Abstract
Effective self-management is key to living well with Parkinson’s disease and one important aspect is disease-specific knowledge. This article explores how people with Parkinson’s disease in Sweden (1) acquire disease-specific knowledge and (2) use Parkinson’s disease–related healthcare. Data were collected through an online survey, which had 346 respondents (16–87 years old, median age: 68 years, 51% male; time since diagnosis: 0–31 years, median time: 7 years). Our results show that disease-specific knowledge is mainly found online, especially for women with Parkinson’s disease and people with Parkinson’s disease of working age, that most people with Parkinson’s disease in Sweden see their neurologist for 1 h or less per year and only one in two people with Parkinson’s disease has regular contact with other Parkinson’s disease–related healthcare professionals. We also find that people with Parkinson’s disease reporting higher levels of specific knowledge also are more likely to be satisfied with the amount of time they get with their neurologist, regardless of the amount of time.
Keywords: disease-specific knowledge, health information seeking, online survey, Parkinson, self-management
Introduction
Parkinson’s disease (PD) is a chronic neurodegenerative disease resulting in motor and non-motor symptoms causing significant burdens on individual patients and family members, as well as on healthcare and society.1 PD is extremely individual in nature and the range and fluctuations of symptoms often require complex medication regimens.2 The prevalence increases with age; median age of onset is 60 years although 10 per cent of people with Parkinson’s disease (PwP) are younger than 45.1,3 The number of PwP in Sweden is about 22,000.4 Worldwide, the number of PwP is predicted to double between the years 2005 and 2030.5
Healthcare has historically dealt with caring for acute injuries and illnesses where healthcare professionals were experts and patients passive recipients of care.6 Chronic conditions, however, require a very different model for healthcare, one that is based more on patients’ self-management and patient education.7,8
When in need of health-related or medical information, people with chronic diseases turn to different sources. In a study from the United States,9 the following percentages were reported: health professionals: 93 per cent, friend or family member: 60 per cent, books or similar: 56 per cent, Internet: 44 per cent, insurance provider: 38 per cent, and other sources: 6 per cent. Although many studies explore patients’ online information-seeking behaviour,10–13 we have not found any similar studies looking at other sources too for other countries, including Sweden, or for PwP.
Internet access has accelerated the search for information and resources, and patients with chronic diseases actively use the Internet to search disease-related information outside of healthcare. For example, in the United States, 51 per cent of adults living with chronic conditions go online to find health-related information.9 Another US study reports that about half of the population with chronic conditions would appreciate guidance when searching for health information online.14 A survey study from Japan15 demonstrated a lower use of Internet for health purposes; 23.4 per cent used a computer to acquire health information and 6 per cent used cell phones. We have not been able to find any similar study for a Swedish population but we know that Internet use in Sweden is high; in 2015, in total, 91 per cent of the population were online with slightly higher use (>95%) for ages 8–55 years.16 There are, however, differences in use of the Internet across the population; a different study shows that among those 65 and older, being male, high education, not living alone, not being cognitively impaired, being younger within the studied population and urban living correlated significantly with higher Internet use.17
Specifically in PD, effective self-management is crucial to successfully managing the disease and includes knowledge about the disease, medications and side effects, monitoring of symptoms, finding reliable sources of information and knowing when to take action.18–20 A large majority of PwP want to be active in health-related decisions and to have access to correct and relevant information.21–23 Online tools and services are frequently used among people with chronic diseases and have also been observed in PD.24–26 A US study shows that PwP often have access to and feel comfortable using computers, mobile phones and the Internet.27
The concept of health literacy has emerged as a way of describing, measuring and improving patient education. It was originally defined as ‘the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions’.28 With the increasing use of online services, eHealth literacy has been developed. There are a number of different definitions of eHealth literacy and one of the most frequently used is ‘the ability to seek, find, understand and appraise health information from electronic sources and apply knowledge gained to addressing or solving a health problem’.29 It seems that health and eHealth literacy in the context of PD are under-researched concepts. A search using search terms ‘health literacy’ OR ‘ehealth literacy’ AND ‘Parkinson*’ in several databases (PubMed, Web of Science and CINAHL) revealed only three studies, two of which were abstracts for conference posters and the third, a pilot study. One of the conference abstracts determined the readability of letters sent from clinics to PwP and states that there might be a discrepancy between PwP’s self-rated understanding and the actual readability.30 The other one reports a study of health literacy in 121 PwP using two brief assessments and concluded that low health literacy is common in the investigated population and is likely to be even more prevalent in a general population of PwP.31 The pilot study reports a prospective study of the functional health literacy of 44 men with PD and concludes that contrary to existing literature, PwP can be expected to preserve health literacy.32
Rather than to study the full concept of health literacy, we wanted to study one specific aspect, namely, acquisition of disease-specific knowledge. This has previously been studied in the context of chronic disease,9,15 but we have not been able to find any previous studies of this aspect specifically for PD. In this article, we use the term disease-specific knowledge as meaning all knowledge relating to PD, including but not limited to knowledge about symptoms, medication and other treatments, side effects, disease management and healthcare provision. This is relevant because raising the level of disease-specific knowledge among PwP has been found to increase health-related quality of life.33,34 A recent study in China assessed the knowledge of PD among PwP and noted a great need for improvement in key areas such as disease management and awareness of medication side effects.35
Since health professionals and healthcare are traditionally the main sources of validated disease-specific knowledge,36 it is worth looking at time that is available to provide this knowledge. In the United States, PwP have appointments with their neurologist three to four times a year;37 in Italy, one to three times,38 and in Sweden, once a year.4 This indicates a discrepancy between the availability and significance of healthcare as a source of disease-specific knowledge.
We investigated two research questions:
-
How do PwP in Sweden
Acquire disease-specific knowledge?
Use PD-specific healthcare?
Methods
Data were collected from PwP in Sweden by means of a survey developed in a step-wise process. The survey (in Swedish) was designed and distributed using the online tool Typeform.39
General information about the survey (purpose of the study, investigator, instructions for responding) was included and questions were kept short and focussed to reduce the risk of respondents abandoning the survey before completion.40 The survey questions are listed in Table 3 of Appendix 1 and include questions on background (gender, year of birth, place of living and education level), year of diagnosis and the importance, level and main source of disease-specific knowledge. There were also questions on how much time is spent in healthcare every year (neurologist and other healthcare professionals), as well as an assessment of time sufficiency. Response options were numerical, categorical or free text. When asked about their opinion, respondents were given a five-point Likert scale to choose from, where the middle option signified a neutral opinion.
The survey was first tested on a smaller pilot group with PD, four participants (50% women) with varying ages (49–67 years) and time since diagnosis (6–13 years), in a fully functional online form. Some minor text edits were made before distributing more broadly using the online tool. To maximise the number of responses, the web link to the survey was distributed to PwP in Sweden via email to patient organisations and patient groups, as well as social media and personal networks. No incentives were offered for responding. The survey was made available as soon as it was ready and data collection was terminated when the number of new responses tapered off. It was online for 4 weeks (7 March–4 April 2015), after which the results were downloaded and analysed.
Only respondents living in Sweden were included in the analysis and duplicate answers were excluded. Age and time since diagnosis were calculated from year of birth and year of diagnosis. Categorical and numerical variables were analysed with an interactive calculation tool41 using the χ2 test with statistical significance defined at p < .05.
This study is exempted from ethical approval by the regional ethical review board in Stockholm (according to decision 2015/1572-31/4).
Results
Background data
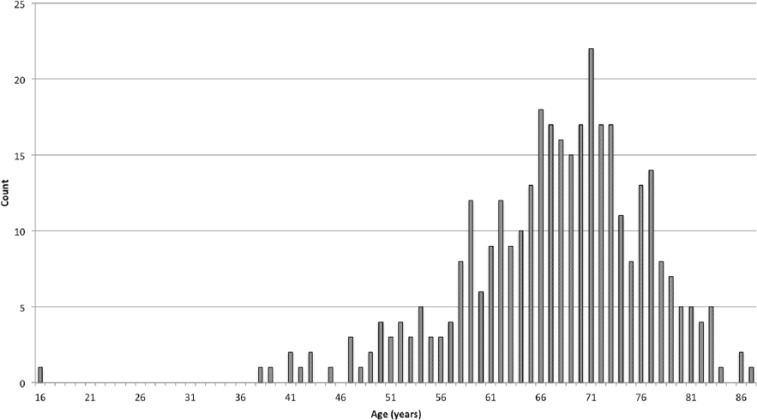
The survey had 346 valid responses, 11 of which did not give year of diagnosis, and 48 per cent of the unique visitors completed the survey. The age (Table 1 and Figure 1) and gender (Table 1 and Figure 2) distributions are consistent with what would be expected in a population with PD and representative for Swedish PwP compared to a study by Lökk et al.4 There is one 16-year-old respondent, who is unusually young for PD but rare forms have been reported with juvenile onset.42
Table 1.
Respondent characteristics.
| Respondent characteristics | Number of respondents | Interval | Median | |
|---|---|---|---|---|
| Age | 346 | 16–87 years | 68 years | 51% male |
| Time since diagnosis | 335 | 0–31 years | 7 years | |
| Education level | ||||
| Compulsory school (<9 years) | 74 (21%) | |||
| Upper secondary school (9–12 years) | 93 (27%) | |||
| University (>12 years) | 179 (52%) | |||
Figure 1.
Age distribution of the respondents.
Figure 2.
Time since diagnosis for the respondents.
Our respondents are relatively well educated (Table 1), 52 per cent have completed more than 12 years of education, which is more than the general population in Sweden, where 30–35 per cent of the population are reported to have studied for 12 years or more.43
Disease-specific knowledge
Results regarding self-reported importance, level and main source of disease-specific knowledge are presented in Table 2. In total, 91 per cent of the respondents considered knowledge about PD important (4 or 5 on the Likert scale for Importance of knowledge) and 55 per cent reported to have been able to acquire the knowledge they need (4 or 5 on the Likert scale for Level of knowledge). When asked which is their main source of disease-specific knowledge, 36 per cent responded that they had found the information themselves online, 29 per cent from patient organisations and similar, and 25 per cent from healthcare.
Table 2.
Importance, level and source of knowledge.
| Importance of knowledge | 1 | 2 | 3 | 4 | 5 | Total |
|---|---|---|---|---|---|---|
| How important is knowledge about your disease to you? (1 = unimportant, 5 = very important) | 0 | 9 | 22 | 53 | 262 | 346 |
| 0% | 3% | 6% | 15% | 76% | 100% | |
| Level of knowledge | 1 | 2 | 3 | 4 | 5 | Total |
| Have you been able to acquire the knowledge you need about your disease? (1 = not at all, 5 = absolutely) | 17 | 35 | 103 | 121 | 70 | 346 |
| 5% | 10% | 30% | 35% | 20% | 100% | |
| Source of knowledge | ||||||
| Which of these is your main source of knowledge about your disease? Pick one. | ||||||
| Information I have found myself online | 123 | 36% | ||||
| Information from patient organisations, etc. | 100 | 29% | ||||
| Information from healthcare | 87 | 25% | ||||
| Information from other patients | 18 | 5% | ||||
| Information from family, relatives and friends | 9 | 3% | ||||
| Other sources | 9 | 3% | ||||
| Total | 346 | 100% | ||||
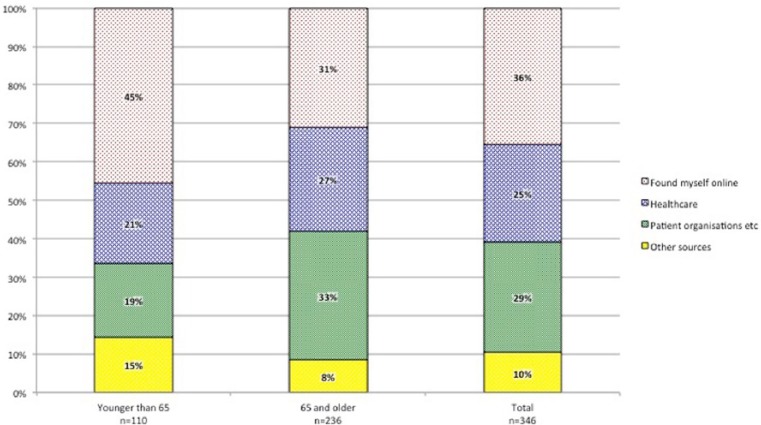
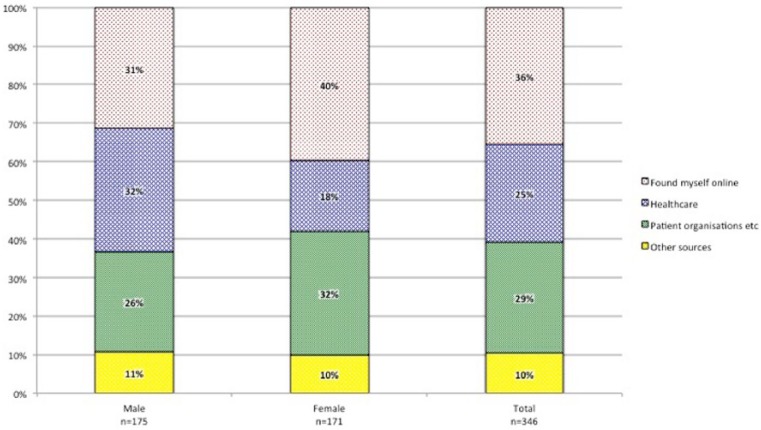
People with different education levels could be expected to report different levels and sources of knowledge; however, chi-square analyses of our respondents showed that neither level (p = .58) nor source of knowledge (p = .18) are significantly associated with education level. Furthermore, age, gender or time since diagnosis could be expected to influence level and source of knowledge. We have chosen to use the definition of ‘older adults’ from the Swedish National Board for Health and Welfare44 (65 years). For ‘time since diagnosis, we use the median value (7 years) for separating into two groups. We found that the self-reported level of knowledge is not significantly associated with age (p = .41), gender (p = .64) or time since diagnosis (p = .41). Similarly, the self-reported main source of knowledge is not significantly associated with time since diagnosis (p = .18). Analyses show, however, that significantly different main sources of knowledge are reported depending on age (χ2 = 13.6, df = 3, p = .003) and gender (χ2 = 9.62, df = 3, p = .022). Online information is the most important main source of disease-specific knowledge for PwP under 65 years of age, whereas the group 65 and older more often report patient organisations as their main source (Figure 3). It is worth noting that the 31 per cent of the group 65 and older who report Internet as their main source of disease-specific knowledge is still a relatively high number. Men and women also report significantly different sources (Figure 4); women more often find their information online. To enable the use of chi-square testing for analysing source of knowledge, the response options ‘other patients’, ‘family, relatives and friends’ and ‘other sources’ were merged.
Figure 3.
Self-reported primary source of disease-specific knowledge for different age groups.
Figure 4.
Self-reported primary source of disease-specific knowledge for different genders.
Time in healthcare
When it comes to time spent in healthcare (Table 4 of Appendix 1), 35 per cent visited their neurologist once and 38 per cent twice during 2014. Three visits were made by 10 per cent of the respondents and 9 per cent had four visits or more. This means that 8 per cent (n = 29) of our respondents did not see a neurologist at all during the year. As for the length of visits, 14 per cent met with their neurologist for up to 15 min, 48 per cent between 15 and 30 min, 23 per cent for 30–45 min and 14 per cent for an hour or more per visit. We calculated the total yearly time with the neurologist from number of visits and time per visit. In total, 60 per cent (n = 206) saw their neurologist for up to an hour during the year (Figure 5; Table 4 of Appendix 1).
Figure 5.
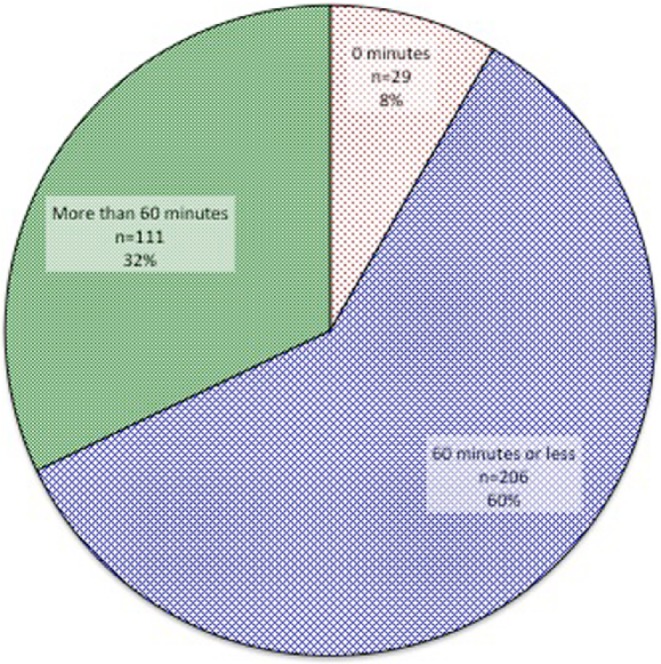
Total time with neurologist in 2014.
When asked if they considered the time they have with their neurologist to be sufficient, 35 per cent of the respondents said no (1 or 2 on the Likert scale), 43 per cent said yes (4 or 5 on the Likert scale) and 22 per cent were neutral (3 on the Likert scale) (Table 4 of Appendix 1). As expected, there is a significant association between spending more time per year with your neurologist and being satisfied with the amount of time spent (χ2 = 16.8, df= 4, p = .002).
On the question about regular contact with other healthcare professionals, 47 per cent (n = 161) reported that they had met with a nurse, speech therapist, physiotherapist or similar during 2014 (Table 5 of Appendix 1). About one-third of the people with no time with their neurologist (9 out of 29) reported that they had regular contact with other healthcare professionals, for example, nurse, physiotherapist or speech therapist. Of these, one person had 10–20 h and the remaining eight had up to 5 h during the year.
One could expect that people who spend more time with their neurologist per year would report higher levels of disease-specific knowledge and also more often report healthcare as their main source of knowledge. Chi-square analyses show, however, that yearly time with neurologist is not significantly associated with level (p = .43) or main source of knowledge (p = .15).
A person’s gender, level of education or age could be expected to have an effect on their expectations on and satisfaction with healthcare. Furthermore, that the time since diagnosis might influence how much contact with the neurologist is perceived as needed. Analyses of our data show, however, that PwP’s satisfaction with the time they get with their neurologist is not significantly associated with age (p = .17), gender (p = .63), time since diagnosis (p = .44) or education level (p = .83).
Furthermore, we also found a significant association between self-reported level of knowledge and satisfaction with the time with the neurologist every year (χ2 = 30.1, df = 4, p < .001). This means that PwP reporting a higher level of knowledge were more likely to be satisfied with the time they had with their neurologist, regardless of how short or long that time was.
Discussion
The aim of this study was to explore how PwP in Sweden acquire disease-specific knowledge and to investigate the use of PD-related healthcare in Sweden. The results from our survey indicate that Swedish PwP mainly acquire their disease-specific knowledge online and that the Internet is an even more important source of information for women with PD, as well as PwP under 65 years of age. We also see that most PwP in Sweden see their neurologist for 1 h or less per year. In the following sections, the results and methods will be discussed in more detail.
Discussion of results
It is hardly a surprising finding that the Internet is an important source of knowledge for PwP considering the increasing online presence of patients across all diseases. Age and gender seem to have a significant influence on the main source of knowledge, influence that appears independent from time since diagnosis, education level or time spent with neurologist per year. The fact that our data show that women to a higher degree find their information online could be seen as contradicting earlier research that suggests that men in Sweden are more online than women17 but could also be seen as an indication that even though women are less online than men, they mainly find their disease-specific knowledge online.
Should the fact that people find their disease-specific information online be perceived as a problem? Not necessarily, because although it is important to acknowledge that it can be difficult finding correct and relevant information online, Internet does enable patients to more effectively manage their health and healthcare.45 ‘Internet-informed’ patients influence the patient–provider relationship and contribute to making healthcare more patient-centered while healthcare professionals can overestimate the risks of online health information.46,47 Results from a study among American patients with chronic conditions showed that a majority, 94 per cent, reported that they had not been harmed by health information they found online.9 It is, however, important to note that Internet use can be an issue for PwP. Excessive use of Internet may be a sign of impulse control dysfunction, a known side effects of PD medications.48,49
The effects of PD can also have an influence on our results. With the progression of the disease, for example, hand function may be affected, presenting as impaired fine motor skills and/or severe tremor. This could result in reduced ability to use keyboard, computer mouse or touch screens, hence making it more difficult to respond to online surveys.
The quality and accessibility of the information provided online can potentially be an issue. Indeed, the quality of information found can be difficult to assess for PwP. Misinformation can be both deliberate with the purpose to promote a specific product or cause and unintended mistakes. Both of these can be problematic and should be explored further. When it comes to readability, a study of PD information websites in English aimed towards PwP showed that the majority of the sites studied did not comply with readability guidelines.50 Whether or not this is the case for Swedish websites with information on PD is not known, and based on the survey results, we cannot know which sites the respondents use to gather information, nor if our respondents defined ‘the knowledge you need’ in the same way or regarded the information they found as being credible, reliable and helpful. In accordance with existing research, we also cannot know in what way the information given is perceived and understood.8
Would it not be better if healthcare took a larger responsibility in educating patients? There may of course be a role here for healthcare professionals to involve PwP more in their treatment and care, and according to a Dutch study, PwP expect healthcare to provide relevant information, tailored to the individual’s needs.22 However, as is reflected in a different study, advances in medicine and time constraints in healthcare make it hard for healthcare professionals to keep up with new knowledge and patients’ needs and expectations, which often leaves patients feeling frustrated with the information provided.45 The study even suggests that patients who are more Internet-savvy than their providers often feel better able to find the health-related information they need by themselves online.45 As we can see from our results, most PwP have 60 min or less with healthcare annually, leaving little room for continuous information provision or patients’ questions. In combination with the high Internet use in Sweden, even among the older population, it could be assumed that Swedish PwP might sometimes be able to find the information they need more easily than their healthcare providers.
It is also important to note that there is a difference between information and knowledge. Healthcare professionals might feel confident that they provide the right information at the right time but, for time constraints or other reasons, they are not able to ensure that the information is properly received and transformed into knowledge by the individual. The perception of what kind of information is relevant at different times and stages of the disease might also vary between healthcare and PwP, and even between PwPs. This makes it, of course, very difficult for healthcare professionals to provide information relevant to each PwP at every occasion. Furthermore, we would argue that different sources might provide different types of information. It might be feasible to think that certain types of information would be best if given by healthcare, whereas other kinds might be best found elsewhere, a topic that would need further exploration in the future.
We also see the fact that PwP find their information online as part of the on-going shift from patients being passive recipients of care to active participants who have the possibility to be experts in managing their own disease and situation.23 Considering the complexity of the disease and treatments, we believe it is unreasonable to expect the limited time PwP have in healthcare to be sufficient to adequately address all the relevant issues. We therefore propose that other avenues for supporting the acquisition of disease-specific knowledge for PwP are explored. Our data show that also fellow patients, in the form of patient organisations and similar, are important sources of disease-specific knowledge. We propose to combine the power of the Internet with the force of patients to complement the current information provision by healthcare. By utilising the networking powers of online communities and online learning, we believe that some of the pressure on healthcare can be alleviated. This is developed further in ‘Future work’ below.
Discussion of methods
Choosing an online survey as a data collection method has its own advantages and limitations. Although online surveys are a fast and efficient way to collect data,40 they bias the results in favour of people who are already active online and probably use Internet as a knowledge source. Our respondents are more educated than the Swedish population in general and a higher level of education has been shown to significantly predict the use of Internet for health purposes.45 This means that our results might overestimate the proportion of people who mainly find their information online. However, since Sweden, in general, has a very high use of Internet, the overestimate is likely to be minor.
Respondents were asked to self-assess their level of disease-specific knowledge and relate it to the knowledge they considered themselves needing. They were also asked to self-report the frequency and length of healthcare visits. Relying on self-assessments and recall gives rise to uncertainties in the responses.
Despite the weaknesses described above, our results contribute to new knowledge in an under-explored research field and they point towards a development where the importance in online sources for patients’ knowledge acquisition increases.
Our survey collected responses from about 1.5 per cent of all PwP in Sweden and when comparing with a study reporting age and gender distribution in that population,4 our population seems reasonably representative, with some lack of responses in the higher age groups.
Future work
As far as the authors know, this is the first study exploring acquisition of disease-specific knowledge by PwP. Our questions were not detailed but rather general. Future research should focus on exploring the satisfaction of PwP with online information, investigating whether different sources provide different kind of information and individualising the knowledge type, form and delivery to patient needs and preferences. Exploring ways to objectively assess PwP disease-specific knowledge is another future research focus, as well as looking at potential methods for ensuring the quality of online health information, to avoid inappropriate guidelines and recommendations. In a subsequent next step, the results from the proposed work, an online service for implementing these ideas could be developed.
Conclusion
PwP in Sweden mainly find their disease-specific information online, especially so for women and people in working age. At the same time, healthcare has a very limited possibility to provide disease-specific information since the majority of PwP see their neurologist for 1 h or less per year. Moreover, only 1 out of 2 has contact with other PD-specific healthcare professionals. Given the overburdened healthcare system, it would be worth exploring other ways of guiding patients to relevant and accurate health information, such as education programmes and peer support networks delivered by patient organisations or other entities independently from healthcare. The timing, content and delivery mode of PD-specific knowledge need to be addressed in future research.
Acknowledgments
All authors have actively contributed to the work reported in this article: all authors took part in designing the survey, as well as writing, revising and approving the article.
Appendix 1
Table 3.
Survey questions and response options.
| Question | Reply options |
|---|---|
| Gender? | M/F |
| Year of birth? | Numeric |
| County council of residence? | Dropdown of all Swedish county councils |
| Highest completed education? | Compulsory school (<9 years) |
| Upper secondary school (9–12 years) | |
| University (>12 years) | |
| Year of diagnosis? | Numeric |
| How important is knowledge about your disease to you? | Scale from 1 to 5 where 1 = unimportant, 5 = very important |
| Which of these is your main source of knowledge about your disease? Pick one. | Healthcare |
| Patient organisations and similar | |
| Found myself online | |
| Other patients | |
| Family, relatives and friends | |
| Other sources | |
| Have you been able to acquire the knowledge you need about your disease? | Scale from 1 to 5 where 1 = not at all, 5 = absolutely |
| How many times did you see your neurologist during 2014? | None |
| Once | |
| Twice | |
| Three times | |
| Four times or more | |
| I do not have a neurologist | |
| Non-mandatory comment about visits to the neurologist | Free text |
| How long is each visit on average? Pick the time closest to the actual time. | About 15 min |
| About 30 min | |
| About 45 min | |
| An hour or more | |
| Do you also have regular contacts with other healthcare professionals, for example, nurse, speech therapist, physical therapist, social worker? | Yes |
| No | |
| I do not know | |
| Total time spent in healthcare for PD during 2014 (neurologist visits excluded) | Up to 5 h |
| Between 5 and 10 h | |
| Between 10 and 20 h | |
| More than 20 h | |
| Non-mandatory comment about your other healthcare contacts | Free text |
| Do you think your time with the neurologist is sufficient? | Scale from 1 to 5 where 1 = not at all, 5 = absolutely |
| Non-mandatory comment about the time spent with the neurologist | Free text |
Table 4.
Time with neurologist.
| Number of visits | |||||||
| How many times did you see your neurologist during 2014? | None | Once | Twice | Three times | Four times or more | I don’t have a neurologist | Total |
| 25 | 120 | 133 | 34 | 30 | 4 | 346 | |
| 7% | 35% | 38% | 10% | 9% | 1% | 100% | |
| Length per visit | |||||||
| How long is each visit on average? | About 15 min | 15–30 min | 30–45 min | 1 h or more | Total | ||
| 50 | 165 | 81 | 50 | 346 | |||
| 14% | 48% | 23% | 14% | 100% | |||
| Total time | |||||||
| Total time with neurologist in 2014 | 0 min | 15–60 min | 61–120 min | >120 | Total | ||
| 29 | 206 | 92 | 19 | 346 | |||
| 8% | 60% | 27% | 5% | 100% | |||
| Time sufficiency | |||||||
| Do you think your time with the neurologist is sufficient? (1 = not at all, 5 = absolutely) | 1 | 2 | 3 | 4 | 5 | Total | |
| 67 | 55 | 76 | 72 | 76 | 346 | ||
| 19% | 16% | 22% | 21% | 22% | 100% | ||
Table 5.
Total time spent in healthcare for PD.
| Total time spent in healthcare for PD during 2014 (neurologist visits excluded) | Count |
|---|---|
| <5 h | 70 |
| 5–10 h | 18 |
| 10–20 h | 26 |
| >20 h | 47 |
| Total | 161 |
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was financially supported by FORTE, the Swedish Research Council for Health, Working Life and Welfare (grant no. 2014-4238); and Vinnova, the Swedish Governmental Agency for Innovation Systems.
Contributor Information
Sara Riggare, Karolinska Institutet, Sweden.
Pär J Höglund, Jönköping University, Sweden.
Maria Hägglund, Karolinska Institutet, Sweden.
References
- 1. Lees AJ, Hardy J, Revesz T. Parkinson’s disease. Lancet 2009; 373: 2055–2066. [DOI] [PubMed] [Google Scholar]
- 2. Fincher L, Ward C, Dawkins V, et al. Using Telehealth to educate Parkinson’s disease patients about complicated medication regimens. J Gerontol Nurs 2009; 35: 16–25. [DOI] [PubMed] [Google Scholar]
- 3. Katzenschlager R, Head J, Schrag A, et al. Fourteen-year final report of the randomized PDRG-UK trial comparing three initial treatments in PD. Neurology 2008; 71: 474–480. [DOI] [PubMed] [Google Scholar]
- 4. Lökk J, Borg S, Svensson J, et al. Drug and treatment costs in Parkinson’s disease patients in Sweden. Acta Neurol Scand 2012; 125: 142–147. [DOI] [PubMed] [Google Scholar]
- 5. Dorsey ER, Constantinescu R, Thompson JP, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology 2007; 68: 384–386. [DOI] [PubMed] [Google Scholar]
- 6. Lawn S, Schoo A. Supporting self-management of chronic health conditions: common approaches. Patient Educ Couns 2010; 80: 205–211. [DOI] [PubMed] [Google Scholar]
- 7. Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003; 26: 1–7. [DOI] [PubMed] [Google Scholar]
- 8. Butterworth K, Allam O, Gray A, et al. Providing confusion: the need for education not information in chronic care. Health Informatics J 2012; 18: 111–123. [DOI] [PubMed] [Google Scholar]
- 9. Fox S, Purcell K. Chronic disease and the Internet, 2010, http://pewinternet.org/Reports/2010/Chronic-Disease.aspx
- 10. Ayers SL, Kronenfeld JJ. Chronic illness and health-seeking information on the Internet. Heal 2007; 11: 327–347. [DOI] [PubMed] [Google Scholar]
- 11. Matthews AK, Sellergren SA, Manfredi C, et al. Factors influencing medical information seeking among African American cancer patients. J Heal Commun 2002; 7: 205–219. [DOI] [PubMed] [Google Scholar]
- 12. Rahmqvist M, Bara A-C. Patients retrieving additional information via the Internet: a trend analysis in a Swedish population, 2000–05. Scand J Public Health 2007; 35: 533–539. [DOI] [PubMed] [Google Scholar]
- 13. Wahlstedt E, Ekman B. Patient choice, Internet based information sources, and perceptions of health care: evidence from Sweden using survey data from 2010 and 2013. BMC Health Serv Res 2016; 16: 325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chiu J, Silver M, Lee K, et al. Consumer use of ‘Dr Google’: a survey on health information-seeking behaviors and navigational needs. J Med Internet Res 2015; 17: e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Takahashi Y, Ohura T, Ishizaki T, et al. Internet use for health-related information via personal computers and cell phones in Japan: a cross-sectional population-based survey. J Med Internet Res 2011; 13: e110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Findahl O, Davidsson P. Swedes and the Internet 2015 (in Swedish), 2015, www.internetstatistik.se
- 17. Berner J, Rennemark M, Jogréus C, et al. Factors influencing Internet usage in older adults (65 years and above) living in rural and urban Sweden. Health Informatics J 2015; 21(3): 237–249. [DOI] [PubMed] [Google Scholar]
- 18. Sunvisson H, Ekman SL, Hagberg H, et al. An education programme for individuals with Parkinson’s disease. Scand J Caring Sci 2001; 15: 311–317. [DOI] [PubMed] [Google Scholar]
- 19. Chenoweth L, Gallagher R, Sheriff JN, et al. Factors supporting self-management in Parkinson’s disease: implications for nursing practice. Int J Older People Nurs 2008; 3: 187–193. [DOI] [PubMed] [Google Scholar]
- 20. Calne SM, Kumar A. Young onset Parkinson’s disease. Practical management of medical issues. Parkinsonism Relat Disord 2008; 14: 133–142. [DOI] [PubMed] [Google Scholar]
- 21. Kleiner-Fisman G, Gryfe P, Naglie G. A patient-based needs assessment for living well with Parkinson disease: implementation via nominal group technique. Parkinsons Dis 2013; 2013: 11–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. van der Eijk M, Faber MJ, Al Shamma S, et al. Moving towards patient-centered healthcare for patients with Parkinson’s disease. Parkinsonism Relat Disord 2011; 17: 360–364. [DOI] [PubMed] [Google Scholar]
- 23. Kremer JAM, van der Eijk M, Aarts JWM, et al. The individual formerly known as patient, TIFKAP. Minerva Med 2011; 102: 505. [PubMed] [Google Scholar]
- 24. van der Eijk M, Faber MJ, Aarts JWM, et al. Using online health communities to deliver patient-centered care to people with chronic conditions. J Med Internet Res 2013; 15: e115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wicks P, Stamford J, Grootenhuis MA, et al. Innovations in e-health. Qual life Res 2014; 23(1): 195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wicks P, Massagli M, Frost J, et al. Sharing health data for better outcomes on PatientsLikeMe. J Med Internet Res 2010; 12: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dobkin RD, Rubino JT, Friedman J, et al. Barriers to mental health care utilization in Parkinson’s disease. J Geriatr Psychiatry Neurol 2013; 26: 105–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ratzan SC, Parker RM. Health literacy – identification and response. J Health Commun 2006; 11: 713–715. [DOI] [PubMed] [Google Scholar]
- 29. Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res 2006; 8: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fitzsimmons P. Sharing clinic letters with Parkinson’s disease patients – a multicenter quantitative health literacy study. Age and Ageing 2011; 40: ii40. [Google Scholar]
- 31. Fleisher J, Minger J, Fitts W, et al. Low health literacy: an under-recognized obstacle in Parkinson’s disease. In: Movement disorders, 2014, pp. S158–S159, http://www.neurology.org/content/82/10_Supplement/P3.075
- 32. Armistead-Jehle P, Cifu DX, Wetzel R, et al. Health literacy among patients diagnosed with movement disorders: a pilot study. PM R 2010; 2: 43–47. [DOI] [PubMed] [Google Scholar]
- 33. Shimbo T, Goto M, Morimoto T, et al. Association between patient education and health-related quality of life in patients with Parkinson’s disease. Qual Life Res 2004; 13: 81–89. [DOI] [PubMed] [Google Scholar]
- 34. A’Campo LEI, Wekking EM, Spliethoff-Kamminga NGA, et al. The benefits of a standardized patient education program for patients with Parkinson’s disease and their caregivers. Parkinsonism Relat Disord 2010; 16: 89–95. [DOI] [PubMed] [Google Scholar]
- 35. Li J, Chen D, Song W, et al. Survey on general knowledge on Parkinson’s disease in patients with Parkinson’s disease and current clinical practice for Parkinson’s disease among general neurologists from Southwest China. Clin Neurol Neurosurg 2014; 118: 16–20. [DOI] [PubMed] [Google Scholar]
- 36. Hoving C, Visser A, Mullen PD, et al. A history of patient education by health professionals in Europe and North America: from authority to shared decision making education. Patient Educ Couns 2010; 78: 275–281. [DOI] [PubMed] [Google Scholar]
- 37. Dorsey ER, Voss TS, Shprecher DR, et al. A U.S. survey of patients with Parkinson’s disease: satisfaction with medical care and support groups. Mov Disord 2010; 25: 2128–2135. [DOI] [PubMed] [Google Scholar]
- 38. Cosentino M, Martignoni E, Michielotto D, et al. Medical healthcare use in Parkinson’s disease: survey in a cohort of ambulatory patients in Italy. BMC Health Serv Res 2005; 5: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Typeform. https://www.typeform.com (accessed 10 May 2016).
- 40. Sue VM, Ritter LA. Conducting online surveys. 2nd ed. Thousand Oaks, CA: SAGE, 2012. [Google Scholar]
- 41. Preacher KJ. Calculation for the chi-square test: an interactive calculation tool for chi-square tests of goodness of fit and independence, 2001, http://quantpsy.org
- 42. Schrag A, Schott JM. Epidemiological, clinical, and genetic characteristics of early-onset Parkinsonism. Lancet Neurol 2006; 5: 355–363. [DOI] [PubMed] [Google Scholar]
- 43. Statistiska Centralbyrån. Utbildningsnivå efter kön (in Swedish), http://www.scb.se/sv_/Hitta-statistik/Statistik-efter-amne/Miljo/Miljoekonomi-och-hallbar-utveckling/Indikatorer-for-hallbar-utveckling/21312/21319/Aldre-indikatoruppsattning-2001-uppdaterad-2006/Utbildningsniva-efter-kon/ (2010, accessed 1 February 2016).
- 44. National Board of Health and Welfare. Läkemedelsorsakad sjuklighet hos äldre (in Swedish), 2014, https://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/19621/2014-12-13.pdf
- 45. Anderson JG. Consumers of e-health: patterns of use and barriers. Soc Sci Comput Rev 2004; 22:242–248. [Google Scholar]
- 46. McMullan M. Patients using the Internet to obtain health information: how this affects the patient-health professional relationship. Patient Educ Couns 2006; 63: 24–28. [DOI] [PubMed] [Google Scholar]
- 47. Ferguson T, Frydman G. The first generation of e-patients. BMJ 2004; 328: 1148–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wu K, Politis M, O’Sullivan SS, et al. Problematic Internet use in Parkinson’s disease. Parkinsonism Relat Disord 2014; 20: 482–487. [DOI] [PubMed] [Google Scholar]
- 49. Samuel M, Rodriguez-oroz M, Antonini A, et al. Management of impulse control disorders in Parkinson’s disease: controversies and future approaches pharmacologic management. Mov Disord 2015; 30: 150–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Fitzsimmons PR, Michael BD, Hulley JL, et al. A readability assessment of online Parkinson’s disease information. J R Coll Physicians Edinb 2010; 40: 292–296. [DOI] [PubMed] [Google Scholar]