Abstract
Purpose
Reliable radiographic measurement techniques are important for investigating limb alignments prior to and following paediatric anterior cruciate ligament (ACL) reconstruction. We investigated the inter- and intraobserver reliability of alignment measurements from lower extremity anteroposterior and lateral radiographs of adolescents having undergone transphyseal ACL reconstruction
Methods
A total of 15 of 90 patients who had undergone transphyseal ACL reconstruction were randomly selected for alignment measurements of radiographs of operative and nonoperative limbs. Radiographs were de-identified, randomized to three varying sequences and made available in electronic format to three blinded investigators: a junior orthopaedic resident, a senior orthopaedic resident and a paediatric orthopaedic attending. Coronal measurements comprised the mechanical lateral distal femoral angle (mLDFA), mechanical medial proximal tibial angle (mMPTA) and mechanical axis deviation (MAD), measured from standing teleoroentgenograms of the lower extremities. Tibial slope was measured on lateral knee radiographs of operative limbs. The intra-class correlation coefficient (ICC) was calculated for each of the three coronal measures and for tibial slope.
Results
Intraobserver reliability was excellent across all measures (ICC > 0.75) except for tibial slope in one investigator’s measurements (good or ICC = 0.68 for the operative limbs) and mLDFA in another investigator’s measurements (fair or ICC = 0.49 for the operative limbs, and poor ICC = 0.27 for the nonoperative limbs). Interobserver reliability was excellent across all investigators for all measurements for operative and nonoperative limbs.
Conclusions
Radiographic measurements of lower extremity alignment may be reliably measured on teleoroentgenograms in a subset of youth who underwent transphyseal ACL reconstruction.
Level of Evidence
III
Keywords: interobserver reliability, radiographic measurement, transphyseal anterior cruciate ligament reconstruction, paediatric sports, picture archiving and communication system
Introduction
The prevalence of anterior cruciate ligament (ACL) tears in youth athletes is on the rise at rates greater than that seen in adult populations.1 ACL injuries account for 20% of all knee injuries reported in high school athletes,2 the majority of which may lead to surgery. Despite the risk of growth abnormalities resulting from ACL reconstruction in growing patients, the greater risk of chondral and meniscal injury from delays in treatment3-5 may lead more surgeons to perform these procedures. Between 2000 and 2009, the rate of ACL reconstruction in youths aged 11 to 18 years of age more than doubled.6 Following a patient’s growth after ACL reconstruction is imperative, as surgery near or through open epiphyseal growth plates may lead to growth arrests and limb malalignment independent of the surgical technique.7,8 Faunø et al9 report a 24% rate of radiographic growth disturbance after transphyseal ACL reconstruction despite the reported markedly lower rate of clinically evident deformity identified within that study. The paucity of data may be due in part to under-collection of postoperative radiographic measures.10 Early detection enables early treatment when corrective interventions may be the most efficacious and least risky to the patient.11
Digital radiography offers many advantages over hard-copy systems, including the portability of images, reduced patient exposure to ionizing radiation,12 the ability to produce images with a minimum of disposable resources and ease of storage of images. Software typically offers scalable, high-quality images of radiographic records stored in the cloud, as well as electronic tools that may simplify analysis of images.13 The reliability of commonly employed tools available with software to precisely measure coronal and sagittal plane limb alignments in the growing child has been reported.14 To our knowledge, however, the reliability of such measurements in growing children undergoing ACL reconstruction has not been reported.
Here we examine the inter- and intraobserver reliability of measurements of lower-limb alignments performed by two orthopaedic residents (AOO and AFB) and an orthopaedic attending surgeon (GAS) using digital radiographs and the tools of a single picture archiving and communication system (PACS) in children and adolescents who underwent transphyseal ACL reconstruction. This was performed using a standard set of instructions and as a precursor to a study of limb alignments in a larger population of such patients. We hypothesized that there would be high reliability across examiners for coronal and sagittal plane radiographic measurements for operative and nonoperative limbs in skeletally immature patients.
Materials and methods
An institutional review board-approved study of all patients undergoing ACL reconstruction between 2007 and 2016 identified 90 patients with open distal femur and proximal tibia physes at the time of surgery. All patients underwent transphyseal ACL reconstruction in which soft-tissue grafts were passed across tunnels drilled through the distal femoral and proximal tibial physes. The postoperative radiographic records of 15 of these patients were randomly selected for inclusion in this study. One set of radiographs was selected from each patient. In all, 13 of the 15 sets included radiographs obtained while physes remained open about the knee; two sets included radiographs obtained within a year following physeal closure. Both operative and nonoperative limbs were assessed. The sample size of 15 was selected as described by Bujang and Baharum:15 with alpha and power fixed at 0.05 and 80%, respectively, a minimum sample size of 15 would be sufficient to detect a value of 0.3 for the ICC.
An identification number was assigned to each patient in the study. Radiographic images from each patient were de-identified and arranged in random order as a set of 15 patient studies for lower limb measurement and sent electronically to each reviewer: a third-year orthopaedic resident (AOO), a fifth-year orthopaedic resident (AFB) and a fellowship-trained attending paediatric orthopaedic surgeon (GAS) with more than 15 years’ experience. Images were analyzed three times by each reviewer, with randomly re-ordered images for repeat measurement delivered to reviewers with a minimum of three weeks between repetitions. Instructions with a description of each measurement were made available, including the mechanical lateral distal femoral angle (mLDFA) and mechanical medial proximal tibial angle (mMPTA),16 a modification of a measure for tibial slope as described by Paley et al16 and mechanical axis deviation (MAD) as described by Cho et al.17
The definitions of the angles measured are described below.
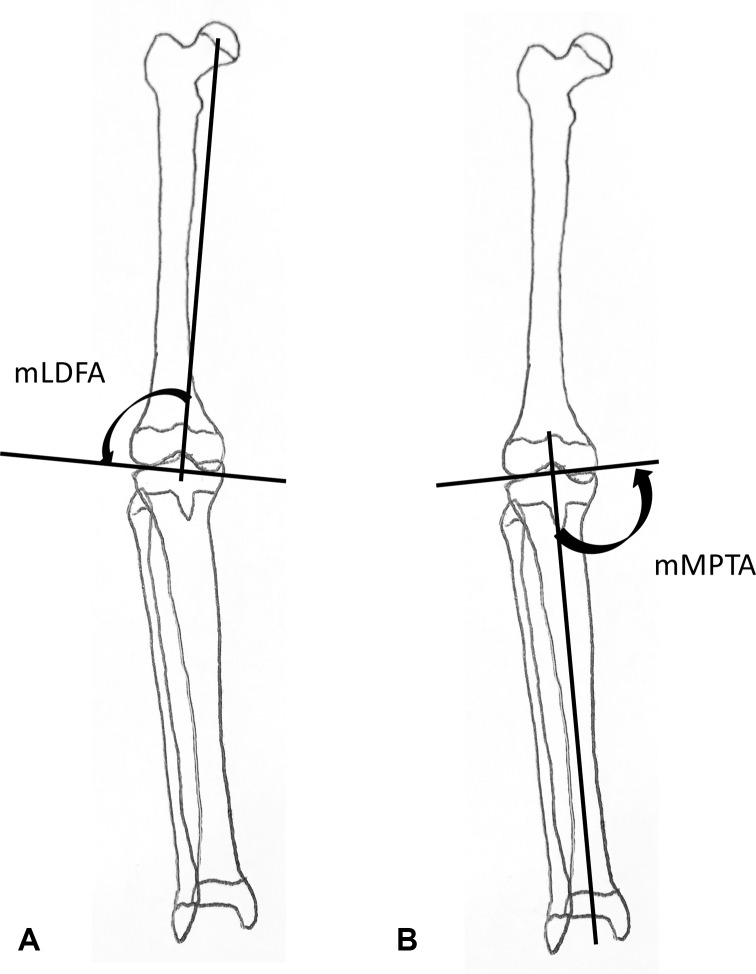
mLDFA: the lateral-based angle between the mechanical axis of the femur (femoral head to centre of trochlea) and a line tangent to the distal-most aspects of the distal femoral epiphysis (Fig. 1a).
Fig. 1.
(A) Coronal plane alignment of the distal femur (mechanical lateral distal femoral angle; mLDFA); (B) coronal plane alignment of the proximal tibia (mechanical proximal tibial angle; mMPTA).
mMPTA: the medial-based angle between the mechanical axis of the tibia (lateral tibial spine or the centre of the proximal tibia epiphysis to a point bisecting the plafond) and a line intersecting the medial- and lateral-most corners of the tibial epiphysis (Fig. 1b).
MAD: the ratio of D (the distance of the limb mechanical axis from the centre of the knee) to half the horizontal width of the tibial epiphysis (HW). By convention, the ratio is positive for valgus and negative for varus alignments (Fig. 2).
Fig. 2.
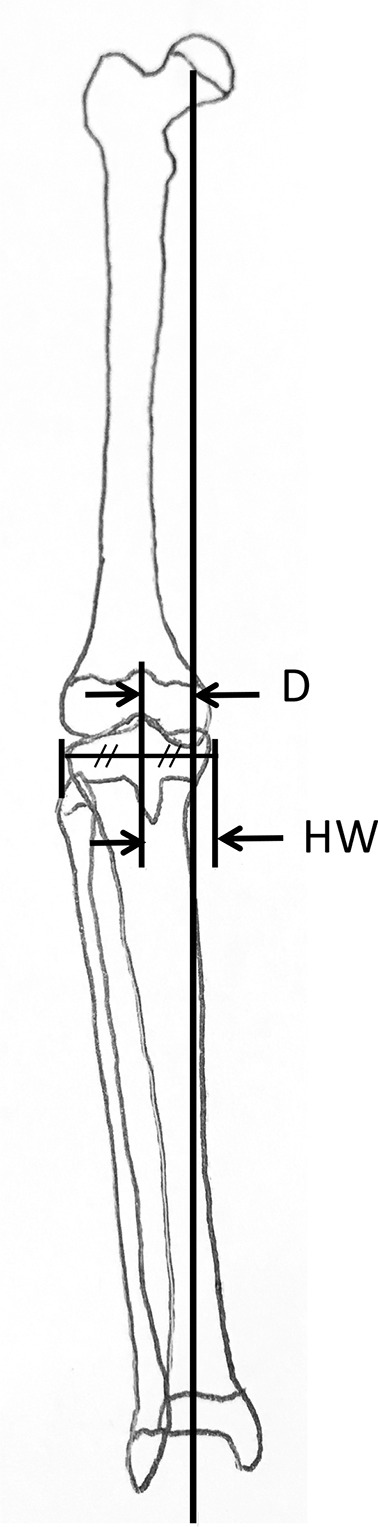
Mechanical axis deviation (MAD) of the lower limb defined as the distance between the mechanical axis and the midpoint of the tibial plateau (D) divided by one-half of the width of the plateau (HW). MAD = D/(HW), as described by Cho.17
Tibial slope: the posterior-based angle between the anterior tibial cortex (distal to the tubercle) and a line connecting the margins of the joint surface of the medial proximal tibial epiphysis (Fig. 3).
Fig. 3.
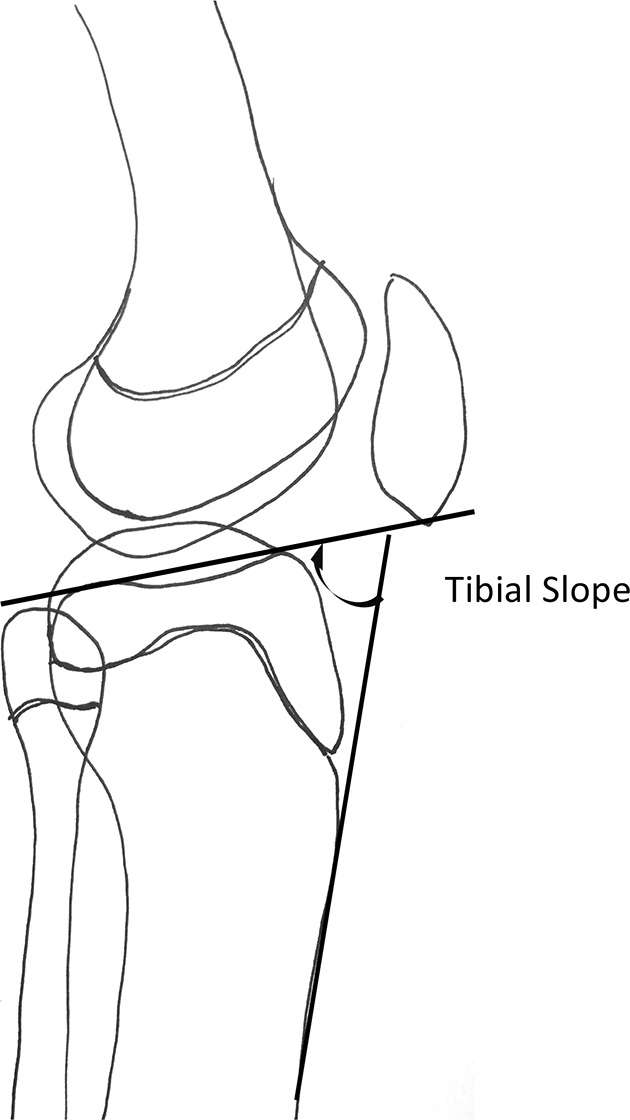
Tibial slope, measured as the angle between the medial epiphysis and the anterior cortex of the proximal tibia distal to the tubercle. Note the concavity of the medial epiphysis in contrast to the convexity of the lateral epiphysis, representing the morphology seen in an older child or adolescent.
All but tibial slope were coronal plane measurements of operative and nonoperative limbs on standing full-length digitally stitched hip-knee-ankle teleoroentgenograms; tibial slope was measured on lateral films of the operative knee. Given the absence of full-length lateral radiographs of the tibia for measurement of the tibial slope as described by Paley et al,16 the anterior cortex of the proximal tibia distal to the tubercle was used as a surrogate reference line. Measurements were made using the Centricity Enterprise Web PACS System (Version 3.0; GE Medical Systems, Barrington, Illinois). Angle measurement and window/level variation tools were available to use at the reviewers’ discretion. All measurements were recorded in Excel files (Microsoft Inc., Redmond, Washington) and returned to the statistician. Statistical calculations were performed using STATA software (Stata 14.2, College Station, Texas). The intra-class correlation coefficients (ICC) were calculated to assess reliability. Intraobserver ICCs were estimated for each rater using a one-way random effects model with absolute agreement with one model per investigator/radiographic combination. Interobserver coefficients were estimated using a two-way random effects model with absolute agreement with one model per set of measurements for each angle. Reliability was considered to be poor (< 0.40), fair (0.40 to 0.59), good (0.60 to 0.74) or excellent (0.75 to 1.00) as described by Cicchetti.18
Results
Intraobserver reliability for operative leg measurements was rated excellent across all measures except for tibial slope in one investigator’s measurements (good or ICC = 0.68) and mLDFA in another investigator’s measurements (fair or ICC = 0.49). For the nonoperative leg, reliability was excellent in all parameters except for one investigator’s measurements of mLDFA (poor or ICC = 0.29) (Table 1). Interobserver reliability in the operative leg was rated excellent across all investigators for measurements of mLDFA (ICC = 0.82), mMPTA (ICC = 0.88), MAD (ICC = 0.93) and tibial slope (ICC = 0.75). For the nonoperative leg, reliabilities were also excellent (Table 2).
Table 1.
Intraobserver reliability: intra-class correlation coefficients (ICC) for the operative and nonoperative limbs
| mLDFA ICC (CI) | mMPTA ICC (CI) | MAD ICC (CI) | Tibial slope ICC (CI) | |
|---|---|---|---|---|
| Operative limb | ||||
| Rater 1 | 0.93 (0.88 to 0.96) | 0.94 (0.90 to 0.97) | 0.95 (0.91 to 0.97) | 0.68 (0.25 to 0.88) |
| Rater 2 | 0.49 (0.07 to 0.74) | 0.85 (0.77 to 0.94) | 0.98 (0.97 to 0.99) | 0.95 (0.82 to 0.98) |
| Rater 3 | 0.90 (0.86 to 0.98) | 0.96 (0.93 to 0.98) | 0.99 (0.99 to 0.99) | 0.92 (0.82 to 0.97) |
| Nonoperative limb | ||||
| Rater 1 | 0.94 (0.85 to 0.97) | 0.94 (0.88 to 0.98) | 0.93 (0.84 to 0.97) | |
| Rater 2 | 0.27 (-0.16 to 0.47) | 0.88 (0.73 to 0.95) | 0.97 (0.91 to 0.98) | |
| Rater 3 | 0.87 (0.70 to 0.95) | 0.97 (0.84 to 0.99) | 0.99 (0.97 to 1.00) |
mLDFA, mechanical lateral distal femoral angle; CI, confidence interval; mMPTA, mechanical medial proximal tibial angle; MAD, mechanical axis deviation
Table 2.
Interobserver reliability: intra-class correlation coefficients (ICC) for the operative and nonoperative limbs
| ICC | CI | p-value | |
|---|---|---|---|
| Operative limb | |||
| Tibial slope | 0.75 | 0.41 to 0.91 | 0.001 |
| mLDFA | 0.82 | 0.67 to 0.90 | < 0.001 |
| mMPTA | 0.88 | 0.77 to 0.94 | < 0.001 |
| MAD | 0.93 | 0.86 to 0.98 | < 0.001 |
| Nonoperative limb | |||
| mLDFA | 0.86 | 0.68 to 0.95 | < 0.001 |
| mMPTA | 0.98 | 0.94 to 0.99 | < 0.001 |
| MAD | 0.92 | 0.81 to 0.97 | < 0.001 |
CI, confidence interval; mLDFA, mechanical lateral distal femoral angle; mMPTA, mechanical medial proximal tibial angle; MAD, mechanical axis deviation
Discussion
This series of a randomly selected set of patients who underwent transphyseal ACL reconstruction identified high interobserver and intraobserver reliability among orthopaedic providers at a variety of levels of experience given a standard set of instructions on measures of coronal and sagittal plane alignment obtained using commonly employed digital radiography software. Others have documented the reliability of making measurements on long lower-limb radiographic films19,20 and have found good to excellent reliability. Segev et al21 described the high reliability of a PACS system with integrated on-screen instructions for measurements of paediatric radiographs. Nowicki et al14 compared digital radiographic angle measures of lower limb alignment in children to measures made on paper copies of digital images and found both provided fair to good reliability using the same ICC criteria utilized in this study, though sagittal plane alignment was not examined.
As noted by Nowicki et al,14 measures requiring a positive or negative value for valgus or varus (in our study, the MAD) could easily be misreported, though we found excellent reliability in our measurement and reporting of MAD. Also, intended angles with measures near 90° (mLDFA and mMPTA) were perhaps at a higher risk of being incorrectly measured, with a chance of the supplement of the desired angle being unintentionally measured merely by reversing the end of one of the two lines of the Cobb angle tool. This may account for our lowest reliabilities in measurements of mLDFA. Though an angle-measuring tool was also available, it required placement of lines tangent to landmarks of interest as well as placement of the angle vertex, while the Cobb angle tool only required placement of the two lines tangent to landmarks of interest. The increased ease of use likely led to adoption of the Cobb angle tool for most angle measurements.
We found that measurements of tibial slope were also less reliable, likely due to the challenge in choosing the appropriate osseous reference on the lateral radiographic images. The lateral articular surface of the tibial plateau may have been more clearly defined as it lay adjacent to the radiographic plate with limb positioning. The medial articular surface of the tibial plateau, the reference we employed, was at times not as clearly defined due in part to the skeletal immaturity of some of the patients included in the study, whose less ossified epiphyses often lacked discrete landmarks.
In addition, choosing the appropriate anterior tibial cortical line was noted to be challenging in those patients with a prominent tibial apophysis. The intended reference line was that obtained by drawing a line parallel to the anterior metaphyseal-diaphyseal proximal tibia, distal to the tubercle. In some patients, this line intersected the tibial apophysis, potentially leading to reviewer error in positioning of the intended axis. We elected not to use the posterior proximal tibial angle measure as described by Paley et al,16 in part because that measurement requires an estimate of the location of the midline of the ankle joint on a lateral view.
Limitations
Our study did not include radiologist reviewers, yet others have shown fairly equivalent reliability between these groups and orthopaedic surgeons when instruction in measurement techniques was given.14 In place of full-length lateral radiographs of the tibia, a surrogate reference line for the sagittal plane axis on lateral knee radiographs was selected that was felt to be reliably identified for measurement of the posterior tibial slope. However, lower reliabilities for this measure suggest otherwise.
Our study only examined the reliability of coronal and sagittal plane measures of alignment by trained reviewers and not the accuracy of the images to depict patients’ true alignments. Mild flexion of the knee, suspected in many patients undergoing preoperative imaging who had recently been injured, in concert with a mild internal or external rotation of the hip could lead to exaggerated measures of valgus or varus of the extremity. Though this study examined only the reliability of measurements made post-transphyseal ACL reconstruction, these reliabilities should apply to preoperative measures of alignments in skeletally immature patients as well.
Conclusion
Though the importance of routine imaging of the lower extremities prior to and following ACL reconstruction in skeletally immature patients to monitor for the presence of growth abnormalities of the distal femur and proximal tibia may be debatable, lower limb coronal and sagittal plane alignments measured with a standard technique in growing children using PACS software are reliable and reproducible when performed by orthopaedic surgeons of varying levels of experience who follow a basic set of instructions. Using a high-quality radiographic imaging system that optimizes the visualization of important radiographic landmarks in carefully positioned patients will aid in producing studies of the greatest value.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
This study was supported in part by the L. T. Staheli Endowment.
Ethical statement
Ethical approval: This research was approved by our Institutional Review Board.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was not required for this study.
ICMJE Conflict of interest statement
Each author certifies and declares that they have no conflict of interest.
Author Contributions
GAS: participated in design, data acquisition, analysis and interpretation of data.
AFB: participated in design, data acquisition, and interpretation of data.
AOO: participated in data acquisition and interpretation of data.
VB: participated in design, data acquisition, analysis and interpretation of data.
All authors were actively involved in the drafting and critical reviews of the manuscript, and each reviewed the final version of the manuscript submitted.
References
- 1.Werner BC, Yang S, Looney AM, Gwathmey FW Jr. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop 2016;36:447-452. [DOI] [PubMed] [Google Scholar]
- 2.Comstock RD, Currie DW, Pierpoint LA Summary Report: National high school sports-related injury surveillance study, 2015-2016 school year, 2016. http://www.ucdenver.edu/academics/colleges/PublicHealth/research/ResearchProjects/piper/projects/RIO/Documents/Original%20Report_Final%202015%2016%2009%2003%2016.pdf (date last accessed 21 January 2019).
- 3.Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy 2002;18:955-959. [DOI] [PubMed] [Google Scholar]
- 4.Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med 2012;40:2128-2133. [DOI] [PubMed] [Google Scholar]
- 5.Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med 2014;42:2769-2776. [DOI] [PubMed] [Google Scholar]
- 6.Dodwell ER, Lamont LE, Green DW, et al. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med 2014;42:675-680. [DOI] [PubMed] [Google Scholar]
- 7.Kocher MS, Saxon HS, Hovis WD, Hawkins RJ. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and The ACL Study Group. J Pediatr Orthop 2002;22:452-457. [PubMed] [Google Scholar]
- 8.Collins MJ, Arns TA, Leroux T, et al. Growth abnormalities following anterior cruciate ligament reconstruction in the skeletally immature patient: a systematic review. Arthroscopy 2016;32:1714-1723. [DOI] [PubMed] [Google Scholar]
- 9.Faunø P, Rømer L, Nielsen T, Lind M. The risk of transphyseal drilling in skeletally immature patients with anterior cruciate ligament injury. Orthop J Sports Med 2016;4:2325967116664685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moksnes H, Engebretsen L, Seil R. The ESSKA paediatric anterior cruciate ligament monitoring initiative. Knee Surg Sports Traumatol Arthrosc 2016;24:680-687. [DOI] [PubMed] [Google Scholar]
- 11.Shifflett GD, Green DW, Widmann RF, Marx RG. Growth arrest following ACL reconstruction with hamstring autograft in skeletally immature patients: a review of 4 cases. J Pediatr Orthop 2016;36:355-361. [DOI] [PubMed] [Google Scholar]
- 12.Uffmann M, Schaefer-Prokop C. Digital radiography: the balance between image quality and required radiation dose. Eur J Radiol 2009;72:202-208. [DOI] [PubMed] [Google Scholar]
- 13.Balkman JD, Loehfelm TW. A cloud-based multimodality case file for mobile devices. Radiographics 2014;34:863-872. [DOI] [PubMed] [Google Scholar]
- 14.Nowicki PD, Vanderhave KL, Farley FA, et al. Reliability of digital radiographs for pediatric lower extremity alignment. J Pediatr Orthop 2012;32:631-635. [DOI] [PubMed] [Google Scholar]
- 15.Bujang M, Baharum N. A simplified guide to determination of sample size requirements for estimating the value of the intraclass correlation coefficient: a review. Arch Orofac Sci 2017;12:1-11. [Google Scholar]
- 16.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994;25:425-465. [PubMed] [Google Scholar]
- 17.Cho TJ, Choi IH, Chung CY, et al. Hemiepiphyseal stapling for angular deformity correction around the knee joint in children with multiple epiphyseal dysplasia. J Pediatr Orthop 2009;29:52-56. [DOI] [PubMed] [Google Scholar]
- 18.Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess 1994;6:284-290. [Google Scholar]
- 19.Feldman DS, Henderson ER, Levine HB, et al. Interobserver and intraobserver reliability in lower-limb deformity correction measurements. J Pediatr Orthop 2007;27:204-208. [DOI] [PubMed] [Google Scholar]
- 20.Gordon JE, Chen RC, Dobbs MB, et al. Interobserver and intraobserver reliability in the evaluation of mechanical axis deviation. J Pediatr Orthop 2009;29:281-284. [DOI] [PubMed] [Google Scholar]
- 21.Segev E, Hemo Y, Wientroub S, et al. Intra- and interobserver reliability analysis of digital radiographic measurements for pediatric orthopedic parameters using a novel PACS integrated computer software program. J Child Orthop 2010;4:331-341. [DOI] [PMC free article] [PubMed] [Google Scholar]