Abstract
Purpose:
To evaluate the incidence, related perioperative factors, clinical characteristics, and possible etiologies of epithelial keratitis after cataract surgery.
Methods:
A retrospective chart review of 666 eyes in 666 patients who underwent cataract surgery was performed to evaluate the incidence of epithelial keratitis and related factors in the postoperative period.
Results:
Postoperative epithelial keratitis developed in 15 eyes. Eleven of the 15 eyes were diagnosed with herpes simplex keratitis (HSK); 10 of the 11 eyes were diagnosed by polymerase chain reaction, and the remaining 1 eye by clinical diagnosis. All patients diagnosed with HSK had no previous clinical history of the infection before undergoing cataract surgery. Initially, the diagnosis of all 15 eyes was toxic keratitis, but the final diagnosis of 11 of the initial 15 was found to be epithelial herpes keratitis. The incision location was shown to be related to the occurrence of HSK in our study (P < 0.05).
Conclusions:
HSK epithelial keratitis after cataract surgery is a relatively uncommon complication and can be misdiagnosed in its early disease course because of its relative rarity. This study explores the possibility that the temporal corneal penetrating incisional approach used in routine cataract surgery interrupts the corneal nerves and subsequently can trigger reactivation of HSK.
Keywords: corneal epithelium, Herpes simplex keratitis, cataract surgery, toxic keratitis
Epithelial keratitis after cataract surgery derives from a wide range of etiologies such as preoperative and postoperative dry eye, intraoperative surgical trauma, injudicious use of topical steroid medication, or infection.1–3
Specifically, herpes simplex keratitis (HSK) has been documented in the literature as a possible complication after various ocular surgical procedures, such as cataract surgery,4–6 vitrectomy,7 laser-assisted in situ keratomileusis,8,9 excimer laser surgery,10 penetrating keratoplasty (PK),11 and lamellar keratoplasty including Descemet membrane endothelial keratoplasty.12,13 HSK after ocular surgery can be due to either secondary infection/reactivation of herpes simplex virus (HSV) or primary infection/newly acquired HSV infection.11,13,14
In evaluating outcomes of postoperative infections in our retrospective review of 666 eyes in 666 patients after cataract surgery, we found a relatively high incidence of HSK. Fifteen eyes developed epithelial keratitis after cataract surgery within a postoperative period of 1 year. Eleven of the 15 eyes were diagnosed with HSK.
We present our analysis of these outcomes in the context of perusal of the current literature surrounding this topic and explore possible perioperative factors that may have contributed to the development of this complication.
MATERIALS AND METHODS
This study was performed in accordance with the tenets of the Declaration of Helsinki and with Institutional Review Board approval of St. Vincent’s Hospital. We retrospectively reviewed a series of 666 patients and documented cases of unexpected development of epithelial keratitis (further divided into either postoperative toxic keratitis or HSK) after routine uneventful cataract surgery at a single institution within a postoperative period of 1 year. Epithelial keratitis was defined as superficial punctate erosion and/or epithelial defect.
Surgeries were performed under retrobulbar anesthesia (2.0% lidocaine and 0.5% bupivacaine). Additional topical anesthetics such as Alcaine (proparacaine hydrochloride) were instilled at 5-minute intervals until 10 minutes before the start of surgery and clear corneal incision. A Whitestar Signature phacoemulsification machine (Abbott Medical Optics, Inc, Santa Ana, CA) was used with standardized machine settings at the discretion of the surgeon.
In cases in which epithelial keratitis occurred after cataract surgery, the following were reviewed and documented: 1) time before the appearance of keratitis, 2) location of the lesion, 3) layer of cornea of the lesion, 4) location of the incision, 5) accompanying diseases, 6) initial diagnosis and clinical manifestation, 7) perioperative medication, and 8) the result of HSV-1 polymerase chain reaction (PCR).
PCR was performed within 2 days of initial clinical manifestation of epithelial keratitis. Samples were collected in one of 2 ways: 1) a tear sample rinsed with 500 μL saline solution15 or 2) direct scraping of the corneal lesion.
Statistical analysis was performed using the Pearson χ2 test. P < 0.05 was considered to be statistically significant.
In addition, a literature review of previous publications on this topic was conducted with the following PubMed search terms: “herpes simplex,” “cataract,” “phacoemulsification,” and “postoperative infection.”
RESULTS
A summary of demographic characteristics of patients is shown in Tables 1, 2, and 3. All patients denied any history of previous ocular infections, and all corneas were documented as clear at preoperative slit-lamp examination.
TABLE 1.
Summary of Patients
| Operation | Phaco + PCL (499 Eyes) | Phaco + PCL + PPV (167 Eyes) | |||
|---|---|---|---|---|---|
| Incision Location | Temporal (141 Eyes) | Superior (358 Eyes) | Temporal (106 Eyes) | Superior (61 Eyes) | |
| Corneal epithelial keratitis (15 eyes) | HSK+ | 9 | 0 | 2 | 0 |
| TK+ | 1 | 1 | 1 | 1 | |
HSK+, eyes that showed postoperative HSK; Phaco + PCL + PPV, phacoemulsification and posterior chamber lens insertion and pars plana vitrectomy; Phaco + PCL, phacoemulsification and posterior chamber lens insertion; TK+, eyes that did not show postoperative HSK but showed toxic keratitis.
TABLE 2.
Clinical Features of Patients With Postoperative Toxic Keratitis
| Case | Sex/Age (yrs) | Underlying Disease |
History of HSK | Type of Surgery | Cornea Before Cataract Operation |
Time Between Surgery and Presentation (d) |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female/66 | None | No history | Phaco + PCL | Clear | 5 | ||||
| 2 | Female/71 | None | No history | Phaco + PCL | Clear | 5 | ||||
| 3 | Female/55 | None | No history | Phaco + PCL + PPV | Clear | 7 | ||||
| 4 | Female/61 | DM | No history | Phaco + PCL + PPV | Clear | 2 | ||||
| Case |
Perioperative Medication |
Initial Diagnosis |
Initial Clinical Manifestation |
Incision Location |
Final Diagnosis |
Medication After Diagnosis |
HSV-1 PCR |
|||
| 1 | Topical steroids and antibiotics | Toxic keratitis | Diffuse SPEs | Superior | Toxic keratitis | Lubrication | Negative | |||
| 2 | Topical steroids and antibiotics | Toxic keratitis | Diffuse SPEs | Temporal | Toxic keratitis | Lubrication | Negative | |||
| 3 | Topical steroids and antibiotics | Toxic keratitis | Diffuse SPEs | Temporal | Toxic keratitis | Lubrication | Negative | |||
| 4 | Topical steroids and antibiotics | Toxic keratitis | Diffuse SPEs | Superior | Toxic keratitis | Lubrication | Negative | |||
PE, superficial punctate erosion; Phaco + PCL, phacoemulsification and posterior chamber lens insertion; Phaco +PCL + PPV, phacoemulsification and posterior chamber lens insertion and pars plana vitrectomy.
TABLE 3.
Clinical Features of Patients With Postoperative HSK
| Case | Sex/Age (yrs) | Underlying Disease |
History of HSK | Type of Surgery | Cornea Before Cataract Operation |
Time Between Surgery and Presentation (d) |
Perioperative Medication |
|
|---|---|---|---|---|---|---|---|---|
| 1 | Female/69 | DM | No history | Phaco + PCL + PPV | Clear | 7 | Topical steroids and antibiotics | |
| 2 | Female/71 | None | No history | Phaco + PCL | Clear | 5 | Topical steroids and antibiotics | |
| 3 | Female/65 | None | No history | Phaco + PCL | Clear | 20 | Topical steroids and antibiotics | |
| 4 | Female/58 | DM | No history | Phaco + PCL + PPV | Clear | 14 | Topical brimonidine, topical steroids, and antibiotics | |
| 5 | Female/62 | DM | No history | Phaco + PCL | Clear | 21 | Topical steroids and antibiotics | |
| 6 | Female/75 | Rheumatoid arthritis | No history | Phaco + PCL | Unknown | 10 | Oral steroids, topical steroids, and antibiotics | |
| 7 | Female/76 | Rheumatoid arthritis | No history | Phaco + PCL | Some SPEs | 20 | Oral steroids, topical steroids, and antibiotics | |
| 8 | Female/75 | None | No history | Phaco + PCL | Clear | 7 | Topical steroids and antibiotics | |
| 9 | Female/68 | None | No history | Phaco + PCL | Clear | 20 | Topical steroids and antibiotics | |
| 10 | Female/71 | None | No history | Phaco + PCL | Clear | 15 | Topical steroids and antibiotics | |
| 11 | Female/65 | None | No history | Phaco + PCL | Clear | 30 | Topical steroids and antibiotics | |
| Case |
Initial Diagnosis |
Initial Clinical Menifestation |
Incision Location |
Final Diagnosis |
Medication After HSK Diagnosis |
HSV-1 PCR | ||
| 1 | Toxic keratitis | Epithelial defect | Temporal | Epithelial HSK | Oral acyclovir | Positive | ||
| 2 | Toxic keratitis | Epithelial defect | Temporal | Epithelial HSK | Oral valacyclovir | Positive | ||
| 3 | Toxic keratitis | Severe SPEs and epithelial irregularity | Temporal | Epithelial HSK | Oral valacyclovir | Positive | ||
| 4 | Toxic keratitis | Diffuse SPEs and some Descemet membrane folds | Temporal | Epithelial HSK | Oral acyclovir | Positive | ||
| 5 | Toxic keratitis | Diffuse SPEs | Temporal | Epithelial HSK | Valacyclovir | Positive | ||
| 6 | Uveitis | Some SPEs, linear KPs, and corneal edema | Temporal | Linear endotheliitis | Oral and topical acyclovir; oral and topical steorids | Not applied | ||
| 7 | Toxic keratitis | Epithelial defect with edema | Superotemporal | Epithelial HSK | Oral and topical acyclovir | Positive | ||
| 8 | Toxic keratitis | Epithelial defect | Temporal | Epithelial HSK | Oral valacyclovir | Positive | ||
| 9 | Toxic keratitis | Severe SPEs and epithelial irregularity | Temporal | Epithelial HSK | Oral valacyclovir | Positive | ||
| 10 | Toxic keratitis | Epithelial defect | Temporal | Epithelial HSK | Oral valacyclovir | Positive | ||
| 11 | Toxic keratitis | Epithelial defect and SPEs | Temporal | Epithelial HSK | Oral valacyclovir | Positive | ||
KP, keratic precipitate; Phaco + PCL + PPV, phacoemulsification and posterior chamber lens insertion and pars plana vitrectomy; Phaco + PCL, phacoemulsification and posterior chamber lens insertion; SPE, superficial punctate erosion.
Among the total 666 eyes of 666 patients who had undergone cataract surgery, 15 eyes (2.25%) developed postoperative epithelial keratitis (corneal erosion and/or superficial punctate keratitis) (Tables 1, 2 and 3).
Four of the 15 eyes were diagnosed with toxic keratitis (Table 2). This complication occurred within 7 days postoperatively. The mean time to develop the initial clinical manifestation was 4.75 days. Time to initial onset was shorter in toxic keratitis than in HSK (mean time to initial clinical manifestation: 15 days).
The corneal lesion of toxic keratitis resolved completely within 10 days of the initial onset by decreasing the topical medication and vigorously lubricating the eye. One patient with this complication had diabetes mellitus.
The remaining 11 eyes were diagnosed with HSK (Table 3). This complication occurred within 30 days postoperatively. The mean time to develop the initial clinical manifestation was 15 days.
Two patients had pars plana vitrectomy immediately after cataract surgery with clear corneal incision. In addition, one of these 2 patients had used topical brimonidine starting several months before surgery.
Three patients had diabetes mellitus, and 2 patients had rheumatoid arthritis. The 2 patients with rheumatoid arthritis had been taking low-dose oral steroids starting several years before undergoing cataract surgery.
Ten of the 11 patients were initially diagnosed with toxic keratitis but were later diagnosed with epithelial HSK by detection of HSV type I virus by PCR. All these patients were treated with oral antiviral therapy.
One patient was initially diagnosed with toxic keratitis and uveitis but was later clinically diagnosed with linear HSK endotheliitis (Table 3, case 6). This patient was treated with topical and oral antiviral medications and steroids.
Two hundred forty-seven of the 666 patients had temporal corneal incision approaches, and 419 of the 666 patients had superior corneal incision approaches during cataract surgery (Table 1). Ten of the 11 patients with HSK had temporal corneal incisions (2.5–3.0 mm cataract wound), and 1 patient had a superotemporal incisional location. There was no documented HSK complication with a superior corneal incision approach. As in the literature, the prevalence of HSK of our study was significantly higher with a temporal corneal incision approach than with a superior corneal incision approach (P < 0.05).
The location of the HSK lesion (epithelial defect or dendritic lesion) was not adjacent to the temporal incision, except in the 1 previously described patient who was clinically diagnosed with linear HSK endotheliitis—linear keratic precipitates and corneal edema adjacent to the temporal incision were found on postoperative slit-lamp examination. At the time of the initial clinical manifestation, all patients with HSK were treated with topical antibiotics and topical steroids.
Four hundred ninety-nine of the 666 patients had cataract surgery alone, and the remaining 167 patients had pars plana vitrectomy in addition to cataract surgery. The prevalence rate of HSK in eyes with cataract surgery was 1.80% (9 of 499 eyes) and 1.19% (2 of 167 eyes) with pars plana vitrectomy and cataract surgery. This was not statistically significant (P > 0.05) (Table 1).
DISCUSSION
Epithelial keratitis after cataract surgery has various etiologies.2,3,16 Early recognition of the cause and subsequent prompt treatment should be undertaken to ensure optimal final visual prognosis. Even in patients with no previous clinical history of ocular infections who later develop epithelial corneal lesions after routine, uneventful surgery, surgeons should be cognizant of the possible infectious etiology of the presenting lesion.
Initially, the lesion may be treated as toxic keratitis or postoperative dry eye, warranting conservative treatment: stop offending toxic medications and vigorously lubricate the eye.17 However, if the lesion is refractory to initial treatment or progresses even after cessation of toxic medications and adequate, copious corneal lubrication, epithelial herpes keratitis should be suspected as a probable cause. Postoperative manifestations of HSK in this study, that is, primarily punctate erosions, were different from nonoperative manifestations of HSK, in which dendrites were typically present at the outset.
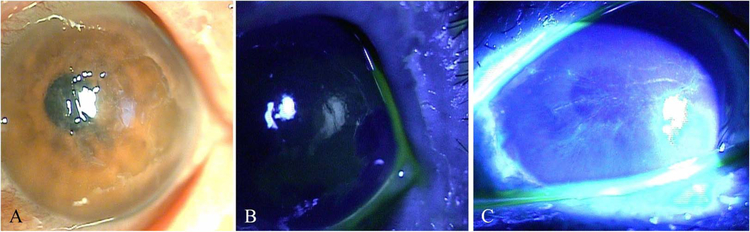
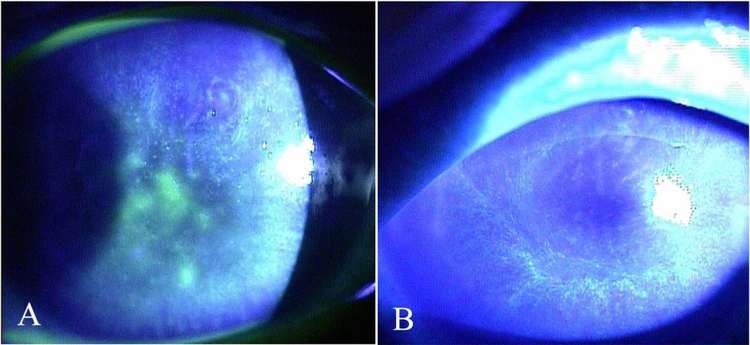
The initial diagnosis of 10 of the 11 documented patients was toxic keratitis—postoperative slit-lamp examination showed corneas with epithelial irregularities, which progressed to typical dendritic keratitis within 2 to 3 days of onset (Figs. 1 and 2). Because of the lack of previously known history of HSK, these lesions were presumed to be either postoperative uveitis or toxic keratitis. However, PCR of epithelial scrapings or tear samples showed HSK.
FIGURE 1.
HSK after phacoemulsification and posterior chamber intraocular lens insertion and pars plana vitrectomy (Table 3, case 1). A, Initial visit—initial presentation of corneal epithelial defect. B, Two days after the initial visit—enlargement of corneal epithelial defect. C, Five days after the initial visit—progression of an epithelial lesion to a dendritic corneal lesion.
FIGURE 2.
HSK after phacoemulsification and posterior chamber intraocular lens insertion (Table 3, case 3). A, Initial visit—initial presentation of epithelial irregularity. B, Three days after the initial visit—progression of an epithelial irregularity to a dendritic corneal lesion.
As many as 50% to 60% of patients are latently infected with HSV-1 (type 1) and presumably harbor the dormant virus in their sensory ganglia. Local trauma such as corneal surgeries can reactivate the virus and cause secondary infections.11,13,14 Among the reported occurrences of HSK after ocular surgery, HSK after PK has been reported more frequently than HSK after cataract surgery.4–6,11,13,14 We suspect that this is due to the near-360-degree larger disturbance of the subepithelial trigeminal nerve plexus in PK than in cataract surgery, in which there is only a small degree of disturbance. Another plausible contributing factor is the longer duration of corticosteroid use after PK than after cataract surgery. However, these 2 factors may play a role in elucidating the possible etiologies of HSK after cataract surgery: 1) trauma to the subepithelial trigeminal nerve plexus by the corneal incision location and 2) intensive treatment with topical corticosteroids in the postoperative period.4–6
With respect to the corneal incision location and HSK prevalence, nearly all patients who developed postoperative HSK in our retrospective study had a temporal corneal incisional approach (1 patient with a superotemporal incisional approach). The corneal nerves are derived from the long ciliary nerves of the ophthalmic division of the fifth (trigeminal) cranial nerve; these nerves enter the limbus predominantly at the 9-o’clock and 3-o’clock positions.18 We suspect that corneal nerves are more likely severed with a temporal incision than with a superior incision, and hence, this can contribute to triggering HSV reactivation. A literature review of previous studies shows a reported increased prevalence of HSK with temporal (and superotemporal) incisions than with superior incisions4–6,19 (see Table, Supplemental Digital Content 1, http://links.lww.com/ICO/A649).
We found no relationship between the location of the HSK lesion and the cataract incision location. Barequet and Wasserzug4 had similar findings—the location of HSK in the cornea was not adjacent or related to the cataract corneal incision site. Jhanji et al,6 however, reported all 3 cases of post-cataract HSK adjacent to the corneal incision.
One patient (Table 3, case 6) was clinically diagnosed with herpetic keratouveitis—postoperative slit-lamp examination showed linear endotheliitis, corneal edema around the temporal corneal incision, and linear keratic precipitates at the margin of corneal edema. However, this diagnosis was clinical and not definitively confirmed by PCR; hence, we cannot exclude the possibility of cytomegalovirus endotheliitis or herpes zoster virus (HSV) endotheliitis. Nevertheless, the configuration of keratic precipitates and low intraocular pressure combined with the response to oral and topical acyclovir makes HSV more likely.21
Olson et al19 reported 2 patients with linear HSV endotheliitis after uneventful cataract extraction (see Table, Supplemental Digital Content 1, http://links.lww.com/ICO/A649). The zone of endotheliitis was reported to have corresponded to the location of the corneal incision during cataract surgery—the linear keratic precipitate and corneal edema of the 2 patients were found to be just adjacent to the temporal corneal incision.19 They suggested that HSV endotheliitis after cataract surgery is related to inflammation associated with the location of the cataract corneal incision and trauma to corneal nerves.19,20
Additional surgery (eg, pars plana vitrectomy) had no significant effect on triggering activation of HSK (P >0.05). The prevalence of HSK was 1.80% in cataract surgery alone and 1.19% in cataract surgery concomitant with pars plana vitrectomy.
Antiglaucoma drug latanoprost,4,11,22 atopy,5 and immunosuppressive agents such as cyclosporine5 have also been connected with postoperative HSK.23 Immunosuppressive agents used in rheumatoid disease (Table 3, cases 6 and7) could also have played a role in HSK reactivation.24
Based on the results of our study, we suggest that regardless of the patient’s previous history of keratitis, if the patient develops typical or atypical punctate epithelial keratitis in the early postoperative period after cataract surgery (especially with a temporal clear corneal incision), close follow-up and empiric treatment of HSK are warranted.
Supplementary Material
Footnotes
The authors have no funding or conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.corneajrnl.com).
REFERENCES
- 1.Steinert RF. Cataract surgery in the presence of other ocular comorbidity In: Cataract Surgery. 3rd ed. Philadelphia: Elsevier Inc; 2010. chap 34. [Google Scholar]
- 2.Yeniad B, Canturk S, Esin OF, et al. Toxic keratopathy due to abuse of topical anesthetic drugs. Cutan Ocul Toxicol. 2010;29:105–109. [DOI] [PubMed] [Google Scholar]
- 3.Kwon JW, Chung YW, Choi JA, et al. Comparison of postoperative corneal changes between dry eye and non-dry eye in a murine cataract surgery model. Int J Ophthalmol. 2016;9:218–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barequet IS, Wasserzug Y. Herpes simplex keratitis after cataract surgery. Cornea. 2007;26:615–617. [DOI] [PubMed] [Google Scholar]
- 5.Patel NN, Teng CC, Sperber LTD, et al. New-onset herpes simplex virus keratitis after cataract surgery. Cornea. 2009;28:108–110. [DOI] [PubMed] [Google Scholar]
- 6.Jhanji V, Ferdinands M, Sheorey H, et al. Unusual clinical presentations of new-onset herpetic eye disease after ocular surgery. Acta Ophthalmol. 2012;90:514–518. [DOI] [PubMed] [Google Scholar]
- 7.Chen HS, Yeung L, Yang KJ, et al. Persistent corneal epithelial defect after pars plana vitrectomy. Retina. 2016;36:148–155. [DOI] [PubMed] [Google Scholar]
- 8.Jain V, Pineda R. Reactivated herpetic keratitis following laser in situ keratomileusis. J Cataract Refract Surg. 2009;35:946–948. [DOI] [PubMed] [Google Scholar]
- 9.Arora T, Sharma N, Arora S, et al. Fulminant herpetic keratouveitis with flap necrosis following laser in situ keratomileusis: case report and review of literature. J Cataract Refract Surg. 2014;40:2152–2156. [DOI] [PubMed] [Google Scholar]
- 10.Jabbur NS, O’Brien TP. Recurrence of keratitis after excimer laser keratectomy. J Cataract Refract Surg. 2003;29:198–201. [DOI] [PubMed] [Google Scholar]
- 11.Rezende RA, Uchoa UBC, Raber IM, et al. New onset of herpes simplex virus epithelial keratitis after penetrating keratoplasty. Am J Ophthalmol. 2004;137:415–419. [DOI] [PubMed] [Google Scholar]
- 12.Zarei-Ghanavati S, Alizadeh R, Yoo SH. Herpes simplex virus endothelitis following Descemet’s membrane endothelial keratoplasty. J Ophthalmic Vis Sci. 2015;10:184–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghosh S, Jhanji V, Lamoureux E, et al. Acyclovir therapy in prevention of recurrent herpes keratitis following penetrating keratoplasty. Am J Ophthalmol. 2008;145:198–202. [DOI] [PubMed] [Google Scholar]
- 14.Tullo A Pathogenesis and management of herpes simplex virus keratitis. Eye. 2003;17:919–922. [DOI] [PubMed] [Google Scholar]
- 15.Fukuda M, Deai T, Hibino T, et al. Quantitative analysis of herpes simplex virus genome in tears from patients with herpetic keraittis. Cornea. 2003;22(suppl 1):S55–S60. [DOI] [PubMed] [Google Scholar]
- 16.Cho YK, Kim MS. Dry eye after cataract surgery and associated intraocular risk factors. Korean J Ophthalmol. 2009;23:65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krachmer JH, Mannis MJ, Holland EJ. Cornea. 3rd ed. Philadelphia: Mosby Elsevier; 2011. [Google Scholar]
- 18.Donnenfeld ED, Solomon K, Perry HD, et al. The effect of hinge position on corneal sensation and dry eye after LASIK. Ophthalmology. 2003; 110:1023–1030. [DOI] [PubMed] [Google Scholar]
- 19.Olsen TW, Hardten DR, Meiusi RS et al. Linear endotheliitis. Am J Ophthalmol. 1994;117:468–474. [DOI] [PubMed] [Google Scholar]
- 20.Rice RL, Tuberville AW, Wood TO. Endothelial line associated with pseudophakic bullous keratopathy. Cornea. 1985–1986;4:42–46. [PubMed] [Google Scholar]
- 21.Morishige N, Morita Y, Yamada N, et al. Differential changes in intraocular pressure and corneal manifestations in individuals with viral endothelitis after keratoplasty. Corena. 2016;35:602–606. [DOI] [PubMed] [Google Scholar]
- 22.Kaufman HE, Varnell ED, Thomson HW. Latanoprost increases the severity and recurrence of herpetic keratitis in rabbit. Am J Ophthalmol. 1999;127:531–536. [DOI] [PubMed] [Google Scholar]
- 23.Maier AKB, Ozulugedik S, Rottler J, et al. Efficacy of postoperative immunosuppression after keratoplasty in Herpes Keratitis. Cornea. 2011; 30:1398–1405. [DOI] [PubMed] [Google Scholar]
- 24.Fragoso PL, de Los Bueis AB, Ljubetic LB, et al. Herpes simplex keratitis in rheumatoid arthritis patients. Ocul Immunol Inflamm. 2016; 24:282–287. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.