Short abstract
Objectives
In this paper, we report the long-term outcomes of the endovascular treatment of femoropopliteal occlusive disease, focusing on the importance of calcification and runoff outflow on limb salvage and patency, and the factors associated with these outcomes at a single center.
Methods
This retrospective cohort study included consecutive patients with femoropopliteal occlusive who underwent femoropopliteal angioplasty at the Division of Vascular and Endovascular Surgery, Hospital do Servidor Público Estadual, São Paulo, Brazil, between January 2015 and July 2017.
Results
In total, 86 femoropopliteal occlusive angioplasties were performed in 86 patients, with an initial technical success rate of 95.34%. The mean ± standard deviation follow-up time was 880 ± 68.84 days. The analysis was performed at 720 days. Technical failure occurred in four patients, who were excluded from the analysis, leaving 82 patients and 82 femoropopliteal occlusive angioplasties. The estimated primary patency, secondary patency, limb salvage, and overall survival rates at 720 days were 60%, 96%, 90%, and 82.5%, respectively. In univariate and multivariate analyses, Cox regression showed worse primary patency rates in patients with one tibial vessel or isolated popliteal artery runoff (p = 0.005), calcification grade 4 (p = 0.019), calcification grade > 2 (p = 0.017), small vessel diameter < 4 mm (p = 0.03) or primary angioplasty without stenting (p = 0.021). A univariate analysis showed worse limb salvage in patients with one tibial vessel or isolated popliteal artery runoff (p = 0.039).
Conclusions
In this study, the main factors associated with worse outcomes in the endovascular treatment of femoropopliteal occlusive in terms of loss of primary patency were one tibial vessel or isolated popliteal artery runoff, calcification grade 4, or calcification grade > 2, small vessel diameter < 4 mm, and no stents use. One tibial vessel or isolated popliteal artery runoff was also associated with limb loss in a univariate Cox regression analysis.
Keywords: Arterial thrombosis, thrombosis, cardiology, peripheral vascular disease, hypertension, cardiology, antiplatelets, stroke treatment—medical, cardiology
Introduction
The endovascular treatment of femoropopliteal occlusive (FEPO) disease is now very well established in the global literature. Stenosis and occlusion of the superficial femoral and popliteal arteries may lead to incapacitating claudication and potentially critical limb ischemia, with limb loss and a severe impact on the patient’s quality of life and overall survival.1
In recent years, the treatment of FEPO has undergone substantial changes. Most treatment guidelines previously recommended endovascular interventions for single, short, and focal lesions, and open surgery for extensive FEPO. However, with recent improvements in the technology and in endovascular techniques, the guidelines now advocate endovascular treatment rather than open surgery as the primary intervention for focal or extensive disease.2,3 Many studies have evaluated the factors affecting the outcomes of endovascular treatment of FEPO, mainly Trans-Atlantic Inter-Society Consensus (TASC) classifications and the length of arterial lesions, but few have examined the influence of the arterial calcification index or tibial vessel runoff.
In this paper, we report the long-term outcomes of the endovascular treatment of FEPO, focusing on limb salvage and patency, and the factors associated with these outcomes, especially infrapopliteal vessel runoff and the calcification index of the femoropopliteal arteries.
Methods
This retrospective cohort study included consecutive patients with FEPO who underwent femoropopliteal angioplasty at the Division of Vascular and Endovascular Surgery, Hospital do Servidor Público Estadual, São Paulo, Brazil, between January 2015 and July 2017. The patient data were collected from the hospital’s database using Microsoft Access® software (Microsoft, Seattle, WA). The data obtained included the patients’ general and demographic characteristics and information recorded during outpatient follow-up visits. The patients’ hospital records were also consulted if necessary. The details of the surgical procedures were retrieved from the database and the patients’ medical records. In our department, all patients undergo cardiac evaluation by a specialist to assess their cardiac risk, based on the guidelines for perioperative cardiovascular evaluation and care in noncardiac surgery published by the American Heart Association.4
Patients with critical limb ischemia who underwent femoropopliteal angioplasty during the index period were eligible for the study. Patients who experienced an initial technical failure were excluded from the study. The arteriographic procedures performed were reevaluated in all patients to ensure the protocols were accurately reported. After the arteriograms were reviewed, the patients were classified according to established protocols, including the TASC II classification,5,6 the diameter and length of the catheter balloons and stents used, and other factors associated with endovascular treatment.
In our department, we prefer to use bare-metal stents for femoropopliteal angioplasty. Patients receive 300 mg of clopidogrel as the loading dose immediately after the procedure, and continue receiving 75 mg/day of clopidogrel for six months after surgery and aspirin (100 mg/day) for life. This dose of aspirin is administered to all patients unless there are contraindications. All patients in this study received some type of statin, either before or after surgery. The indications for angioplasty were based on the TASC II guidelines.5,6 In our department, we use primary nitinol stents for superficial femoral artery occlusion. For popliteal angioplasty, we use a primary balloon with selective stenting if the first two attempts at primary angioplasty have been unsuccessful due to dissection or recoil.
The arteriography procedures performed on the patients were reevaluated to confirm the accurate execution of our departmental protocols. The patients were then evaluated according to the TASC II classification, the length of the target lesion, the use of stenting, and other factors associated with endovascular treatment.5,6 The required information was obtained for each patient and independently assessed to determine the Bollinger classification of the femoropopliteal and infrapopliteal segments. The Bollinger Score consists of a vectorial score that considers the pattern of occlusion, stenosis, and plaques, and an additive score that describes the severity of the lesion. Four categories of occlusive lesions were defined, in descending order of severity: complete occlusion of the lumen, >50% stenosis, 25–50% stenosis, and plaques with <25% stenosis. The length of the occlusion was also considered when scoring the angiogram, using a previously described semiquantitative method for evaluating routine lower-limb arteriograms.7 We classified the patients according to whether runoff was via one or two tibial vessels or via an isolated popliteal segment, which was defined as a patent popliteal artery of at least 7 cm that had no communication with the tibioperoneal trunk or tibial vessels. We also stratified the patients into two groups according to runoff, based on the Bollinger Score.
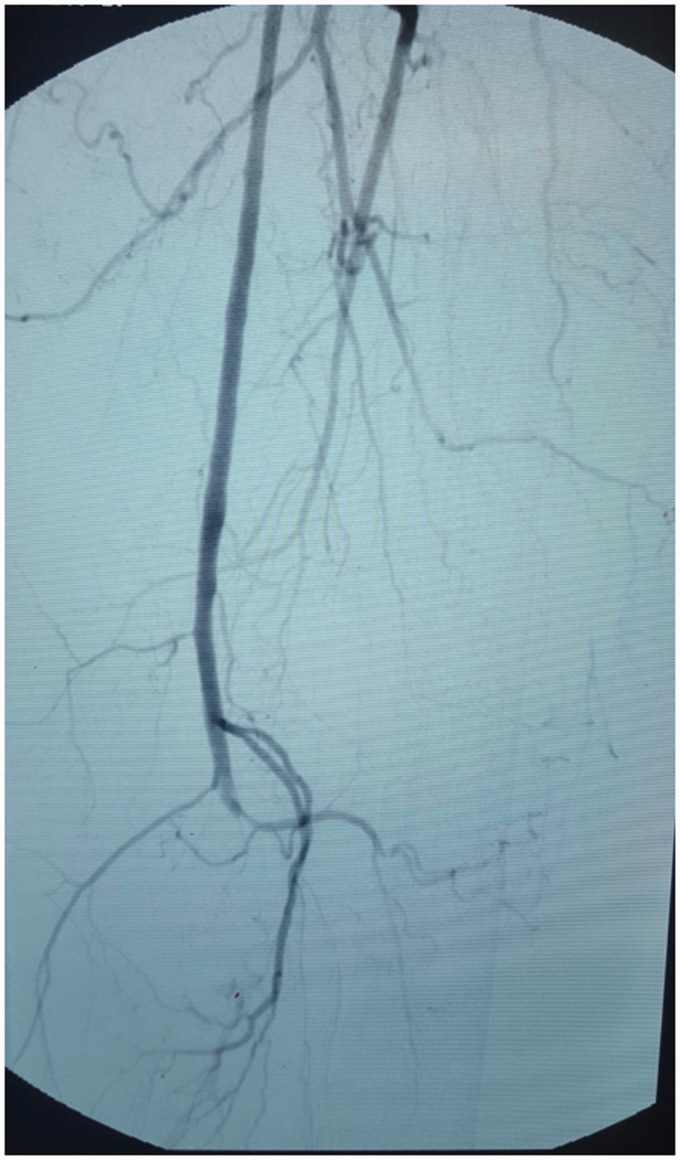
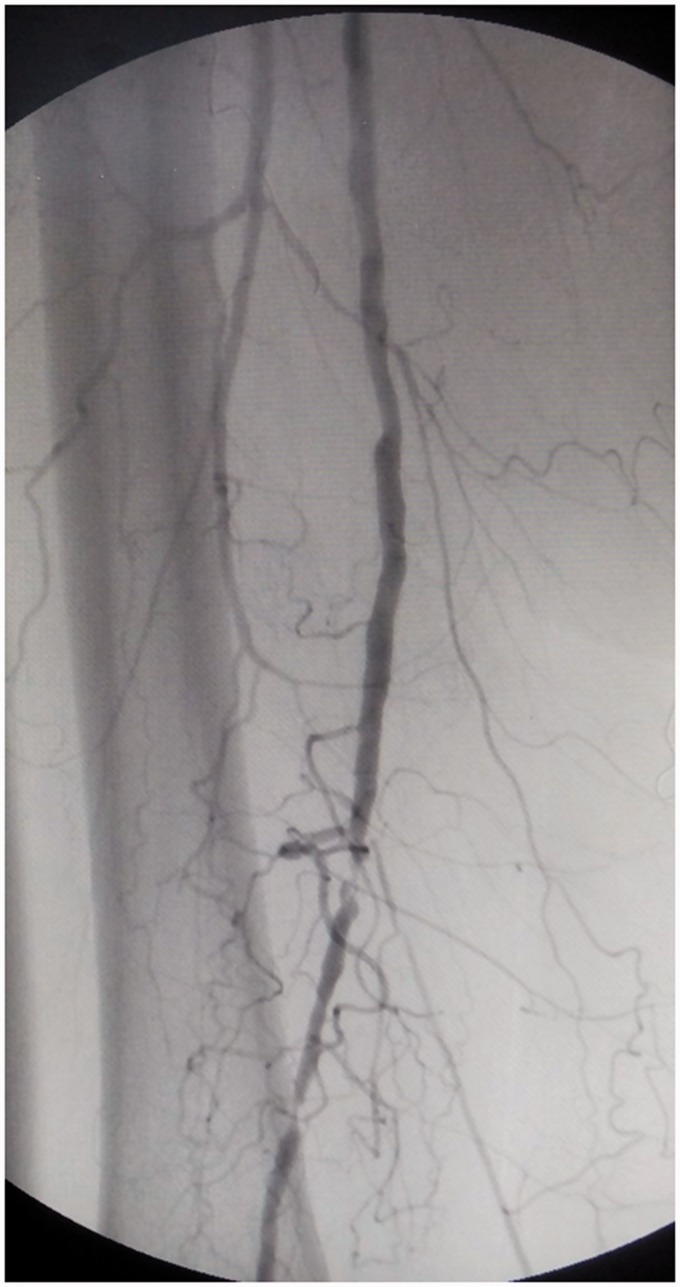
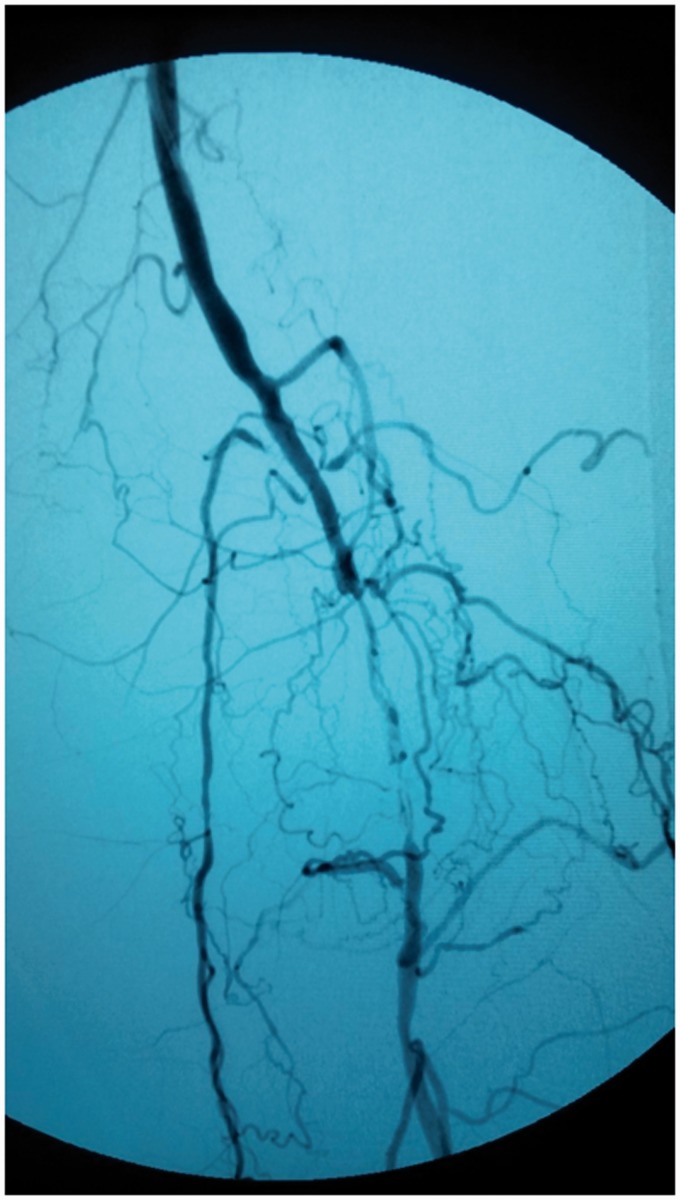
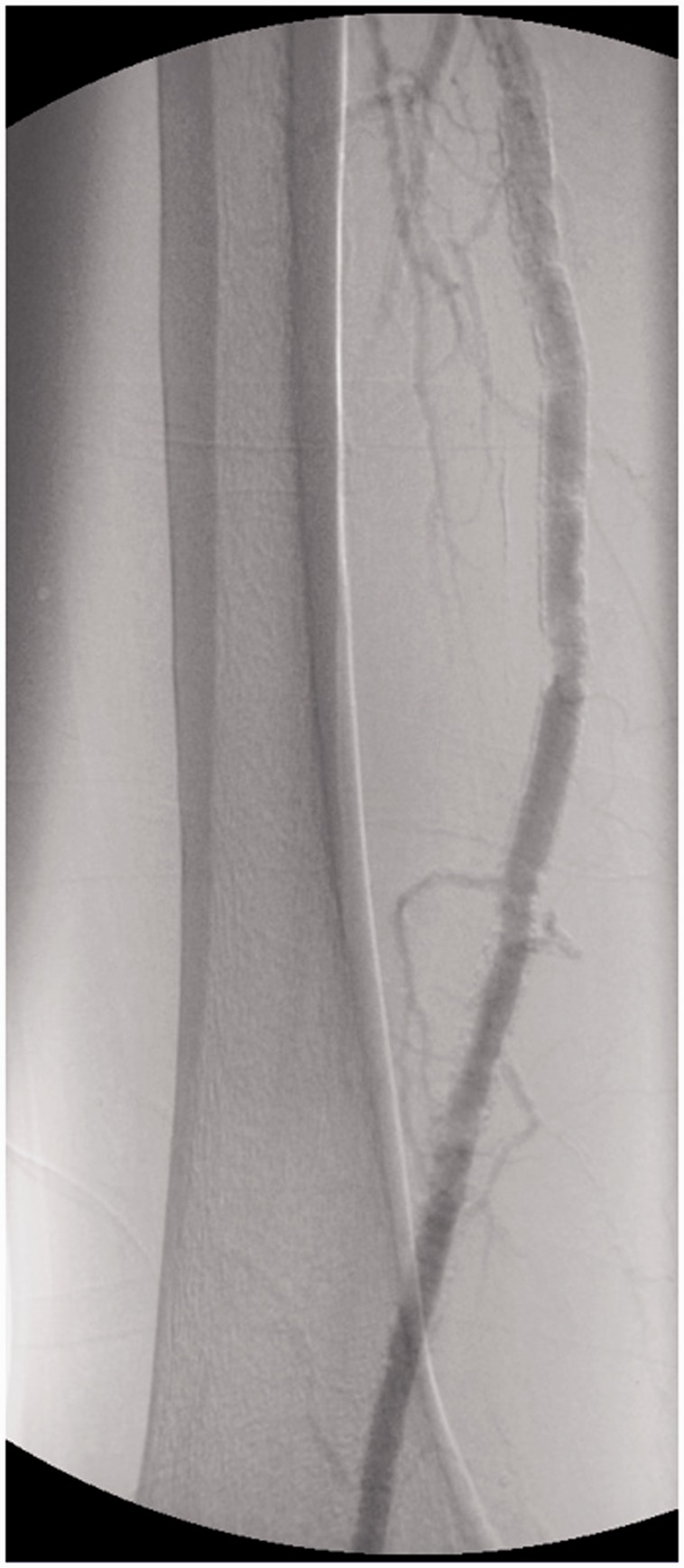
The grade of calcification of the femoropopliteal arteries was defined with the proposed peripheral arterial calcium-scoring system (PACSS).8 This score describes the intimal and medial vessel wall calcification at the target lesion site, assessed with high-intensity fluoroscopy and digital subtraction angiography in the anterioposterior projection. There are five grades: grade 0, no visible calcium at the target lesion site (Figure 1); grade 1, unilateral calcification of <5 cm (Figure 2); grade 2, unilateral calcification of >5 cm (Figure 3); grade 3, bilateral calcification of <5 cm (Figure 4); and grade 4, bilateral calcification of >5 cm (Figure 5). We termed grades of 2 and higher as intense calcification, and those less than grade 2 as low calcification.
Figure 1.
PACCS 0.
Figure 2.
PACCS 1.
Figure 3.
PACCS 2.
Figure 4.
PACCS 3.
Figure 5.
PACCS 4.
The initial technical success of the femoropopliteal angioplasty was defined as residual stenosis of ≤30%, no dissection after the procedure, and prompt restoration of the blood flow in the previously stenotic or occluded artery. Procedures such as debridement and minor amputations were also performed during hospitalization, if necessary.
All the patients were followed up with outpatient visits at the following timings after discharge: 15 days, 1 month, 3 months, 6 months, 12 months, and every 6 months thereafter. The following information was recorded at each visit: pulse palpation, ankle–brachial index (ABI), and symptoms. Whenever possible, we also examined the patients with arterial duplex ultrasonography at 1, 3, 6, and 12 months after surgery, and every 6 months thereafter. If any clinical or sonographic changes were observed, the case was discussed at a departmental meeting to assess whether reintervention was required. Occlusion of the treated artery was defined as no flow, segmental, or complete, based on duplex ultrasonography. Significant restenosis was defined as >50% based on angiographic estimation or ultrasound derived velocity parameters (peak systolic velocity ratio ≥ 2.0)
ABI with a decrease > 0.15 suggested an alteration in the patency of the angioplasty.
In this paper, we report the long-term outcomes of the endovascular treatment of FEPO disease, focusing on the importance of calcification and the runoff outflow on limb salvage and patency, and the factors associated with these outcomes at a single center.
All statistical analyses were performed with SPSS 15.0 for Windows® (SPSS Inc., Chicago, IL). Percentages of patients and descriptive statistics were calculated. The χ2 test and Student’s t-test were used to compare univariate data. Survival curves for estimated limb salvage, patency, and survival rates were constructed with the Kaplan–Meier method. Cox regression was used in the univariate and multivariable analyses. In all analyses, p values of <0.05 were considered statistically significant. The sample size calculation can often be based on the normal approximation N = (Zα + Zβ)2 × α2/δ2, where Zα = 1.96, Zβ = 0.84, α = 9 (percentual of population with calcification index in previous studies), δ = 2.94 (hazard ratio (HR) of PACCS 4 calcification in previous studies), N = 73.46 patients, to assume 5% of probability of type 1 error and 80% power. PACCS (Peripheral arterial calcium-scoring system). [AQ1]
Results
In total, 86 femoropopliteal angioplasties were performed in 86 patients, with an initial technical success rate of 95.34%. The mean ± standard deviation follow-up time was 880 ± 68.84 days. The analysis was performed at 720 days, with a follow-up rate of 96.8% in two years. Technical failure occurred in four patients, and involved the failure to progress a 0.035-inch guidewire through the lesion in all four patients. These patients were excluded from the analysis, leaving 82 patients and 82 femoropopliteal angioplasties.
The general characteristics of the patients are listed in Table 1 and the perioperative data in Table 2. The indication for revascularization was critical limb ischemia in all patients (100%) (Table 2). The perioperative mortality rate was 4.8% (Table 2). The endovascular procedures are summarized in Table 3. The left limb was treated in the majority (51.2%) of patients. The ipsilateral anterograde femoral artery was the commonest puncture site (93.9%). Isolated angioplasty of the femoropopliteal segment was performed in 32.6% of patients, and most patients underwent femoropopliteal and infrapopliteal angioplasty with 67.4%. Self-expandable nitinol stents were used in 65.5% of patients. None of the stents fractured during follow-up. When we classified the arteriographic lesions according to the TASC II system, type B lesions were the commonest (in 51.2% of patients). The predominant PACSS calcification score was grade 4 (47.5%). Twenty-six (31.7%) patients had two tibial vessel runoff, 52 patients (63.4%) had one tibial vessel runoff, and four patients (4.9%) had isolated popliteal artery outflow. The Bollinger classification was worse in patients with one tibial vessel or isolated popliteal segment runoff (mainly the distal anterior tibial artery (p = 0.029), proximal peroneal artery (p = 0.001), distal peroneal artery (p = 0.000), or proximal posterior tibial artery (p = 0.048)), than in patients with two infrapopliteal artery runoff (Table 4).
Table 1.
General patient characteristics.
| Variable | Value |
|---|---|
| Age, years | 74.5 ± 9.1 |
| Females | 47 (57.3%) |
| Concomitant diseases | |
| Hypertension | 74 (90.2%) |
| Diabetes mellitus | 67 (81.7%) |
| Heart disease | 25 (30.5%) |
| Chronic kidney failure (CKF) | 39 (40.6%) |
| Dialysis CKF | 17 (21%) |
| Tobacco use | 19 (23.2%) |
| Cilostazol use | 7 (8%) |
Data are expressed as means ± standard deviations or numbers (percentages) of patients.
Table 2.
Perioperative data.
| Variable | Value |
|---|---|
| Elevated cardiac risk | 7 (8.5%) |
| Infection | 20 (24.3%) |
| Perioperative mortality rate | 4 (4.8%) |
| Rutherford 4 | 9 (10.9%) |
| Rutherford 5 | 53 (64.6%) |
| Rutherford 6 | 20 (24.4%) |
| Indication for revascularization | |
| Pain at rest | 9 (10.9%) |
| Ulcer/gangrene | 73 (89.1%) |
Table 3.
Endovascular procedures.
| Variable | Value |
|---|---|
| Treated limb | |
| Right | 40 (48.8%) |
| Left | 42 (51.2%) |
| Artery puncture site | |
| Ipsilateral anterograde femoral artery | 77 (93.9%) |
| Contralateral retrograde femoral artery | 5 (6%) |
| TASC lesion type | |
| A | 20 (24.4%) |
| B | 42 (51.2%) |
| C | 8 (9.8%) |
| D | 12 (14.6%) |
| PACCS | |
| Grade 0 | 1 (1.2%) |
| Grade 1 | 7 (8.5%) |
| Grade 2 | 9 (10.9%) |
| Grade 3 | 26 (31.7%) |
| Grade 4 | 39 (47.5%) |
| Femoropopliteal Vessel diameter > 4 mm | 54 (66%) |
| Femoropopliteal Lesion length > 6 cm | 56 (69.4%) |
TASC: Trans-Atlantic Inter-Society Consensus.
Table 4.
Bollinger classification.
| Femoropopliteal and infrapopliteal arteries | Group 2 arteries runoff | Group 1 artery/isolated popliteal artery segment | P value |
|---|---|---|---|
| Proximal Supfema | 3.42 ± 3.28 | 4.48 ± 4.96 | .111 |
| Distal Supfemb | 6.23 ± 5.1 | 7.06 ± 5.68 | .132 |
| Proximal POPc | 7.54 ± 5.57 | 7.54 ± 5.56 | .724 |
| Distal POPd | 3.85 ± 4,15 | 4.21 ± 4,7 | .102 |
| Proximal PTe | 7.29 ± 6.14 | 11.85 ± 5.51 | .048 |
| Distal PTf | 6.26 ± 5.95 | 11.57 ± 5.57 | .649 |
| Proximal ATg | 8.31 ± 6.26 | 11.13 ± 5.94 | .073 |
| Distal ATh | 7.29 ± 6.26 | 11.69 ± 5.97 | .029 |
| Proximal PERi | 5.29 ± 5.77 | 7.37 ± 1.56 | .001 |
| Distal PERj | 3.67 ± 2.37 | 7.81 ± 1.90 | .000 |
aProximal superficial femoral.
bDistal superficial femoral.
cProximal popliteal.
dDistal popliteal.
eProximal posterior tibial.
fDistal posterior tibial.
gProximal anterior tibial.
hDistal anterior tibial.
iProximal peroneal.
jDistal peroneal.
The mean ABI was greater after surgery than before surgery (0.65 vs. 0.52, respectively; p = 0.01). Twenty patients (24.3%) required reintervention, with endovascular surgery in 14 patients (17%), femoropopliteal bypass surgery in four patients (4.87%), and femorotibial bypass in two patients (2.4%).
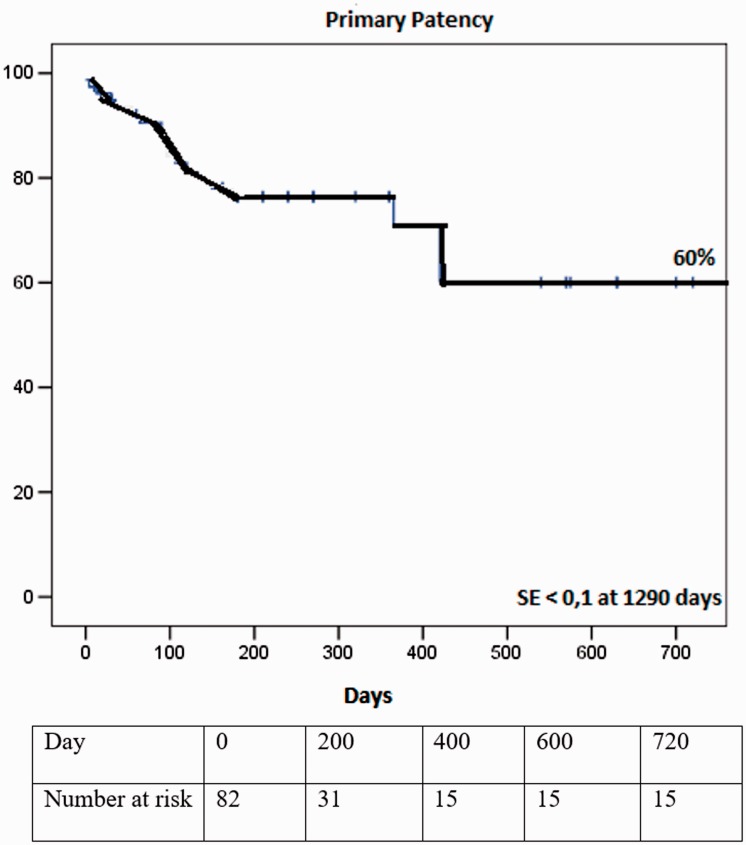
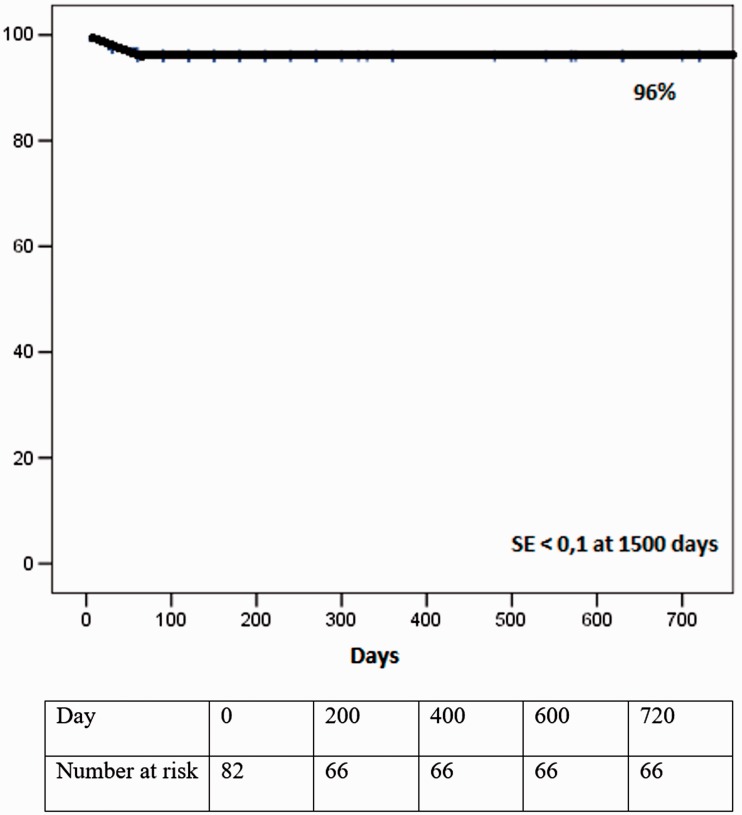
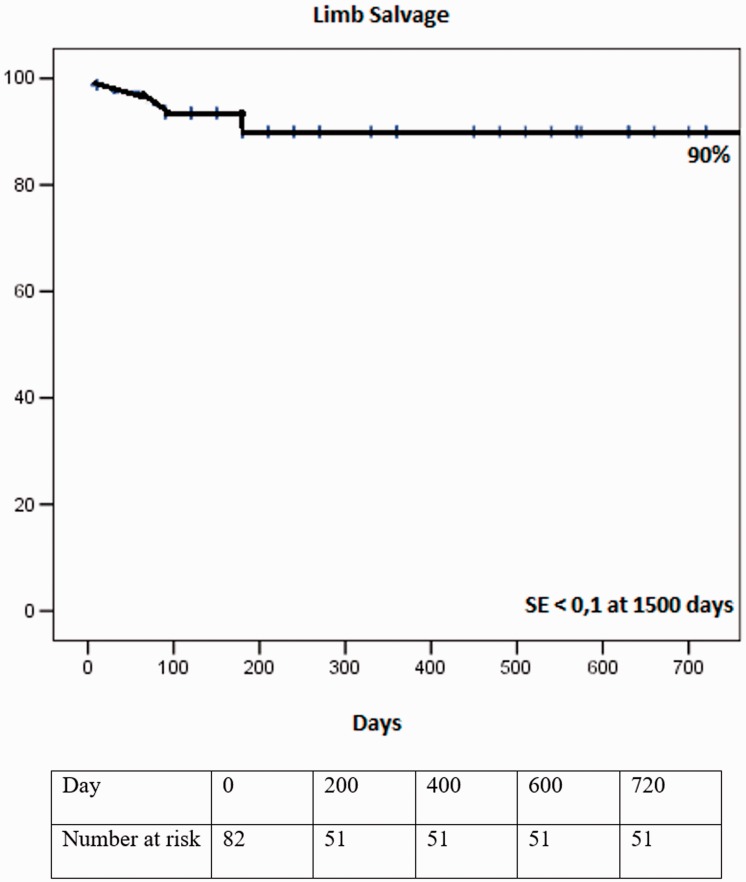
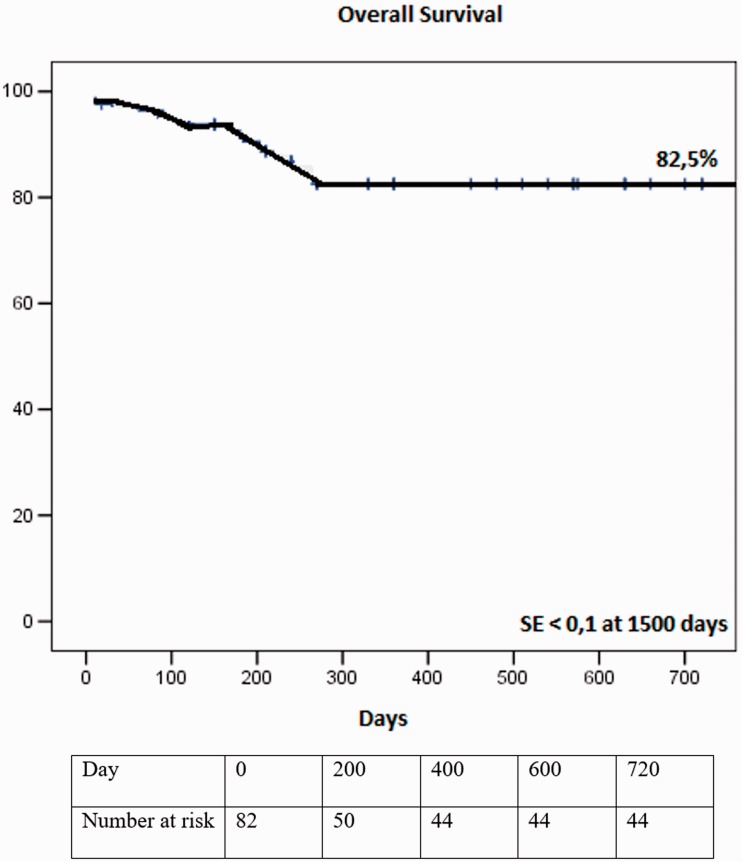
The estimated primary patency, secondary patency, limb salvage, and overall survival rates at 720 days were 60% (Figure 6), 96% (Figure 7), 90% (Figure 8), and 82.5% (Figure 9), respectively.
Figure 6.
Kaplan–Meier analysis of the primary patency rate. Primary patency rate at 720 days was 60% and the standard error was <10%.
Figure 7.
Kaplan–Meier analysis of the secondary patency rate. Secondary patency rate at 720 days was 96% and the standard error was <10%.
Figure 8.
Kaplan–Meier analysis of the limb salvage rate. Limb salvage rate at 720 days was 90% and the standard error was <10%.
Figure 9.
Kaplan–Meier analysis of overall survival. Survival rate at 720 days was 82.5% and the standard error was <10%.
In univariate and multivariate analyses, Cox regression (Table 5) showed worse primary patency rates in patients with one tibial vessel or isolated popliteal artery runoff (p = 0.005; HR = 7.69), calcification grade 4 (p = 0.019; HR = 5.48), grade calcification > 2 (p = 0.017; HR = 5.73), vessel diameter < 4 mm (p = 0.03; HR = 2.567 and no stenting (p = 0.0021; HR = 5.31).
Table 5.
Cox regression analysis of factors associated with primary patency.
| Variable |
Univariate analysis |
Multivariate analysis |
||||||
|---|---|---|---|---|---|---|---|---|
| B | HR | 95% CI | P | B | HR | 95% CI | P | |
| Diabetes | .423 | .793 | .415–5.609 | .524 | .597 | .875 | 0.415–4.233 | .671 |
| Active tobacco use | .244 | .406 | .377–4.297 | .696 | .244 | .390 | 0.820–4.681 | .642 |
| Chronic kidney disease | .542 | .890 | .188–1.051 | .345 | .542 | .890 | 0.538–4.567 | .831 |
| Runoffa | 1.412 | 7.698 | 1.221–10.501 | .005 | 1.885 | 7.906 | 1.411–14.294 | .005 |
| PACCS | 1.722 | 5.480 | 1.331–21.429 | .019 | 1.032 | 5.571 | 1.531–24.234 | .019 |
| TASC AB + CD | .631 | 1.331 | 0.542–1.543 | .172 | 0.711 | 0.915 | 0.339–12.230 | .249 |
| Calcification severityb | 3.953 | 5.731 | 1.324–2.111 | .017 | 4.243 | 5.314 | 1.334–5.433 | .017 |
| Use of stents (yes/no) | .596 | 5.313 | 1.093–3.012 | .021 | .596 | 5.314 | 1.212–3.555 | .021 |
| Lesion lengthc | .607 | 1.292 | 0.191–1.552 | .256 | .225 | 0.067 | 0.146–4.369 | .795 |
| Dialysis chronic kidney failure (CKF) | .978 | .332 | 0.049–2.257 | .260 | .226 | .0898 | 0.456–2.354 | .260 |
| Rutherford 4/5 + 6 | .676 | .716 | 0.483–7.990 | .345 | .676 | .891 | 0.483–7.890 | .345 |
| Cardiac failure | .930 | .906 | 0.522–12.304 | .249 | .567 | .930 | .522–11.365 | .622 |
| Cilostazol use | 1.475 | 2.214 | 0.006–2.006 | 2.194 | 1.475 | .111 | .006–2.345 | .137 |
| Vessel diameterd | 1.456 | 2.567 | 1.567–3.889 | 0.03 | 1.345 | 2.787 | 1.345–3.903 | 0.03 |
B: coefficient; HR: hazard ratio; CI: confidence interval; TASC: Trans-Atlantic Inter-Society Consensus.
aTwo tibial vessels vs. one tibial vessel + popliteal artery isolated segment.
bHigh severity score (>2) vs. moderate severity score (<2).
cLesion length > 6 cm vs. < 6 cm.
dVessel diameter < 4mm ≥ 4mm—popliteal/superficial femoral artery.
In a univariate analysis, Cox regression showed worse limb salvage rates in patients with one tibial vessel or isolated popliteal artery runoff (p = 0.039; HR = 4.69). A multivariate analysis showed no differences in the limb salvage rates among the covariates analyzed (Table 6).
Table 6.
Cox regression analysis of factors associated with limb loss (major amputation).
| Variable |
Univariate analysis |
Multivariate analysis |
||||||
|---|---|---|---|---|---|---|---|---|
| B | HR | 95% CI | P | B | HR | 95% CI | P | |
| Diabetes | .255 | .016 | .415–5.609 | .900 | .392 | .106 | 0.415–14.233 | .671 |
| Active tobacco use | 1.244 | .257 | .077–44.297 | .612 | 12.244 | .001 | 0.120–14.681 | .975 |
| Chronic kidney disease | 1.542 | .634 | .138–11.051 | .426 | 1.542 | .908 | 0.538–4.567 | .831 |
| Runoffa | 2.412 | 4.698 | 1.221–10.501 | .039 | 1.885 | 7.906 | 1.411–14.294 | .975 |
| PACCS | 2.722 | .480 | .331–21.429 | .959 | .032 | .002 | 1.531–24.234 | .616 |
| TASC AB + CD | .631 | 1.331 | 0.542–1.543 | .172 | 0.711 | 0.915 | 0.339–12.230 | .249 |
| Calcification severityb | 1.953 | .731 | 0.024–2.111 | .469 | 4.243 | 8.314 | 1.334–5.433 | .959 |
| Use of stents (yes/no) | .680 | 2.323 | 0.823–4.729 | .127 | .680 | 2.323 | 0.823–4.729 | .127 |
| Lesion lengthc | .225 | .067 | 0.146–4.336 | .795 | .680 | .056 | 0.256–4.759 | .987 |
| Arterial segment treatmentd | .464 | .912 | 0.105–3.760 | .611 | .464 | .256 | 0.105–3.760 | .611 |
| Dialysis CKF | .882 | .898 | 0.077–2.442 | .343 | .676 | .288 | 0.408–4.770 | .343 |
| Rutherford 4/5 + 6 | .180 | .062 | 0.291–4.927 | .803 | .722 | .106 | 0.291–4.927 | .803 |
| Cardiac failure | .697 | .906 | 0.577–6.986 | .273 | .456 | 2.987 | 0.467–5.325 | .273 |
| Cilostazol use | −1.577 | 1.265 | 0.017–2.472 | .213 | −1.567 | 1.266 | 0.198–3.456 | .213 |
TASC: Trans-Atlantic Inter-Society Consensus;.B: coefficient; HR: hazard ratio; CI: confidence interval.
aTwo tibial vessels vs. one tibial vessel + popliteal artery isolated segment.
bHigh severity score (>2) vs. moderate severity score (<2).
cLesion length > 6 cm vs. < 6 cm.
dFemoropopliteal segment angioplasty vs. femoropopliteal + infrapopliteal segment angioplasty.
Cox regression showed that none of the covariates analyzed was associated with reintervention, including calcification grade, runoff, diabetes, chronic renal failure, or TASC classification (Table 7).
Table 7.
Cox regression analysis of factors associated with reintervention.
| Variable |
Univariate analysis |
Multivariate analysis |
||||||
|---|---|---|---|---|---|---|---|---|
| B | HR | 95% CI | P | B | HR | 95% CI | P | |
| Diabetes | .028 | .002 | .242–4.363 | .847 | .028 | .001 | 0.415–4.233 | .970 |
| Chronic kidney disease | 1.542 | .634 | .138–11.051 | .680 | .056 | .908 | 0.538–4.567 | .831 |
| Runoffa | .415 | .141 | .174–13.501 | .707 | .885 | 7.906 | 1.411–14.294 | .975 |
| PACCS | 2.722 | .480 | .331–21.429 | .807 | .032 | .002 | 1.531–2.234 | .616 |
| TASC AB + CD | .631 | 1.331 | .542–1.543 | .559 | 0.711 | 0.915 | 0.339–2.230 | .249 |
| Calcification severityb | 1.953 | .731 | .024–2.111 | .807 | 4.243 | 8.314 | 0.334–2.433 | .959 |
| Dialysis CKF | .794 | .388 | .129–2.890 | .534 | .794 | .674 | 0.129–2.890 | .534 |
| Cilostazol use | −2.543 | .789 | .019–3.567 | .456 | .908 | .908 | 0.567–3.456 | .145 |
| Vessel diameterc | 1.456 | 2.345 | 1.345–3.567 | .456 | 1.456 | 2.135 | 0.234–3.456 | .567 |
B: coefficient; HR: hazard ratio; CI: confidence interval; TASC: Trans-Atlantic Inter-Society Consensus.
aTwo tibial vessels vs. one tibial vessel + popliteal artery isolated segment.
bHigh severity score (>2) vs moderate severity score (<2).
cVessel diameter < 4 mm ≥ 4 mm—popliteal/superficial femoral artery.
None of the covariates analyzed (calcification grade, runoff, TASC, diabetes, chronic renal failure) affected the overall survival rate or was associated with worse results (Table 8).
Table 8.
Cox regression analysis of factors associated with overall survival rate.
| Variable |
Univariate analysis |
Multivariate analysis |
||||||
|---|---|---|---|---|---|---|---|---|
| B | HR | 95% CI | P | B | HR | 95% CI | P | |
| Diabetes | .398 | .002 | .242–4.363 | .351 | .028 | .001 | 0.180–4.233 | .970 |
| Chronic kidney disease | .264 | .641 | .138–11.051 | .680 | .056 | .908 | 0.538–4.567 | .831 |
| Runoffa | .415 | .141 | .174–13.501 | .707 | .885 | 7.906 | 1.411–14.294 | .975 |
| PACCS | 2.722 | .480 | .331–21.429 | .807 | .032 | .002 | 1.531–2.234 | .616 |
| TASC AB + CD | .167 | 1.331 | 0.542–1.543 | .179 | .711 | 0.915 | 0.339–2.230 | .970 |
| Calcification severityb | .933 | .731 | .024–2.111 | .962 | 4.243 | 8.314 | .334–2.433 | .846 |
| Dialysis CKF | .445 | .898 | .488–3.345 | .965 | .987 | .788 | .245–5.322 | .786 |
| Rutherford 4/5 + 6 | .201 | .952 | .124–5.392 | .818 | .962 | .044 | .123–6.337 | .835 |
| Cardiac failure | .930 | .806 | .522–6.789 | .137 | .890 | .908 | .522–12.304 | .213 |
B: coefficient; HR: hazard ratio; CI: confidence interval; TASC: Trans-Atlantic Inter-Society Consensus.
aTwo tibial vessels vs. one tibial vessel + popliteal artery isolated segment.
bHigh severity score (>2) vs. moderate severity score (<2).
Five transfemoral amputations (6.1%) and two transtibial amputations (2.4%) were performed within 720 days of surgery.
Discussion
In a multivariate Cox regression analysis, Lida et al.9 identified female sex (HR 1.899; 95% confidence interval (CI) 1.318–2.737; p < 0.001), ABI < 0.6 (HR 1.921; 95% CI 1.348–2.736; p < 0.001), TASC II C/D lesion (HR 2.068; 95% CI 1.346–3.177; p = 0.0009), stent fracture (HR 1.937; 95% CI 1.203–3.118; p = 0.006), and no administration of cilostazol (HR 2.102; 95% CI 1.394–3.172; p < 0.001) as strong independent risk factors for restenosis. In our study, there were no cases of stent fracture and the factors associated with worse outcomes of the endovascular treatment of FEPO, in terms of loss of primary patency, were one tibial vessel or isolated popliteal artery runoff (p = 0.005), calcification grade 4 (p = 0.019), calcification grade > 2 (p = 0.017), femoropopliteal vessel diameter < 4 mm (p = 0.03) or primary ballooning without stenting (p = 0.021). Very few studies in the literature have evaluated whether these factors are predictive of worse outcomes. In terms of infrapopliteal artery outflow, as in the present study, Salapura et al.10 showed that one month after femoropopliteal angioplasty, 23% of patients with compromised runoff developed restenosis or reocclusion, compared with 11% of patients with good runoff (p = 0.03). After six months, the incidence of restenosis or reocclusion had increased in both groups at approximately equal rates, and the difference was no longer significant: 39/80 (49%) in the compromised runoff group vs. 36/83 (43%) in the good runoff group after 6 months (p = 0.49), and 42/73 (57%) vs. 38/73 (52%), respectively, after 12 months (p = 0.51). They concluded that compromised postprocedural infrapopliteal runoff predisposes patients to early restenosis or reocclusion after femoropopliteal angioplasty. The deterioration of infrapopliteal runoff in the year after femoropopliteal angioplasty was accompanied by worsening of the long-term femoropopliteal patency. These findings are consistent with our results, but it is important to note that we conducted our analysis at 720 days after surgery, a longer period than was used by Salapura et al.
In the present study, a Cox regression univariate analysis showed that infrapopliteal vessel or isolated popliteal arterial segment runoff was associated with worse limb salvage. The Bollinger classification indicated that outflow was worse in the patients with one infrapopliteal vessel or isolated popliteal arterial segment runoff than in those with two infrapopliteal vessel runoff, which explains the worse primary patency and limb salvage rates in the former group. These findings differ from those of a previous study undertaken in our department, in which de Athayde Soares et al.11 investigated whether the number of infrapopliteal arteries undergoing endovascular treatment was associated with the limb salvage rate in patients with critical limb ischemia. The conclusion drawn was that it is not necessary to treat the largest number of arteries possible in these patients. Instead, the artery most amenable to endovascular procedures should be treated to maximize the limb salvage and secondary patency rates. Although that study exclusively investigated infrapopliteal angioplasty, it is noteworthy that the Bollinger classification was similar in both groups (one infrapopliteal artery vs. two infrapopliteal arteries), demonstrating similar infrapopliteal outflow and runoff.
Another factor related to worse primary patency rates in the present study was the grade of calcification in the femoropopliteal arteries, defined and scored with PACSS. PACSS grade 4 and grade > 2 were factors related to worse primary patency. However, the reintervention rate was not influenced by these factors. In contrast, when Hiramori et al.12 investigated the relationship between the outcomes of endovascular therapy for femoropopliteal lesions and vessel diameter, the outcomes for small vessels were significantly worse in the stent group, whereas the outcomes regarding target lesion revascularization and major adverse limb events were similar. After adjustment, a small vessel (≤4 mm) remained an independent predictor of restenosis (HR 1.69; 95% CI 1.44–1.98; p < 0.0001). The authors concluded that the vessel diameter, especially in small vessels (≤4 mm), is associated with poor endovascular therapy outcomes. These findings are similar of those ones found in this present study, where femoropopliteal vessel diameter < 4 mm was associated to a worse primary patency. Another important study in which the results were similar to ours was performed by Okuno et al.13 who investigated whether the severity of lesion calcification, assessed with PACSS, was associated with the clinical outcomes after endovascular therapy for superficial femoral artery lesions. A multivariate analysis showed that PACSS grade 4 (HR 2.74, 95% CI 1.56–4.83; p < 0.001), diabetes (HR 1.52, 95% CI 1.06–2.20; p = 0.022), lesion length (HR 1.04, 95% CI 1.01–1.07; p = 0.006), and vessel diameter (HR 0.80, 85% CI 0.65–0.98; p = 0.038) were associated with the loss of primary patency. In our study, neither the TASC classification nor diabetes was related to the loss of patency, but PACSS grade 4 and severe calcification (grade > 2) were related to the loss of primary patency. Another factor related to a worse outcome for primary patency in this study was primary angioplasty with stenting. This finding is similar to that of Acin et al.14 who performed a meta-analysis of randomized controlled trials of the efficacy and safety of balloon angioplasty with optional stenting vs. routine stenting. Based on three studies, the target lesion revascularization at 12 months was better in the stent group than in the non-stent group (odds ratio [OR] 2.47; 95% CI 0.72–8.49; p = 0.065), but the difference was not statistically significant. However, the 12-month binary restenosis rate was significantly lower in the primary stenting group (OR 3.02; 95% CI 1.3–6.71; p < 0.001). They concluded that primary stenting, mainly for long lesions, may be the best option for first-line endovascular treatment of symptomatic disease in the femoropopliteal segment. The reintervention rate and overall survival were not affected by this factor.
The overall perioperative mortality rate in our study was 4.8%, which is satisfactory. The survival rate at 720 days was 82.5%. When we analyzed the factors associated with survival using Cox regression, no factor was related to a worse survival rate (diabetes mellitus, chronic kidney failure, tobacco use, PACSS, or runoff score). Our estimated survival rate and perioperative mortality rate are similar to those reported in other studies. For example, in a meta-analysis by Mwipatayi et al.15 in a total of 934 patients, 452 underwent balloon angioplasty (273 patients were male), and 482 underwent stenting (297 patients were male). The 30-day mortality rate was 4%, with a failure rate of 2%. Overall, complications were observed in 11% of patients. The one-year primary patency rates after balloon angioplasty ranged from 45% to 84.2% and at two years, ranged from 25% to 77.2%. Only one study published the four-year primary patency rate, which was 44%. In the stent implantation group, the one-year primary patency rate varied from 63% to 90%, and the two-year primary patency ranged from 46% to 87%. These data are quite similar to those in the present study, in which the estimated primary patency, secondary patency, limb salvage, and overall survival rates at 720 days were 60%, 96%, 90%, and 82.5%, respectively. Soga et al.16 reported primary patency rates of 79.8%, 66.7%, and 63.1%, and secondary patency of 90.4%, 87.3%, and 86.2% at one, three, and five years, respectively. In a multivariate analysis based on the Cox proportional HR, cilostazol administration (HR; 0.52; p < 0.0001), stent fracture (HR 1.6; p = 0.03), hemodialysis (HR 1.7; p = 0.01), and TASC II class C/D (HR 2.4; p < 0.0001) were independent predictors of primary patency. In our study, the TASC classification did not influence the results for primary patency or limb salvage.
In our department, we do not perform infrapopliteal angioplasty based on the angiosome concept. According to de Athayde Soares et al.,17 the estimates of limb salvage were similar in groups direct and indirect (87% and 92.3%, respectively, at 360 days; p ¼ 0.241). The analysis of secondary function did not differ between the two groups (65.1% and 58.3%, respectively, within 360 days; p = 0.92). Operative mortality was 8.3% in group 1 and 8% in group 2 (p = 0.60), and survival at 360 days was 78.5% in group 1 and 78.3% in group 2 (p = 0.86), which were not significantly different. They have found no evidence to support revascularization based on the concept of the angiosome in preference to revascularization of the artery that is most amenable to endovascular treatment for limb salvage and secondary function.
This study has some important limitations. In particular, this retrospective study involved the analysis of consecutive data collected from medical records and our institutional database. This limitation can be addressed with a prospective study. Further investigation must be performed to enable a direct comparison to be made among the patient groups regarding infrapopliteal artery runoff score after femoropopliteal endovascular treatment.
Conclusion
In this study, the main factors associated with worse outcomes of the endovascular treatment of FEPO in terms of loss of primary patency were one tibial vessel or isolated popliteal artery runoff, calcification grade 4, calcification grade > 2, femoropopliteal vessel diameter < 4 mm, or angioplasty without the use of stents. In a Cox Regression univariate analysis, one tibial vessel or isolated popliteal artery runoff was also related to limb loss. Based on the results of this study, we conclude that the endovascular treatment of FEPO is safe, with satisfactory and reproducible long-term outcomes, and has a low perioperative mortality rate.
Acknowledgements
None.
Contributorship
Writing: RAS
Data collection: MJM, FCBN, AMP, RDA
Revision: MFM, FCBN, RS, RDA, RAS
Critical analysis: MJM, FCBN, MFM, RAS, RS, APM, RDA
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
Ethical approval was not sought for the present study because it is a retrospective analysis, without further new interventions in patients. Recently published The National Code on Clinical Trials has declared that ethics approval is not necessary for real retrospective studies. Ethics approval to conduct this study was waived by Hospital do Servidor Público estadual de São Paulo ethics committee. CAE: 33835714.7.0000.5463
Guarantor
RAS
Informed consent
Written informed consent was obtained from all subjects before the study since it is a protocol that all patients read and accept once they are admitted in the Hospital for treatment. It is a written informed consent explaining about the possibility of treatment, and possibility of research studies, maintaining the confidentiality of the patient’s informations.
Trial registration
Not applicable.
References
- 1.Agarwal S, Sud K, Shishehbor MH. Nationwide trends of hospital admission and outcomes among critical limb ischemia patients: from 2003-2011. J Am Coll Cardiol 2016; 67: 1901–1913. [DOI] [PubMed] [Google Scholar]
- 2.Weinberg MD, Lau JF, Rosenfield K, et al. Part 2: medical and endovascular treatment. Nat Rev Cardiol 2011; 8: 429–441. [DOI] [PubMed] [Google Scholar]
- 3.Fakhry F, Spronk S, Van der Laan L. Endovascular revascularization and supervise exercise for peripheral artery disease and intermittent claudication: a randomized clinical trial. JAMA 2015; 314: 193644. [DOI] [PubMed] [Google Scholar]
- 4.Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for non-cardiac surgery. J Am Coll Cardiol 2007; 50: E159–E241. [DOI] [PubMed] [Google Scholar]
- 5.Norgren L, Hiatt W, Dormandy J, et al. on behalf of the TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg 2007; 33: S5–75. [DOI] [PubMed] [Google Scholar]
- 6.Norgren L, Hiatt WR, Dormandy JA, et al. on behalf of the TASC II Working Group. Inter-society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg 2007; 43: S1–67. [DOI] [PubMed] [Google Scholar]
- 7.Bollinger A, Breddin K, Hess H, et al. Semi-quantitative assessment of lower limb atherosclerosis from routine angiographic images. Atherosclerosis 1981; 38: 339–346. [DOI] [PubMed] [Google Scholar]
- 8.Joye J. The PATRIOT (peripheral approach to recanalization in occluded totals) study results. Am J Cardiol 2007; 100: S24. [Google Scholar]
- 9.Lida O, Soga Y, Hirano K, et al. Long-term outcomes and risk stratification of patency following nitinol stenting in the femoropopliteal segment: retrospective multicenter analysis. J Endovasc Ther 2011; 18: 753–761. [DOI] [PubMed] [Google Scholar]
- 10.Salapura V, Blinc A, Kozak M, et al. Infrapopliteal run-off and the outcome of femoropopliteal percutaneous angioplasty. Vasa 2010; 39: 159–168. [DOI] [PubMed] [Google Scholar]
- 11.De Athayde Soares R, Matielo MF, Brochado Neto FC, et al. Number of infrapopliteal arteries undergoing endovascular treatment is not associated with the limb salvage rate in patients with critical limb ischemia. J Vasc Surg 2016; 64: 1344–1350. [DOI] [PubMed] [Google Scholar]
- 12.Hiramori S, Soga Y, Lida O, et al. Relationship between clinical outcomes and vessel size in endovascular therapy for femoropopliteal lesions. J Vasc Surg 2017; 65: 1690–1697. [DOI] [PubMed] [Google Scholar]
- 13.Okuno S, Lida O, Shiraki T, et al. Impact of calcification on clinical outcomes after endovascular therapy for superficial femoral artery disease: assessment using the peripheral artery calcification scoring system. J Endovasc Ther 2016; 23: 731–737. [DOI] [PubMed] [Google Scholar]
- 14.Acin F, de Haro J, Bleda S, et al. Primary nitinol stenting in femoropopliteal occlusive disease: a meta-analysis of randomized controlled trials. J Endovasc Ther 2012; 19: 585–595. [DOI] [PubMed] [Google Scholar]
- 15.Mwipatayi BP, Hockings A, Hofmann M, et al. Ballon angioplasty compared with stenting for treatment of femoropopliteal occlusive disease: a meta-analysis. J Vasc Surg 2008; 47: 461–469. [DOI] [PubMed] [Google Scholar]
- 16.Soga Y, Lida O, Hirano K, et al. Mild-term clinical outcome and predictors of vessel patency after femoropopliteal stenting with self-expandable nitinol stent. J Vasc Surg 2010; 52: 608–615. [DOI] [PubMed] [Google Scholar]
- 17.De Athayde Soares R, Brochado Neto FC, Matielo MF, et al. Concept of angiosome does not affect limb salvage in infrapopliteal angioplasty. Ann Vasc Surg 2016; 32: 34–40. [DOI] [PubMed] [Google Scholar]