA. Physeal stapling versus 8-plate hemiepiphysiodesis for guided correction of angular deformity about the knee. J Pediatr Orthop 2009;29:481-485. [DOI] [PubMed] [Google Scholar]
- 13.Jelinek EM, Bittersohl B, Martiny F, et al. . The 8-plate versus physeal stapling for temporary hemiepiphyseodesis correcting genu valgum and genu varum: a retrospective analysis of thirtyfive patients. Int Orthop 2012;36:599-605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kanellopoulos AD, Mavrogenis AF, Dovris D, et al. . Temporary hemiepiphysiodesis with blount staples and eight-plates in pigs. Orthopedics 2011;344:263. [DOI] [PubMed] [Google Scholar]
- 15.Goyeneche RA, Primomo CE, Lambert N, Miscione H. Correction of bone angular deformities: experimental analysis of staples versus 8-plate. J Pediatr Orthop 2009;29:736-740. [DOI] [PubMed] [Google Scholar]
- 16.Burghardt RD, Herzenberg JE. Temporary hemiepiphysiodesis with the eight-Plate for angular deformities: mid-term results. J Orthop Sci 2010;15:699-704. [DOI] [PubMed] [Google Scholar]
- 17.Burghardt RD, Kanellopoulos AD, Herzenberg JE. Hemiepiphyseal arrest in a porcine model. J Pediatr Orthop 2011;31:e25-e29. [DOI] [PubMed] [Google Scholar]
- 18.Schoenleber SJ, Iobst CA, Baitner A, Standard SC. The biomechanics of guided growth: does screw size, plate size, or screw configuration matter? J Pediatr Orthop B 2014;23:122-125. [DOI] [PubMed] [Google Scholar]
- 19.Anderson M, Green WT, Messner MB. Growth and predictions of growth in the lower extremities. J Bone Joint Surg [Am] 1963;45-A:1-14. [PubMed] [Google Scholar]