1. Introduction
Recent research highlights the need for ongoing recovery support of adolescents following treatment for substance use disorders. While treatment often results in reduced alcohol and other drug (AOD) use or abstinence, these effects are tempered by high rates of premature dropout from services, relapse within 90 days of discharge, and recurring cycles of substance use disorder (SUD) remission, recurrence, and treatment readmission (Brown, Vik, & Creamer, 1989; Cornelius et al., 2003; Dennis et al., 2004; Godley, Dennis, Godley, & Funk, 2004; Godley, Godley, Dennis, Funk, & Passetti, 2007; Hser et al., 2001; Waldron, Slesnick, Brody, Turner, & Peterson, 2001; Winters, Tanner-Smith, Bresani, & Meyers, 2014). However, most research of the clinical course of substance use disorders in adolescents has consisted of secondary analysis of datasets and has analyzed single points of AOD use change over time, rather than the more complex course of these problems over extended periods of time (e.g., remission, relapse, recovery stabilization; Buckheit, Moskal, Spinola, & Maistro, 2018).
Existing sources of post-treatment recovery support for adolescents are marked by varying levels of empirical evidence and fall into one of two categories: professionally-directed “formal aftercare or continuing care services” or peer-based support provided within “recovery communities” (Fisher, 2014). Formal continuing care is typically offered in outpatient clinics to clients who complete their acute episode of care. Clients are usually expected to attend weekly clinic-based group counseling led by clinical staff. Continuing care sessions tend to focus on relapse prevention with other content reflecting the treatment orientation of the clinical program. When adolescents participate in professionally-directed continuing care, there is ample evidence indicating improved substance use outcomes (Burleson, Kaminer, & Burke, 2012; Garner, Godley, Funk, Lee, & Garnick, 2010; Godley & Godley, 2011; Godley et al., 2007, 2014; Kaminer, Burleson, & Burke, 2008; Sterling, Chi, Campbell, & Weisner, 2009).
Recovery communities are a less studied source of recovery support services for adolescents and include mutual support groups, recovery coaches, recovery residences, recovery high schools and collegiate recovery programs, and recovery-focused social clubs. Substance use disorder treatment programs commonly refer adolescents to mutual support groups and in particular, Alcoholics Anonymous (AA) and Narcotics Anonymous (NA; Drug Strategies, 2003; Humphreys et al., 2004; Jainchill, 2000; Jason, Mericle, Polcin, & White, 2013; Kelly et al., 2016). Recovery coaches are newer to the field and help individuals after treatment by offering support, consultation, motivation, feedback, skills training, and assistance in reducing barriers to needed services (Loveland & Boyle, 2005; White, 2009; White & Evans, 2014). Recovery high schools and collegiate recovery communities typically provide group and individual counseling and use eclectic therapeutic approaches (Finch & Karakos, 2014; Finch, Tanner-Smith, Hennessey, & Moberg, 2017; Moberg & Finch, 2008). While more rigorous research is needed of all of these models with adolescent populations, data analyzed to-date indicate that participation in these recovery support services may be beneficial in terms of reduced substance use, increased abstinence rates, longer periods of sustained abstinence, improved academic performance, and improved mental health symptoms (Finch & Wegman, 2012; Kelly & Myers, 2007; Kelly et al., 2017; Passetti, Godley, & Godley, 2012; Passetti & White, 2008; Rattermann, 2014; Ryan, Perron, Moore, Victor, & Park, 2017; Ryan, Victor, Moore, Mowbray, & Perron, 2016; Valentine, 2011).
Even though recovery support services may help adolescents maintain treatment gains, adolescents encounter multiple barriers to initiating and engaging in them. There are not many recovery coaches who specifically target the adolescent population and there are only 40 recovery schools in the United States, with enrollment under 40 students per school (Tanner-Smith, Finch, Hennessy, & Moberg, 2018). Additionally, professionally-provided recovery support and peer-based mutual support groups are often grounded in adult-oriented models that have been applied to adolescents with minimal adaptation. Mutual support groups that offer adolescent-focused meetings vary greatly in terms of their availability and accessibility; therefore, most meetings consist of mainly adult members (Drug Strategies, 2003; Jainchill, 2000; Kelly, Myers, & Brown, 2005; Passetti et al., 2012). Furthermore, continuing care is typically clinic-based and offered only to individuals who complete an acute episode of care, leaving those with transportation issues, who live far away, and who do not complete treatment without support. Not surprisingly, there is often poor linkage from inpatient and residential programs to clinic-based continuing care programs (Godley & Godley, 2011; Godley et al., 2014), and a significant percentage of youth who start attending 12-step meetings eventually stop going (Kelly, Brown, Abrantes, Kahler, & Myers, 2008; Kelly, Myers, & Brown, 2000). Chi and colleagues (2012) found positive effects of post-treatment participation in 12-step meetings, but only 14% of youth studied sustained participation more than 1 year.
Compounding the issue is evidence that recovery support services should extend at least 1 year post-treatment, with some clinical leaders recommending 5 years of post-treatment monitoring and support (DuPont, Compton, & McLellan, 2015; White, 2009), but even 1 year of sustained support is not a part of routine care within the current treatment system (Dennis & Scott, 2007; Flynn & Brown, 2016; McKay, 2005, 2009). First, specialized adolescent treatment programs for substance use disorders are relatively few in number, and provider shortages will most likely increase due to inadequate compensation, high turnover, stigma, and as the aging workforce retires (SAMHSA, 2013; Zornitsky, 2014). Second, the expanded caseloads and clinical staff time needed to provide services for longer periods of time are not possible. Third, funding for treatment from state or federal sources and traditional private payor sources often excludes reimbursement for continuing care and recovery support services (Koyanagi, Alfano, & Stein, 2008). These factors leave most adolescents with few viable options for recovery monitoring and support after treatment.
Assertive Continuing Care (ACC) is an approach that has addressed some of these barriers. ACC differs from usual continuing care in two important ways: (a) adolescents are provided ACC, even if they do not successfully complete their acute treatment episode; and (b) clinicians minimize missed appointments by meeting with adolescents in their homes and other community settings, overcoming a host of factors related to missed clinic appointments (e.g., distance from clinic, transportation, and vacillating motivation). In two separate randomized trials, ACC resulted in high continuing care initiation rates, main effects for ACC in improving days of abstinence and early remission rates, and beneficial effects in clinical outcomes for adolescents with unsuccessful discharges from treatment relative to those who completed (Godley & Godley, 2011; Godley et al., 2007, 2014). Despite positive findings, obstacles to providing services remain. ACC can be expensive to deliver because of the staff time and travel required, and payor sources for continuing care remains challenging. Further, outcome effect sizes of ACC, while significant relative to usual continuing care, are generally small (using Cohen’s d), even when augmented with contingency management for abstinence and prosocial activities (Godley et al., 2014). The combination of implementation barriers and small effect sizes supports examining whether a less costly, longer duration intervention might provide similar or improved benefit over time.
A novel approach that addresses many of the barriers adolescents encounter when accessing and engaging in recovery support services is to deliver support by telephone provided by trained volunteers. Studies of programs for smoking cessation and monitoring and treating chronic mental and physical health problems (such as depression, obsessive-compulsive disorder, hypertension, diabetes, and rheumatology problems) indicate that telephone care can be as effective as in-person meetings (Bosworth et al., 2005; Greist et al., 2002; Kim & Oh, 2003; Lichtenstein, Glasgow, Lando, Ossip-Klein, & Boles, 1996; Osgood-Hynes et al., 1998; Pal, 1998; Simon, VonKorff, Rutter, & Wagner, 2000; Stead, Perera, & Lancaster, 2006; Taylor et al., 2003). Telephone-based continuing care for substance use disorders has shown promise with adults (Cacciola et al., 2008; Godley et al., 2010; McKay et al., 2004, 2011) and adolescents (Garner, Godley, Passetti, Funk, & White, 2014; Kaminer & Napolitano, 2004).
While telephone-delivered care has been applied to a wide range of problems, volunteers also have a history of being trained to provide support to a variety of patients and clients. Volunteers have been shown to help patients increase the duration of breast feeding in new mothers (Dennis, Hodnett, Gallop, & Chalmers, 2002), improve coping with back pain (Von Korff et al., 1998), and improve the health behaviors and health status of chronic disease patients (Lorig et al., 1999). Similarly, studies of volunteers suggest that they can contribute to the enhancement of treatment and long-term recovery outcomes (Bassuk, Hanson, Greene, Molly, & Laudet, 2016; Reif et al., 2014). Volunteer service to others in mutual support groups has also been associated with increased engagement with treatment, improved treatment retention, and/or decreased alcohol and other drug use (Boyd et al., 2005; Dembo, Wothke, Livingston, & Schmeidler, 2002; Grant, Ernst, Streissguth, Phipps, & Gendler, 1996; Lee, Pagano, Johnson, & Post, 2016; Leigh, Hodgins, Milne, & Gerrish, 1999; Pagano, Friend, Tonigan, & Stout, 2004; Stahler et al., 2007; Zemore, Kaskutas, & Ammon, 2004). Additional detailed background and description of volunteers in substance use care is provided in a companion paper (Passetti et al., under review).
Volunteer Recovery Support for Adolescents (VRSA) is a model that trains volunteers to provide recovery monitoring and support for adolescents after their discharge from residential treatment for substance use problems. The model combines post-treatment monitoring techniques (Dennis & Scott, 2012) with a subset of procedures from the Adolescent Community Reinforcement Approach (Godley, Smith, Meyers, & Godley, 2016). Based on a substantial body of research concluding that substance-using peers are a significant predictor of alcohol and other drug use and that positive peer support is associated with long-term recovery, VRSA focuses on increasing affiliation with peers who support recovery and increasing participation in recovery-focused activities, including mutual support group attendance (Bassuk et al., 2016; Creemers et al., 2010; Leung, Toumbourou, & Hemphill, 2014; Van Ryzin, Fosco, & Dishion, 2012) and continuing care treatment (Godley et al., 2007). A quasi-experimental study demonstrated that youth receiving VRSA had significantly greater improvement in their recovery environment risk (e.g., more participation in 12-step mutual aid, less fighting, less victimization) when compared to a matched sample, and had significant indirect improvement in substance use and substance-related problems (Garner et al., 2014).
The present study reports findings of a randomized trial testing the hypotheses that relative to services as usual (SAU), VRSA would lead to the following significant direct effects: (1) more pro-recovery peers and recovery management activities; and (2) less AOD use and problems, and higher rates of remission at the end of the intervention phase and 3 months post intervention. The indirect effects hypothesis predicted that relative to SAU, VRSA would significantly: (3) reduce AOD use and problems and increase remission at the end of the intervention phase and 3 months post-intervention via pro-recovery peers and recovery management activities.
2. Method
2.1. Design
Participants were recruited into the study by research staff upon admission to any one of four residential treatment programs for substance use disorders located in Arizona and Illinois between January 2013 and February 2016. After agreeing to participate, eligible and enrolled adolescents were randomly assigned by research staff either to SAU or VRSA within each site using urn randomization software (Charpentier, 2003). Urn randomization uses a Bayesian approach that adjusts the probability of assignment to condition in a way to minimize any differences in the stratification variables (Dennis, Perl, Huebner, & McLellan, 2000; Stout, Wirtz, Carbonari, & Del Boca, 1994). Urn randomization was conducted by site and included gender (male/female), age (median split), race (Caucasian/not Caucasian), number of days abstinent out of the 90 days prior to residential treatment admission (median split), treatment readiness (median split of an index measuring an individual’s motivation for and resistance to substance use treatment), Substance Problems Scale score (described under section 2.4; median split), presence of a mental health disorder (yes/no), social risk (median split of an index measuring how much time an individual spends with people using alcohol or other drugs, involved with illegal activities, not in school or work, or who have never been in treatment), and being on probation or parole (yes/no).
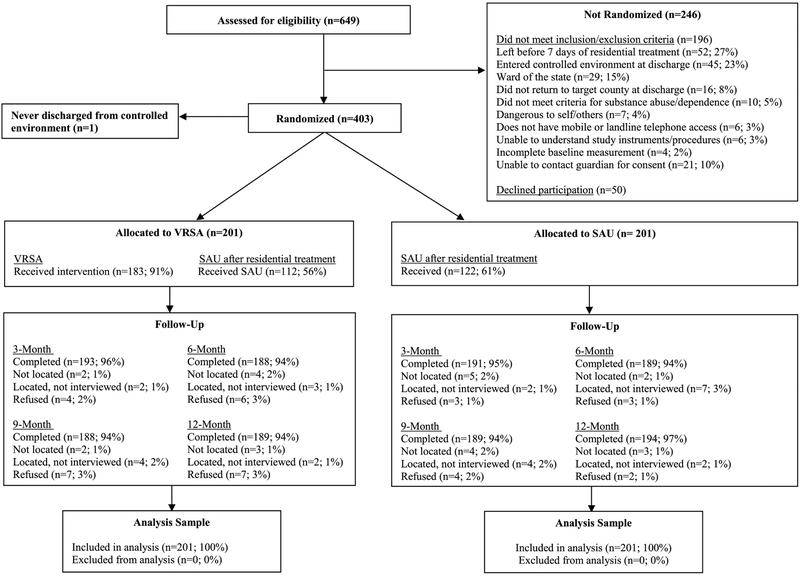
Two hundred two adolescents were assigned to the SAU condition, and 201 were assigned to VRSA between January 2013 and February 2016. Research staff or volunteer notified participants and guardians of their condition assignment at residential discharge. Research staff who did not deliver interventions collected data during study intake and at 3, 6, 9, and 12 months after residential discharge. Follow-up interview completion rates were 95% at 3 months, 94% at 6 months, 94% at 9 months, and 95% at 12 months.
2.2. Participants
Participation was voluntary and under the supervision of Chestnut Health Systems’ Institutional Review Board. In order to be enrolled, adolescents had to meet the following eligibility criteria: (a) be aged 12–18 at the time of residential treatment admission; (b) meet DSM-IV-TR diagnostic criteria for alcohol or other substance abuse or dependence; (c) be enrolled in and remain in residential treatment for at least 7 days; (d) reside in the study’s geographical catchment area; and (e) have access to a mobile or landline phone. Adolescents were not eligible if they: (a) showed evidence of a psychotic or organic state of sufficient severity to interfere with understanding of project instruments, project procedures, or the informed consent process; (b) were deemed an imminent danger to self or others; (c) were currently a ward of state child protective services in Illinois; or (d) were scheduled to enter a state juvenile correctional institution within 3 months of residential treatment discharge. Out of 649 adolescents screened, 453 were eligible, and 403 (90%) agreed to participate (see Figure 1). Enrolled youth were primarily male (86%), Caucasian (49%) with approximately equal distributions for African American (18%), Hispanic (14%), and mixed ethnic groups (19%). The primary drug of choice was cannabis followed by alcohol with a variety of other drugs constituting the remainder of use. Eighty five percent of the sample reported AOD use weekly or more often. There were no significant differences between conditions on demographic or clinical intake measure (see Table 1).
Fig. 1.
Participant flow by experiment condition.
Table 1.
VRSA Participant Intake Characteristics by Condition Assignment
| SAU (n = 201) |
VRSA (n = 201) |
Total (n = 403) |
χ2 | P | |
|---|---|---|---|---|---|
| Female | 15% | 17% | 16% | 0.32 | 0.588 |
| Race | 2.25 | 0.528 | |||
| Caucasian | 49% | 48% | 49% | ||
| African American | 19% | 18% | 18% | ||
| Hispanic | 16% | 12% | 14% | ||
| Other/Mixed | 16% | 21% | 19% | ||
| Non-white | 51% | 52% | 51% | 0.02 | 0.921 |
| Age | 1.51 | 0.496 | |||
| 12–14 Years Old | 14% | 14% | 14% | ||
| 15–17 Years Old | 78% | 81% | 79% | ||
| 18–20 Years Old | 8% | 5% | 7% | ||
| Regular Peer Alcohol Use\l | 69% | 66% | 68% | 0.42 | 0.523 |
| Regular Peer Drug Use\2 | 88% | 89% | 89% | 0.05 | 0.875 |
| Current CJ Involvement\3 | 82% | 86% | 84% | 1.10 | 0.340 |
| Controlled Environment\3 | 68% | 72% | 70% | 0.70 | 0.448 |
| Victimized in past year\4 | 29% | 30% | 29% | 0.17 | 0.743 |
| Weekly AOD use\3 | 87% | 83% | 85% | 1.02 | 0.327 |
| Weekly Alcohol Use\3 | 27% | 25% | 26% | 0.32 | 0.650 |
| Weekly Cannabis Use\3 | 77% | 75% | 76% | 0.24 | 0.644 |
| Age of First Use Under 15 | 91% | 88% | 89% | 1.36 | 0.262 |
| Substance Use Severity | 0.13 | 0.942 | |||
| Substance Use\5\7 | 5% | 5% | 5% | ||
| Substance Abuse\5\7 | 15% | 16% | 16% | ||
| Substance Dependence\5\7 | 80% | 79% | 79% | ||
| Any Prior Substance Treatment | 75% | 74% | 74% | 0.01 | 1.000 |
| Any internalizing disorders\7\8 | 54% | 57% | 56% | 0.36 | 0.616 |
| Any externalizing disorders\7 | 73% | 75% | 74% | 0.18 | 0.735 |
| Any MH Treatments\6 | 65% | 71% | 68% | 1.57 | 0.238 |
| Mean(SD) | t | P | |||
| Residential length of stay | 80.08(80.02) | 71.43(52.38) | 75.74(67.65) | 1.28 | 0.200 |
| Pro-Recovery People Index\3 | 14.55(5.42) | 13.93(5.51) | 14.24(5.47) | 1.13 | 0.259 |
| Drug Free Sobriety Activities\3 | 0.41(0.48) | 0.40(0.47) | 0.40(0.47) | 0.15 | 0.878 |
| Substance Abuse Treatment Index\3 | 0.09(0.15) | 0.11(0.19) | 0.10(0.17) | −1.13 | 0.259 |
| Alcohol or Other Drug Use\3 | 0.73(0.34) | 0.72(0.36) | 0.73(0.35) | 0.05 | 0.960 |
| Substance Problem Scale | 5.81(4.61) | 5.16(4.76) | 5.49(4.69) | 1.39 | 0.116 |
Notes. \1 = Spent time in the past year with 1 or more people socially who got drunk weekly; \2 Spent time in the past year with 1 or more people socially who used drugs quarterly; \3 During the past 90 days; \4 Attacked with a weapon, beaten, sexually assaulted, or emotionally abused; \5 Based on selfreport GAIN items that map onto DSM IV criteria; \6 During Lifetime; \7 During past year; \8 Major Depression, generalized anxiety, or traumatic stress disorder; \9 Attention Deficit Hyperactivity Disorder or conduct disorder.
2.3. Interventions
2.3.1. Services As Usual (SAU)
Adolescents assigned to the SAU condition received the typical services offered at discharge from residential treatment. At three of the study’s performance sites, adolescents who left treatment as planned received recommendations for participation in continuing care at an outpatient program in their home communities as well as other recovery support services, such as mutual aid groups. An appointment was made for the first continuing care session, and a disclosure was signed and sent to the program to check if the adolescent connected after leaving residential care. If adolescents left residential treatment against staff advice or at staff request, recommendations for continuing care and recovery support services were made to caregivers. One of the performance sites provided direct care coordination after discharge with case managers, probation officers, biological parents, or child welfare workers rather than make formal recovery support recommendations. SAU at each site was delivered as it would be independent of this experiment.
2.3.2. Volunteer Recovery Support for Adolescents (VRSA)
In addition to SAU, adolescents assigned to the VRSA condition received study-provided recovery support services that combined a small subset of Adolescent Community Reinforcement Approach (A-CRA) procedures with VRSA-specific procedures. A-CRA is an evidence-based treatment for youth with substance use problems that has been described in detail elsewhere (Dennis et al., 2004; Godley, Smith, Meyers, & Godley, 2009, 2016). Since VRSA was delivered by volunteers rather than clinicians, A-CRA procedures were chosen for implementation in this study based on their ability to be provided by individuals without clinical degrees and experience while maintaining a focus on increasing pro-recovery peers and activities. VRSA used the following A-CRA procedures during recovery support sessions: (a) increasing pro-social behavior (involvement with pro-recovery peers and activities); (b) goal setting; and (c) client-directed homework. More specifically, volunteers were trained to talk to adolescents about time spent participating in substance-free pro-recovery activities and with nonsubstance-using people. Any attempts by adolescents to do so were praised by the volunteers, and ways to increase these behaviors and reduce barriers to engagement were identified. Volunteers also facilitated setting goals that were positive, specific, brief, and under the adolescent’s control to achieve. Any obstacles to completing goal-related homework were explored along with focusing on ways to overcome them. Progress on goal achievement was discussed during the next session. VRSA-specific “procedures” included: (a) general convivial conversation with the adolescent and providing an opportunity to talk about how things were going; (b) asking about any use of substances since the last call; (c) asking about any cravings or opportunities to use substances that were experienced; (d) the identification of any upcoming situations that might present a risk for relapse and problem-solving for how to handle those events; and (e) referrals for further treatment services when adolescents reported relapse or mental health problems. VRSA protocol was flexible so that sessions were conversational rather than adhering to a strict procedural format.
Health and human services students served as volunteers and were trained at the research facility over a 6-hour period. Prior recovery experience was not required, and only 1 volunteer identified themselves as being in recovery. Their average age was 23 years old, and 86% were female. Eighty-two percent identified as White, 1% as African-American, and less than 1% as Native American or Asian. Nineteen percent were Hispanic. Once training was completed, volunteers recorded recovery support sessions and uploaded recordings to a secure website along with information about session dates, times, and procedures covered. All support sessions completed by short-term volunteers (1 academic semester) were reviewed by research staff. If a volunteer decided to become long-term (i.e., volunteer longer than 1 academic semester), random sessions were reviewed once the initial semester of commitment was completed. If any problems were identified, sessions were reviewed more frequently until those issues were resolved. Analysis of participants receiving 1+ telephone call with one long-term volunteer (n=62 participants) versus those with multiple short-term volunteers (n=121 participants) revealed no significant differences on substance use outcomes.
Each reviewed session was rated for fidelity to the VRSA model by assigning a numeric rating between 1 and 5 for every procedural component delivered using a standardized scoring manual based on prior A-CRA and VRSA model fidelity (Smith, Lundy, & Gianini, 2007; Garner, Barnes, & Godley, 2009; Garner et al., 2014). A score of 1 indicated poor fidelity, and a score of 5 indicated excellent fidelity. Feedback was provided to volunteers in written form through a web-based system and orally through weekly supervision in person, over the phone, or via Skype. A detailed description of VRSA and the volunteer characteristics, recruitment, retention rates, training, supervision, implementation, and fidelity results can be found at Passetti et al. (under review).
Volunteers attempted to initiate recovery support sessions with adolescents assigned to the VRSA condition by telephone immediately after residential discharge. VRSA was designed to add 9 months of recovery support services to approximately 3 months of residential treatment in accordance with extended monitoring and treatment recommendations (Dennis & Scott, 2007; McKay, 2005, 2009). Recovery support sessions were scheduled weekly for the 3 months after discharge. For the subsequent 6 months, session frequency was adjusted based on adolescent’s needs and functioning (McKay, 2005). Sessions were kept at the same rate or increased in frequency for those adolescents who reported any of the following since the last contact: (a) any alcohol or other substance use; (b) 1 or more days of alcohol or substance-related problems; (c) worsening of existing problems; (d) the emergence of new problems; or (e) a request to continue weekly contacts. Conversely, session frequency was decreased to or maintained at every other week when a youth reported: (a) no alcohol or other substance use for at least 30 consecutive days; or (b) a request to have contacts less often.
Volunteers were instructed to complete sessions at times convenient to adolescents, including evenings and weekends. Sessions lasted approximately 15 to 20 minutes and were conversational in tone. Text messaging was used to remind adolescents of upcoming support sessions, request them to answer calls from the volunteer, support goal completion, to check in on birthdays or after special events (e.g., a job interview), and to complete a support session if requested by an adolescent. The average number of text messages sent per week varied greatly and depended on youth preference and responsiveness.
2.4. Assessment Procedures
Adolescents were assessed at intake to residential treatment and all post-discharge time points by interviewers certified in the Global Appraisal of Individual Needs (GAIN; Dennis, Titus, White, Unsicker, & Hodgkins, 2003). A supplemental form was also administered with the GAIN that gathered data related to involvement with pro-recovery people and activities. Urine samples were collected and screened by research staff using an immunochromatographic assay with a 1-step drug cup (CLIAwaived.com, San Diego, CA) at the 3- and 12-month follow-up for alcohol, amphetamines, barbiturates, benzodiazepines, cocaine, opiates, methadone, MDMA/methylenedioxymethamphetamine/ecstasy, methamphetamine, PCP/phencyclidine, and THC/marijuana. Temperature and contaminant-monitored instant urine test kits were used to give feedback to study participants regarding substance use just prior to administering the interview questions. All research staff were trained and received feedback on all of the above measures (including urine testing) and until certified in GAIN administration (see Titus et al., 2012 for more details). To maintain quality, GAIN interviews were recorded and randomly selected for review and feedback. Compared to urinalysis results, false negative reporting on the GAIN interview was 2.4% at 3 months and 3.1% at 12 months for the total sample, with no significant difference between conditions.
The following measures were used in tests of the direct and indirect effects of VRSA:
Pro-Recovery People Index (PRPI; Longabaugh, Wirtz, Zywiak, & O’Malley, 2010) was used to assess the degree to which adolescents spent time with pro-recovery people. Adolescents were asked to list people they spent most of their time with in the past 90 days, describe their relationship to each person, rate how important each person was to them during the past 90 days (1=not at all important to 6=extremely important), and rate how supportive each person was to their recovery during the past 90 days (1=not at all supportive to 4=extremely supportive). The index was calculated by multiplying the importance of each person by how supportive the person was to the participant’s recovery and then averaging across all important people. Because PRPI is a measurement made up of multiple indicators (people) of support, which are weighted by importance, the indicators would not be expected to be highly correlated. Thus, internal consistency would not be a good measure of reliability (Bollen, 1984).
Drug-Free Sobriety Activities (DFSA) is the proportion of days out of the past 90 days that the participant was involved in drug-free activities related to sobriety. Higher scores indicate increasingly more involvement in drug-free sobriety activities.
Substance Abuse Treatment Index (SATI) is the percentage of days out of the past 90 days in which the participant received outpatient or intensive outpatient continuing care treatment for substance use. Higher scores indicate increasingly more involvement in substance abuse treatment continuing care (GAIN Coordinating Center, 2012). Similar to PRPI, SATI is an index made up of multiple indicators that are not expected to be correlated, and internal consistency would not be a good measure of reliability.
Self-Help Activities Scale (SHAS) is a count of self-help activities endorsed out of 19 possible activities (e.g., spoken during meeting, had a sponsor, read recovery-related readings, worked the 12 steps). Higher scores indicate a participant was increasingly involved in self-help activities (GAIN Coordinating Center, 2012). Internal consistency using Cronbach’s α ranged from .952 to .959 across observation waves.
Alcohol and Other Drug Use (AOD) was calculated as the self-reported proportion of days using any alcohol or other drugs while in the community (the denominator excluded days the participant was in a controlled environment where access to alcohol and other drugs was prohibited) out of the past 90 days. Higher scores indicate increasingly more days of substance use during the past 90 days. Adolescent self-reported measures of substance use from the GAIN have been shown to be consistent with collateral reports and urine testing (Godley, Godley, Dennis, Funk, & Passetti, 2002). The impact of VRSA on alcohol use was initially examined separately from other drug use. There was no significant direct effect of VRSA on alcohol use. Alcohol use and other drug use were correlated (r (402) = .36, p < .001 at the 9-month observation; r(402) = .33, p < .001 at the 12-month observation), thus they were combined to assess direct and indirect effects in the structural equation model to improve fit and performance.
Substance Problem Scale (SPS) is a count of past month symptoms of substance use disorders, and substance induced health and psychological disorders based on the DSM-IV. Higher scores indicate greater severity of drug problems (GAIN Coordinating Center, 2012). Cronbach’s α for internal consistency ranged from .903 to .927 across observation waves.
Remission.
A participant was considered to be in (early full) remission (APA, 2000) if: (a) they were living in the community; (b) abstinent from all drugs and alcohol in the past month; and (c) reported no past month AOD-related problems. A value of 1 indicates a participant met all of the aforementioned criteria, while a value of 0 indicates that a participant did not meet at least one of the criteria (GAIN Coordinating Center, 2012).
2.5. Statistical Analysis
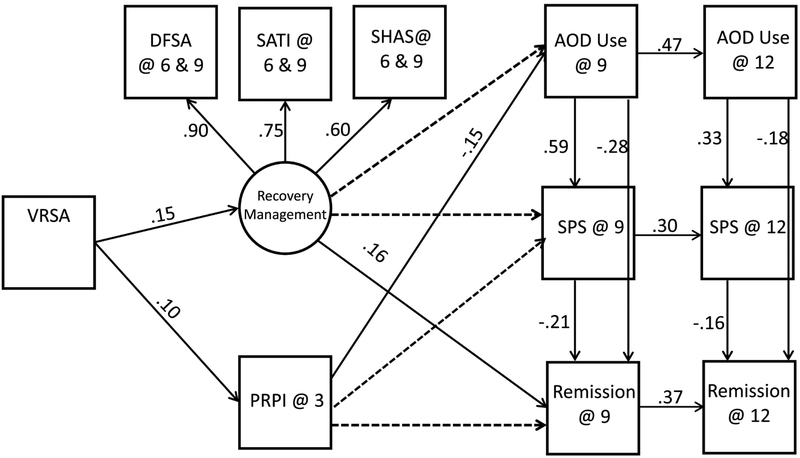
Development of the analytic model was guided by our theory of change as expressed through the hypotheses. The direct effects of condition assignment (SAU=0; VRSA=1) were assessed through a series of bivariate linear and logistic regression analyses, where each proximal (e.g., PRPI, DFSA, SATI, SHAS) and distal outcome (e.g., AOD use, SPS, remission status) were regressed on condition assignment. Cohen’s d was calculated to quantify effect sizes for the direct effects. Subsequently, a structural equation model (SEM) was developed to assess the indirect effects of condition assignment on the distal outcomes through the proximal outcomes (O’Rourke & MacKinnon, 2018). The significance levels of the indirect effects were determined using bootstrap bias-corrected confidence intervals (Preacher & Hayes, 2004; Shrout & Bolger, 2002). DFSA, SATI, and SHAS were analyzed as a latent variable, referred to as recovery management hence forth. In the SEM, they were correlated (rDFSA,SATI(402) = .49, p < .001; rDFSA,SHAS(402) = .67, p < .001; rSATI,SHAS(402) = .44, p < .001). The final model was developed through an iterative process where paths were eliminated based on significance (α = .05) of the path coefficients and the model fit indices. Figure 2 illustrates both the hypothesized and final model. A collection of fit indices were examined to determine model fit (Tanaka, 1993). IBM SPSS AMOS version 24.0.0 structural equation modeling software was used to assess the model. Intake values of AOD use and SPS were included in the analysis of both the direct and indirect effects to control for intake differences. The intake value of remission was not included in any analyses because it was not significantly related to remission at the 9- or 12 month observation.
Fig. 2.
Hypothesized model and final results. Notes. VRSA = Volunteer Recovery Support for Adolescents, PRPI = Pro Recovery People Index, DFSA = Drug Free Sobriety Activities, SATI = Substance Abuse Treatment Index, SHAS = Self Help Activities Scale, AOD=Alcohol & Other Drugs, and SPS = Substance Problem Scale. All paths were in the hypothesized model. Solid paths represent the final model. The fit indices for the model were: χ2/df = 1.93, Comparative Fit Index = 0.95, Normed Fit Index = 0.90, and Root Mean Square Error of Approximation = 0.048.
Follow-up rates at each wave exceed 93% and between 4.7% and 7.7% of data were missing for any given variable used in the analyses. Missing data were replaced with the SPSS Replace Missing Value procedure in which records were sorted by site, gender, race, and relevant context variables and then replaced with the median of the four nearest valid responses (McDermeit, Funk, & Dennis, 1999).
A dose-response analysis was conducted for VRSA participants to examine the relationship between percent of VRSA sessions completed and the proximal outcomes and AOD remission status at the end of VRSA. Regression analyses were used to examine incremental improvement in the dose-response relationship.
3. Results
3.1. VRSA Initiation and Exposure
Sixty-three percent of participants received their first VRSA support call within 2 weeks of residential discharge. The observed session completion rate was 51% (2,135/4,211 possible sessions), with 49% of participants completing more than half of all scheduled support calls and 76% finishing the planned 9-month support call period. The average fidelity score was 3.77 (.56), indicating above average to good fidelity across all volunteers and protocol procedures. See Passetti et al. (under review) for more detailed fidelity results. No adverse events related to the research were reported.
3.2. Direct Effects of VRSA
A series of bivariate linear regression models revealed that VRSA had significant direct effects on all proximal outcomes (see Table 2). VRSA had a positive impact on change in pro-recovery people from intake to 3 months such that participants randomized to VRSA reported a greater increase in the number of pro-recovery people in their lives compared to participants randomized to SAU (Cohen’s d = .20). Participants randomized to VRSA also had greater increases in drug-free sobriety activities (Cohen’s d = .21), substance abuse treatment (Cohen’s d = .31), and self-help activities (Cohen’s d = .30), indicating that they engaged in more mutual aid group activities and additional continuing care treatment than participants randomized to SAU. No significant direct effects of VRSA were found for distal outcomes: AOD use, substance problems, or remission.
Table 2.
Bivariate linear regression results for direct effects for proximal outcomes, where each outcome was regressed on condition assignment(N = 402)
| Outcomes | B | SE(B) | β | p-value |
|---|---|---|---|---|
| Pro-Recovery People Index change @ 3 months | 1.219 | .436 | .098 | .035 |
| Sobriety Related Activities @ 6 & 9 months | .062 | .029 | .106 | .033 |
| Self-Help Activity Scale @ 6 & 9 months | 2.037 | .671 | .150 | .003 |
| Substance Abuse Treatment Index @ 6 & 9 months | .055 | .018 | .154 | .002 |
3.3. Indirect Effects of VRSA
The indirect effects of VRSA on the distal outcomes via the proximal outcomes were analyzed using a structural equation model to test the hypothesized model. Both hypothesized and final model with fit statistics are shown in Figure 2. All paths retained in the final model were significant. In addition to significant direct effects on change in pro-recovery people and recovery management, the structural equation model revealed significant indirect effects on AOD use, substance problems, and remission at both 9- and 12-month follow-up interviews (see Table 3). VRSA had significant indirect effects on both AOD use and substance problems via change in pro-recovery people, where increased pro-recovery people predicted decreased AOD use and decreased AOD use predicted decreased substance problems. VRSA had a significant indirect effect on remission via recovery management, where increased mutual aid group involvement and participation in continuing care treatment predicted an increased rate of remission.
Table 3.
Indirect effects of VRSA on distal outcomes (N = 402)
| Indirect Effect | B | β | 95% C.I. | p-value |
|---|---|---|---|---|
| Alcohol & Other Drug Use @ 9 Months | −.012 | −.015 | −.039, −.001 | .033 |
| Alcohol & Other Drug Use @ 12 Months | −.005 | −.007 | −.020, −.001 | .024 |
| Substance Problem Scale @ 9 Months | −.058 | −.009 | −.025, −.001 | .031 |
| Substance Problem Scale @ 12 Months | −.032 | −.005 | −.014, .000 | .029 |
| Remission @ 9 Months | .028 | .030 | .010, .063 | .006 |
| Remission @ 12 Months | .011 | .013 | .005, .027 | .008 |
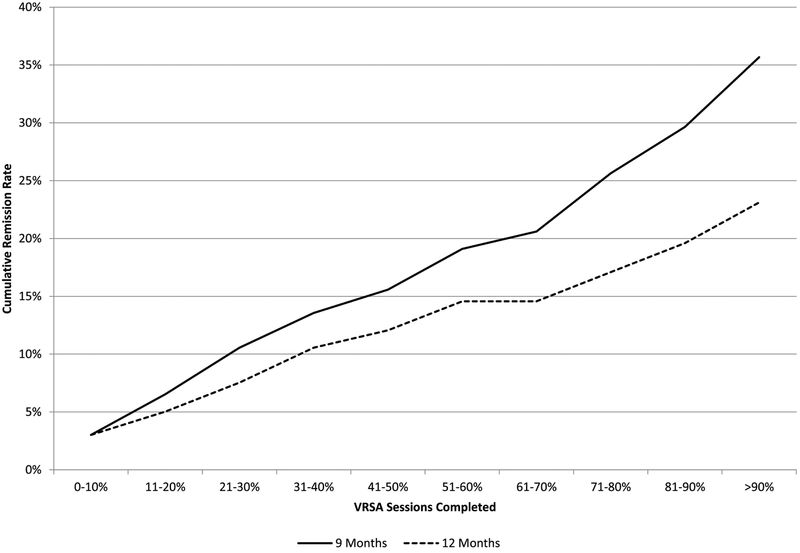
3.4. VRSA Condition Dose-Response
VRSA call completion rates (ratio of completed to expected recovery support calls) had direct positive effects on each recovery management variable (DFSA, SATI, SHAS) and AOD remission at 9 months. As call completion rates increased, so did each of the aforementioned outcomes. For every 10% increase in call completion rate, VRSA participants increased their count of drug-free sobriety activities by nearly 1 activity (B = .937, t(197) = 2.614, p = .010) and increased their percentage of days in continuing care outpatient substance use treatment by 1.5% (B = .015, t(197) = 3.064, p = .002). For every 20% increase in call completion rate, participants increased the number of self-help activities they engaged in by 1 activity (B = .509, t(197) = 2.783, p = .006). As the recovery management support call completion rate improved, so did the AOD remission rate for VRSA participants (Figure 3). Every 10% increase in recovery support call completion rate significantly increased the odds of being in remission at the end of the VRSA intervention phase – 9 months after residential discharge (OR = 1.14, p = .012, 95% CI = 1.03, 1.27). However, the dose-response result at the 12-month follow-up (3 months post VRSA) was not significant. Figure 3 depicts the 9- and 12-month dose-response relationship.
Fig. 3.
Dose response at the end of VRSA intervention phase (9 month follow-up) and 3 months post-VRSA (12-month follow-up).
4. Discussion
This study is the first known randomized trial of a volunteer delivered, adaptive recovery management and support intervention for youth. The results indicated that the VRSA direct effects hypotheses received mixed support in the intent to treat analyses. Compared to the SAU condition, per hypothesis 1, there was a significant effect for VRSA participants to improve proximal outcomes. Both recovery management activities and pro-recovery people were significantly improved by VRSA relative to SAU youth. However, analyses did not confirm direct effects for distal outcomes (AOD use, problems, and remission) for hypothesis 2.
Hypothesis 3, relating to indirect effects of VRSA, was confirmed. Analyses providing evidence that relative to SAU, VRSA (through its twin effects of increasing association with pro-recovery peers and recovery management activities) reduced AOD use and problems and increased the rate of remission from substance use at the 9- and 12-month follow-ups. Moreover, the SEM met widely recommended criteria for demonstrating indirect effects in clinical trials (e.g., theory driven models of change over time; Longabough, Magill, Morgenstern, & Huebner, 2011; MacKinnon, 2008; O’Rourke & MacKinnon, 2018; Shrout & Bolger, 2002).
In the current study, we found that VRSA increased the likelihood that a participant would engage in recovery management activities (sobriety related activities, self-help, and additional substance use treatment) after discharge from residential treatment, which in turn increased the likelihood that a participant would be in remission at the end of the intervention out to 3 months beyond the intervention. Also, VRSA participants were more likely to increase their pro-recovery peer network, which in turn decreased the likelihood of AOD use and substance problems at the end of the intervention and out to 3 months beyond the intervention. These findings provide initial evidence that support calls made by the volunteers continued to have some effectiveness 3 months after the last calls were made.
The dose-response analysis demonstrated that compared to the low VRSA session completers, participants with high rates of VRSA session completion engaged in recovery management at higher rates, reported a greater increase in pro-recovery peers, and demonstrated higher rates of remission at 9 months post-discharge from residential treatment. Despite the decrease in remission at the 12-month follow-up (3 months post intervention phase), there was still a significant indirect effect of VRSA on all substance outcomes.
These results suggest two possible VRSA change mechanisms. First, higher VRSA session completion rates may lead to improvements in recovery management variables, such as continuing care outpatient treatment attendance and mutual support group attendance and affiliation due to the A-CRA short-term goal setting and homework review procedures conducted during each VRSA session. Second, as VRSA session completion rates increased, the possibility that recovery support calls were temporally aligned with high-risk substance use opportunities may have assisted youth in developing specific plans to avoid a recurrence of AOD use and related problems. Change mechanisms related to call completion rates and specific intervention procedures are an important area for future research as remission rates were noteworthy for the high call completers. For example, nearly half (49%) of the 60 VRSA participants completing 70+ % of their expected recovery support calls were in remission at the end of the 9-month intervention phase. However, this high completer group also experienced a decline in remission at 12 months. The optimal duration of VRSA calls is not clear, although several researchers have suggested post-treatment support continue for 12+ months (Dennis & Scott, 2007; McKay, 2005, 2009; White, Boyle, & Loveland, 2002) and as long as 5 years (DuPont et al., 2015). Finally, research is needed to better understand client, volunteer, and protocol factors that may increase VRSA recovery support call completion for youth with low completion of expected sessions.
When comparing results from this study to other published studies of telephone-based recovery support, findings are generally consistent. Kaminer et al. (2008) conducted a randomized study of active aftercare, including a brief telephone cognitive behavior therapy condition following completion of outpatient counseling for adolescents with alcohol use disorders. Similar to the reduction in substance use found in this study (although indirect), youth receiving active aftercare (in-person or by phone) were less likely to relapse over time and report fewer drinking and heavy drinking days per month than those with no active aftercare. In one randomized study (Godley et al.; 2010), paraprofessional staff and volunteers delivered telephone-based continuing care to adults for the first 3 months after residential discharge. At 3month follow-up, clients receiving telephone continuing care reported significantly fewer pastmonth substance problems than those who received usual continuing care, but like the present study, these data supported extending the intervention for a longer time as results eroded after the intervention was withdrawn. Additionally, McKay et al. (2011) found that 18 months of telephone continuing care after intensive outpatient treatment improved drinking outcomes (% of days drinking) for participants with alcohol dependence, but those effects also did not persist after the end of the intervention. A 1-year telephone-based continuing care program after residential treatment was implemented by the Betty Ford Center. Similar to the dose-response relationship identified in this study, the researchers concluded that greater participation in the program was associated with higher rates of 12-step meeting attendance and contact with a sponsor (Cacciola et al., 2008).
Consistent with other research in the substance use treatment field (Boyd et al., 2005; Dembo et al., 2002; Garner et al., 2014; Grant, Ernst, Pagaliluan, & Streissguth, 2003; Leigh et al., 1999), results from the present study demonstrate that volunteers can be successfully trained and supervised to implement a recovery support intervention for adolescents. Volunteers initiated recovery support within 14 days of residential discharge for 63% of participants. This finding is important because it is based on a widely accepted performance measure of continuity of care (Garnick et al., 2002), exceeds rates associated with usual continuing care (Garner et al., 2010; Garnick et al., 2002), and predicts higher rates of early remission after residential treatment (Garner et al., 2010). In addition, volunteers were able to complete 51% of all expected recovery support calls, which compares favorably to protocol implementation reported in published studies of telephone-based continuing care and recovery support (Cacciola et al., 2008; Garner et al., 2014; Godley et al., 2010; McKay et al., 2011); however, the rate was less than homedelivered ACC at 78% (Garner et al., 2010).
The comparatively high rate of VRSA recovery support session completion is not surprising given the assertive nature of the model. Volunteers initiated contacts with youth in accordance with the adaptive decision rules guiding the schedule of sessions throughout the 9month intervention phase. Rather than waiting for adolescents to call in for scheduled appointments, volunteers were trained to make repeated attempts to complete recovery support sessions every time one was expected. By design, this level of effort was meant to increase the likelihood that volunteers would be responsive to potential relapse cues closer in time to their actual occurrence than might be achieved by quarterly recovery management checkups (Dennis & Scott, 2012; Scott & Dennis, 2011) and over a longer post-treatment support period than relatively short-term adolescent continuing care models (Godley et al., 2007, 2014; Kaminer et al., 2008).
4.1. Study Strengths and Limitations
This study builds on the findings of an earlier quasi-experimental study (Garner et al., 2014), suggesting that student volunteers can be an effective source of recovery support for youth. Additional strengths included strong implementation, monitoring, measurement, and statistical methods that facilitated tests of direct and indirect relationships between condition assignment and outcomes, and the assessment of VRSA dose-response relationship. The sample was relatively large for a youth study and ethnically diverse. Youth were treated for substance use disorders that were typically complicated by high rates of co-occurring mental health and/or juvenile justice problems, making this sample generally similar to youth in substance use disorder treatment, particularly residential treatment. In addition, the high rate of participant enrollment and follow-up supports external validity of the findings. However, these youth were largely from rural and small to medium size urban communities and may not be representative of youth from large metropolitan areas.
Limitations included the reliance on self-report measures of substance use and problems, although research has generally pointed to the accuracy of self-reports (Buchan, Dennis, Tims, & Diamond, 2002; Del Boca & Noll, 2000; Godley et al., 2007). Self-report validity was further supported by using temperature and contaminant monitored instant urine test kits to give feedback to study participants regarding substance use just prior to administering the interview questions. This study was conducted with adolescents admitted to residential treatment where youth are often exposed, if not required, to participate in 12-step mutual aid meetings, and this may have provided a foundation for the VRSA calls to increase proximal recovery management outcomes. It is unclear to what extent VRSA calls would be effective with youth who may receive less indoctrination into 12-step mutual aid during outpatient treatment.
The use of volunteers to deliver the VRSA intervention was supported, but the typical volunteer served 1 academic semester, suggesting that most youth were served by at least 2 volunteers. While volunteer turnover meant that most youth had to form relationships with new volunteers, there was no significant differences in substance outcomes for youth completing sessions with 1 volunteer versus those completing sessions with multiple volunteers. A detailed discussion of volunteers, including strengths and limitations, is provided in a companion paper (Passetti et al., under review).
The lack of direct effects on substance use outcomes may be viewed as a study limitation; however, both the indirect effects and dose-response results lend support to important mechanisms underlying improved outcomes (pro-recovery people and activities). These mechanisms are consistent with recent research supporting the need for increasing sources of positive, recovery enhancing people and activities to help prevent relapse and develop the recovery capital needed to support long-term recovery (Best et al., 2012; Cloud & Granfield, 2008; McKay, 2017). Potential mechanisms of VRSA responsible for change in the proximal outcomes (e.g., volunteer characteristics, intervention procedures) were not studied and requires additional research. Finally, it is possible that high VRSA session completers were different than low session completers, which could have contributed to the observed dose-response relationship. Additional research to explore the extent of pre-existing intake differences as well as other measured variables should be conducted to inform new methods to better engage low session completers.
4.2. Conclusion
Barriers for treatment providers to offer extended continuing care include: (a) lack of payor coverage for continuing care; (b) shortage of clinical time due to large caseloads; (c) difficulty maintaining adolescent attendance at community clinics over an extended period of time; and (d) distance and transportation issues, especially for youth from rural and small urban communities (Flynn & Brown, 2016; Godley & Godley, 2011). Although VRSA requires commitment of resources to cover costs for a project manager to recruit, train, and supervise volunteers, remaining support costs are minimal. Providers may also consider developing decision rules for transferring youth to VRSA in order to decrease large caseloads and create more time for counselors to respond to new referrals. AOD remission at 12 months was similar to the more intensive and expensive assertive continuing care (Godley et al., 2014), supporting the possibility that the present study may offer a cost-effective alternative for the field. Future research is needed to expand the range of youth who achieve high recovery support session completion rates, assess the effect of increasing recovery support call duration, and to test VRSA with outpatient youth.
Highlights.
Volunteer Recovery Support for Adolescents (VRSA) increases pro-recovery peers and activities.
VRSA improves substance use outcomes via pro-recovery peers and activities.
All outcomes improved significantly with incremental increases in VRSA dosage.
Student volunteers were effective in the delivery of VRSA.
VRSA succeeded in overcoming most barriers to sustaining recovery support for youth.
Acknowledgements
The authors acknowledge the student volunteers from Illinois State University nursing, psychology, and social work departments and University of Illinois at Urbana-Champaign social work department who worked diligently to contact youth and provide recovery support assistance. We also thank research assistants Bryan Dematteis, Karen Day, Tamara Sargus, and Cate Clifton for recruiting participants and collecting participant data; Stephanie Schade for recruiting, training, and supervising volunteers; and Lily Anderson for support and assistance throughout the study. We are indebted to Dr. Michael Dennis for consultation on statistical methods and analyses and to Kelli Wright for manuscript preparation.
Research reported in this publication was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under award number R01AA021118. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association (APA). (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. doi: 10.1176/appi.books.9780890423349. [DOI] [Google Scholar]
- Bassuk EL, Hanson J, Greene RN, Molly R, & Laudet A (2016). Peer-delivered recovery support services for addictions in the United States: A systematic review. Journal of Substance Abuse Treatment, 63, 1–9. doi: 10.1016/j.jsat.2016.01.003 [DOI] [PubMed] [Google Scholar]
- Best D, Honor S, Karpusheff J, Loudon L, Hall R, Groshkova T, & White W (2012). Well-being and recovery functioning among substance users engaged in post-treatment recovery support groups. Alcoholism Treatment Quarterly, 30, 397–406. doi: 10.1080/07347324.2012.718956 [DOI] [Google Scholar]
- Bollen KA (1984). Multiple indicators: Internal consistency or no necessary relationship? Quality and Quantity, 18(4), 377–385. doi: 10.1007/BF00227593 [DOI] [Google Scholar]
- Bosworth HB, Olsen MK, Gentry P, Orr M, Dudley T, McCant F, & Oddone EZ (2005). Nurse administered telephone intervention for blood pressure control: A patienttailored multifactorial intervention. Patient Education and Counseling, 57, 5–14. doi: 10.1016/j.pec.2004.03.011 [DOI] [PubMed] [Google Scholar]
- Boyd MR, Moneyham L, Murdaugh C, Phillips KD, Tavakoli A, Jackwon K,…Vyavaharkar M (2005). A peer-based substance abuse intervention for HIV+ rural women: A pilot study. Archives of Psychiatric Nursing, 19, 10–17.doi: 10.1016/j.apnu.2004.11.002 [DOI] [PubMed] [Google Scholar]
- Brown SA, Vik PW, & Creamer VA (1989). Characteristics of relapse following adolescent substance abuse treatment. Addictive Behaviors, 14(3), 291–300. doi: 10.1016/0306-4603(89)90060-9 [DOI] [PubMed] [Google Scholar]
- Buchan BJ, Dennis ML, Tims FM, & Diamond GS (2002). Cannabis use: Consistency and validity of self-report, on-site urine testing, and laboratory testing. Addiction, 97(suppl. 1), s98–s108. doi: 10.1046/j.1360-0443.97.s01.1.x [DOI] [PubMed] [Google Scholar]
- Buckheit KA, Moskal D, Spinola S, & Maistro SA (2018). Clinical course and relapse among adolescents presenting for treatment of substance use disorders: Recent findings. Current Addiction Reports, 5(2), 174–191. doi: 10.1007/s40429-018-0209-8 [DOI] [Google Scholar]
- Burleson JA, Kaminer Y, & Burke RH (2012). Twelve-month follow-up of aftercare for adolescents with alcohol use disorders. Journal of Substance Abuse Treatment, 42, 78–86. doi: 10.1016/j.jsat.2011.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacciola, Camilleri AC, Carise D, Rikoon SH, McKay JR, McLellan AT,…Schwarzlose JT (2008). Extending residential care through telephone counseling: Initial results from the Betty Ford Center Focused Continuing Care Protocol. Addictive Behaviors, 33, 1208–1216. doi: 10.1016/j.addbeh.2008.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charpentier PA (2003). Urn randomization program gRand v1.10. New Haven, CT: Yale University. [Google Scholar]
- Chi FW, Campbell CI, Sterling S, & Weisner C (2012). Twelve-step attendance trajectories over 7 years among adolescents entering substance use treatment in an integrated health plan. Addiction, 107(5), 933–942. doi: 10.1111/j.1360-0443.2011.03758.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloud W, & Granfield R (2008). Conceptualizing recovery capital: Expansion of a theoretical construct. Substance Use and Misuse, 43(12–13), 1971–1986. doi: 10.1080/10826080802289762 [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Maisto SA, Pollock NK, Martin C,S, Salloum IM, Lynch KG, & Clark DB (2003). Rapid relapse generally following treatment for substance use disorders among adolescents. Addictive Behaviors, 2, 381–386. doi: 10.1016/S0306-4603(01)00247-7 [DOI] [PubMed] [Google Scholar]
- Creemers HE, Dijkstra JK, Vollebergh WA, Ormel J, Verhulst FC, & Huizink AC (2010). Predicting life-time and regular cannabis use during adolescence; the roles of temperament and peer substance use: the TRAILS study. Addiction, 105(4), 699–708. doi: 10.1111/j.1360-0443.2009.02819.x [DOI] [PubMed] [Google Scholar]
- Del Boca FK, & Noll JA (2000). Truth or consequences: The validity of self-report data in health services research on addictions. Addiction, 95(suppl. 3), s347–s360. doi: 10.1080/09652140020004278 [DOI] [PubMed] [Google Scholar]
- Dembo R, Wothke W, Livingston S, & Schmeidler J (2002). The impact of a family empowerment intervention on juvenile offender heavy drinking: A latent growth model analysis. Substance Use and Misuse, 37(11), 1359–1390. doi: 10.1081/JA-120014082 [DOI] [PubMed] [Google Scholar]
- Dennis CL, Hodnett E, Gallop R & Chalmers B (2002). The effect of peer support on breast-feeding duration among primiparous women: A randomized controlled trial. Canadian Medical Association Journal, 166(1), 21–28. [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Godley SH, Diamond GS, Tims FM, Babor T, Donaldson J,…Funk RR (2004). The Cannabis Youth Treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment, 27, 197–213. doi: 10.1016/j.jsat.2003.09.005 [DOI] [PubMed] [Google Scholar]
- Dennis ML, Perl HI, Hueber RB, & McLellan AT (2000). Methodological challenges in study design and implementation: Twenty-five strategies for improving the design, implementation and analysis of health services research related to alcohol and other drugs. Addiction, 95(suppl. 3), s281–s308. doi: 10.1046/j.1360-0443.95.11s3.2.x [DOI] [PubMed] [Google Scholar]
- Dennis ML, & Scott CK (2007). Managing addiction as a chronic condition. Addiction Science and Clinical Practice, 4(1), 45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, & Scott CK (2012). Four-year outcomes from the Early Re-Intervention Experiment (ERI) with recovery management checkups (RMC). Drug and Alcohol Dependence, 121(1), 10–17. doi: 10.1016/j.drugalcdep.2011.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Titus JC, White M, Unsicker J, & Hodgkins D (2003). Global Appraisal of Individual Needs (GAIN): Administration guide for the GAIN and related measures. Bloomington, IL: Chestnut Health Systems. [Google Scholar]
- Drug Strategies. (2003). Treating teens: A guide to adolescent drug programs. Washington, DC: Author. [Google Scholar]
- DuPont RL, Compton WM, & McLellan AT (2015). Five-year recovery: A new standard for assessing effectiveness of substance use disorder treatment. Journal of Substance Abuse Treatment, 58, 1–5. doi: 10.1016/j.jsat.2015.06.024 [DOI] [PubMed] [Google Scholar]
- Finch AJ, & Karakos H (2014). Substance abuse recovery and schooling: The role of recovery high schools and collegiate recovery communities. Peabody Journal of Education, 89(2), 159–164. doi: 10.1080/0161956X.2014.895644 [DOI] [Google Scholar]
- Finch AJ, Tanner-Smith E, Hennessy E, & Moberg DP (2017). Recovery high schools: Effect of schools supporting recovery from substance use disorders. The American Journal of Drug and Alcohol Abuse, 44(2), 174–184. doi: 10.1080/00952990.2017.1354378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch AJ, & Wegman H (2012). Recovery high schools: Opportunities for support sand personal growth for students in recovery. Prevention Researcher, 19(5), 12–16. [Google Scholar]
- Fisher EA (2014). Recovery supports for young people: What do existing supports reveal about the recovery environment? Peabody Journal of Education, 89(2), 258–270. doi: 10.1080/0161956X.2014.897104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn PM, & Brown BS (2016). Matching treatment to rhetoric: A challenge to policy and programming. Journal of Substance Abuse Treatment, 64, 1–2. doi: 10.1016/j.jsat.2015.06.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- GAIN Coordinating Center. (2012). NORMS including alpha, mean, N, sd, ICC for Adolescents (12–17), Young Adults (18–25) and Adults (18+) by gender race and age using the CSAT 2011 SA Dataset (excluding ATM & CYT)[Electronic version]. Normal, IL: Chestnut Health Systems; Retrieved from http://gaincc.org/_data/files/Psychometrics_and_Publications/Resources/GAIN-I_NORMS.xls [Google Scholar]
- Garner BR, Barnes BN, & Godley SH (2009). Monitoring fidelity in the Adolescent Community Reinforcement Approach (A-CRA): The training process for A-CRA raters. Journal of Behavior Analysis in Health, Sports, Fitness, and Medicine, 2(1), 43–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner BR, Godley MD, Funk RR, Lee MT & Garnick DW (2010). The Washington Circle continuity of care performance measure: Predictive validity with adolescents discharged from residential treatment. Journal of Substance Abuse Treatment, 38(1), 3–11. doi: 10.1016/j.jsat.2009.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner BR, Godley MD, Passetti LL Funk RR, & White WL (2014). Recovery support for adolescent with substance use disorders: The impact of recovery support telephone calls provided by pre-professional volunteers. Journal of Substance Abuse and Alcoholism, 2(2), 1–11. PMCID: PMC4285388 [PMC free article] [PubMed] [Google Scholar]
- Garnick DW, Lee MT, Chalk M, Gastfriend D, Horgan CM, McCorry F,…Merrill EL (2002). Establishing the feasibility of performance measures for alcohol and other drugs. Journal of Substance Abuse Treatment, 23(4), 375–385. doi: 10.1016/S0740-5472(02)00303-3 [DOI] [PubMed] [Google Scholar]
- Godley MD, & Godley SH (2011). Assertive Continuing Care for adolescents In Kelly J, & White W (eds.), Addiction recovery management: Theory, science, and practice (pp. 103126). New York: Springer Science. [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk RR, & Passetti LL (2002). Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. Journal of Substance Abuse Treatment, 23, 21–32. doi: 10.1016/S07405472(02)00230-1 [DOI] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk RR, & Passetti LL (2007). The effectiveness of assertive continuing care on continuing care linkage, adherence, and abstinence following residential treatment for substance use disorders in adolescents. Addiction, 102, 81–93. doi: 10.1111/j.1360-0443.2006.01648.x [DOI] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL, & Petry N (2014). A randomized trial of Assertive Continuing Care and contingency management for adolescents with substance use disorders. Journal of Consulting and Clinical Psychology, 82, 40–51. doi: 10.1037/a0035264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godley SH, Dennis ML, Godley MD, & Funk RR (2004). Thirty-month relapse trajectory cluster groups among adolescents discharged from outpatient treatment. Addiction, 99 (Suppl. 2), 129–139. doi: 10.1111/j.1360-0443.2004.00860.x [DOI] [PubMed] [Google Scholar]
- Godley SH, Garner BR, Passetti LL, Funk RR, Dennis ML, & Godley MD (2010). Adolescent outpatient treatment and continuing care: Main findings from a randomized clinical trial. Drug and Alcohol Dependence, 110, 44–54. doi: 10.1016/j.drugalcdep.2010.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godley SH, Smith JE, Meyers RJ, & Godley MD (2009). Adolescent Community Reinforcement Approach (A-CRA) In Springer DW, & Rubin A (eds.), Substance abuse treatment for youth and adults (pp. 109–201). Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Godley SH, Smith JE, Meyers RJ, & Godley MD (2016). The Adolescent Community Reinforcement Approach: A clinical guide for treating substance use disorders. Normal, IL: Chestnut Health Systems. [Google Scholar]
- Grant TM, Ernst CC, Pagalilauan G, & Streissguth A (2003). Postprogram follow‐ up effects of paraprofessional intervention with high‐ risk women who abused alcohol and drugs during pregnancy. Journal of Community Psychology, 31(3), 211–222. doi: 10.1002/jcop.10048 [DOI] [Google Scholar]
- Grant TM, Ernst CC, Streissguth AP, Phipps P, & Gendler B (1996). When case management isn’t enough: A model of paraprofessional advocacy for drug- and alcoholabusing mothers. Journal of Case Management, 5, 3–11. [PubMed] [Google Scholar]
- Greist JH, Marks IM, Baer L, Kobak KA, Wenzel KW, Hirsch MJ,…Clary CM (2002). Behavior therapy for obsessive-compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. The Journal of Clinical Psychiatry, 63(2), 138–145. doi: 10.4088/JCP.v63n0209 [DOI] [PubMed] [Google Scholar]
- Hser YI, Grella CE, Hubbard RL, Hsieh SC, Fletcher BW, Brown BS, & Anglin MD (2001). An evaluation of drug treatments for adolescents in four U.S. cities. Archives of General Psychiatry, 58(7), 689–695. doi: 10.1001/archpsyc.58.7.689 [DOI] [PubMed] [Google Scholar]
- Humphreys K, Wing S, McCarty D, Chappel J, Gallant L, Haberle B,…Weiss R (2004). Self-help organizations for alcohol and drug problems: Toward evidence-based practice and policy. Journal of Substance Abuse Treatment, 26(3), 151–158. doi: 10.1016/S07405472(03)00212-5 [DOI] [PubMed] [Google Scholar]
- Jainchill N (2000). Substance dependency treatment for adolescents: Practice and research. Substance Use and Misuse, 35(12–14), 2031–2060. doi: 10.3109/10826080009148249 [DOI] [PubMed] [Google Scholar]
- Jason LA, Mericle AA, Polcin DL, & White WL (2013). The role of recovery residences in promoting long-term addiction recovery. American Journal of Community Psychology, 52, 406–411. doi: 10.1007/s10464-013-9602-6 [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, & Burke RH (2008). Efficacy of outpatient aftercare for adolescents with alcohol use disorders: A randomized controlled study. Journal of the American Academy of Child and Adolescent Psychiatry, 47(12), 1405–1412. doi: 10.1097/CHI.0b013e318189147c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminer Y, & Napolitano C (2004). Dial for therapy: Aftercare for adolescent substance use disorders. Journal of the American Academy of Adolescent Psychiatry, 43(9), 1171–1174. doi: 10.1097/01.chi.0000133260.98666.bf [DOI] [PubMed] [Google Scholar]
- Kelly JF, Brown SA, Abrantes A, Kahler CW, & Myers M (2008). Social recovery model: An 8-year investigation of adolescent 12-step group involvement following inpatient treatment. Alcoholism: Clinical and Experimental Research, 32(8), 1468–1478. doi: 10.1111/j.1530-0277.2008.00712.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Kaminer Y, Kalher CW, Hoeppner B, Yeterian J, Cristello JV, & Timko C (2017). A pilot randomized clinical trial testing integrated 12-step facilitation (iTSF) treatment for adolescent substance use disorder. Addiction, 112(12), 2155–2166. doi: 10.1111/add.13920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, & Myers MG (2007). Adolescents’ participation in Alcoholics Anonymous and Narcotics Anonymous: Review, implications, and future directions. Journal of Psychoactive Drugs, 39(3), 259–269. doi: 10.1080/02791072.2007.10400612 [DOI] [PubMed] [Google Scholar]
- Kelly JF, Myers MG, & Brown SA (2000). A multivariate process model of adolescent 12-step attendance and substance use outcome following inpatient treatment. Psychology of Addictive Behaviors, 14(4), 376–389. doi: 10.1037/0893-164X.14.4.376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Myers MG, & Brown SA (2005). The effects of age composition of 12-step groups on adolescent 12-step participation and substance use outcome. Journal of Child and Adolescent Substance Abuse, 15(1), 63–72. doi: 10.1300/J029v15n01_05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Yeterian JD, Cristello JV, Kaminer Y, Kahler CW, & Timko C (2016). Developing and testing twelve-step facilitation for adolescents with substance use disorder: Manual development and preliminary outcomes. Substance Abuse: Research and Treatment, 10, 55–64. doi: 10.4137/SART.S39635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H-S, & Oh J-A (2003). Adherence to diabetes control recommendations: Impact of nurse telephone calls. Journal of Advanced Nursing, 44, 256–261. doi: 10.1046/j.13652648.2003.02800.x [DOI] [PubMed] [Google Scholar]
- Koyanagi C, Alfano E, & Stein L (2008). Following the rules: A report on federal rules and state actions to cover community mental health services under Medicaid. Washington, DC: Bazelon Center for Mental Health Law. [Google Scholar]
- Lee MT, Pagano ME, Johnson BR, & Post SG (2016). Love and service in adolescent addiction recovery. Alcoholism Treatment Quarterly, 34(2), 197–222. doi: 10.1080/07347324.2016.1148513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh G, Hodgins DC, Milne R, & Gerrish R (1999). Volunteer assistance in the treatment of chronic alcoholism. American Journal of Drug and Alcohol Abuse, 25(3), 543–559.doi: 10.1081/ADA-100101878 [DOI] [PubMed] [Google Scholar]
- Leung RK, Toumbourou JW, & Hemphill SA (2014). The effect of peer influence and selection processes on adolescent alcohol use: A systematic review of longitudinal studies. Health Psychology Review, 8(4), 426–457. doi: 10.1080/17437199.2011.587961 [DOI] [PubMed] [Google Scholar]
- Lichtenstein E, Glasgow RE, Lando HA, Ossip-Klein DJ, & Boles SM (1996). Telephone counseling for smoking cessation: Rationales and meta-analytic review of evidence. Health Education Research, 11(2), 243–257. doi: 10.1093/her/11.2.243 [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Magill M, Morgenstern J, & Huebner R (2011). Mechanisms of behavior change in treatment for alcohol and other drug use disorders In McCrady BS, & Epstein EE (eds.), Addictions. New York: Oxford University Press. [Google Scholar]
- Longabaugh R, Wirtz PW, Zywiak WH, O’Malley SS (2010). Network support as a prognostic indicator of drinking outcomes: The COMBINE study. Journal of Studies on Alcohol and Drugs, 71(6), 837–846. doi: 10.15288/jsad.2010.71.837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Stewart AL, Brown BW, Bandura A,…Holman HR (1999). Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Medical Care, 37(1), 5–14. [DOI] [PubMed] [Google Scholar]
- Loveland D & Boyle M (2005). Manual for recovery coaching and personal recovery plan development. IL: Illinois Department of Human Services of Alcoholism and Substance Abuse. [Google Scholar]
- MacKinnon DP (2008). Introduction to statistical mediation analysis. New York: Taylor & Francis. [Google Scholar]
- McDermeit (Ives) M, Funk RR, & Dennis ML (1999). Data cleaning and replacement of missing values. Bloomington, IL: Chestnut Health Systems. [Google Scholar]
- McKay JR (2005). Is there a case for extended interventions for alcohol and drug use disorders? Addiction, 100(11), 1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x [DOI] [PubMed] [Google Scholar]
- McKay JR (2009). Continuing care research: What we have learned and where we are going. Journal of Substance Abuse Treatment, 36(2), 131–145. doi: 10.1016/j.jsat.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR (2017). Making recovery more rewarding: Difficult with possible unintended consequences, but successful examples are out there. Addiction, 112, 763–764. doi: 10.1111/add.13752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Ratichek S, Morrison R, Koppenhalver J, & Pettinato HM (2004). The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12-month outcomes. Journal of Consulting and Clinical Psychology, 72(6), 967–979. doi: 10.1037/0022-006X.72.6.967 [DOI] [PubMed] [Google Scholar]
- McKay JR, Van Horn D, Oslin DW, Ivey M, Drapkin ML, Coviello DM,…Lynch KG (2011). Extended telephone-based continuing care for alcohol dependence: 24-month outcomes and subgroup analyses. Addiction, 106, 1760–1769. doi: 10.1111/j.13600443.2011.03483.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moberg PD, & Finch AJ (2008). Recovery high schools: Feasibility of rigorous outcomes research Paper presented at the Joint Meeting on Adolescent Treatment Effectiveness (JMATE), Washington, DC. [Google Scholar]
- O’Rourke HP, & MacKinnon DP (2018). Reasons for testing mediation in the absence of an intervention effect: A research imperative in prevention and intervention research. Journal of Studies on Alcohol and Drugs, 79(2), 171–181. doi: 10.15288/jsad.2018.79.171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osgood-Hynes DJ, Greist JH, Marks IM, Baer L, Heneman SW, Wenzel KW,…Vitse HM (1998). Self-administered psychotherapy for depression using a telephoneaccessed computer system plus booklets: An open U.S.-U.K. study. The Journal of Clinical Psychiatry, 59(7), 358–365. doi: 10.4088/JCP.v59n0704 [DOI] [PubMed] [Google Scholar]
- Pagano ME, Friend KB, Tonigan JS, & Stout RL (2004). Helping other alcoholics in Alcoholics Anonymous and drinking outcomes: Findings from Project MATCH. Journal of Studies on Alcohol, 65(6), 766–773. PMCID: PMC3008319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal B (1998). Following up outpatients by telephone: Pilot study. British Medical Journal, 316, 1647 Retrieved from http://www.jstor.org/stable/25179362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passetti LL, Godley SH, & Godley MG (2012). Youth participation in mutual support groups: History, current knowledge, and areas for future research. Journal of Groups in Addiction and Recovery, 7, 253–278. doi: 10.1080/1556035X.2012.705707 [DOI] [Google Scholar]
- Passetti LL, Greene AR, White WL, & Godley MD (under review). The Volunteer Recovery Support for Adolescents (VRSA) experiment: Design and implementation. [Google Scholar]
- Passetti LL, & White WL (2008). Recovery support meetings for youths: Considerations when referring young people to 12-step and alternative groups. Journal of Groups in Addiction and Recovery, 2, 97–121. doi: 10.1080/15560350802081280 [DOI] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. doi: 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Rattermann MJ (2014). Measuring the impact of substance abuse on student academic achievement and academic growth. Advances in School Mental Health Promotion, 7(2), 123135. doi: 10.1080/1754730X.2014.888225 [DOI] [Google Scholar]
- Reif S, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS,…Delphin-Rittman ME (2014). Peer recovery support for individuals with substance use disorders: Assessing the evidence. Psychiatric Services, 65(7), 853–861. doi: 10.1176/appi.ps.201400047 [DOI] [PubMed] [Google Scholar]
- Ryan JP, Perron BE, Moore A, Victor BG, & Park K (2017). Timing matters: A randomized controlled trial of recovery coaches in foster care. Journal of Substance Abuse Treatment, 77, 178–184. doi: 10.1016/j.jsat.2017.02.006 [DOI] [PubMed] [Google Scholar]
- Ryan JP, Victor BG, Moore A, Mowbray O, & Perron BE (2016). Recovery coaches and the stability of reunification for substance abusing families in child welfare. Children and Youth Services Review, 70, 357–363. doi: 10.1016/j.childyouth.2016.10.002 [DOI] [Google Scholar]
- Scott CK, & Dennis ML (2011). Recovery management checkups with adult chronic substance users In Kelly J, & White W (eds.), Addiction recovery management: Theory, science and practice (pp. 87–102). New York: Springer Science. [Google Scholar]
- Shrout PE, & Bolger N (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7(4), 422–445. doi: 10.1037//1082989X.7.4.422 [DOI] [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Rutter C, & Wagner E (2000). Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. British Medical Journal, 320, 550–554. Retrieved from http://www.jstor.org/stable/25187284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JE, Lundy SL, & Gianini L (2007). Community Reinforcement Approach (CRA) and Adolescent Community Reinforcement Approach (A-CRA) therapist coding manual. Normal, IL: Chestnut Health Systems. [Google Scholar]
- Stahler GJ, Mazzella J, Mennis S, Chakravorty G, Rengert R, & Spiga R (2007). The effect of individual program, and neighborhood variables on continuity of treatment among dually diagnosed individuals. Drug and Alcohol Dependence, 87(1), 54–62. doi: 10.1016/j.drugalcdep.2006.07.010 [DOI] [PubMed] [Google Scholar]
- Stead LF, Perera R, & Lancaster T (2006) Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews, Issue 3, Art No CD002850. doi: 10.1002/14651858.CD002850.pub2 [DOI] [PubMed] [Google Scholar]
- Sterling S, Chi F, Campbell C, & Weisner C (2009). Three-year chemical dependency and mental health treatment outcomes among adolescents: The role of continuing care. Alcoholism: Clinical and Experimental Research, 33(8), 1417–1429. doi: 10.1111/j.15300277.2009.00972.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, & Del Boca FK (1994). Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol, 12(Supplement), 70–75. doi: 10.15288/jsas.1994.s12.70 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2003). Report to Congress on the nation’s substance abuse and mental health workforce issues. Washington, DC: Author. [Google Scholar]
- Tanaka JS (1993). Multifaceted conceptions of fit in structural equation modeling In Bollen KA & Long JS (eds.), Testing structural equation models (pp. 10–39). Newbury Park, CA: Sage. [Google Scholar]
- Tanner-Smith EE, Finch AJ, Hennessy EA, & Moberg DP (2018). Who attends recovery high schools after substance use treatment? A descriptive analysis of school aged youth Journal of Substance Abuse Treatment, 89, 20–27. doi: 10.1016/j.jsat.2018.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Thordarson DS, Spring T, Yeh AH, Corcoran KM, Eugster K, & Tisshaw C (2003). Telephone-administered cognitive behavior therapy for obsessive-compulsive disorder. Cognitive Behaviour Therapy, 32, 13–25. doi: 10.1080/16506070310003639 [DOI] [PubMed] [Google Scholar]
- Titus JC, Smith DC, Dennis ML, Ives M, Twanow L, & White MK (2012). Impact of a training and certification program on the quality of interviewer-collected self-report assessment data. Journal of Substance Abuse Treatment, 42(2), 201–212. doi: 10.1016/j.jsat.2011.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine P (2011). Peer-based recovery support services within a recovery community organization: The CCAR experience In Kelly J, & White WL (eds.), Addiction recovery management: Theory, science and practice (pp. 259–280). New York: Springer Science. [Google Scholar]
- Van Ryzin MJ, Fosco GM, & Dishion TJ (2012). Family and peer predictors of substance use from early adolescence to early adulthood: An 11-year prospective analysis. Addictive Behaviors, 37(12), 1314–1324. doi: 10.1016/j.addbeh.2012.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Korff M, Moore JE, Lorig K, Cherkin DC, Saunders K,…Comite F (1998). A randomized trial of a lay person-led self-management group intervention for back pain patients in primary care. Spine, 23(23), 2608–2615. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Turner CW, & Peterson TR (2001). Treatment outcomes for adolescent substance abuse at four- and seven-month assessments. Journal of Consulting and Clinical Psychology, 69(5), 802–813. doi: 10.1037/0022-006X.69.5.802 [DOI] [PubMed] [Google Scholar]
- White WL (2009). Peer-based addiction recovery support: History, theory, practice, and scientific evaluation. Chicago, IL: Great Lakes Addiction Technology Transfer Center and Philadelphia Department of Behavioral Health and Mental Retardation Services. [Google Scholar]
- White WL, Boyle M, & Loveland D (2002). Addiction as chronic disease: From rhetoric to clinical application. Alcoholism Treatment Quarterly, 3/4, 107–130. doi: 10.1300/J020v20n03_06 [DOI] [Google Scholar]
- White WL, & Evans AC (2014). The recovery agenda: The shared role of peers and professionals. Public Health Reviews, 35, 4. doi: 10.1007/BF03391703 [DOI] [Google Scholar]
- Winters KC, Tanner-Smith EE, Bresani E, & Meyers K (2014). Current advances in the treatment of adolescent drug use. Adolescent Health, Medicine, and Therapeutics, 5, 199210. doi: 10.2147/AHMT.S48053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Kaskutas LA, & Ammon LN (2004). In 12-step groups, helping helps the helper. Addiction, 99(8), 1015–1023. doi: 10.1111/j.1360-0443.2004.00782.x [DOI] [PubMed] [Google Scholar]
- Zornitsky J (2014). The adequacy of the behavioral health workforce to meet the need for services: Overview of key findings. Sudbury, MA: Advocates for Human Potential; Available at: http://www.ahpnet.com/AHPNet/media/AHPNetMediaLibrary/News/AHP-BH-Workforce-Paper-July-2014.pdf [Google Scholar]