Abstract
The painful shoulder is the most common condition seen in specialist shoulder clinics. It is often associated with lack of range of motion and reduced shoulder function. Lack of sleep and difficulties in performing basic daily life activities are common findings. Subacromial Impingement Syndrome (SAIS) has been considered as the most common cause of shoulder pain since it was described in 1852. Charles Neer, in 1972, described the presence of a “proliferative spur and ridge” on the undersurface of the acromion, which needs to be removed to improve the symptoms (acromioplasty). Neer’s “impingement” hegemony was undisputed for at least 30 years. A more extensive knowledge of the pathogenesis of SAIS, however, has led authors to challenge the role of “impingement” in the shoulder pain and the role of surgical intervention. The aim of this review was to understand if there is still a role for surgical decompression in patients with SAIS. A literature review was performed in PubMed, PEDro, Embase, and the Cochrane Central Register of Controlled Trials using impingement, subacromial space, rotator cuff tears, tendinopathy, and tendinitis as key words. Randomized clinical trials (RCTs) with long-term follow-up comparing surgical intervention and conservative treatments in SAIS were preferred; however, prospective articles studying the outcome of surgical decompression and physiotherapy were also included. The majority of the studies showed no difference in the outcome between patients randomized to surgical decompression or conservative management. However, some studies reported better results after surgery, especially in the long term. Interpretation of the results is very difficult as most of the studies are of poor quality and have short follow-up. In our opinion, the type of subacromial lesion needs to be considered; this may offer an explanation to the difference in severity of symptoms and to the varying degrees of response to certain treatments, including surgery. Further studies are mandatory to better understand the role of surgery in SAIS.
Keywords: impingement, bursitis, supraspinatus tendon, rotator cuff, rotator cuff tears, tendinopathy, tendinitis
Introduction
Subacromial Impingement Syndrome (SAIS) is the commonest disorder of the shoulder, accounting for 44%–65% of all complaints of shoulder pain.1
In a Dutch study, the incidence of new cases of rotator cuff tendonitis in general practice was found to be around 3.2–4.2 per 1,000 person-years, and the corresponding incidence of shoulder pain (all causes) was 11.2 per 1,000 person-years.2 In the United Kingdom, the estimated percentage of people seeking treatment for shoulder pain in the general practice setting is between 20% and 50% in a life time.3 Among these patients, one in four sought medical care for SAIS.4 Its prevalence is especially high in repetitive overhead sports such as swimming, volleyball, handball, and manual jobs requiring prolonged overhead position of the arm (builders, electricians, hairdressers, etc).
Shoulder impingement results from an “inflammation and degeneration of the anatomical structures in the region of the subacromial space”.5 The subacromial space is defined by the humeral head inferiorly, the anterior edge and under surface of the anterior third of the acromion, coracoacromial ligament, and the acromioclavicular joint superiorly. The height of space between acromion and humeral head ranges from 1.0 to 1.5 cm as seen on radiographs (anteroposterior view).6 As the arm is abducted or rotated, the subacromial space width changes and the humerus gets closer to the anteroinferior edge of the acromion. This is true especially at 90° of abduction and 45° internal rotation of the shoulder.7
If the fine balance that regulates the shoulder kinematics is compromised, the humeral head migrates superiorly and the bursa protecting the rotator cuff, as well as the cuff itself becomes increasingly compressed.
Neer described the presence of a proliferative “spur” and ridge on the undersurface of the acromion (anterolaterally), which was recognized as the cause of the “impingement” as it reduced the subacromial space and therefore made it easier for the rotator cuff to get in contact with the acromion. He consequently described a technique to excise the “spur” in order to treat the symptoms coming from the contact between the acromion and the humeral head. This procedure was called “acromioplasty”.8 Neer was also one of the first to classify the impingement lesions and described three stages depending on the amount of damage in the subacromial space and the age of the patient (Table 1).
Table 1.
Neer’s classification: stages of subacromial impingement
| Stage 1: Edema and hemorrhage, age <25 years, reversible |
| Stage 2: Fibrosis and tendinitis, age 25–40 years, recurrent pain with activity |
| Stage 3: Bone spurs and tendon rupture, age >40 years, progressive disability |
Different hypotheses were considered to describe the pathogenesis of the SAIS; however, a clear explanation has not been found yet.
First of all, it is not clear yet if the damage to the rotator cuff tendons leads to the impingement (intrinsic mechanism) or if the impingement causes the damage to the tendons (extrinsic mechanism).9,10 The theories supporting the intrinsic mechanism are becoming more and more popular in the last few years.11,12 These theories argue that the poor vascularity of the supraspinatus tendon (SSP) insertion could be a significant factor in the pathogenesis of degenerative rotator cuff tears.10,12 The SSP mainly derives its blood supply from the anterior circumflex humeral and suprascapular arteries; near its insertion at the greater tuberosity, there is an avascular area, also called “critical” zone, which is usually where the tear originates.10 The insertional damage to the tendon fibers usually increases in size with the patient’s age, and it is more common in diabetic patients and patients with rheumatoid arthritis.13 Histological findings are more typical of a “failed healing response”, with a haphazard proliferation of tenocytes, intracellular abnormalities in tenocytes, disruption of collagen fibers, and subsequent increase in noncollagenous matrix.11,14
For 40 years, the supporters of the extrinsic theory tried to correlate shoulder pain to shoulder “impingement”. The shape of the acromion was examined and classified into flat (type I), curved (type II), or hooked (type III) and considered cause of “impingement” as result of the reduced distance in the subacromial space.15,16 The shape is age related or congenital is not clear.17 Also the anatomy of the thoracic spine was taken into consideration as it was seen to be linked to different possible orientations of the scapula. In patients with “impingement”, the scapula can be found to be more protracted and the thoracic spine18 more flexed. Today, extrinsic factors also include those which have a biological implication on the subacromial space such as heavy physical loading, injury, vibration, infection, smoking, genetic factors, and fluoroquinolone antibiotics19 which ultimately lead to rotator cuff diseases and shoulder pain. Dynamic, muscle-related theories were also described: weakness in the rotator cuff alters the glenohumeral and scapulothoracic kinematics with consequent superior migration of the humeral head and loss of the compression forces that regulate the glenohumeral movements. Similarly, periscapular muscle weakness lead to a late activation of the lower trapezius and the serratus anterior and an early recruitment of the upper trapezius fibers20 reducing the ability to externally rotate, tilt posteriorly, and rotate the scapula upward, so that it is more difficult to clear the humeral head during the movements of abduction and external rotation.21
Today, the uncertainty regarding the pathogenesis of SAIS is reflected by the confusion regarding its treatment. Since Neer’s “impingement” description in 1972,8 acromioplasty with bursectomy has been the gold standard for patients unresponsive to conservative treatments. In the last years, authors challenged the need for surgery in SAIS. A more comprehensive understanding of the pathogenesis lead to the publication of several papers which questioned the benefit of decompression surgery and the rationale of the “impingement” mechanism stating that placebo effect, prolonged rest, and intense physiotherapy after surgery have to be considered the true treatments.22–27
Conservative treatment yields satisfactory results within 2 years in 60% of cases. Studies showed that conservative management of shoulder impingement syndrome resolves the problem in 70%–90% of patients.28 In the absence of major structural damage, conservative multimodal treatment for 3–6 months is the initial therapy of choice. Conservative management includes exercise therapy, ultrasound treatment, and subacromial injections (Table 2).
Table 2.
Conservative treatment options
| Immobilization |
| Nonsteroidal antiinflammatory drugs |
| Cortisone injections |
| Physical therapy |
| Ultrasound |
| Application of heat and electricity |
| Manual therapy |
| Elastic therapeutic tape |
| Acupuncture |
Today, acromioplasty has left space to arthroscopic subacromial decompression (ASD) procedure, which is the gold standard to surgically treat SAIS. The procedure includes debridement of the subacromial bursa, resection of the coracoacromial ligament, and the anterolateral edge of the acromion, as well as any underhanging osteophytes from the acromioclavicular joint.29 In the last 25 years, ASD was often adopted because of lower morbidity: including risks of infection and neurovascular damage.
This review of the literature describes the historically accepted methods of treatment of SAIS and wants to discuss if acromioplasty (open or arthroscopic) is to be considered as an out-of-date procedure today and hence is not necessary in patients who have failed to improve with conservative management. The aim of the study was to analyze and describe the current concepts linked to SAIS and shoulder pain and clarify the role of subacromial decompression in the treatment of SAIS.
Literature search and study selection
A search of the literature in PubMed, PEDro, Embase, and the Cochrane Central Register of Controlled Trials was conducted to identify relevant publications from Neer’s paper in 1972 until 2018. Key words such as shoulder impingement syndrome, subacromial space, subacromial decompression, rotator cuff impingement, rotator cuff tears, tendinopathy, and tendinitis were used for the literature search.
All the articles were in English, except one published in German. Reference lists of retrieved articles and articles on surgical interventions for SAIS were screened for additional publications. Names of first authors of selected articles were used for citation tracking.
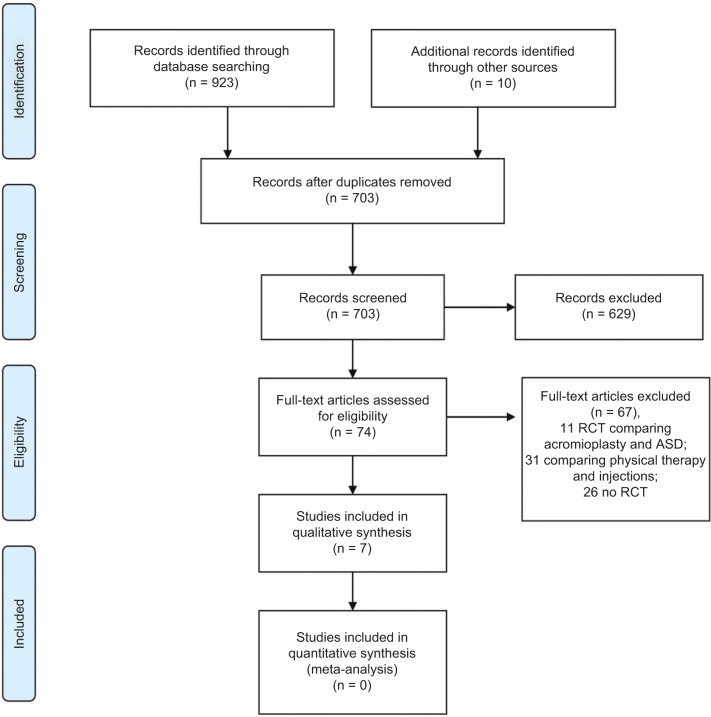
The articles were independently reviewed by two authors (PC and GS) and the inclusion criteria analyzed from the titles and abstracts of the references retrieved by the literature search. A third reviewer (OH) was consulted if disagreement regarding the inclusion criteria was met. RCTs comparing surgical treatment and conservative treatment for the management of SAIS were included. Prospective articles studying outcome of surgical decompression and physical therapy were also included. Studies focusing on surgical repair of rotator cuff tears, adhesive capsulitis, and shoulder instability were excluded. All the studies included reported outcomes in adult patients (>18 years) only. In all the studies, patients underwent surgery only if failed to improve with conservative treatments for 3–6 months. Mixtures of outcome measures were used in the studies selected. However, the Constant Score appeared to be the most frequently used even if not always as primary outcome measurement. A quantitative analysis (meta-analysis) was not possible because of the diversity in outcome measures used in the various studies (Figure 1). A qualitative analysis was hence performed. The minimum follow-up was 6 months27 and the longest was 13 years.22 Studies with large group of patients enrolled and long-term follow-up were preferred. Inclusion and exclusion criteria are reported in Table 3. Each article was graded (unclear, low, or high risk of bias) based on sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, other possible bias, intention-to-treat analysis, selective reporting, and baseline characteristics. The risk of bias assessment was completed by one author (PC) and checked by a second author (GS). Disagreements were resolved by discussion, and a third author (OH) was consulted if consensus could not be reached. A Physiotherapy Evidence Database (PEDro) scale was used for rating the seven selected RCT papers.
Figure 1.
Flowchart of search strategy.
Source: From Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 2009;6(7):e1000097; doi:10.1371/journal.pmed1000097. For more information, visit www.prisma-statement.org.45
Abbreviations: ASD, arthroscopic subacromial decompression; RCT, randomized clinical trial.
Table 3.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Randomized control trials comparing surgical treatment (either open or arthroscopic) and conservative treatment or no treatment for SAIS | Randomized control trials comparing open and arthroscopic acromioplasty |
| Prospective studies analyzing outcome of ASD for the treatment of SAIS | Studies including patients with rotator cuff tears who underwent ASD only |
| Prospective studies analyzing outcome of conservative treatment (physical therapy) for the treatment of SAIS | Studies including patients with rotator cuff tears who underwent rotator cuff repair only |
| Adult patients (>18 years of age) | Studies including patients with rotator cuff tears who underwent rotator cuff repair and ASD |
| Conservative treatment for a minimum of 3–6 months before surgical intervention was considered | Studies including patients with adhesive capsulitis |
| Minimum follow-up of 6 months | Studies including patients with instability |
| Studies comparing ASD and bursectomy alone | Studies including children (<18 years of age) |
| Studies with minimum follow-up less than 6 months | |
| Young patients (<18 years of age) |
Abbreviations: SAIS, Subacromial Impingement Syndrome; ASD, arthroscopic subacromial decompression.
Results
The results from seven RCTs, mainly comparing conservative treatment and surgical treatment, were collected and analyzed. Discrepancy in the results was observed (Table 4). The results of an RCT comparing ASD and bursectomy alone were analyzed as it was considered to add value to high quality, two fair, and two poor using the PEDro scale.
Table 4.
Randomized control trials included in the literature review
| Authors | Study type | Year | Patients | Mean age | Follow-up (months) | Group 1 | Group 2 | Group 3 | Results |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Haahr et al33 | RCT | 2005 | 90 | 44 | 6–12 | ASD + physiotherapy | Physiotherapy – strengthening the stabilizers and decompressors of the shoulder | n/a | No statistically significant difference in CS No difference in mean pain and dysfunction score |
| Brox et al46 | RCT | 1993 | 125 | 48 | 6 | ASD + physiotherapy | Physiotherapy – supervised | Placebo – laser therapy | No difference in Neer score, VAS |
| Rahme et al32 | RCT | 1998 | 42 | 42 | 6 | Open acromioplasty+physiotherapy | Physiotherapy – strengthening and endurance training | n/a | VAS better in the surgical group |
| Peters andKohn31 | RCT | 1997 | 72 | 56 | 48 | Open acromioplasty+ASD + physiotherapy | Two week hospital stay: physiotherapy supported with NSAIDs and corticosteroid injections | n/a | No difference between the groups |
| Beard et al27 | RCT | 2017 | 313 | 53 | 6–12 | ASD + physiotherapy | Placebo – arthroscopy only + physiotherapy | No treatment | The OX and the CS showed no difference between decompression and arthroscopy only at 6 months and 1 year, but both surgical groups were better than no treatment at both timepoints. Similar findings observed for the other outcome measurements: PainDETECT, EQ-5D-3L Index, EQ VAS, HADS |
| Ketola et al22 | RCT | 2017 | 140 | 47.1 | 156 | ASD + physiotherapy | Physiotherapy – supervised | n/a | Self-reported pain and VAS; disability, working ability and pain at night (VAS), SDQ improved in both groups compared with preoperative findings, but no difference was found between the two groups. |
| Farfaras et al34 | RCT | 2018 | 95 | 45 | 30 | Open acromioplasty+ physiotherapy | ASD + physiotherapy | Physiotherapy – supervised | The strength improves in both surgical groups (statistically significant improvement only in the open acromioplasty group (P=0.003), but did not in the conservative group). CS improved (P<0.005) in the surgical groups only. The Watson and Sonnabend score did not show difference between groups (P=0.14) |
Abbreviations: ASD, arthroscopic subacromial decompression; CS, constant score; EQ-5D-3L, Index EuroQol 5 dimensions 3 levels; EQ VAS, EuroQol visual analog scale; HADS, Hospital Anxiety and Depression Scale; OS, Oxford score; RCT, randomized clinical trial; SDQ, Shoulder Disability Questionnaire score.
Brox et al30 randomized 125 patients to ASD, physiotherapy, and laser therapy (placebo group). No differences were found between the three groups in duration of sick leave to 6 months (median 3 months) and daily intake of analgesics. Participants in both groups that received active treatment improved significantly more than those in the placebo group at 6 months: median differences between exercises (13.0 [95% CI 7 to 20]) and surgery (19.5 [95% CI 12 to 27]) compared with placebo (mean change in Neer score –0.3 with placebo compared with 10.8 in the exercise group and 20.2 in the surgery group). Treatment costs were higher for those given surgery (720 pounds) vs those given supervised exercises (390 pounds). This was predominantly due to hospitalization in the surgical group.
Peters and Kohn31 compared either arthroscopic or open acromioplasty to physiotherapy in 72 patients. Surgical patients improved from 54 at baseline to 84 on the Subjective Shoulder Rating Scale; similarly, with no significant difference, patients treated conservatively improved from 59 to 74.
Rahme et al32 presented the results of 42 patients. At 6 months, treatment in the surgical group had been successful in 12/21 (57%) patients vs 6/18 (33%) in the physiotherapy group. Before the 12 months follow–up, 13 patients decided to have surgery, therefore, a direct comparison of the two groups at 12 months was not possible.
In 2004, Haahr et al33 randomized 90 patients either to ASD or to physiotherapy with exercises aiming at strengthening the stabilizers and decompressors of the shoulder. Of the 90 patients enrolled, 84 completed follow-up (41 in the surgery group, 43 in the training group). The mean CS at baseline was 34.8 in the training group and 33.7 in the surgery group. After 12 months, the mean scores improved to 57.0 and 52.7, respectively, the difference being nonsignificant. No difference in mean pain and dysfunction score improvement was found.
In 2017, a group of researchers from Oxford published a multicenter, randomized, pragmatic, parallel-group trial with 313 patients treated by 51 surgeons in 32 hospitals in the United Kingdom between 2012 and 2015.27 They randomized the participants to ASD, arthroscopy only (with no soft tissue or bone removal), and no treatment. Mean Oxford Shoulder Score did not differ between the two surgical groups at 6 months (decompression 32.7 points [SD 11.6] vs arthroscopy 34.2 points [9.2]; mean difference –1.3 points (95% CI –3.9 to 1.3, P=0.3141). Both surgical groups showed a small benefit over no treatment (mean 29.4 points [SD 11.9], decompression was higher by 2.8 points [95% CI 0.5 to 5.2], P=0.0186; mean difference vs arthroscopy by 4.2 points [1.8 to 6.6], P=0.0014), but these differences were not clinically important. Another study by Ketola et al22 reported the long-term results (11–13 years) of arthroscopic acromioplasty in the treatment of rotator cuff tendinopathy observed in 140 patients. The participants were randomized to ASD and supervised exercises and supervised exercises only. At 2 years, 5 years (results previously published23,24), and over 10 years22 follow-up, self-reported pain and visual analog scale (VAS), disability, working ability, pain at night (VAS), and Shoulder Disability Questionnaire score improved in both groups compared with the baseline but no difference was found between the two groups.
Farfaras et al34 published the results of an RCT comparing open acromioplasty, ASD, and physical therapy in SAIS at 10 years follow-up. The strength in both surgical treatment groups improved over time, but the improvement was statistically significant only in the open acromioplasty group (P=0.003). No statistically significant difference over time was seen in the conservative group. CS improved significantly in both surgical groups (open acromioplasty, P=0.003; ASD, P=0.011) while, instead, it did not in the group that was treated with physiotherapy only. The Watson and Sonnabend score did not show significant difference among the groups (P=0.14). Ultrasound and XRs were used at the follow-up to detect possible rotator cuff tears, superior migration of the humeral head, bursitis, and gleno humeral osteoarthritis; no differences were found in the three groups.
Discussion
For the past 50 years, since Charles Neer introduced the acromioplasty technique, surgical intervention has been often considered in those patients who failed with conservative treatment.
In the last years, concerns raised regarding the benefit of performing surgery in SAIS. New considerations regarding the pathogenesis11 of the disease have challenged the technique proposed by Neer in 1972.8 Authors have proposed that postoperative rest and physiotherapy might be the real cures for SAIS; different studies have concluded that surgery could only have a placebo effect and might be not necessary.
The results of RCT studies published in the last 15–20 years reflect the progress made in understanding the pathogenesis of shoulder pain; the “impingement” concept, as Neer described it, looks antiquate today.11 Better understanding of the intrinsic mechanisms as causes of the pain and disability experienced by the patients have emphasized the importance of rotator cuff tendons state in the natural history of the sub-acromial pain. For this reason, it has been proposed to change the name to “anterolateral” shoulder pain syndrome instead of “impingement” syndrome, which emphasized more on the mechanical aspect of the problem.11 Hence, shoulder pain is not necessarily caused by the contact between the acromion and the cuff, but originates from the rotator cuff tendons12 and is mediated by the free nerve endings in the bursa.35
This new concept is supported by a number of RCTs (Peters and Kohn,31 Haahr et al,33 Ketola et al22–24) that haven’t observed the supremacy of surgery on conservative treatment. Physiotherapy was seen to provide good outcome, comparable to those achieved with surgery but without the costs and the complications that are intrinsically connected to surgery. More recently, in 2017, Beard et al27 showed that the outcome achieved by the surgical groups are statistically significantly better than those reached by the no treatment group, however, the differences have uncertain clinical mean.27 The difference was more significant at 6 months compared with 12 months follow-up as most of the patients in the no treatment group felt much improved and satisfied with the results after 1 year. Interestingly, one of the two surgical groups had only a diagnostic arthroscopy and no removal of soft tissue or bone from the subacromial space was undertaken (placebo group). Following these findings, they suggested that the results of the ASD group could be related to the prolonged rest and postoperative physiotherapy and not to the procedure itself. Despite the study having some limitations, such as the level of noncompliance to treatment allocation and the short follow-up, it strongly disputes the need for surgery for SAIS. To reinforce these findings, Henkus et al26 reported the results of an RCT with 57 patients and 2.5 years mean follow-up where the results of arthroscopic bursectomy only and ASD were compared. No differences were found in the two groups. This study stressed the strength of placebo effect related to surgery and challenged the need for removal of bone from the acromion as might not be necessary. As the RCT published by Beard et al27 has got very limited follow-up and therefore the results need to be analyzed very carefully, Ketola et al22 described long-term results (11–13 years) of an RCT assessing the benefit of arthroscopic acromioplasty and supervised exercises compared to supervised exercises only, in the treatment of rotator cuff tendinopathy. At 10 years22 follow–up, no differences were seen in the outcome of the two groups despite a significant improvement was seen in the outcome compared with the baseline.
However, despite the number of RCTs challenging the need for surgery in SAIS, it is necessary to critically analyze the data and avoid confusion. The surgical findings observed in the subacromial space36 during shoulder arthroscopy are hard to be explained if not for a contact between the rotator cuff and the acromion. The classification described by Atoun et al36 (Copeland–Levy classification) applies to different degrees of damage observed on the undersurface of the acromion and the bursal side of the rotator cuff. These findings are secondary to an “impingement”, considered as a mechanical contact between the humeral head and acromion,37 but can be primarily related to an intrinsic impairment of the rotator cuff (mainly the SSP tendon insertion) with loss of shoulder depression function.38
None of the reviewed studies consider the degree of subacromial damage occurred to the rotator cuff and the acromion and coracoacromial ligament. Intrinsic tendon damage and consequent rotator cuff failure were already described by Neer et al as “fibrillation”. Arthroscopy helped to classify the different lesions and their severity36 and confirmed that, despite the pathogenesis, a contact between the cuff and the acromion occurs in certain patients with SAIS. Under this circumstance, we believe that surgical decompression can still be considered the appropriate treatment.29,34,39–41
An RCT published by Farfaras et al34 reported the good results of ASD at 10-year follow-up. They found that the groups randomized to surgery (open or arthroscopic decompression) maintained better long-term results (CS) compared with the patients randomized to physical therapy. These outcomes are in line with other study results which, however, are not coming from randomized trial and have shorter follow-up.40,42 Considering the long-term effect of surgical decompression, also for patients >60 years of age,34 authors considered the possibility of long-term protective effect of subacromial decompression in SAIS patients.40,43 Even if there were no statistically significant differences, Farfaras et al34 reported a higher incidence of rotator cuff tears at the follow-up (ultrasound) in the group treated with physical therapy compared with the surgical groups (open acromioplasty: 1; ASD: 1; physiotherapy: 4).
Further studies are necessary to separately analyze in different groups, patients with signs of intrinsic failure of the rotator cuff and involvement of the acromial arch, considered as structural changes in the subacromial space, from patients with no abnormality. Patients with a more advanced stage of the disease might benefit from surgical decompression more than those in whom marked changes in the subacromial space have not occurred yet.
This might explain well why some patients often struggle to regain good shoulder function with conservative treatment only and hence they are often referred to secondary care centers to consider surgical intervention.
Conclusion
SAIS is considered to be one of the most common forms of shoulder pathology in the general population3 disabling numerous patients. The pathogenesis is not fully understood, but recent studies moved the attention from the extrinsic mechanism of “impingement”8 to intrinsic causes related to poor microvascularity of the insertion of the SSP tendon.11,13,14 The source of pain is mediated by the free nerve endings which are in the bursa and is thought to be related to the degree of damage to the SSP tendon.35
Hence, as the “spur” described by Neer8 is not considered the source of the pain anymore, acromioplasty was challenged.22,27 Several RCTs22,25,27,33,44 reported that acromioplasty does not add any benefit to conservative treatments. Placebo effect of surgery and the effectiveness of prolonged rest and physiotherapy were considered as the real cures for the symptoms.
However, the conclusion is not that simple as other studies reported good outcome after ASD and better long-term results when compared with patients treated with conservative treatments only.29,34,39–41 Many RCTs which encourage the use of exercises and physiotherapy, as these seem to give similar results to surgery, do not offer solution to those patients who fail in conservative management. Classification of the subacromial lesions needs to be considered to fully understand the response of SAIS patients to different treatments. Surgical decompression still needs to be considered when conservative treatment fails. In this specific group of patients, we believe the outcome of surgery can be compared with the intraoperative classification of the impingement lesion. Further RCTs with stricter clinical and imaging criteria must be developed to further understand the response of patients with SAIS to conservative treatment and surgery. A better understanding of the anatomopathology is mandatory to improve our indications to treatment.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Bhattacharyya R, Edwards K, Wallace AW. Does arthroscopic sub-acromial decompression really work for sub-acromial impingement syndrome: a cohort study. BMC Musculoskelet Disord. 2014;15:324. doi: 10.1186/1471-2474-15-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54(12):959–964. doi: 10.1136/ard.54.12.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Linsell L, Dawson J, Zondervan K, et al. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology (Oxford) 2006;45(2):215–221. doi: 10.1093/rheumatology/kei139. [DOI] [PubMed] [Google Scholar]
- 4.Bodin J, Ha C, Petit Le Manac’h A, et al. Risk factors for incidence of rotator cuff syndrome in a large working population. Scand J Work Environ Health. 2012;38(5):436–446. doi: 10.5271/sjweh.3285. [DOI] [PubMed] [Google Scholar]
- 5.Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009;90(11):1898–1903. doi: 10.1016/j.apmr.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 6.Pesquer L, Borghol S, Meyer P, Ropars M, Dallaudière B, Abadie P. Multimodality imaging of subacromial impingement syndrome. Skeletal Radiol. 2018;47(7):923–937. doi: 10.1007/s00256-018-2875-y. [DOI] [PubMed] [Google Scholar]
- 7.Graichen H, Bonel H, Stammberger T, Englmeier KH, Reiser M, Eckstein F. Subacromial space width changes during abduction and rotation--a 3-D MR imaging study. Surg Radiol Anat. 1999;21(1):59–64. doi: 10.1007/BF01635055. [DOI] [PubMed] [Google Scholar]
- 8.Neer CS., 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54(1):41–50. [PubMed] [Google Scholar]
- 9.Uhthoff HK, Sarkar K. Classification and definition of tendinopathies. Clin Sports Med. 1991;10(4):707–720. [PubMed] [Google Scholar]
- 10.Lohr JF, Uhthoff HK. The microvascular pattern of the supraspinatus tendon. Clin Orthop Relat Res. 1990;254:35–38. [PubMed] [Google Scholar]
- 11.McFarland EG, Maffulli N, Del Buono A, Murrell GA, Garzon-Muvdi J, Petersen SA. Impingement is not impingement: the case for calling it “Rotator Cuff Disease”. Muscles Ligaments Tendons J. 2013;3(3):196–200. [PMC free article] [PubMed] [Google Scholar]
- 12.Ozaki J, Fujimoto S, Nakagawa Y, Masuhara K, Tamai S. Tears of the rotator cuff of the shoulder associated with pathological changes in the acromion. A study in cadavera. J Bone Joint Surg Am. 1988;70(8):1224–1230. [PubMed] [Google Scholar]
- 13.Ling SC, Chen CF, Wan RX. A study on the vascular supply of the supraspinatus tendon. Surg Radiol Anat. 1990;12(3):161–165. doi: 10.1007/BF01624517. [DOI] [PubMed] [Google Scholar]
- 14.Del Buono A, Battery L, Denaro V, Maccauro G, Maffulli N. Tendinopathy and inflammation: some truths. Int J Immunopathol Pharmacol. 2011;24(1 Suppl 2):45–50. doi: 10.1177/03946320110241S209. [DOI] [PubMed] [Google Scholar]
- 15.Bigliani LU, Levine WN. Subacromial impingement syndrome. J Bone Joint Surg Am. 1997;79(12):1854–1868. [PubMed] [Google Scholar]
- 16.Weiner DS, Macnab I. Superior migration of the humeral head. A radiological aid in the diagnosis of tears of the rotator cuff. J Bone Joint Surg Br. 1970;52(3):524–527. [PubMed] [Google Scholar]
- 17.Seitz AL, McClure PW, Finucane S, Boardman ND, 3rd, Michener LA. Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both? Clin Biomech (Bristol, Avon) 2011;26(1):1–12. doi: 10.1016/j.clinbiomech.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 18.Lewis JS, Wright C, Green A. Subacromial impingement syndrome: the effect of changing posture on shoulder range of movement. J Orthop Sports Phys Ther. 2005;35(2):72–87. doi: 10.2519/jospt.2005.35.2.72. [DOI] [PubMed] [Google Scholar]
- 19.Danielson P, Andersson G, Alfredson H, Forsgren S. Marked sympathetic component in the perivascular innervation of the dorsal paratendinous tissue of the patellar tendon in arthroscopically treated tendinosis patients. Knee Surg Sports Traumatol Arthrosc. 2008;16(6):621–626. doi: 10.1007/s00167-008-0530-1. [DOI] [PubMed] [Google Scholar]
- 20.Ludewig PM, Braman JP. Shoulder impingement: biomechanical considerations in rehabilitation. Man Ther. 2011;16(1):33–39. doi: 10.1016/j.math.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diederichsen LP, Nørregaard J, Dyhre-Poulsen P, et al. The activity pattern of shoulder muscles in subjects with and without subacromial impingement. J Electromyogr Kinesiol. 2009;19(5):789–799. doi: 10.1016/j.jelekin.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 22.Ketola S, Lehtinen JT, Arnala I. Arthroscopic decompression not recommended in the treatment of rotator cuff tendinopathy a final review of a randomised controlled trial at a minimum follow-up of ten years. Bone Joint J. 2017;99-B(6):799–805. doi: 10.1302/0301-620X.99B6.BJJ-2016-0569.R1. [DOI] [PubMed] [Google Scholar]
- 23.Ketola S, Lehtinen J, Arnala I, et al. Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome?: a two- year randomised controlled trial. J Bone Joint Surg Br. 2009;91(10):1326–1334. doi: 10.1302/0301-620X.91B10.22094. [DOI] [PubMed] [Google Scholar]
- 24.Ketola S, Lehtinen J, Rousi T, et al. No evidence of long-term benefits of arthroscopic acromioplasty in the treatment of shoulder impingement syndrome: five-year results of a randomised controlled trial. Bone Joint Res. 2013;2(7):132–139. doi: 10.1302/2046-3758.27.2000163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dorrestijn O, Stevens M, Winters JC, van der Meer K, Diercks RL. Conservative or surgical treatment for subacromial impingement syndrome? A systematic review. J Shoulder Elbow Surg. 2009;18(4):652–660. doi: 10.1016/j.jse.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 26.Henkus HE, de Witte PB, Nelissen RG, Brand R, van Arkel ER. Bursectomy compared with acromioplasty in the management of subacromial impingement syndrome: a prospective randomised study. J Bone Joint Surg Br. 2009;91(4):504–510. doi: 10.1302/0301-620X.91B4.21442. [DOI] [PubMed] [Google Scholar]
- 27.Beard DJ, Rees JL, Cook JA, et al. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): a multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. Lancet. 2018;391(10118):329–338. doi: 10.1016/S0140-6736(17)32457-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garofalo R, Conti M, Massazza G, Cesari E, Vinci E, Castagna A. Sub-coracoid impingement syndrome: a painful shoulder condition related to different pathologic factors. Musculoskelet Surg. 2011;95(Suppl 1):S25–S29. doi: 10.1007/s12306-011-0142-7. [DOI] [PubMed] [Google Scholar]
- 29.Ellman H. Arthroscopic subacromial decompression: analysis of one- to three-year results. Arthroscopy. 1987;3(3):173–181. doi: 10.1016/s0749-8063(87)80061-0. [DOI] [PubMed] [Google Scholar]
- 30.Brox JI, Gjengedal E, Uppheim G, et al. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prospective, randomized, controlled study in 125 patients with a 2 1/2-year follow-up. J Shoulder Elbow Surg. 1999;8(2):102–111. doi: 10.1016/s1058-2746(99)90001-0. [DOI] [PubMed] [Google Scholar]
- 31.Peters G, Kohn D. Mid-term clinical results after surgical versus conservative treatment of subacromial impingement syndrome. Unfallchi rurg. 1997;100(8):623–629. doi: 10.1007/s001130050167. German. [DOI] [PubMed] [Google Scholar]
- 32.Rahme H, Solem-Bertoft E, Westerberg CE, Lundberg E, Sörensen S, Hilding S. The subacromial impingement syndrome. A study of results of treatment with special emphasis on predictive factors and pain-generating mechanisms. Scand J Rehabil Med. 1998;30(4):253–262. doi: 10.1080/003655098444002. [DOI] [PubMed] [Google Scholar]
- 33.Haahr JP, Østergaard S, Dalsgaard J, et al. Exercises versus arthroscopic decompression in patients with subacromial impingement: a randomised, controlled study in 90 cases with a one year follow up. Ann Rheum Dis. 2005;64(5):760–764. doi: 10.1136/ard.2004.021188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Farfaras S, Sernert N, Rostgard Christensen L, Hallström EK, Kartus JT. Subacromial decompression yields a better clinical outcome than therapy alone: a prospective randomized study of patients with a minimum 10-year follow-up. Am J Sports Med. 2018;46(6):1397–1407. doi: 10.1177/0363546518755759. [DOI] [PubMed] [Google Scholar]
- 35.Vangsness CT, Ennis M, Taylor JG, Atkinson R. Neural anatomy of the glenohumeral ligaments, labrum, and subacromial bursa. Arthroscopy. 1995;11(2):180–184. doi: 10.1016/0749-8063(95)90064-0. [DOI] [PubMed] [Google Scholar]
- 36.Atoun E, Gilat R, van Tongel A, et al. Intraobserver and interob-server reliability of the Copeland-Levy classification for arthroscopic evaluation of subacromial impingement. J Shoulder Elbow Surg. 2017;26(12):2167–2172. doi: 10.1016/j.jse.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 37.Flatow EL, Soslowsky LJ, Ticker JB, et al. Excursion of the rotator cuff under the acromion. Patterns of subacromial contact. Am J Sports Med. 1994;22(6):779–788. doi: 10.1177/036354659402200609. [DOI] [PubMed] [Google Scholar]
- 38.Neviaser A, Andarawis-Puri N, Flatow E. Basic mechanisms of tendon fatigue damage. J Shoulder Elbow Surg. 2012;21(2):158–163. doi: 10.1016/j.jse.2011.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klintberg IH, Svantesson U, Karlsson J. Long-term patient satisfaction and functional outcome 8-11 years after subacromial decompression. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):394–403. doi: 10.1007/s00167-009-0963-1. [DOI] [PubMed] [Google Scholar]
- 40.Lunsjö K, Bengtsson M, Nordqvist A, Abu-Zidan FM. Patients with shoulder impingement remain satisfied 6 years after arthroscopic subacromial decompression: a prospective study of 46 patients. Acta Orthop. 2011;82(6):711–713. doi: 10.3109/17453674.2011.623571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Björnsson H, Norlin R, Knutsson A, Adolfsson L. Fewer rotator cuff tears fifteen years after arthroscopic subacromial decompression. J Shoulder Elbow Surg. 2010;19(1):111–115. doi: 10.1016/j.jse.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 42.Roddy E, Zwierska I, Hay EM, et al. Subacromial impingement syndrome and pain: protocol for a randomised controlled trial of exercise and corticosteroid injection (the SUPPORT trial) BMC Musculoskelet Disord. 2014;15:81. doi: 10.1186/1471-2474-15-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Biberthaler P, Beirer M, Kirchhoff S, Braunstein V, Wiedemann E, Kirchhoff C. Significant benefit for older patients after arthroscopic subacromial decompression: a long-term follow-up study. Int Orthop. 2013;37(3):457–462. doi: 10.1007/s00264-012-1760-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ng C, Bialocerkowski A, Hinman R. Effectiveness of arthroscopic versus open surgical stabilisation for the management of traumatic anterior glenohumeral instability. Int J Evid Based Healthc. 2007;5(2):182–207. doi: 10.1111/j.1479-6988.2007.00064.x. [DOI] [PubMed] [Google Scholar]
- 45.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brox JI, Staff PH, Ljunggren AE, Brevik JI. Arthroscopic surgery compared with supervised exercises in patients with rotator cuff disease (stage II impingement syndrome) BMJ. 1993;307(6909):899–903. doi: 10.1136/bmj.307.6909.899. [DOI] [PMC free article] [PubMed] [Google Scholar]