Abstract
Background:
Fish oil is among the most common natural supplements for treatment of hypertriglyceridemia or prevention of cardiovascular disease. However, ongoing concerns about possible bleeding risk has led to recommendations that patients stop taking fish oil prior to surgery and/or delay in elective procedures for patients taking fish oil
Methods and Results:
We tested the effect of fish oil supplementation on peri-operative bleeding in a multinational, placebo-controlled trial involving 1516 patients who were randomized to perioperative fish oil (EPA + DHA; 8–10 g over 2–5 days preoperatively, then 2 g/day postoperatively) or placebo. Primary outcome was major peri-operative bleeding as defined by the Bleeding Academic Research Consortium (BARC). Secondary outcomes include peri-operative bleeding per TIMI and ISTH definitions, chest tube output, and total units of blood transfused. Mean(SD) participants age was 63(13) years, and planned surgery included CABG (52%) and valve surgery (50%). The primary outcome occurred in 92 patients (6.1%). Compared to placebo, risk of BARC bleeding was not higher in the fish oil group: OR=0.81, 95%CI=0.53–1.24; absolute risk difference=1.1% lower (95%CI= −3.0 to 1.8%). Similar findings were seen for secondary bleeding definitions. The total units of blood transfused were significantly lower in the fish oil group compared to placebo (mean=1.61 vs 1.92, p<0.001). Evaluating achieved plasma phospholipid n-3-PUFA levels with supplementation (on the morning of surgery), higher levels were associated with lower risk of BARC bleeding, with substantially lower risk in the third (OR=0.30 [95%CI, 0.11–0.78]) and fourth (0.36 [95%CI, 0.15–0.87]) quartiles, compared with the lowest quartile.
Conclusions:
Fish oil supplementation did not increase peri-operative bleeding; and reduced the number of blood transfusions. Higher achieved n-3-PUFA levels were associated with lower risk of bleeding. These novel findings support the need for reconsideration of current recommendations to stop fish oil or delay procedures prior to cardiac surgery.
Clinical Trial Registration
URL: http://Clinicaltrials.gov
Unique identifier: NCT00970489
Keywords: Diet and Nutrition, Cardiovascular Surgery, Quality and Outcomes
Fish oil provides a concentrated source of the long-chain omega-3 fatty acids eicosapentaenoic and docosahexaenoic acids (EPA and DHA). These fatty acid have a wide array of biologic activities related to cardiovascular health, including lowered blood pressure and triglycerides, and improved endothelial vasodilator function.1, 2 Accordingly, individuals having or at risk for cardiovascular disease (CVD) frequently use fish oil supplements, with about 8% of such people taking either prescription or supplement fish oil.3, 4 Yet, concerns persist regarding possible bleeding risks of fish oil consumption, particularly during major surgical procedures. EPA and DHA may compete with arachidonic acid (AA) for incorporation into the platelet membrane or cyclooxygenase-mediated pathways,5 leading to reduced production of AA-derived prothrombotic metabolites such as thromboxane A2 and increased production of anti-thrombotic EPA metabolites that could reduce platelet activation and aggregation. Concerns over the potential risk of bleeding associated with this antiplatelet effect have led to recommendations that patients stop taking fish oil supplements prior to surgery and for delay in elective surgical procedures for patients taking fish oil.6–11 Yet, little or no objective clinical evidence supports this practice. The risk of increased bleeding with fish oil consumption remains largely theoretical, as prior clinical trials have not reported significantly increased risk of bleeding with fish oil supplementation.12–16 However, few of these prior trials enrolled patients undergoing surgery, existing studies in surgical patients have been generally small (up to several hundred patients), and few prior studies prospectively collected information on bleeding during and after surgery in a standardized fashion. Thus, rigorous evaluation of the effect of fish oil supplements on bleeding risk during and after surgery is needed. Understanding the presence and magnitude of such possible risks has considerable importance for clinical practice and for guidelines on fish oil use before surgery for those taking fish oil, including 19 million American adults.3
The Omega-3 Fatty Acids for Prevention of Postoperative Atrial Fibrillation (OPERA) trial was a multinational, placebo-controlled randomized trial designed to test the effect of peri-operative fish oil supplementation on postoperative atrial fibrillation (PoAF) in a broad, generalizable population of patients undergoing cardiac surgery.17 This trial that included more than 1,500 patients across 3 nations is the largest trial to-date that studied randomized peri-operative use of fish oil and standardized, prospective evaluation of intra- and post-operative bleeding outcomes. In an initial report from the OPERA trial, fish oil supplementation reduced the number of units of peri- and post-operative blood transfusion. The present investigation more comprehensively evaluates the effect of randomized fish oil treatment on a range of standardized intra- and post-op bleeding outcomes; whether other patient or surgery characteristics modified these effects; and also how circulating phospholipid omega-3 fatty acid concentrations at baseline and achieved after supplementation relate to these risk of bleeding. While bleeding outcomes, including clinical bleeding and transfusion requirements, were prespecified safety endpoints of the OPERA trials, the present investigation should be considered as a secondary analysis of the trial.
METHODS
The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure
Study Design and Patients
The design and primary results of OPERA have been described.17, 18 Briefly, 1,516 patients undergoing cardiac surgery were recruited across 28 centers in the United States, Italy and Argentina between Aug 2010 and Jun 2012 (Figure S1). Inclusion criteria were broad and generalizable including: age ≥18 years; upcoming cardiac surgery (any combination of coronary artery bypass graft [CABG], valve surgery, or other cardiac surgery opening the pericardium); and sinus rhythm at enrollment. Exclusion criteria included: regular use (≥3 days/wk) of fish oil within the prior 4 weeks; known allergy to fish oil or olive oil (placebo); current pregnancy; or inability to provide informed written consent. The study was approved by the Institutional Research Boards or equivalent of all participating institutions, and all patients provided written informed consent.
Interventions
Upon enrollment, the central Data Coordinating Center block-randomized patients to receive 1g capsules containing prescription fish oil (Lovaza, GSK; 465 mg of EPA + 375 mg of DHA) or matched placebo (olive oil) by means of computer-generated numbers, stratified by enrolling medical center and planned valve surgery (yes/no). All drugs were prepared in identical capsules with similar coatings to minimize taste differences. All investigators, patients, and providers were blinded to treatment assignment.
Based on the time period between enrollment and day of cardiac surgery, a total loading dose of 10 g was provided over 3 to 5 days (or 8 g over 2 days) prior to surgery, including 2 g on the morning of surgery. Postoperatively, a uniform dose of 2 g per day was provided starting on post-op day 1 until discharge or postoperative day 10, whichever came first.
Fatty acid analysis
In a subset of 564 patients in the US and Italy, objective biomarkers of plasma phospholipid fatty acids were measured as previously described.19 Briefly, fasting blood samples were collected at enrollment and on the morning of cardiac surgery, EDTA-anticoagulated, and stored at −70°C. Plasma phospholipid EPA, DPA, and DHA were measured as percent of total fatty acids by the Fred Hutchinson Cancer Research Institute (Seattle, WA). Phospholipids were separated by thin-layer chromatography and fatty acid methyl esters were subsequently prepared by direct transesterification. Final analysis was performed by gas chromatography. The inter-assay coefficients of variation for EPA, DPA and DHA were each <3%.
Endpoints
For the primary analysis, we followed the recommendations of the Bleeding Academic Research Consortium (BARC) for the standardized definition of peri-operative bleeding.20 Our main endpoint was the occurrence of a BARC type 4 or 5 event defined as the composite of fatal bleeding; peri-operative intracranial bleeding; reoperation after closure of the sternotomy for the purpose of controlling bleeding; transfusion of 5+ packed red blood cell units or whole blood, excluding cell saver, within 48 hours; or 24-hour chest tube output >2 L. In addition, we examined other commonly used bleeding measures including: (1) TIMI major bleeding defined as fatal bleeding, any intracranial bleeding, or clinically overt bleeding with drop in hemoglobin ≥5 g/dL or hematocrit ≥15 percent (accounting for transfusions); (2) TIMI minor bleeding defined as non-major bleeding that is clinically overt with drop in hemoglobin ≥3 g/dL or hematocrit ≥10 percent (accounting for transfusions), not overt but with drop in hemoglobin ≥4 g/dL or hematocrit ≥12 percent (accounting for transfusions), or clinically overt and requiring medical or surgical intervention, prolonging hospitalization, or prompting evaluation; (3) International Society on Thrombosis and Hemostasis (ISTH) surgical bleeding defined as fatal bleeding, symptomatic bleeding in a critical area or organ, extrasurgical site bleeding with drop in hemoglobin ≥2 g/dL or ≥2 units blood transfusion within 24–48 hours, surgical site bleeding that requires a second intervention, surgical site bleeding that is unexpected and prolonged and/or causes hemodynamic instability with drop in hemoglobin ≥2 g/dL or ≥2 units blood transfusion within 24 hours, in patients who received at least one dose of study drug; (4) chest tube output (ml) during the first 24 hours after cardiac surgery; and (5) total units of blood transfused. We also examined biomarkers related to bleeding including platelet counts, international normalized ratio (INR), plasminogen activator inhibitor-1 (PAI-1) levels, and 11-Dehydrothromboxane-B2 (11-dhTXB2) levels at post-op day 2. All bleeding outcomes were prespecified safety endpoints of the OPERA trials.
Methods of measurements for PAI-1 and 11-dhTXB2
PAI-1 antigen levels were determined using 2-site ELISA (Imulyse, Biopool AB), inter- and intra-assay CV of 0.019 and 0.024, detection limit 20 ng/mL
11-dhTXB2 was measured as established by Morrow and Minton.21 Internal standard [2H4]-11-dehydro-TxB2 was added to acidified urine, and the sample purified by C-18 solid phase extraction and converted to the methyloxime, pentafluorobenzyl ester, trimethylsilyl ether derivative for analysis by GC/MS. Assay interday variability ~10%; precision ±7%; accuracy 90%.
Covariates
Standardized data were collected on other key risk factors including patient demographics, cardiovascular risk factors, major comorbidities, medical/surgical history, anthropometry, home and peri-operative medications, baseline laboratory indices, and surgical characteristics. In addition, clinical follow up data were collected daily over the course of the trial.
Statistical analysis
The effect of fish oil supplementation on peri-operative bleeding was evaluated via intention-to-treat analysis comparing endpoints between the two randomized groups. Binary endpoints (e.g., BARC type 4 or 5 event, TIMI major bleeding event, TIMI minor bleeding event, ISTH surgical bleeding) were compared using logistic regression; volume of chest tube output as well as biomarkers of bleeding (except platelets), using linear regression (with robust variance); and total units of blood transfused and platelet counts, using Poisson regression. All analyses adjusted for the stratifying variables used in the randomization process (enrolling medical center and planned valve surgery (yes/no)) in order to account for the potential correlation of observations within these variables.22 We evaluated for potential interaction between treatment effect and clinically relevant variables including age (<65 vs. ≥65 years), gender, preoperative antithrombotic therapy (i.e. antiplatelet and/or anticoagulant), type of surgery (i.e. CABG vs. valve surgery), cardiopulmonary bypass use, and surgical access (open vs. mini thoracotomy). Interactions were evaluated separately for each variable by introducing a multiplicative interaction term between the treatment effect and the variable within the same model, and statistical significance was assessed using the Wald test. Given that interaction analyses were exploratory, alpha level was Bonferroni –adjusted for the six variables (12 hypothesis) tested per endpoint.
In a subset of 564 subjects with blood measurements of plasma phospholipid fatty acids, the association between omega-3 levels and occurrence of BARC type 4 or 5 bleeding event was examined based on levels at enrollment (reflecting habitual levels) and on achieved levels on the morning of cardiac surgery (reflecting habitual levels plus additional incorporation due to fish oil supplementation). The within-subject change between these two time points (reflecting potential inter-individual variability in response to supplementation) was also calculated.23 Each measure of omega-3 fatty acids was evaluated as indicator variable in quartiles in a multivariable logistic regression model that adjusted for potential confounding covariates including age, gender, race, body mass index, diabetes, hypertension, dyslipidemia, smoking, alcohol, preoperative antithrombotic therapy, type of surgery, cardiopulmonary bypass use, and open vs. mini thoracotomy surgical access.24–29 Test of linear trend across quartiles was assessed by entering the quartile variable as a single ordinal variable in the model. We also evaluated potential for nonlinear associations using a semi-parametric multivariable-adjusted restricted cubic spline model, after excluding patients with values<1st or >99th percentile of measured phospholipid omega-3 fatty acids to minimize the influence of outliers. Finally, we evaluated independent predictors of peri-operative bleeding using multivariable-adjusted logistic regression with backward stepwise selection procedure (P-exclusion=0.20, P-inclusion=0.10). Covariates above reported in the literature to associate with risk of peri-operative bleeding were considered for inclusion into the model while fish oil treatment assignment was retained for comparison.24–29 All analyses were performed using STATA 14 (StataCorp, College Station, Texas) with two-tailed alpha=0.05.
RESULTS
Among this large, multinational population of patients undergoing cardiac surgery, mean (SD) age was 63 (13) years and 72% were men. CABG was planned in 52%, valve surgery in 50%, and other types of cardiac surgeries in 18% (proportions are not mutually exclusive, as some patients could have more than one type of surgery). Of those enrolled and randomized, 96.4% ultimately underwent cardiac surgery. Details of surgery and peri-operative medications have been published,17 and baseline patient characteristics were comparable between the two treatment groups (Table 1).
Table 1:
Baseline characteristics of 1,516 patients undergoing cardiac surgery in the OPERA trial, overall and according to treatment assignment.
| Total (n=1516) |
Fish oil (n=758) |
Placebo (n=758) |
|
|---|---|---|---|
| Age, mean (SD), years | 64 (13) | 64 (13) | 64 (12) |
| Men, No. (%) | 1094 (72) | 551 (73) | 543 (72) |
| White race, No. (%) | 1450 (96) | 724 (96) | 726 (96) |
| Country, No. (%) | |||
| Italy | 764 (50) | 383 (51) | 381 (50) |
| United States | 445 (29) | 221 (29) | 224 (30) |
| Argentina | 307 (20) | 154 (20) | 153 (20) |
| BMI, median (IQR), kg/m2 | 27 (6.01) | 27 (5.93) | 27 (6.22) |
| Waist circumference, median (IQR), cm | 98 (15) | 97 (15) | 99 (17) |
| Diabetes mellitus, No. (%) | 393 (26) | 194 (26) | 199 (26) |
| Hypertension, No. (%) | 1135 (76) | 572 (76) | 563 (75) |
| Current smoking, No. (%) | 195 (13) | 99 (13) | 96 (13) |
| Dyslipidemia, No. (%) | 937 (62) | 460 (61) | 477 (63) |
| Total Cholesterol, mg/dL, mean (SD) | 176 (42) | 175 (42) | 177 (42) |
| Congestive heart failure, No. (%) | 416 (27) | 204 (27) | 212 (28) |
| Chronic renal failure, No. (%) | 96 (6.32) | 44 (5.81) | 52 (6.92) |
| Prior history of Afib, No. (%) | 114 (7.51) | 52 (6.92) | 62 (8.23) |
| COPD, No. (%) | 170 (11) | 80 (11) | 90 (12) |
| Prior PCI, No. (%) | 179 (12) | 80 (11) | 99 (13) |
| Cardiac surgery, No. (%) ‡ | |||
| CABG | 782 (52) | 378(50) | 404(54) |
| Valvular* | 756 (50) | 385 (51) | 371 (49) |
| Others | 274 (18) | 139 (18) | 135 (18) |
Abbreviations: OPERA, Omega-3 Fatty Acids for Prevention of Post-Operative Atrial Fibrillation trial; Afib, atrial fibrillation; PoAF, post-operative atrial fibrillation; BMI, body mass index; COPD, chronic obstructive pulmonary disease; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft surgery.
Numbers for each type of cardiac surgery are not mutually exclusive, as some patients underwent multiple procedures (e.g., CABG + valve surgery).
Valvular surgery performed include aortic (69%), mitral (26%), combination of aortic and mitral (4.0%), and others (1.2%).
The primary endpoint of a BARC type 4 or 5 bleeding event occurred in 92 patients (6.1%); TIMI major bleeding, in 73 patients (4.8%), TIMI minor bleeding, in 113 patients (7.5%), and ISTH surgical bleeding, in 99 patients (6.5%). Risk of bleeding was not higher in the fish oil group compared to placebo for any of these outcomes (Table 2). For example, comparing fish oil to placebo, the OR for BARC bleeding was 0.81 (95%CI= 0.53–1.24); absolute risk difference=1.1% lower (95% CI= −3.0 to 1.8%). The fish oil group had significantly fewer units of blood transfused compared to placebo (mean=1.61 vs 1.92, p<0.001), attributable to significantly lower requirements for blood transfusions both during (P=0.002) and after (P=0.006) surgery. No significant differences were identified in post-operative platelet counts, INR, PAI-1, or 11-dhTXB2 levels (Table S1).
Table 2.
Effect of fish oil supplementation on risk of peri-operative bleeding in 1516 patients undergoing cardiac surgery in the OPERA trial.
| Fish oil (n=758) |
Placebo (n=758) |
OR or RR† (95% CI) |
P value | |
|---|---|---|---|---|
| BARC type 4 or 5 bleeding, No (%) | 42 (5.51) | 50 (6.61) | 0.81 (0.53, 1.24) | 0.34 |
| TIMI major bleeding, No (%) | 31 (4.12) | 42 (5.51) | 0.71 (0.44, 1.14) | 0.16 |
| TIMI minor bleeding, No (%) | 54 (7.11) | 59 (7.81) | 0.89 (0.60, 1.30) | 0.55 |
| ISTH surgical bleeding, No (%) | 45 (5.92) | 54 (7.10) | 0.80 (0.53, 1.21) | 0.30 |
| 24-hr chest tube output, ml, median (IQR) | 388 (330) | 370 (300) | 0.48 | |
| Total units of blood transfused, mean (SD) | 1.61 (2.62) | 1.92 (3.33) | 0.83 (0.77, 0.90) | <0.001 |
| median (25th, 75th percentile) | 1.00 (0, 2.00) | 1.00 (0, 3.00) | ||
| Total units during surgery, mean (SD) | 0.80 (1.51) | 1.00 (1.80) | 0.84 (0.76, 0.94) | 0.002 |
| median (25th, 75th percentile) | 0 (0, 2.00) | 0 (0, 2.00) | ||
| Total units after surgery, mean (SD) | 0.81 (1.82) | 0.92 (2.13) | 0.85 (0.76, 0.95) | 0.006 |
| median (25th, 75th percentile) | 0 (0, 1.00) | 0 (0, 1.00) |
Abbreviations: OR, odds ratio; RR, rate ratio; CI, confidence interval; BARC, Bleeding Academic Research Consortium; IQR, interquartile range; SD, standard deviation;
The first four estimates are odds ratios; the remainder, rate ratios.
In exploratory subgroup analyses, results did not differ significantly in patient subgroups by age, gender, preoperative antithrombotic therapy, or cardiopulmonary bypass use (P-interaction=NS for each). In other subgroup analyses, the effect of fish oil on total unit of blood transfused appeared more pronounced in patients who underwent valve surgery, compared with CABG (P-interaction < 0.001) and in patients who underwent mini thoracotomy, compared with open thoracotomy (P-interaction = 0.001) (Table S2).
Evaluating objective biomarkers of plasma phospholipid omega-3 fatty acids, baseline levels associated with a non-significant trend towards lower bleeding risk (P-trend=0.05) (Table 3). Achieved levels of omega-3 fatty acids on the morning of cardiac surgery associated significantly with lower risk of bleeding, with 70% lower risk in the third quartile ((OR= 0.30 [95% CI, 0.11–0.78]) and 64% lower risk in the fourth quartile (0.36 [95% CI, 0.15–0.87]), compared with the lowest quartile (P-trend=0.01). Changes in plasma phospholipid omega-3 fatty acids from baseline to morning of surgery associated with a nonsignificant trend toward lower bleeding risk (P-trend=0.09). In restricted cubic spline analyses, there was little statistical evidence for nonlinearity in these relationships (P-nonlinearity≥0.05 each), although visual inspection suggested that the lower risk of bleeding might be less pronounced (although still with little evidence for increased bleeding risk) at highest omega-3 levels (Figure 1A-C).
Table 3.
Association between circulating plasma phospholipid omega-3 fatty acid levels and risk of BARC type 4 or 5 peri-operative bleeding in 564 patients undergoing cardiac surgery in the OPERA trial.
| Quartiles of plasma phospholipid omega-3 fatty acid levels† | P for trend‡ | ||||
|---|---|---|---|---|---|
| 1st | 2nd | 3rd | 4th | ||
| Baseline concentration | |||||
| % of fatty acids, mean ± SE | 3.25 ± 0.03 | 3.99 ± 0.02 | 4.79 ± 0.03 | 6.61 ± 0.11 | 0.05 |
| No. of cases/no. of patients | 19 / 142 | 11 / 140 | 12 / 141 | 11 / 141 | |
| Odds ratio (95% CI) | 1.00 (reference) | 0.54 (0.23, 1.31) | 0.49 (0.21, 1.13) | 0.42 (0.17, 1.02) | |
| Post-supplementation concentration on the morning of surgery | |||||
| % of fatty acids, mean ± SE | 3.61 ± 0.04 | 4.84 ± 0.03 | 6.00 ± 0.03 | 8.03 ± 0.10 | 0.01 |
| No. of cases/no. of patients | 19 / 139 | 14 / 136 | 8 / 138 | 11 / 137 | |
| Odds ratio (95% CI) | 1.00 (reference) | 0.58 (0.26, 1.3) | 0.30 (0.11, 0.78) | 0.36 (0.15, 0.87) | |
| Change in concentration from baseline to morning of surgery | |||||
| % of fatty acids, mean ± SE | −0.26 ± 0.06 | 0.32 ± 0.01 | 1.05 ± 0.03 | 2.77 ± 0.08 | 0.09 |
| No. of cases/no. of patients | 14 / 131 | 19 / 131 | 7 / 131 | 11 / 130 | |
| Odds ratio (95% CI) | 1.00 (reference) | 1.80 (0.79, 4.1) | 0.56 (0.21, 1.5) | 0.81 (0.32, 2.0) | |
Abbreviations: BARC, Bleeding Academic Research Consortium; CI, confidence interval; SE, standard error
omega-3=sum of EPA+DPA+DHA
Test of linear trend across quartiles was assessed by entering the quartile variable as a single ordinal variable in a multivariable-adjusted logistic regression
Figure 1.
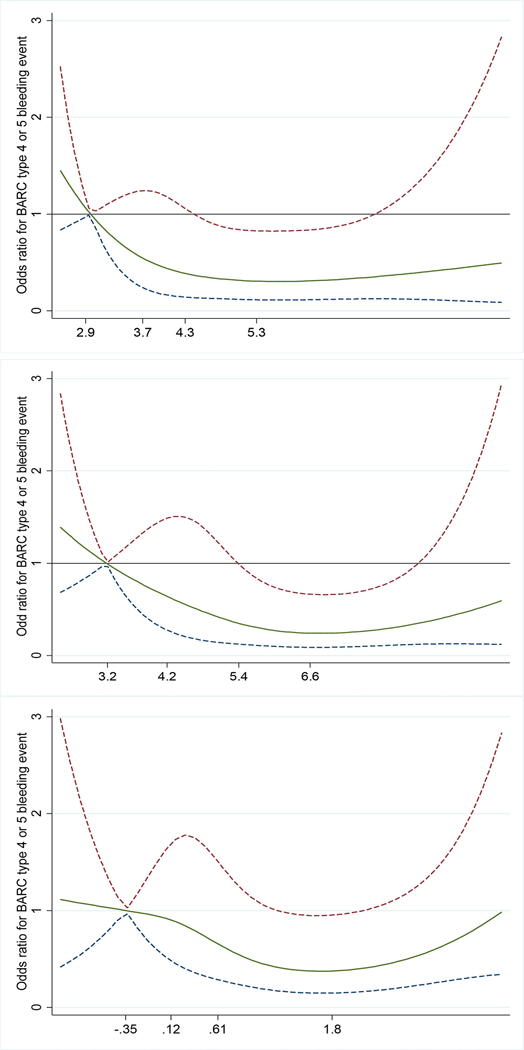
Multivariable-adjusted association between baseline (top panel), morning of surgery (middle panel), and change in (bottom panel) plasma phospholipid omega-3 fatty acids and risk of BARC type 4 or 5 peri-operative bleeding in 564 patients undergoing cardiac surgery in the OPERA trial. The solid green line and the dashed lines represent odds ratio and 95% CI respectively, in comparison to the reference level (5th percentile) representing the median value of the first decile. The values shown on the x‐axis correspond to the 5th, 25th, 50th, and 75th percentiles of plasma phospholipid omega-3 fatty acid levels. P value for nonlinearity= 0.15, 0.07, and 0.10, respectively; P value for linearity = 0.05, 0.01, and 0.09, respectively.
When we evaluated independent predictors of BARC type 4 or 5 bleeding, cardiopulmonary bypass use was the strongest predictor (OR=5.65, 95% CI=1.72–18), followed by valvular surgery (with or without concomitant CABG), preoperative antithrombotic therapy, female sex, and presence of diabetes (Figure 2).
Figure 2.
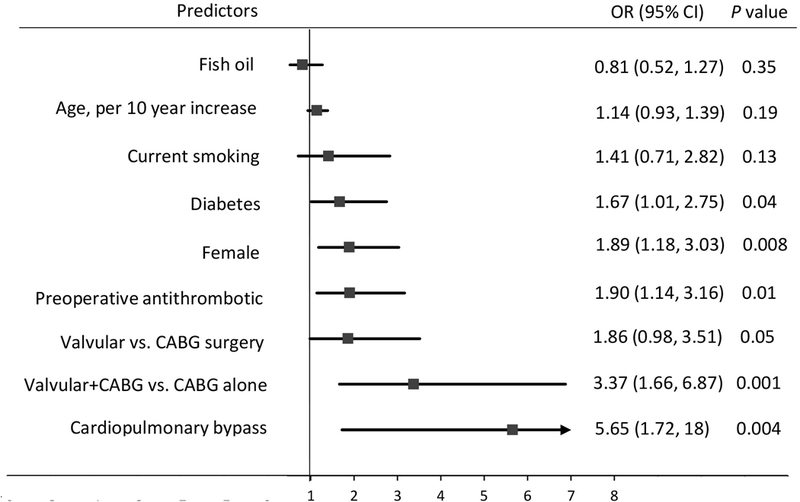
Variables retained in the selection model predicting a BARC type 4 or 5 peri-operative bleeding event in 1516 patients undergoing cardiac surgery in the OPERA trial. Randomized fish oil supplement use is retained in the model for comparison.
Minor adverse events related to fish oil use, such as gastrointestinal upset, burping, and fish oil taste, occurred more commonly in the fish oil group compared to placebo. Other serious adverse events were generally similar between the two groups (Table S3).
DISCUSSION
The OPERA trial was a multinational, placebo-controlled randomized trial that showed that fish oil supplementation does not decrease the incidence of postoperative atrial fibrillation in cardiac surgery patients. In this secondary analysis of OPERA, we showed that fish oil supplementation did not lead to increased peri-operative bleeding across multiple commonly used bleeding definitions. On the contrary, patients randomized to fish oil required fewer units of blood transfusions, compared to placebo. In addition, high achieved (post-supplementation) levels of plasma phospholipid omega-3 fatty acids– reflecting habitual levels plus additional incorporation due to fish oil supplementation – associated with lower risk of peri-operative bleeding.
Findings were similar across multiple patient subgroups, with none showing higher bleeding risk with fish oil supplementation. This was also true for subgroups experiencing increased absolute risk of peri-operative bleeding, such as for patients receiving cardiopulmonary bypass, valve surgery, and preoperative antithrombotic therapy. The broad recruitment criteria, multinational population, and consistent results across patient subgroups support generalizability of our findings. The beneficial effect of fish oil on total units of blood transfused was also apparent across subgroups. The potentially larger benefit among patients who underwent valve surgery, compared to CABG; and among those who had mini thoracotomy, compared to open thoracotomy; should be considered exploratory subgroup analyses and viewed with caution.
Omega-3 polyunsaturated fatty acids in fish oil lower blood triglycerides and improve cardiovascular hemodynamics and endothelial function.2 Numerous prospective observational studies and large randomized clinical trials have evaluated the clinical benefits of these fatty acids,30–32 and multiple randomized trials like REDUCE-IT and STRENGTH are ongoing.33, 34 While findings of more recent randomized trials have been inconsistent, meta-analyses suggest that omega-3 polyunsaturated fatty acids significantly reduce coronary heart disease mortality, including fatal myocardial infarction and sudden cardiac death, leading the American Heart Association to recommend fish oil supplementation to prevent CVD events in patients with prevalent coronary heart disease; and reduce mortality and hospitalizations in patients with heart failure with reduced ejection fraction.35 The US Food and Drug Administration has approved fish oil for the treatment of hypertriglyceridemia and also a qualified health claim that omega-3 fatty acids may reduce the risk of coronary heart disease.36 It is therefore unsurprising that 19 million American adults take fish oil daily.3
Yet, questions regarding a potential bleeding risk with fish oil use have persisted. An initial suggestion of potential bleeding risk was seen among Eskimos consuming high levels of omega-3 fatty acids from sea mammals,37 who had higher medically tested bleeding time compared to typical westerners as well as high levels of EPA and DHA in platelet lipids. Following these early results, several mechanistic studies of EPA and DHA and platelet function suggested diminished platelet aggregation, with a variety of proposed molecular mechanisms.37–43 These experimentally observed effects raised concern about a potential bleeding risk with fish oil supplements,8, 11 which has led many health care providers and organizations to request that patients should stop taking fish oil for at least one week before surgery.9, 10, 44, 45 This standard of practice can therefore delay patient care as well as increase hospital length of stay and cost. Yet, these recommendations, based on theoretical and mechanistic concerns, have not been supported by empiric evaluations of bleeding risk in clinical practice.
Few prior studies have suggested increased clinical bleeding related to fish oil use. Clarke and colleagues reported increased incidence of epistaxis in children treated for hypercholesterolemia,46 but this finding could not be reproduced in a similar study involving children on dialysis, who could have even higher absolute risk of bleeding.47, 48 Yokoyama and colleagues reported a higher rate of minor bleeding (fundal, subcutaneous and epistaxis) with EPA ethyl ester and statin (1.1%) versus statin alone (0.6%) in an adult Japanese cohort with hypercholesterolemia,49 speculated to be due to higher baseline levels of EPA among Japanese populations. 13 Yet, other large trials of fish oil in patients with hypercholesterolemia or at higher cardiovascular risk have not reported increased bleeding risk.12–16 Fewer trials, generally up to several hundred patients each, have evaluated bleeding risk with fish oil in patients undergoing major surgery, finding no significantly increased risk.15, 50, 51 However, none of these prior reports have assessed or reported a comprehensive range of bleeding endpoints. Our study, involving a large, diverse patient population undergoing various high risk cardiac surgical procedures, provides the most robust prospective evaluation to date of the effect of randomized fish oil supplementation on peri-operative bleeding.
Few prior studies have evaluated fish oil in relation to blood transfusion requirements. In a randomized controlled trial of 200 cardiac surgery patients who were randomized to fish oil vs placebo, Farquharson and colleagues reported reduced rate of red blood cell transfusion in the fish oil group compared to controls.50 In addition, there was a nonsignificant lower rate of major bleeding (defined as total blood loss >3 L through chest tube drains) and volume of blood loss in the fish oil group compared to controls. Together with our findings, these results suggest that fish oil could reduce blood transfusion requirements in patients undergoing cardiac surgery. This claim is further supported by the finding of an inverse association between achieved (post-supplementation) levels of plasma phospholipid omega-3 fatty acids and the risk of bleeding in our study. Similar inverse association was also reported by Del Brutto and colleagues who demonstrated a lower rate of cerebral microbleed among adults who consumed large amount of oily fish,52 concluding that fish oil supplementation may prevent incident cerebral microbleed among high-risk individuals. Although the exact mechanism for this beneficial effect of fish oil in patients undergoing surgery is unknown, previously described platelet-sparing effect of fish oil may potentially play a role. Acute inflammation and biochemical changes associated with components of cardiac surgery have been shown to lead to platelet activation and paradoxically increase loss of platelet function and increase bleeding risk. For example, platelets are known to be activated during cardiopulmonary bypass,53 resulting in both quantitative and qualitative platelet defects. Hence, it is not uncommon to use platelet-sparing medications to prevent hemorrhage during cardiopulmonary bypass. Fish oil may provide platelet-sparing effects similar to these medications and reduce bleeding and transfusion needs. Our findings therefore support the need for further experimental and clinical studies to test this hypothesis and evaluate relevant pathways.
Our investigation has several strengths. Notably, it is the largest study to-date to provide detailed evaluations of several standardized bleeding endpoints in a randomized controlled analysis. In addition, the broad inclusion criteria and multinational enrollment enhance the external validity of our findings. The consistently lower trend of bleeding endpoints in the fish oil group, compared to control, across multiple subgroups and similar to other prior smaller trials implies a reassuring robust conclusion from our result.
Potential limitations require consideration. While bleeding outcomes, including clinical bleeding and transfusion requirements, were prespecified safety endpoints of the OPERA trials, these findings should be considered as secondary analyses of the trial. Long-term effects of fish oil supplementation may differ from short-term effects. In this light, our analysis of the relationship between plasma phospholipid levels at enrollment with peri-operative bleeding may best reflect habitual/long-term dietary exposure and provide relevant findings for this question. The similar observed trend for lower peri-operative bleeding risk with higher omega-3 levels at both enrollment (baseline) and morning of surgery (post-supplementation) does not support any major difference between long- and short-term effects. OPERA was not specifically designed to test the effect of fish oil supplements on peri-operative bleeding. For example, it is possible that the identified lower bleeding risk is a chance finding. However, bleeding outcomes were prespecified safety endpoints, and the lower absolute risk of bleeding across multiple bleeding endpoints in the fish oil group provides strong evidence of at least no increased peri-operative bleeding risk with fish oil use.”. Lastly, this trial involved patients undergoing cardiac surgery, which may limit generalizability to other types of surgery. Yet, similar absence of bleeding risk has been reported in prior, smaller studies of patients undergoing other types of procedures.12, 54, 55
Few concerns over potential antiplatelet effect of oleic acid in olive oil (placebo in OPERA) has been alluded to,56, 57 which may raise the question of whether olive oil is a suitable control for this analysis. As found in prior systematic reviews of fish oil RCTS,31, 32 olive oil is a commonly used placebo. No prior studies have identified any molecular or clinical signal of bleeding risk with olive oil. In addition, the dose used in OPERA is so minor, compared to background intake, as to be unlikely to have a significant effect. Olive oil contains mainly oleic acid (up to 83%),58 a monounsaturated fatty acid commonly found in numerous vegetable oils and animal fats. 2 g/d of olive oil (i.e. ~1.6g of oleic acid) were provided as placebo in OPERA. In the U.S., mean monounsaturated fat intake is about 30 g/d.59 Hence, it is unlikely that adding an additional 1.6 g/d (5%) above background intake would have any meaningful effects. Furthermore, nearly half of the participants in OPERA trial were enrolled in Italy, a country where olive oil is an essential ingredient in their cuisine and where background intake would be even higher. We also found no significant difference when analysis was stratified by the 3 countries in OPERA. Thus, it seems unlikely that the use of olive oil as a placebo explains the findings.
In summary, in this large, multinational population of contemporary patients undergoing cardiac surgery, fish oil supplementation did not increase peri-operative bleeding; and reduced the number of peri-operative blood transfusions. Higher achieved omega-3 levels were associated with lower risk of bleeding. These novel findings support the need for mechanistic studies to elucidate potential mechanisms, such as platelet-sparing effects, as well as reconsideration of current recommendations to stop fish oil or delay procedures prior to cardiac surgery.
Supplementary Material
What is known
Fish oil is among the most commonly used natural supplements with associated cardiovascular benefits
Elective surgeries/procedures for patients taking fish oil tend to be delayed due to concern for theoretical bleeding risk associated with the potential antiplatelet effect of fish oil
Limited clinical evidence exists to change this practice
What the study adds
Our study provides the most robust evidence to-date that fish oil supplementation does not lead to increase peri-operative bleeding. Hence, surgeries/procedures should not be delayed for patients taking fish oil
A relatively novel finding that fish oil supplementation may reduce the number of blood transfusion after surgery merits further evaluation in future RCTs
Acknowledgments
Funding:
The parent OPERA trial was supported by the NIH (RC2-HL101816), GlaxoSmithKline, Sigma Tau, and Pronova BioPharma. No additional funding was received for this analysis and manuscript. The funders had no role in the design or conduct of this study; the collection, management, analysis, or interpretation of the data; or the preparation, review, or approval of the manuscript.
Footnotes
Disclosure: Dr. Mozaffarian reports honoraria or consulting from Astra Zeneca, Acasti Pharma, GOED, DSM, Haas Avocado Board, Nutrition Impact, Pollock Communications, Boston Heart Diagnostics, and Bunge; chapter royalties from UpToDate; and research funding from the National Institutes of Health and the Gates Foundation. Dr. Harris reports membership on Scientific Advisory Boards for Marine Ingredients and the Seafood Nutrition Partnership, and is the President of OmegaQuant, LLC, a laboratory that offers blood omega-3 testing. None of the other authors have any relevant disclosure.
REFERENCES
- 1.Lavie CJ, Milani RV, Mehra MR and Ventura HO. Omega-3 polyunsaturated fatty acids and cardiovascular diseases. Journal of the American College of Cardiology. 2009;54:585–94. [DOI] [PubMed] [Google Scholar]
- 2.Mozaffarian D and Wu JH. Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol. 2011;58:2047–67. [DOI] [PubMed] [Google Scholar]
- 3.Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002–2012 National health statistics reports; no 79. Hyattsville, MD: National Center for Health Statistics; 2015 [PMC free article] [PubMed] [Google Scholar]
- 4.Singh SR and Levine MA. Potential interactions between pharmaceuticals and natural health products in Canada. Journal of clinical pharmacology. 2007;47:249–58. [DOI] [PubMed] [Google Scholar]
- 5.Calder PC. Mechanisms of action of (n-3) fatty acids. The Journal of nutrition. 2012;142:592S–599S. [DOI] [PubMed] [Google Scholar]
- 6.McNamara D Fish Oil Supplements an Issue in Cardiac Surgery. https://www.mdedge.com/familypracticenews/article/30717/cardiology/fish-oil-supplements-issue-cardiac-surgery. 2010. Accessed on January 14, 2018
- 7.Bays HE. Safety considerations with omega-3 fatty acid therapy. The American journal of cardiology. 2007;99:35C–43C. [DOI] [PubMed] [Google Scholar]
- 8.Rowe DJ and Baker AC. Perioperative risks and benefits of herbal supplements in aesthetic surgery. Aesthetic surgery journal. 2009;29:150–7. [DOI] [PubMed] [Google Scholar]
- 9.Stanford Health Care. Preparing for Mohs Surgery. https://stanfordhealthcare.org/medical-treatments/m/mohs-micrographic-surgery/preparing-for-surgery.html. Accessed on January 14, 2018
- 10.University of Washington Medicine. Medications to Avoid Before Surgery. https://depts.washington.edu/anesth/care/anesthesiology/hmc/meds.shtml. Accessed on January 14, 2018
- 11.WebMD. Surgery Patients Unaware of Herbal Risks. http://www.webmd.com/drug-medication/news/20090416/surgery-patients-unaware-of-herbal-risk#1. Accessed on January 14, 2018
- 12.Harris WS. Expert opinion: omega-3 fatty acids and bleeding-cause for concern? The American journal of cardiology. 2007;99:44c–46c. [DOI] [PubMed] [Google Scholar]
- 13.Villani AM, Crotty M, Cleland LG, James MJ, Fraser RJ, Cobiac L and Miller MD. Fish oil administration in older adults with cardiovascular disease or cardiovascular risk factors: is there potential for adverse events? A systematic review of the literature. International journal of cardiology. 2013;168:4371–5. [DOI] [PubMed] [Google Scholar]
- 14.Thies F, Garry JM, Yaqoob P, Rerkasem K, Williams J, Shearman CP, Gallagher PJ, Calder PC and Grimble RF. Association of n-3 polyunsaturated fatty acids with stability of atherosclerotic plaques: a randomised controlled trial. Lancet (London, England). 2003;361:477–85. [DOI] [PubMed] [Google Scholar]
- 15.Eritsland J, Arnesen H, Gronseth K, Fjeld NB and Abdelnoor M. Effect of dietary supplementation with n-3 fatty acids on coronary artery bypass graft patency. Am J Cardiol. 1996;77:31–6. [DOI] [PubMed] [Google Scholar]
- 16.DeCaterina R, Giannessi D, Mazzone A, Bernini W, Lazzerini G, Maffei S, Cerri M, Salvatore L and Weksler B. Vascular prostacyclin is increased in patients ingesting omega-3 polyunsaturated fatty acids before coronary artery bypass graft surgery. Circulation. 1990;82:428–38. [DOI] [PubMed] [Google Scholar]
- 17.Mozaffarian D, Marchioli R, Macchia A, Silletta MG, Ferrazzi P, Gardner TJ, Latini R, Libby P, Lombardi F, O’Gara PT, Page RL, Tavazzi L, Tognoni G and Investigators O. Fish oil and postoperative atrial fibrillation: the Omega-3 Fatty Acids for Prevention of Post-operative Atrial Fibrillation (OPERA) randomized trial. JAMA. 2012;308:2001–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mozaffarian D, Marchioli R, Gardner T, Ferrazzi P, O’Gara P, Latini R, Libby P, Lombardi F, Macchia A, Page R, Santini M, Tavazzi L and Tognoni G. The omega-3 Fatty Acids for Prevention of Post-Operative Atrial Fibrillation trial--rationale and design. American heart journal. 2011;162:56–63 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu JH, Marchioli R, Silletta MG, Macchia A, Song X, Siscovick DS, Harris WS, Masson S, Latini R, Albert C, Brown NJ, Lamarra M, Favaloro RR and Mozaffarian D. Plasma phospholipid omega-3 fatty acids and incidence of postoperative atrial fibrillation in the OPERA trial. Journal of the American Heart Association. 2013;2:e000397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, Kaul S, Wiviott SD, Menon V, Nikolsky E, Serebruany V, Valgimigli M, Vranckx P, Taggart D, Sabik JF, Cutlip DE, Krucoff MW, Ohman EM, Steg PG and White H. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123:2736–47. [DOI] [PubMed] [Google Scholar]
- 21.Morrow JD and Minton TA. Improved assay for the quantification of 11-dehydrothromboxane B2 by gas chromatography-mass spectrometry. Journal of chromatography. 1993;612:179–85. [DOI] [PubMed] [Google Scholar]
- 22.Kahan BC and Morris TP. Improper analysis of trials randomised using stratified blocks or minimisation. Statistics in medicine. 2012;31:328–40. [DOI] [PubMed] [Google Scholar]
- 23.Akintoye E, Wu JH, Hou T, Song X, Yang J, Hammock B and Mozaffarian D. Effect of fish oil on monoepoxides derived from fatty acids during cardiac surgery. Journal of lipid research. 2016;57:492–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dial S, Delabays E, Albert M, Gonzalez A, Camarda J, Law A and Menzies D. Hemodilution and surgical hemostasis contribute significantly to transfusion requirements in patients undergoing coronary artery bypass. The Journal of thoracic and cardiovascular surgery. 2005;130:654–61. [DOI] [PubMed] [Google Scholar]
- 25.McDonald SB, Renna M, Spitznagel EL, Avidan M, Hogue CW Jr, Moon MR, Barzilai B, Saleem R, McDonald JMand Despotis GJ. Preoperative use of enoxaparin increases the risk of postoperative bleeding and re-exploration in cardiac surgery patients. Journal of cardiothoracic and vascular anesthesia. 2005;19:4–10. [DOI] [PubMed] [Google Scholar]
- 26.Nuttall GA, Erchul DT, Haight TJ, Ringhofer SN, Miller TL, Oliver WC, Zehr KJand Schroeder DR. A comparison of bleeding and transfusion in patients who undergo coronary artery bypass grafting via sternotomy with and without cardiopulmonary bypass. Journal of cardiothoracic and vascular anesthesia. 2003;17:447–51. [DOI] [PubMed] [Google Scholar]
- 27.Ray JG, Deniz S, Olivieri A, Pollex E, Vermeulen MJ, Alexander KS, Cain DJ, Cybulsky I and Hamielec CM. Increased blood product use among coronary artery bypass patients prescribed preoperative aspirin and clopidogrel. BMC cardiovascular disorders. 2003;3:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Magovern JA, Sakert T, Benckart DH, Burkholder JA, Liebler GA, Magovern GJ Sr. and Magovern GJ Jr. A model for predicting transfusion after coronary artery bypass grafting. The Annals of thoracic surgery. 1996;61:27–32. [DOI] [PubMed] [Google Scholar]
- 29.Moskowitz DM, Klein JJ, Shander A, Cousineau KM, Goldweit RS, Bodian C, Perelman SI, Kang H, Fink DA, Rothman HC and Ergin MA. Predictors of transfusion requirements for cardiac surgical procedures at a blood conservation center. The Annals of thoracic surgery. 2004;77:626–34. [DOI] [PubMed] [Google Scholar]
- 30.Mozaffarian D and Rimm EB. Fish intake, contaminants, and human health: evaluating the risks and the benefits. Jama. 2006;296:1885–99. [DOI] [PubMed] [Google Scholar]
- 31.Leon H, Shibata MC, Sivakumaran S, Dorgan M, Chatterley T and Tsuyuki RT. Effect of fish oil on arrhythmias and mortality: systematic review. BMJ (Clinical research ed). 2008;337:a2931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marik PE and Varon J. Omega-3 dietary supplements and the risk of cardiovascular events: a systematic review. Clinical cardiology. 2009;32:365–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bhatt DL, Steg PG, Brinton EA, Jacobson TA, Miller M, Tardif JC, Ketchum SB, Doyle RT Jr, Murphy SA, Soni PN, Braeckman RA, Juliano RA, Ballantyne CM; REDUCE-IT Investigators. Rationale and design of REDUCE-IT: Reduction of Cardiovascular Events with Icosapent Ethyl-Intervention Trial. Clin Cardiol. 2017 Mar;40(3):138–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nissen S, Lincoff M, Nicholls S. Outcomes Study to Assess STatin Residual Risk Reduction With EpaNova in HiGh CV Risk PatienTs With Hypertriglyceridemia (STRENGTH). https://clinicaltrialsgov/ct2/show/NCT02104817. Accessed on January 14, 2018
- 35.Siscovick DS, Barringer TA, Fretts AM, Wu JH, Lichtenstein AH, Costello RB, Kris-Etherton PM, Jacobson TA, Engler MB, Alger HM, Appel LJ and Mozaffarian D. Omega-3 Polyunsaturated Fatty Acid (Fish Oil) Supplementation and the Prevention of Clinical Cardiovascular Disease: A Science Advisory From the American Heart Association. Circulation. 2017;135:e867–e884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.U.S. Food and Drug Administration. Summary of qualified health claims subject to enforcement discretion. 2014. https://www.fda.gov/Food/LabelingNutrition/ucm073992.htm. Accessed on January 14, 2018
- 37.Dyerberg J and Bang HO. Haemostatic function and platelet polyunsaturated fatty acids in Eskimos. Lancet (London, England). 1979;2:433–5. [DOI] [PubMed] [Google Scholar]
- 38.Knapp HR. Dietary fatty acids in human thrombosis and hemostasis. The American journal of clinical nutrition. 1997;65:1687s–1698s. [DOI] [PubMed] [Google Scholar]
- 39.Siess W, Roth P, Scherer B, Kurzmann I, Bohlig B and Weber PC. Platelet-membrane fatty acids, platelet aggregation, and thromboxane formation during a mackerel diet. Lancet. 1980;1:441–4. [DOI] [PubMed] [Google Scholar]
- 40.Bradlow BA, Chetty N, van der Westhuyzen J, Mendelsohn D and Gibson JE. The effects of a mixed fish diet on platelet function, fatty acids and serum lipids. Thrombosis research. 1983;29:561–8. [DOI] [PubMed] [Google Scholar]
- 41.Driss F, Vericel E, Lagarde M, Dechavanne M and Darcet P. Inhibition of platelet aggregation and thromboxane synthesis after intake of small amount of icosapentaenoic acid. Thromb Res. 1984;36:389–96. [DOI] [PubMed] [Google Scholar]
- 42.Lorenz R, Spengler U, Fischer S, Duhm J and Weber PC. Platelet function, thromboxane formation and blood pressure control during supplementation of the Western diet with cod liver oil. Circulation. 1983;67:504–11. [DOI] [PubMed] [Google Scholar]
- 43.El-Gendy AA and Abbas AM. Effect of omega-3 fatty acids on haemostatic functions in urocortin-treated obese rats. Journal of physiology and biochemistry. 2014;70:809–20. [DOI] [PubMed] [Google Scholar]
- 44.Entrust Medical group. Medications to avoid before surgery. http://www.entrustmd.com/webdocuments/medications-to-avoid-binder.pdf. Accessed on January 14, 2018
- 45.Health Sciences Institute. These excellent supplements need to be sidelined before surgery. http://hsionline.com/2013/10/07/the-most-dangerous-supplements/. Accessed on January 14, 2018
- 46.Clarke JT, Cullen-Dean G, Regelink E, Chan L and Rose V. Increased incidence of epistaxis in adolescents with familial hypercholesterolemia treated with fish oil. The Journal of pediatrics. 1990;116:139–41. [DOI] [PubMed] [Google Scholar]
- 47.Goren A, Stankiewicz H, Goldstein R and Drukker A. Fish oil treatment of hyperlipidemia in children and adolescents receiving renal replacement therapy. Pediatrics. 1991;88:265–8. [PubMed] [Google Scholar]
- 48.Janssen MJ and van der Meulen J. The bleeding risk in chronic haemodialysis: preventive strategies in high-risk patients. The Netherlands journal of medicine. 1996;48:198–207. [DOI] [PubMed] [Google Scholar]
- 49.Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, Oikawa S, Sasaki J, Hishida H, Itakura H, Kita T, Kitabatake A, Nakaya N, Sakata T, Shimada K and Shirato K. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet (London, England). 2007;369:1090–8. [DOI] [PubMed] [Google Scholar]
- 50.Farquharson AL, Metcalf RG, Sanders P, Stuklis R, Edwards JR, Gibson RA, Cleland LG, Sullivan TR, James MJ and Young GD. Effect of dietary fish oil on atrial fibrillation after cardiac surgery. The American journal of cardiology. 2011;108:851–6. [DOI] [PubMed] [Google Scholar]
- 51.Metcalf RG, James MJ, Gibson RA, Edwards JR, Stubberfield J, Stuklis R, Roberts-Thomson K, Young GD and Cleland LG. Effects of fish-oil supplementation on myocardial fatty acids in humans. The American journal of clinical nutrition. 2007;85:1222–8. [DOI] [PubMed] [Google Scholar]
- 52.Del Brutto OH, Mera RM, Ha JE, Del Brutto VJ, Castillo PR, Zambrano M and Gillman J. Oily fish consumption is inversely correlated with cerebral microbleeds in community-dwelling older adults: results from the Atahualpa Project. Aging clinical and experimental research. 2016;28:737–43. [DOI] [PubMed] [Google Scholar]
- 53.Weerasinghe A and Taylor KM. The platelet in cardiopulmonary bypass. The Annals of thoracic surgery. 1998;66:2145–52. [DOI] [PubMed] [Google Scholar]
- 54.Kepler CK, Huang RC, Meredith D, Kim JH and Sharma AK. Omega-3 and fish oil supplements do not cause increased bleeding during spinal decompression surgery. Journal of spinal disorders & techniques. 2012;25:129–32. [DOI] [PubMed] [Google Scholar]
- 55.Meredith DS, Kepler CK, Huang RC, Hirsch B, Nguyen J, Farmer JC, Girardi FP, O’Leary PF and Cammisa FP. The effect of omega-3 fatty-acid supplements on perioperative bleeding following posterior spinal arthrodesis. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2012;21:2659–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nunez D, Randon J, Gandhi C, Siafaka-Kapadai A, Olson MS and Hanahan DJ. The inhibition of platelet-activating factor-induced platelet activation by oleic acid is associated with a decrease in polyphosphoinositide metabolism. The Journal of biological chemistry. 1990;265:18330–8. [PubMed] [Google Scholar]
- 57.Barradasa MA, Christofides JA, Jeremya JY, Mikhailidisa DP, D.E.Fry and P.Dandona. The effect of olive oil supplementation on human platelet function, serum cholesterol-related variables and plasma fibrinogen concentrations: A pilot study. Nutrition Research. 10 403–411. [Google Scholar]
- 58.The Olive Oil Source. Chemical characteristics of olive oil. https://www.oliveoilsource.com/page/chemical-characteristics. Accessed on January 14, 2018
- 59.Ervin RB, Wright JD, Wang CY and Kennedy-Stephenson J. Dietary intake of fats and fatty acids for the United States population: 1999–2000. Advance data. 2004:1–6. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


