Summary
Background
Police kill more than 300 black Americans—at least a quarter of them unarmed—each year in the USA. These events might have spillover effects on the mental health of people not directly affected.
Methods
In this population-based, quasi-experimental study, we combined novel data on police killings with individual-level data from the nationally representative 2013–15 US Behavioral Risk Factor Surveillance System (BRFSS) to estimate the causal impact of police killings of unarmed black Americans on self-reported mental health of other black American adults in the US general population. The primary exposure was the number of police killings of unarmed black Americans occurring in the 3 months prior to the BRFSS interview within the same state. The primary outcome was the number of days in the previous month in which the respondent’s mental health was reported as “not good”. We estimated difference-in-differences regression models—adjusting for state-month, month-year, and interview-day fixed effects, as well as age, sex, and educational attainment. We additionally assessed the timing of effects, the specificity of the effects to black Americans, and the robustness of our findings.
Findings
38 993 (weighted sample share 49%) of 103 710 black American respondents were exposed to one or more police killings of unarmed black Americans in their state of residence in the 3 months prior to the survey. Each additional police killing of an unarmed black American was associated with 0·14 additional poor mental health days (95% CI 0·07–0·22; p=0·00047) among black American respondents. The largest effects on mental health occurred in the 1–2 months after exposure, with no significant effects estimated for respondents interviewed before police killings (falsification test). Mental health impacts were not observed among white respondents and resulted only from police killings of unarmed black Americans (not unarmed white Americans or armed black Americans).
Interpretation
Police killings of unarmed black Americans have adverse effects on mental health among black American adults in the general population. Programmes should be implemented to decrease the frequency of police killings and to mitigate adverse mental health effects within communities when such killings do occur.
Funding
Robert Wood Johnson Foundation and National Institutes of Health.
Introduction
Public awareness of police killings of unarmed black Americans has been galvanised by the high-profile deaths of Oscar Grant, Michael Brown, Eric Garner, Walter Scott, Freddie Gray, and Stephon Clark, among others. Black Americans are nearly three times more likely than are white Americans to be killed by police—accounting for more than 40% of victims of all police killings nationwide—and five times more likely than are white Americans to be killed unarmed.1–3
Beyond the immediate consequences for victims and their families, police killings might also affect the mental health of people not directly connected to the killings or to the people involved. Racism, like trauma, can be experienced vicariously.4,5 Police killings of unarmed black Americans might compromise mental health among other black Americans through various mechanisms, including heightened perceptions of systemic racism and lack of fairness,6 loss of social status and self-regard,7 increased fear of victimisation and greater mortality expectations,8 increased vigilance,9 diminished trust in social institutions,10 reactions of anger, activation of prior traumas, and communal bereavement.11
A large literature has shown associations between racism and health outcomes,7,9,12,13 emphasising the pathogenic roles of discrimination and differential access to socioeconomic opportunities.14 However, a causal link between racism and health outcomes has been difficult to show. Police killings of unarmed black Americans have been interpreted by many as an expression of “structural racism”,15–18 defined by Bailey and colleagues as “the ways in which societies foster [racial] discrimination, via mutually reinforcing [inequitable] systems that in turn reinforce discriminatory beliefs, values, and distribution of resources”.14 Police violence disproportionately wielded against black Americans has been linked in part to the ways officers are trained, methods of identifying and engaging suspects, and uneven enforcement and punishment.19–21 Negative interactions with police have been associated with worse mental health among black men.22 Descriptive studies suggest an elevated prevalence of depression and post-traumatic stress disorder among black Americans living in communities where specific police killings of unarmed black Americans have occurred.23,24 Anecdotal evidence from traditional and social media suggests adverse mental health impacts in the wake of these events. However, the population-level health impacts of police killings have not been quantified in nationally representative data.
Our study aims to fill this gap. We estimated the impact of police killings of unarmed black Americans on self-reported mental health of black American adults in the US general population. We used newly released data on police killings combined with nationally representative survey data from 2013 to 2015. We employed a quasi-experimental design that leveraged state and temporal variation in police killings of unarmed black Americans to estimate causal effects.
Methods
Data sources and measures
We obtained data on respondents from the US Behavioral Risk Factor Surveillance System (BRFSS), a nationally representative, telephone-based, random digit dial survey of non-institutionalised adults aged 18 years and older. We used self-reported race to identify black American respondents. We also extracted information on res pondent sex, age, and educational attainment. We used the 2013–15 BRFSS to match available data on the timing of police killings. We note that some respondents in the 2015 BRFSS sample were in fact interviewed in early 2016.
Data on police killings were obtained from the Mapping Police Violence (MPV) database, which has tracked police killings in the USA since 2013.2 The MPV database draws from several media and crowd-sourced databases for police killings, which helps to address concerns about under-reporting in government statistics.25 Suspected killings are cross-checked against police and criminal records, social media, and obituaries. The database includes information on age, race, and sex of the victim; whether the victim was armed (with any weapon that could be used to harm or kill others); and location of the killing. We used data from the MPV database up to and including 2016 to better quantify the numbers of police killings occurring both before and after the BRFSS interview dates.
Exposures
The primary exposure was the number of police killings of unarmed black Americans occurring in the 3 months prior to the exact date of the BRFSS interview in the same state. BRFSS respondents were defined as exposed on the basis of their state of residence and the interview date. Thus, this exposure definition combines a range of potential exposure mechanisms including word of mouth and stories in print, radio, television, and social media. State of residence was used to define the exposure for several reasons. First, it is the smallest geographical area identified in the public-use BRFSS data files. Second, Google search frequencies of victims’ names from recent high-profile police killings of unarmed black Americans suggest that these events have their greatest salience in the state media markets in which they occur (appendix p 4). Third, ex6isting literature shows a strong relationship between state-level measures of racism and police killings of unarmed black Americans.16 Fourth, police killings might be seen to reflect local police–community relationships and state legal environments. Behavioural responses to police violence correlate strongly with locally reported cases.26
We also constructed a binary exposure variable equal to one if there had been one or more police killings of unarmed black Americans in the same state during the 3 months prior to the BRFSS interview (vs none). Finally, to more precisely elucidate the timing of the effects on mental health, we defined a series of exposure variables representing the number of police killings of unarmed black Americans in the same state in each of the 6 months preceding and after the BRFSS interview date.
Outcomes
The primary outcome was the number of days in the previous month in which the respondent’s mental health was reported as “not good”. The specific question from the BFRSS used to measure respondents’ mental health was worded as follows: “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” This survey item has been shown to have a high degree of internal validity, construct validity, criterion-related validity, and test-retest reliability, and is widely used to monitor trends in population mental morbidity.27 We also considered two secondary outcomes: whether or not an individual reported at least 1 day of poor mental health (vs none) and whether or not an individual reported 14 or more days of poor mental health (vs less than 14 days) in the prior month. The latter measure has been widely used to quantify the population prevalence of frequent mental distress because it correlates with severe mental health conditions.27
Statistical analysis
To estimate the effect of police killings of unarmed black Americans on self-reported mental health in the general population of black American adults, we fit difference-in-differences multivariable regression models specifying the number of poor mental health days as the outcome variable and the number of police killings of unarmed black Americans in the 3 months prior to interview as the primary exposure of interest. We estimated least-squares regression models for the primary outcome and report regression coefficients, which are interpretable as rate differences. We also estimated robust Poisson models for the primary and secondary outcomes, with the exponentiated regression coefficients interpretable as relative rates and risks,28 respectively. In all models, we adjusted for year-month fixed effects to account for national secular trends in the outcome; state-month fixed effects to account for time-invariant state-level confounders and state-specific seasonality in mental health; day-of-week fixed effects; and individual-level age group (ranging from 18–24 years to 80 years and older in 5-year intervals), sex, and level of education fixed effects. We also estimated models replacing the 3-month exposure variable with the binary measure of any police killing of an unarmed black American in the past 3 months. Further details on our methods are provided in the appendix (pp 2–3).
Our models compare the mental health of black Americans surveyed after a police killing of an unarmed black American in the same state with the mental health of black Americans residing in the same state but surveyed before that event or more than 3 months after the event, adjusting for state-specific seasonal patterns in mental health and for temporal trends in mental health of black Americans living in other states. The causal identifying assumptions in our strategy are (1) no endogenous selection into the sample—ie, the timing of the BRFSS interview and participation in the interview were random relative to the timing of police killings, an assumption supported by the random-digit-dial approach to sampling and by our investigation of differential participation following police killings; and (2) unconfoundedness—ie, police killings did not coincide with other factors that could influence mental health. After including state-month and year-month fixed effects, the only unobserved confounders that could remain would be factors that varied at the state-year-month level and whose timing was correlated with police killings and mental health in ways that deviated from normal state-specific seasonal patterns. The unconfoundedness assumption is supported by the quasi-random timing of specific police killings. To the extent that these assumptions are satisfied—which we explored in several sensitivity analyses—our estimates can be interpreted as causal effects.29
We note that our analysis defines as exposed any person living in the state where the police killing occurred, including some people who might not have been substantively exposed to the police killing (or even aware of it). Our causal estimates therefore have an intention-to-treat interpretation, similar to a randomised trial with non-compliance to treatment assignment. Our models capture the aggregate population-level effect, but probably underestimate the effect of police killings on the mental health of subpopulations most directly exposed.
All models were estimated using standard BRFSS survey weights to account for survey design and differential non-response. The overall response rate of the BRFSS ranges between 40% and 45% each year, which is comparable to, if not higher than, other large population-repre6sentative telephone surveys in the USA. We computed heteroscedasticity-robust SEs corrected for clustering at the state level. Clustered SEs adjust for spatial and temporal error correlation among respondents within the same state. We also calculated alternate SEs and p values using the wild cluster bootstrap-t meth od, which addresses the potential for over-rejection of the null hypothesis when the number of cluster units is small.30
We conducted four sensitivity analyses to assess the assumptions needed to infer causality in our model. First, to investigate the possibility of residual confounding, we estimated models replacing the 3-month exposure variable with 12 count variables denoting exposures in each of the 6 months before and after interview. This model allows a prespecified falsification test: if there were unobserved confounders at the state-year-month level, then we would expect the changes in mental health to sometimes precede the actual killing of an unarmed black American, given that there is randomness in the specific timing of these events. Second, we estimated models that additionally included state-year fixed effects or census division-month-year fixed effects (census divisions represent nine geographical regions accounting for the 50 US states). These additional models adjusted for state-specific year-on-year secular trends (eg, worsening crime) and regional shocks (eg, time-limited weather events), respectively, ruling out additional classes of potential confounders. Third, to assess the potential for bias due to non-random participation in BRFSS as a function of exposure to police killings, we re-fit the regression models specifying individual-level demographic characteristics (respondent sex, age, and educational attainment) as the dependent variables. Fourth, we estimated models that additionally included a measure of participant income (which was reported by only 85% of participants).
To assess the specificity of our findings to black Americans, we estimated the effects of police killings of unarmed black Americans on the mental health of white respondents. We also estimated the effects of police killings of armed black Americans and unarmed white Americans on the mental health of both black and white respondents. These analyses help to elucidate the mechanisms accounting for our findings. If police killings of unarmed black Americans affected the mental health of other black Americans through heightened perceptions of structural racism, activation of prior traumas, or through racial identification with the deceased, then we would expect no effect on the mental health of white Americans, nor in any of the cross-race analyses. By contrast, if police killings of unarmed white or black Americans were broadly interpreted as signals of general threats to personal safety, we would expect meaningful cross-race effects of these exposures. Although police killings of armed victims could affect mental health via communal bereavement, these killings are less likely to be perceived as unjustified and we expected little effect on mental health. We did not ex ante specify models examining the consequences of police killings of armed white Americans because our intent was to assess the sensitivity of our findings to changes in the race or armed status of the victim, holding fixed at least one of these attributes. These specifications provide the sharpest, most stringent test of whether killings of black, unarmed victims have specific salience to health outcomes.
Finally, we conducted two additional analyses to guide interpretation of the results. First, we estimated models differentiating between exposure to one police killing versus exposure to two or more. These models help to distinguish between threshold-related versus dose-related consequences of these events. Second, we used subgroup analyses to investigate whether the estimated mental health impacts were confined to a particular subset of black Americans. We stratified the estimates by sex (male or female), age (18–34 years, 35–49 years, 50–64 years, or 65 years and older), education (less than high school, high school graduate, or at least some college), and household income (above and below the sample median: <US$35 000 or ≥$35 000), and tested the null hypotheses that the estimated effects were the same in each subgroup. Unlike our primary specifications, these analyses were not based on a-priori hypotheses and therefore should be regarded as hypothesis-generating exercises. Statistical power to detect meaningful differences across subgroups was limited by sample size.
Data sharing
Replication data and code for our models are available from Harvard Dataverse.
Role of the funding source
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Our final sample included 103 710 black Americans interviewed in the 2013–15 BRFSS, whose mean age was 44·9 years (SD 17·3). After accounting for BRFSS sample weights, approximately half of respondents were women, and half had completed university (table 1). Respondents experienced on average 4·1 days of poor mental health in the month prior to interview; only 2348 (2·42%) survey respondents, who were excluded from the final sample, responded “don’t know” or did not answer this question. 38 993 (weighted sample share 49%) respondents were interviewed 0–3 months after at least one police killing of an unarmed black American in the same state. Respondents were exposed to an average of one police killing of an unarmed black American (range 0–7) in the 3 months prior to interview, or four killings per year (table 1). A map of police killings of unarmed black Americans by state during the study period is shown in the appendix (p 5), with descriptive statistics of the victims in table 2.
Table 1:
Descriptive statistics for black Americans in the 2013–15 BRFSS
| Characteristics | |
|---|---|
| Primary outcome* | |
| Days of poor mental health | 4·1 (8·4, 0–30) |
| Secondary outcomes* | |
| Any poor mental health days | 37 858 (35%) |
| Frequent mental distress† | 12 714 (13%) |
| Exposure‡ | |
| Number of police killings of unarmed black Americans | 1·0 (1·3, 0–7) |
| Any police killings of unarmed black Americans | 38 993 (49%) |
| Covariates | |
| Sex | |
| Female | 67 683 (54%) |
| Male | 36 027 (46%) |
| Age group§ | |
| 18–34 years | 18 093 (33%) |
| 35–64 years | 56 640 (52%) |
| ≥65 years | 27 705 (14%) |
| Completed college or above | 56 341 (51%) |
Data are n (%) or mean (SD, range), where the absolute number (n) refers to the actual number of observations and the percentages refer to the weighted estimates calculated using the BRFSS survey weights. All outcomes were assessed on the 103 710 black American respondents in the 2013–15 US BRFSS. For binary variables (both secondary outcomes, any police killings of unarmed black Americans, sex, age group, and college completion), percentages reflect the sample proportions computed using BRFSS sampling weights. BRFSS=Behavioral Risk Factor Surveillance System.
Outcomes are measured in the 30 days before the interview date.
14 or more days of poor mental health.
All exposures are in the 3 months prior to interview date in the same state as the respondent.
1272 (1%) respondents were categorised as not responding or answered “don’t know”.
Table 2:
Police killings in the MPV database, 2013–16
| Black American | White American | |
|---|---|---|
| Victim reported as unarmed | ||
| Total | 303 | 330 |
| Age, years | 32·4 (11–6) | 38·2 (15–4) |
| Gender | ||
| Female | 25 (8%) | 44 (13%) |
| Male | 278 (92%) | 286 (87%) |
| Victim reported as armed | ||
| Total | 753 | 1426 |
| Age, years | 32·1 (12·1) | 40·2 (13·8) |
| Gender* | ||
| Female | 24 (3%) | 79 (5%) |
| Male | 729 (97%) | 1346 (94%) |
Data are n, n (%), and mean (SD). Data were accessed on May 5, 2017. There were 4358 total police killings from Jan 1, 2013, to Oct 3, 2016; of these, 3116 were of white or black Americans. Data presented here exclude police killings of victims whose armed status was unknown. MPV=Mapping Police Violence.
There was one police killing of an allegedly armed transgender victim who was white.
For the primary outcome, each additional police killing of an unarmed black American in the respondent’s state of residence in the 3 months prior to interview was associated with a 0·14 day (95% CI 0·067–0·22; p=0·00047) increase in the number of poor mental health days, representing a relative increase of 3·3% (1·6–5·1; p=0·00011) at the population level (table 3). Exposure to one or more police killings was associated with a 0·35 day (0·03–0·67; p=0·032) increase in poor mental health days. Exposure to police killings was associated with significant increases in both secondary outcomes (table 3).
Table 3:
Exposure to police killings of unarmed black Americans and poor mental health days among black Americans: regression estimates
| Primary outcome | Secondary outcomes | |||
|---|---|---|---|---|
| Poor mental health days (OLS, rate difference) | Poor mental health days (Poisson, rate ratio) | Any poor mental health days (Poisson, risk ratio) | Frequent mental distress* (Poisson, risk ratio) | |
| Number of police killings of unarmed black Americans† | 0·14 (0·07–0·22) | 1·033 (1·016–1·051) | 1·022 (1·008–1·036) | 1·036 (1·007–1·068) |
| p value | 0·00047 | 0·00011 | 0·0018 | 0·016 |
| Wild cluster bootstrap-t p value‡ | <0·0001 | <0·0001 | <0·0001 | <0·0001 |
| Any police killings of unarmed black Americans (vs none)† | 0·35 (0·03–0·67) | 1·087 (1·006–1·174) | 1·055 (1·007–1·106) | 1·106 (0·986–1·240) |
| p value | 0·032 | 0·035 | 0·024 | 0·085 |
| Wild cluster bootstrap-t p value | <0·0001 | <0·0001 | <0·0001 | 0·039 |
Data are regression estimates (95% CI). All outcomes were assessed on the 103 710 black American respondents in the 2013–15 US Behavioral Risk Factor Surveillance System. Separate regressions were done for the two exposures (number of killings and any killings); additionally, each column represents a separate regression. 95% CIs are corrected for clustering at the state level. All models were adjusted for respondent sex, age group, and level of education; and state-survey month, survey year-survey month, and survey day of week fixed effects. OLS=ordinary least squares.
Defined as 14 days or more of poor mental in the past 30 days.
Exposures are measured in the 30 days before the interview date.
Wild cluster bootstrap-t p values account for potential underestimates of SEs when the number of clusters is small. These were estimated on least-squares (ie, linear probability model) versions of the models listed because they cannot be applied to non-linear estimators (eg, Poisson).
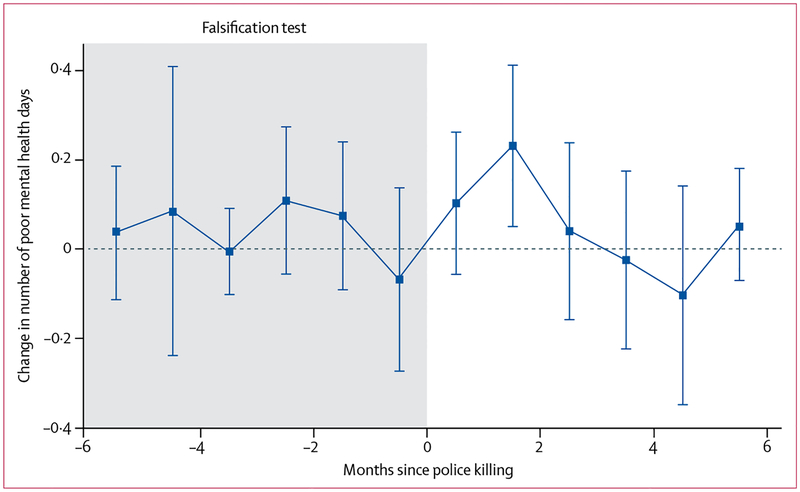
With respect to the timing of effects, increases in the primary outcome were observed in the 2 months after exposures to police killings of unarmed black Americans (figure 1). The largest estimate corresponds to police killings that occurred 30–60 days prior to the interview: each additional police killing during this time window was associated with 0·23 more days of poor mental health (95% CI 0·05 to 0·41; p=0·014). Within the first month after a killing (during which, on average, only half of the 30-day recall period occurred after the exposure), respondents reported 0·10 additional days (−0·06 to 0·26; p=0·20) of poor mental health per each additional killing. There were neither substantively nor statistically significant associations between police killings of unarmed black Americans and the mental health of black respondents interviewed 3–6 months after the police killing, nor with the mental health of the respondents interviewed in the 6 months prior to the police killing (falsification test; figure 1).
Figure 1: Changes in the number of poor mental health days in the 6 months before and after exposure to police killings of unarmed black Americans.
The figure displays coefficients for the association between the number of police killings of unarmed black Americans (in the same state as the respondents) and the mental health of black respondents 6 months on either side of the shooting. Vertical bars indicate 95% CIs. Estimates in the shaded region represent the impacts of a police killing on mental health outcomes assessed within the 6 months before the police killing event (ie, falsification test).
The findings were unchanged with further adjustment for income, state-year fixed effects, or census division-month-year fixed effects (appendix p 6). We found no evidence of differential selection into the sample by exposure to police killings (appendix p 7). Coefficient estimates were similar in magnitude for exposure to one police killing versus two or more (appendix p 8).
In subgroup analyses, point estimates were similar across sex and income groups. Larger associations were estimated for individuals aged 50–65 years and for those with less than high school education, but differences across age and education subgroups were not statistically significant (appendix p 9).
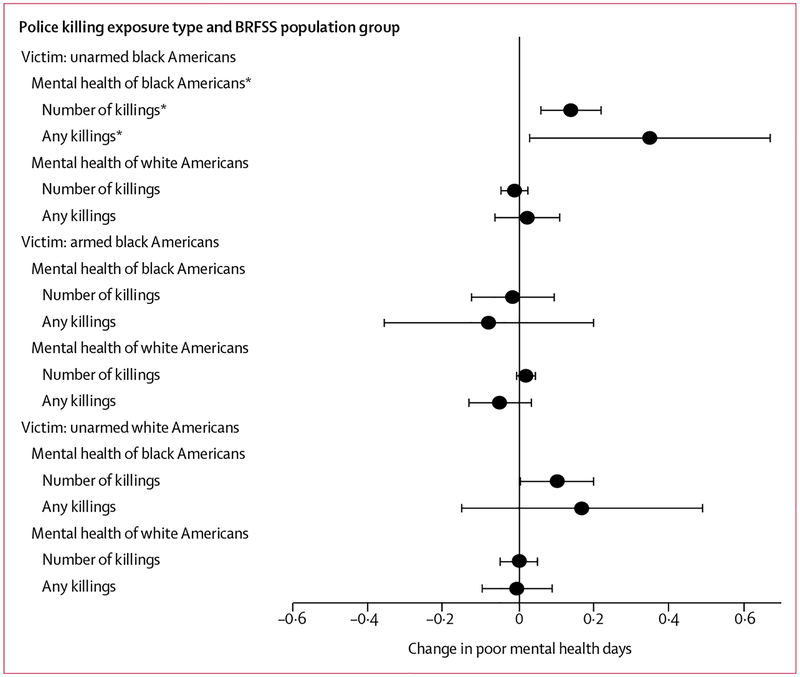
When examining the mechanisms underlying our findings, we found that exposure to police killings of unarmed black Americans was not associated with changes in mental health among white Americans, nor was exposure to police killings of unarmed white Americans (figure 2; appendix p 10). Additionally, exposure to police killings of armed black Americans was not associated with changes in mental health among black or white Americans (figure 2; appendix p 10). We found evidence of a possible association between police killings of unarmed white Americans and the mental health of black Americans, but the effect was imprecisely estimated (the cluster bootstrap-t method yielded a p value of 0·16; figure 2; appendix p 10) and was not robust to the sensitivity analyses we conducted for our main analysis (results available upon request).
Figure 2: Changes in poor mental health days associated with exposure to police killings by race of police killing victim, whether the victim was armed, and race of the BRFSS respondent.
Each estimate in this figure is derived from a separate regression. See appendix for full estimates. BRFSS=Behavioral Risk Factor Surveillance System.*Primary analysis.
Discussion
Police killings of unarmed black Americans were associated with worse mental health among other black Americans in the general US population. These findings were robust to a wide array of specification checks. Our use of a quasi-experimental methodology, coupled with empirical interrogation of potential violations to the unconfoundedness assumption, allows for a causal interpretation of these estimates.29
Our estimates suggest that police killings of unarmed black Americans have a meaningful population-level impact on the mental health of black Americans. Specifically, our estimates imply that police killings of unarmed black Americans could contribute 1·7 additional poor mental health days per person per year, or 55 million (95% CI 27 million–87 million) excess poor mental health days per year among black American adults in the USA (calculated on 33 million black Americans affected by four killings per year, leading to 0·14 excess poor mental health days per month for 3 months after each killing). To contextualise this aggregate estimate, we compare it with the mental health burden of diabetes: people with diabetes have been shown to experience 11·0 additional poor mental health days (95% CI 9·6–12·5) per year.31 Extrapolating this finding to the 20·6% of black Americans with diabetes,32 we estimate that diabetes might be responsible for an additional 75 million poor mental health days among black Americans. Our estimates therefore suggest that the population mental health burden from police killings among black Americans is nearly as large as the mental health burden associated with diabetes.
This substantial burden is even more striking given that our results might underestimate the true mental health spillover effects of police killings of unarmed black Americans. First, many of the killings in our sample received nationwide media coverage, and, consequently, there might have been spillover effects of police killings on mental health among black Americans living in other states. Those mental health spillovers are excluded from our estimates. Second, because these states form the comparison group for our exposure, any spillover effects in other states would bias our estimates of within-state effects toward the null. Third, police killings are systematically under-reported in official sources,25 and it is possible that some killings that were not well publicised were missed even in the MPV database. In our sample, race or ethnicity was unknown for 7·3% of killings of unarmed victims and these were excluded. To the extent that these missing events have mental health consequences of their own, omitting them would bias downwards our estimates of the population mental health impact of police killings. Misattribution of the armed status of a victim, if random, could also bias our estimates toward the null.
Our findings illustrate the generalisability of small-scale studies23,24,33 of mental illness after police violence in exposed communities and support recent calls to treat police killings as a public health issue,17 given the improvements in population mental health that would be likely to accrue if these killings could be averted. Such interventions might be best applied as part of a broader reform package in the criminal justice sector, given growing evidence about how other elements of the criminal justice system (eg, mass incarceration) undermine population health in communities of colour.34 Our findings also highlight the need to implement public health programmes that mitigate adverse mental health spillover effects within these communities when police killings of unarmed black Americans do occur.
Our results point to the importance of structural racism as a driver of population health disparities.14 The striking specificity of the findings—ie, that no spillover effects were observed among white respondents, nor among respondents of either race in response to police killings of unarmed whites or of armed black Americans—suggest that the meaning ascribed to police killings of unarmed black Americans, in light of the historical and institutional context in which they occur, probably mediates the adverse mental health effects of these events on black Americans. There is strong evidence of systematic targeting of black Americans by police in the identification of criminal suspects, as well as in their prosecution, conviction, and sentencing in the criminal justice system.19,20,35 Moreover, police officers who have killed unarmed black Americans are rarely charged, indicted, or successfully prosecuted.36 Racial disparities in law enforcement and legal treatment have a long history in the USA, and state-sanctioned violence in particular has been used to terrorise, dehumanise, and subjugate black Americans.15,20,37 In this context, police killings of unarmed black Americans are perceived by many as manifestations of structural racism and as implicit signals of the lower value placed on black lives by law enforcement and legal institutions—and by society at large.15,38
How does structural racism—represented in racial disparities in police killings—get under the skin and exert its corrosive effects on mental health? The observed adverse mental health spillover effects of police killings of unarmed black Americans could result from heightened perceptions of threat and vulnerability, lack of fairness, lower social status, lower beliefs about one’s own worth, activation of prior traumas, and identification with the deceased.6,7,9,12,39,40 Future research could illuminate the relative importance of these and other pathways.
In this vein, the results provide rare causal evidence about the impact of events widely perceived to reflect structural racism on the mental health of black Americans. While a small literature has identified causal links between historically racially segregated institutions and health,10,41 little—if any—causal evidence exists about the spillover consequences of contemporary events widely perceived as manifestations of structural racism. Our findings have important public health implications given the ubiquity of exposures to racism: 92% of black Americans in a 2017 survey believed that discrimination against their racial group existed today, with at least half reporting personal experiences of discrimination in the workplace or with police.42 Viewing our results in the context of the widespread prevalence of events perceived as originating from structural racism reinforces arguments that the health consequences of racism are likely to be large and pervasive.14
Our study had several limitations, many of which should motivate further research. First, the assignment of exposure was limited by the fact that geographical identifiers in the public use BRFSS files were limited to the state level. We did not have information on the extent to which BRFSS participants were directly aware of police killings. Given that some respondents exposed to a police killing in the same state 3 months prior to the survey might not actually have been aware of the police killing, our estimates have an intention-to-treat interpretation. Our findings provide a valid measure of population impact, but do not capture heterogeneity in individual-level exposures and their mental health consequences. Localised communities, for example, might experience substantially larger effects. Second, despite our quasi-experimental design, it is possible that unmeasured confounders varying at the state-year-month level—and deviating from normal state-specific seasonal patterns—could have biased our estimates. However, our results were robust to further covariate adjustment, and a falsification test provided no evidence of residual confounding. A causal interpretation is further supported by the specificity of the results, consistent with our a-priori hypothesis that police killings of unarmed black Americans have distinct spillover effects on the mental health of other black Americans. Any putative confounder that would bias our primary estimates away from the null would also be expected to bias the other five regression estimates away from the null. Third, although the mental health measure used in the BRFSS has been validated in different contexts, the self-reported nature of our primary outcome is a limitation. Future research should assess spillover effects of police shootings on a wider variety of mental health outcomes (eg, depression and anxiety), mental health service use, adverse stress-related behaviours, and physiological reactions (eg, cortisol levels). Fourth, our study does not focus on other ways in which the criminal justice system disproportionately targets black Americans. It is likely that other forms of structural racism—such as segregation, mass incarceration, and serial forced displacement—also contribute to poor population mental health.7,34 Fifth, our focus on individuals who self-reported their race as “Black/African American” in the BRFSS data—and on those identified as “Black” in the MPV database—draws an artificial boundary that masks heterogeneity within this population. For example, more recent black immigrants or naturalised black Americans from Africa or the Caribbean might experience mental health spillover effects of police shootings differently from other black Americans. However, recent work suggests that Caribbean blacks and black Americans are equally likely to face discrimination.43 Although the racial categories used in this study obscure such complexities, it has been argued that, to the extent that racial classifications are meaningful at all, they have utility in describing shared experiences of racism.44 Sixth, although we were underpowered to examine mental health effects of police killings among other vulnerable populations, such as Hispanics and Native Americans, investigating these relationships is an important direction for future research. Finally, prior evidence suggests that police killings might have adverse mental health impacts on the police officers themselves.45 We did not have the data to estimate these effects. Understanding the extent to which these effects are moderated by the race or armed status of the deceased is an important area for future research.
In our nationally representative, quasi-experimental study, police killings of unarmed black Americans had adverse effects on the mental health of black Americans in the general population. These findings bolster calls to more accurately measure police killings and provide an additional public health rationale to better understand and address the potential pathogenic effects of police killings of unarmed black Americans and other manifestations of structural racism in the USA.
Supplementary Material
Research in context.
Evidence before this study
Mortality related to police use of force is far more prevalent than official statistics suggest, and there have been several recent efforts to quantify and characterise this mortality burden. Black Americans are nearly three times more likely than are white Americans to be killed by police, with the disparity even larger for individuals who are unarmed.
Little is known about the spillover effect of police killings of unarmed black Americans on the mental health of other black Americans in the general population. We searched PubMed for articles published up to Nov 10, 2017, with the search terms “police” AND (“violence” OR “killing” OR “brutality” OR “use of force”) AND (“mental health” OR “psychological” OR “health” OR “depression” OR “anxiety”) AND (“black” OR “African American” OR “black American”). This search returned 104 articles of which three reported on mental health spillover effects of police violence. Yimgang and colleagues found elevated depressive symptoms among black mothers in Baltimore (MD, USA) following Freddie Gray’s death while in police custody. Jackson and colleagues reported a strong correlation between anticipation of negative encounters between black youth and police and heightened depressive symptoms in a sample of pregnant black women in Atlanta (GA, USA). Galovski and colleagues identified high rates of depression in the wake of Michael Brown’s death in Ferguson (MO, USA). Geller and colleagues found a link between aggressive policing practices such as stop-and-frisk and the mental health of black men. To date, no study has assessed this relationship in a national, population-representative sample.
Added value of this study
Combining recently compiled, validated data on police killings with national, population-representative data from the Behavioral Risk Factor Surveillance System (2013–15), we assessed the spillover effect of police killings of unarmed black Americans on the mental health of other black American adults living in the same state. We found that the number of poor mental health days increased by 0·14 days (95% CI 0·07–0·22) for each police killing in the previous 3 months. We found no effect on the mental health of white respondents and no effects of police killings of unarmed white Americans or armed black Americans. At a population level, police killings of unarmed black Americans might cause 55 million excess poor mental health days per year among black American adults in the USA.
Implications of all the available evidence
Police killings of unarmed black Americans have significant effects on the mental health of other black Americans in the general population. Interventions are needed to reduce the prevalence of these killings and to support the mental health of communities affected when they do occur.
Acknowledgments
ASV and ACT acknowledge funding from the Robert Wood Johnson Foundation, Evidence for Action Program. JB acknowledges salary support from the National Institutes of Health (K01-MH105320) and the Peter T Paul Career Development Professorship at Boston University. ASV acknowledges salary support from the National Institutes for Health (K23-MH106362). We would additionally like to acknowledge Zinzi Bailey (University of Miami, Miami, FL), Jonah Birch (New York University, New York, NY), Matthew Erlich (Yale School of Medicine, New Haven, CT), John Jackson (Johns Hopkins Bloomberg School of Public Health, Baltimore, MD), Keith Jones (University of Massachusetts-Boston, Boston, MA), Mathew Kiang (Harvard TH Chan School of Public Health, Boston, MA), Andrew Papachristos (Northwestern University, Evanston, IL), Marsha Parrilla (Danza Orgánica, Boston, MA), Khury Petersen-Smith (Institute for Policy Studies, Washington, DC), Elizabeth Samuels (Yale School of Medicine, New Haven, CT), and participants at the 2018 Population Association of America Annual Meeting (Denver, CO, USA; April 26–28, 2018) for helpful comments and suggestions.
Footnotes
Declaration of interests
We declare no competing interests.
For the MPV database see https://mappingpoliceviolence.org
For the BFRSS see https://www.cdc.gov/BRFSS/
See Online for appendix
For the replication data and code see https://doi.org/10.7910/DVN/VGYI0E
References
- 1.Buehler JW. Racial/ethnic disparities in the use of lethal force by US police, 2010–2014. Am J Public Health 2017; 107: 295–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sinyangwe S, McKesson D, Packnett B. Mapping police violence. 2016. https://mappingpoliceviolence.org/ (accessed May 5, 2017).
- 3.US Census Bureau, Population Division. Annual estimates of the resident population by sex, age, race, and Hispanic origin for the United States and States: April 1, 2010 to July 1, 2016. June, 2017. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=PEP_2016_PEPASR5H&prodType=table, (accessed June 13, 2018).
- 4.Essed P Understanding everyday racism: an interdisciplinary theory. Newbury Park, CA: SAGE Publications, 1991. [Google Scholar]
- 5.Harrell SP. A multidimensional conceptualization of racism-related stress: implications for the well-being of people of color. Am J Orthopsychiatry 2000; 70: 42–57. [DOI] [PubMed] [Google Scholar]
- 6.Harrell JP, Hall S, Taliaferro J. Physiological responses to racism and discrimination: an assessment of the evidence. Am J Public Health 2003; 93: 243–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams DR, Williams-Morris R. Racism and mental health: the African-American experience. Ethn Health 2000; 5: 243–68. [DOI] [PubMed] [Google Scholar]
- 8.Warner TD, Swisher RD. Adolescent survival expectations: variations by race, ethnicity, and nativity. J Health Soc Behav 2015; 56: 478–94. [DOI] [PubMed] [Google Scholar]
- 9.Lewis TT, Cogburn CD, Williams DR. Self-reported experience of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annu Rev Clin Psychol 2015; 11: 407–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alsan M, Wannamaker M. Tuskegee and the health of black men. Q J Econ 2017; 133: 407–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Catalano R, Hartig T. Communal bereavement and the incidence of very low birth weight in Sweden. J Health Soc Behav 2001; 42: 333–41. [PubMed] [Google Scholar]
- 12.Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One 2015; 10: e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams DR, Mohammed SA. Descrimination and racial disparities in health: evidence and needed research. J Behav Med 2009; 32: 20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bailey Z, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017; 389: 1453–63. [DOI] [PubMed] [Google Scholar]
- 15.Taylor K-Y. From #BlackLivesMatter to black liberation. Chicago, IL: Haymarket Books, 2016. [Google Scholar]
- 16.Mesic A, Franklin L, Cansever A, et al. The relationship between structural racism and black-white disparities in fatal police shootings at the state level. J Natl Med Assoc 2018; 110: 106–16. [DOI] [PubMed] [Google Scholar]
- 17.Krieger N, Chen JT, Waterman PD, Kiang MV, Feldman J. Police killings and police deaths are public health data and can be counted. PLoS Med 2015; 12: e1001915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carmichael S, Hamilton CV. Black power: the politics of liberation in America. New York, NY: Vintage Books, 1967. [Google Scholar]
- 19.Hehman E, Flake JK, Calanchini J. Disproportionate use of lethal force in policing is associated with regional racial biases of residents. Soc Psych Pers Sci 2017; published online July 27. DOI: 10.1177/1948550617711229. [DOI] [Google Scholar]
- 20.Alexander M The new Jim Crow. New York, NY: The New Press, 2012. [Google Scholar]
- 21.Civil Rights Division. Investigation of the Ferguson Police Department. March 4, 2015. Washington, DC: US Department of Justice, 2015. [Google Scholar]
- 22.Geller A, Fagan J, Tyler T, Link BG. Aggressive policing and the mental health of young urban men. Am J Public Health 2014; 104: 2321–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Galovski T, Peterson Z, Beagley M, Strasshofer D, Held P, Fletcher T. Exposure to violence during Ferguson protests: mental health effects for law enforcement and community members. J Trauma Stress 2016; 29: 283–92. [DOI] [PubMed] [Google Scholar]
- 24.Yimgang D, Wang Y, Paik G, Hager E, Black M. Civil unrest in the context of chronic community violence: impact on maternal depressive symptoms. Am J Public Health 2017; 107: 1455–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feldman J, Gruskin S, Coull BA, Krieger N. Quantifying underreporting of law-encourcement-related deaths in the United States vital statistics and news-media-based data sources: a capture-recapture analysis. PLoS Med 2017; 14: e1002399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Desmond M, Papachristos AV, Kirk DS. Police violence and citizen crime reporting in the black community. Am Sociol Rev 2016; 81: 857–76. [Google Scholar]
- 27.Slabaugh SL, Shah M, Zack M, et al. Leveraging health-related quality of life in population health management: the case for healthy days. Popul Health Manag 2017; 20: 13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zou G A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004; 159: 702–06. [DOI] [PubMed] [Google Scholar]
- 29.Angrist JD, Pischke JS. Mostly harmless econometrics. Princeton, NJ: Princeton University Press, 2009. [Google Scholar]
- 30.Cameron AC, Miller DL. A practioner’s guide to cluster-robust inference. J Hum Resour 2015; 50: 317–72. [Google Scholar]
- 31.Smith DW. The population perspective on quality of life among Americans with diabetes. Qual Life Res 2004; 13: 1391–400. [DOI] [PubMed] [Google Scholar]
- 32.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 2015; 314: 1021–29. [DOI] [PubMed] [Google Scholar]
- 33.Jackson F, James S, Owens T, Bryan A. Anticipated negative police-youth encounters and depressive symptoms among pregnant African American women: a brief report. J Urban Health 2017; 94: 259–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wildeman C, Wang E. Mass incarceration, public health, and widening inequality in the USA. Lancet 2017; 389: 1464–74. [DOI] [PubMed] [Google Scholar]
- 35.Civil Rights Division Investigation of Baltimore City Police Department. August 10, 2016. Washington, DC: US Department of Justice, 2016.
- 36.Lee JC, Park H. In 15 high-profile cases involving deaths of blacks, one officer faces prison time. The New York Times; December 7, 2017. https://www.nytimes.com/interactive/2017/05/17/us/black-deaths-police.html (accessed Jun 19, 2018). [Google Scholar]
- 37.Wells-Barnett IB. On lynchings (compilation). Mineola, NY: Dover Publications, 2014. [Google Scholar]
- 38.Goff P, Jackson M, Di Leone B, Culotta C, DiTomasso N. The essense of innocence: consequences of dehumanizing black children. J Pers Soc Psychol 2014; 106: 526–45. [DOI] [PubMed] [Google Scholar]
- 39.Krieger N Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv 1999; 29: 295–352. [DOI] [PubMed] [Google Scholar]
- 40.Thompson K, Wilson S. Obama on Trayvon Martin: “If I had a son, he’d look like Trayvon”. The Washington Post; (Washington, DC: ). March 23, 2012. https://www.washingtonpost.com/politics/obama-ifi-had-a-son-hed-look-like-trayvon/2012/03/23/gIQApKPpVS_story.html (accessed March 15, 2018). [Google Scholar]
- 41.Almond D, Chay KY, Greenstone M. Civil rights, the war on poverty, and black-white convergence in infant mortality in the rural South and Mississippi MIT Department of Economics Working Paper No 07–04. Cambridge, MA: MIT Department of Economics, 2007. [Google Scholar]
- 42.National Public Radio, Robert Wood Johnson Foundation, Harvard TH Chan School of Public Health. Discrimination in America: experience and views of African Americans. National Public Radio, Robert Wood Johnson Foundation, Harvard TH Chan School of Public Health, 2017. [Google Scholar]
- 43.Williams DR, Haile R, Mohammed SA, et al. Perceived discrimination and psychological well-being in the US and South Africa. Ethn Health 2012; 17: 111–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams DR. Race and health: basic questions, emerging directions. Ann Epidemiol 1997; 7: 322–33. [DOI] [PubMed] [Google Scholar]
- 45.Robinson H, Sigman M, Wilson J. Duty-related stressors and PTSD symptoms in suburban police officers. Psychol Rep 1997; 81: 835–45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.