Abstract
Objective:
The estimation of demand for treatment is one of the important elements in planning for alcohol and other drug treatment services. This article reports on a demand-projection model used in Australia to estimate the extent of unmet treatment demand by drug type.
Method:
The model incorporated the prevalence of substance use disorders (by drug type and age), with the application of a severity distribution, which distributed the substance abuse disorders into three disability categories: mild, moderate, and severe. The application of treatment rates derived from expert judgments reflecting the proportion of people within disability categories who would be suitable for, likely to seek, and benefit from treatment. Sensitivity analyses incorporating variations to the severity distributions and treatment rates were applied, along with adjustment for polydrug use.
Results:
The estimate for treatment demand for Australia varied between a low of 411,740 people and a high of 755,557 people. The most sensitive parameter is the expected treatment-seeking rate. Given that approximately 200,000 to 230,000 people are currently in treatment, this represents a met demand of between 26.8% and 56.4%.
Conclusions:
There is insufficient alcohol and drug treatment available to meet the demand in Australia, despite Australia’s relatively high met demand, when compared with other countries.
Objectif :
L’estimation de la demande de traitement est l’un des éléments importants de la planification des services de traitement liés à l’usage d’alcool et d’autres drogues. Cet article porte sur un modèle de projection de la demande, utilisé en Australie pour estimer l’étendue de la demande de traitement non-satisfaite par type de substance consommée.
Méthode :
Le modèle intègre la prévalence des troubles de l’utilisation de substance (par type de substance et par âge), l’application d’une répartition de la sévérité des troubles de l’utilisation de substances selon trois catégories (léger, modéré et sévère), ainsi que le recours à des taux de traitement, élaborés à partir du jugement d’experts, reflétant la proportion de personnes dans chaque catégorie de sévérité qui devraient avoir accès, seraient susceptibles de chercher et d’éventuellement bénéficier d’un traitement. Des analyses de sensibilité incorporant différentes variations de la répartition de la sévérité et des taux de traitement ont été menées, incluant des ajustements pour la polyconsommation.
Résultats :
L’estimation de la demande de traitements pour l’Australie varie entre un minimum de 411 740 personnes et un maximum de 755 557 personnes. Le paramètre le plus sensible est le taux de recherche de traitement. Étant donné qu’environ 200 000 à 230 000 personnes sont actuellement en traitement, cela représente une réponse à la demande variant entre 26,8% et 56,4%.
Conclusion:
Il n’y a pas suffisamment de traitement en toxicomanie disponible en Australie pour répondre à la demande, en dépit de la capacité relativement élevée de l’Australie de répondre à la demande comparativement à d’autres pays.
Objetivo:
La estimación de la demanda de tratamiento es uno de los elementos importantes en la planificación de los servicios de tratamiento de alcohol y otras drogas. Este documento informa sobre un modelo de demanda-proyección, usados en Australia para estimar la magnitud de la demanda de tratamiento no satisfecha por tipo de droga.
Método:
El modelo incorporó la prevalencia de trastornos por consumo de sustancias (por tipo de droga y edad), la aplicación de una distribución de gravedad, que distribuyó los trastornos por abuso de sustancias en tres categorías de discapacidad: leve, moderada y grave, y la aplicación de tasas de tratamiento derivadas de expertos que reflejan la proporción de personas dentro de las categorías de discapacidad que sería adecuado para, propensos a buscar, y beneficiarse del tratamiento. Se aplicaron análisis de sensibilidad que incorporan variaciones a las distribuciones de gravedad y las tasas de tratamiento, junto con un ajuste para el uso de polifármacos.
Resultados:
La estimación de la demanda de tratamiento para Australia varió entre un mínimo de 411,740 personas y un máximo de 755,557 personas. El parámetro más sensible es la tasa de búsqueda de tratamiento esperada. Dado que alrededor de 200,000 a 230,000 personas están actualmente en tratamiento, esto representa una demanda satisfecha de entre 26.8% y 56.4%.
Conclusión:
No hay suficiente tratamiento de alcohol y drogas disponible para satisfacer la demanda en Australia, a pesar de la relativamente alta demanda de Australia en comparación con otros países.
Need for treatment, defined as the number of people who meet diagnostic criteria for substance use disorder, where that disorder is known to respond to effective interventions, is commonly estimated from surveys of self-reported symptoms (which lead to diagnoses), which then define the size of the potential population in need of treatment. Researchers have used such needs-based epidemiological models to plan for services (for example, McAuliffe et al., 2002, 2003; Mojtabai & Crum, 2013; Rush & Urbanoski, 2007; Schultz et al., 2003). There are, however, substantial problems for needs-based estimates of treatment, as defined by formal diagnosis (e.g., Kip et al., 2002; Shepard et al., 2005). The assumption behind the definition and measurement of unmet need for alcohol and other drug (AOD) treatment is that substance use diagnosis is an accurate reflection of those who need treatment in the population. This may be the case for medical diseases and mental health disorders (Sareen et al., 2013) but may be less applicable for AOD. “Many experts have argued that diagnosis alone is not a good proxy for treatment need” (Sareen et al., 2013, p. 1941). It is not clear that all people who meet diagnostic criteria would need treatment. At the same time, there may be people who do not meet the formal diagnostic criteria (so-called subthreshold cases) who may be appropriate for treatment (Druss et al., 2007).
In addition, the very definition of the diagnostic criteria is arbitrary (see, for example, the research on the differences between DSM-IV and DSM-5, Mewton et al., 2011, 2013). Formal treatment services are not necessarily always required for remission of AOD problems; the role of maturation and spontaneous remission are important to acknowledge (Walters, 2000). Indeed, Sareen et al. (2013) have shown that people with a substance use disorder (and hence counted as “in need”) who have not received treatment are more likely to remit than those with a substance use disorder who received treatment. Although this is likely attributable to baseline severity differences between the groups, it still demonstrates how the measurement of unmet need based on diagnosis may substantially overestimate the need for treatment.
Demand for treatment, defined as the number of people who are seeking treatment, is likely to be a more useful concept for treatment planning and reflects the reality of patient demand for services. Demand for treatment can be measured as the actual number of people who have sought treatment (Ford, 1985, 1997; Ford & Luckey, 1983; Ford & Schmittdiel, 1983). However, this assumes that past demand predicts future demand and that past demand reflects client needs; both of these assumptions are problematic.
An alternate method is to survey people about their intention to seek treatment. However, in population surveys, the majority of respondents report that they do not need treatment. For example, the U.S. National Survey on Drug Use and Health, 2010 data (Substance Abuse and Mental Health Services Administration [SAMHSA], 2010) showed that, of the 6,384 people who demonstrated a need for treatment (as defined by meeting diagnostic criteria and not being in receipt of treatment in the last 12 months), only 392 felt the need for treatment (6%) and 193 “made the effort to seek treatment” (unsuccessfully) (3%). In the U.S. National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), only 8.5% of those respondents with a substance use disorder perceived the need for treatment (Mojtabai & Crum, 2013). Thus it is likely that perceived need for treatment may represent an underestimate of unmet demand.
Some researchers have generated composite measures of treatment demand. For example, Spence (2003) included diagnosis (DSM-IV) by severity, as well as relapse potential (e.g., the number of previous treatments) plus environmental risk (marital status, employment status, living arrangements, and so on). This measure accommodated factors consistent with the notion of demand for treatment, such as the individual’s circumstances. In addition, they included preference-based need, obtained from a survey (what clients said they wanted).
An important consideration in estimating demand is the extent of the severity of the problem. For those with less severe alcohol or other drug disorders, the demand for treatment is likely to be lower. This requires that the demand estimation be built with considerations of problem severity in mind. The work led by Rush and colleagues (Rush, 1990, 2010; Rush et al., 2012, 2019) explicitly attends to the relationship between problem severity (acuity, complexity, and chronicity) and the continuum of care (from generic brief interventions to intensive specialist services). This recognizes that a single national or local estimate of unmet demand for treatment is not helpful for planners. Planners need to know the unmet demand for different service types by the different levels of client severity. One of the challenges for models such as these, then, is how to estimate the likelihood of treatment seeking by different subpopulations of severity (given that those with a less severe substance use disorder are also less likely to seek treatment). Rush and colleagues (2019) made extensive use of expert opinion (Delphi procedures) to derive the probable rates of help seeking for each subpopulation.
The aim of the research described in this article was to establish estimates of demand for AOD treatment in Australia by drug type, incorporating problem severity, and a spectrum of treatment rates. Furthermore, we sought to match the overall demand estimate with the number of people who have sought treatment—creating an unmet demand estimate. The simple quantum of demand is limited in its usefulness unless it is matched with an accurate estimate of currently met demand. This analysis provides essential information for health planners in developing a treatment service system that can accommodate the number of individuals who would be suitable for, would be likely to seek, and would benefit from AOD treatment in any one year. In addition, this article outlines an approach that could be undertaken by health planners in any country, highlighting the importance of both severity distribution and determining appropriate treatment rates.
Method
The Drug and Alcohol Service Planning (DASP) model, developed between 2010 and 2013 by the New South Wales (NSW) Ministry of Health (Mental Health and Drug and Alcohol Office), aimed to facilitate planning for AOD services in Australia and to provide a basis for national consistency in approaches to planning across all the Australian health jurisdictions. The model followed the principles of population-based planning used in the Mental Health Clinical Care and Prevention (MH-CCP) model of 2000 (Centre for Mental Health, 2001; Pirkis et al., 2007). The DASP model applied the prevalence of substance use disorders, by drug type and age group from epidemiological sources; incorporated a severity rating to distinguish mild, moderate, and severe presentations; and then used expert consensus (the Expert Reference Group) to estimate the treatment rate. The treatment rate reflected the proportion of all those who met diagnostic criteria who would be suitable for, likely to seek, and benefit from treatment in any one year (that is, demand for treatment). The severity ratings (assignment to mild, moderate, or severe disability) were important because these then drove differential treatment rates, and hence they are sensitive measures in terms of the model’s prediction of the demand for treatment.
DASP predictions of treatment demand, therefore, relied on three key variables: the epidemiology (that is, the prevalence of AOD disorders in the community), the severity distribution (the distribution of people with AOD disorders into three disability categories: mild, moderate, and severe), and the treatment rates (the proportion of all people who would be suitable for, likely to seek, and benefit from treatment, given the appropriateness of the treatment services available).
Epidemiology
The epidemiology for the model was based on the Australian Burden of Disease (AUSBoD) (Begg et al., 2007), which in turn relied largely on the 1997 National Survey of Mental Health and Wellbeing (NSMHWB; Australian Bureau of Statistics, 1998a; Hall et al., 1999). The Composite International Diagnostic Interview (CIDI) was used as the interview tool to establish the rates of ICD-10 diagnoses of dependence and harmful use of alcohol, cannabis, sedatives, opioids, and stimulants. The last two classes (opioids and stimulants) are very low-prevalence disorders in the general population, and general population surveys underestimate the prevalence of these drug classes (Degenhardt et al., 2011; Hall et al., 1999). The DASP model therefore sought alternate epidemiology for heroin and stimulants (amphetamine).
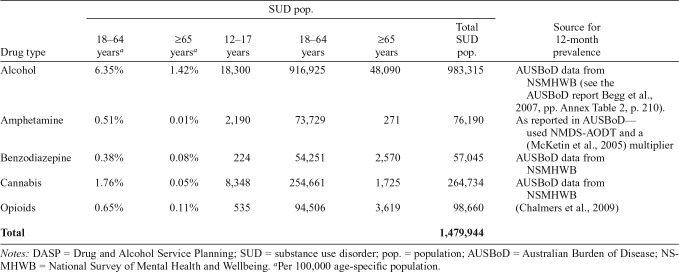
The prevalence rates, their sources, along with the actual population numbers (using the 2006 Australian population estimates taken from the Australian Bureau of Statistics [ABS] online publication 3222.0 – Population Projections, Australia, 2006 to 2101, Series B) are given in Table 1. This assumes that the prevalence rates from the 1997 survey still applied in 2006.
Table 1.
Past-12-month prevalence rates applied in the DASP model, associated data source and population, by drug type
| SUD pop. |
|||||||
| Drug type | 18–64 yearsa | ≥65 yearsa | 12–17 years | 18–64 years | ≥65 years | Total SUD pop. | Source for 12-month prevalence |
| Alcohol | 6.35% | 1.42% | 18,300 | 916,925 | 48,090 | 983,315 | AUSBoD data from NSMHWB (see the AUSBoD report Begg et al., 2007, pp. Annex Table 2, p. 210). |
| Amphetamine | 0.51% | 0.01% | 2,190 | 73,729 | 271 | 76,190 | As reported in AUSBoD— used NMDS-AODT and a (McKetin et al., 2005) multiplier |
| Benzodiazepine | 0.38% | 0.08% | 224 | 54,251 | 2,570 | 57,045 | AUSBoD data from NSMHWB |
| Cannabis | 1.76% | 0.05% | 8,348 | 254,661 | 1,725 | 264,734 | AUSBoD data from NSMHWB |
| Opioids | 0.65% | 0.11% | 535 | 94,506 | 3,619 | 98,660 | (Chalmers et al., 2009) |
| Total | 1,479,944 | ||||||
Notes: DASP = Drug and Alcohol Service Planning; SUD = substance use disorder; pop. = population; AUSBoD = Australian Burden of Disease; NSMHWB = National Survey of Mental Health and Wellbeing.
Per 100,000 age-specific population.
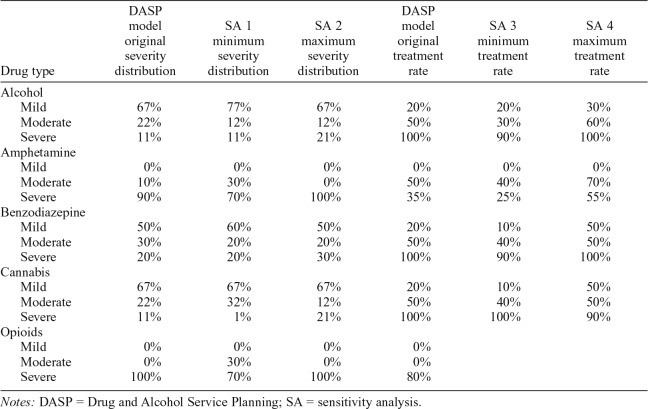
Severity distribution and treatment rate
The DASP model distinguished between mild, moderate, and severe disability. The division into mild, moderate, and severe disability was facilitated by the available Australian data on disability weights from AUSBoD (Begg et al., 2007), which in turn relied on the 12-Item Short Form Survey (SF12) measure of functioning. The proportion of those meeting diagnostic criteria who would fall within the severe disability category, using the AUSBoD disability weights, was calculated first and then was combined with existing research and expert judgment to divide the remaining numbers between mild and moderate disability.
The ratio of mild to moderate to severe disability for alcohol was 6:2:1; that is, for every 6 people mildly disabled, there were 2 moderately disabled and 1 severely disabled (Table 2). The same ratio was used for cannabis (6:2:1). For opioids, no one was classed as having a mild or moderate disability (all were placed in the severe category). For amphetamines, no one was classed as having a mild disability, and, for every 9 severely disabled, there was one moderately disabled. Last, for benzodiazepines, for every 5 people classed as mildly disabled, 3 were classed as moderately disabled and 2 as severely disabled (5:3:2).
Table 2.
DASP model treatment rates for drug class by severity distributions

| Drug type | Severity distribution | Treatment rate |
| Alcohol | ||
| Mild | 67% | 20% |
| Moderate | 22% | 50% |
| Severe | 11% | 100% |
| Amphetamine | ||
| Mild | 0% | 0% |
| Moderate | 10% | 50% |
| Severe | 90% | 35%a |
| Benzodiazepine | ||
| Mild | 50% | 20% |
| Moderate | 30% | 50% |
| Severe | 20% | 100% |
| Cannabis | ||
| Mild | 67% | 20% |
| Moderate | 22% | 50% |
| Severe | 11% | 100% |
| Opioids | ||
| Mild | 0% | 0% |
| Moderate | 0% | 0% |
| Severe | 100% | 90% |
Notes: DASP = Drug and Alcohol Service Planning.
The treatment rate for amphetamine was subject to substantial debate among the expert group, and, although retained at 35% for severe, this number is able to be modified by DASP model end users should they wish.
The treatment rates for each category of severity were established for the DASP model based on existing research and the judgment of the Expert Reference Group. In the 1997 NSMHWB survey (ABS, 1998b), 14% of those with substance use disorders had used services in the past year. A decade later, in the 2007 Australian NSMHWB survey (Slade et al., 2009), 24% of the respondents with substance use disorders used treatment services in the past 12 months. The 2007 figure then informed the absolute minimum treatment rate for the DASP model. In theory the maximum treatment rate would be 100%—that is, everyone with mild, moderate, and severe disability who meets diagnostic criteria for substance use disorder would receive treatment. This is unrealistic for several reasons: (a) spontaneous remission, or natural recovery, is not uncommon (a proportion will never require treatment); (b) some people will seek support for behavior change through unfunded or informal means (such as mutual aid/self-help); (c) some people will not find the AOD services an appropriate match for their needs; and (d) some people will not see the need for treatment and not seek care.
Therefore, the DASP model required expert judgments about treatment rates that incorporated these factors. These expert judgments were informed by earlier research that noted an ideal treatment coverage of 51% for alcohol use disorders (70% for harmful use and 30% for dependence; see also Andrews et al., 2004). Subsequently, the same team reduced this to an average of 38% (50% alcohol harmful use and 25% alcohol dependence) (Andrews et al., 2006). In light of the minimum rate of 24% and a possible optimal rate of 51% as an overall treatment rate (across the severity distribution), the experts deliberated over a series of meetings (having been provided with the above data along with current treatment rates) until consensus was reached among the group. The resultant treatment rates are given in Table 2. Thus, for example, for those with AUD at mild severity (which represents 67% of all AUD), there is a presumed treatment rate of 20%, whereas for those with a severe AUD (11% of all AUD), the treatment rate is 100%. When averaged across severity types, the treatment rate for alcohol was 35%, for amphetamines 36%, for benzodiazepines 45%, for cannabis 35%, and for opioids 90%. It should be noted that there was substantial and sustained debate about the treatment rates in the DASP Expert Reference Group. In addition, end users can modify the treatment rates if they wish.
Sensitivity analyses
Given the significant uncertainties associated with the prevalence rates, the severity distribution, and the treatment rates, a series of sensitivity analyses was undertaken to show how the demand estimates varied with changes in prevalence, severity, and treatment rate. We varied only one of the three parameters at a time, and when we varied a parameter we varied it across all age groups. The prevalence rates were altered by 25 percentage points (both higher and lower), per drug class, per age group. The analyses revealed a linear relationship between the changed prevalence and the predicted demand (and for this reason they are not reported further herein).
For the severity distribution, there was no pre-existing research or guidance to inform the decisions about the percentage changes to be applied, and each drug class needed to be considered separately. The severity distributions for alcohol, benzodiazepines, and cannabis were varied by 10 percentage points. For amphetamine, the minimum severity was varied by 20 percentage points (given 0% in mild severity), and for opioids it was a 30 percentage point change (and no alteration to the maximum as this was the base case). (See Table 3. Note that the severity distributions need to sum to 100%.)
Table 3.
Sensitivity analyses: summary of variations to be tested
| Drug type | DASP model original severity distribution | SA 1 minimum severity distribution | SA 2 maximum severity distribution | DASP model original treatment rate | SA 3 minimum treatment rate | SA 4 maximum treatment rate |
| Alcohol | ||||||
| Mild | 67% | 77% | 67% | 20% | 20% | 30% |
| Moderate | 22% | 12% | 12% | 50% | 30% | 60% |
| Severe | 11% | 11% | 21% | 100% | 90% | 100% |
| Amphetamine | ||||||
| Mild | 0% | 0% | 0% | 0% | 0% | 0% |
| Moderate | 10% | 30% | 0% | 50% | 40% | 70% |
| Severe | 90% | 70% | 100% | 35% | 25% | 55% |
| Benzodiazepine | ||||||
| Mild | 50% | 60% | 50% | 20% | 10% | 50% |
| Moderate | 30% | 20% | 20% | 50% | 40% | 50% |
| Severe | 20% | 20% | 30% | 100% | 90% | 100% |
| Cannabis | ||||||
| Mild | 67% | 67% | 67% | 20% | 10% | 50% |
| Moderate | 22% | 32% | 12% | 50% | 40% | 50% |
| Severe | 11% | 1% | 21% | 100% | 100% | 90% |
| Opioids | ||||||
| Mild | 0% | 0% | 0% | 0% | ||
| Moderate | 0% | 30% | 0% | 0% | ||
| Severe | 100% | 70% | 100% | 80% |
Notes: DASP = Drug and Alcohol Service Planning; SA = sensitivity analysis.
Again, no past research could inform the sensitivity analyses on the treatment rate. A three-step method was used for the treatment rates: first, systematic application of new rates for mild, then moderate and severe treatment rates; followed by selection of those analyses providing minimum and maximum changes; then third, selection of those rates that had face validity (i.e., were clinically realistic). More specifically, the treatment rates were initially systematically varied by increasing mild treatment to 50% and keeping moderate and severe treatment constant; decreasing mild treatment to 10%, decreasing moderate treatment to 10%, and keeping severe treatment at 100%; keeping mild and moderate treatment rates the same as the base case (20% and 50%, respectively) and decreasing the severe treatment rate to 90%; and finally keeping the mild treatment rate at 20%, decreasing the moderate treatment rate to 30%, and decreasing the severe treatment rate to 90%. We examined the results of these analyses and determined those that produced the minimum and maximum change in predicted numbers being treated. This was then moderated by the knowledge of the current Australian treatment service system and treatment-seeking rates to ensure that the sensitivity analyses were clinically realistic. For example, a mild treatment rate of 50% for alcohol use disorders would not be feasible in practice. The resulting treatment rates used in the sensitivity analyses reported here are given in Table 3.
Polydrug use adjustment
The DASP model treated each drug class independently, thus potentially double counting individuals who may have both an alcohol use and a cannabis use disorder, for example. The most parsimonious way to deal with this problem is to adjust the prevalence rates—that is, to reduce the prevalence numbers by those who are dually (or triply) diagnosed. Using Australian data on dual diagnoses (Degenhardt & Hall, 2003; Teesson et al., 2010, 2012), adjustments for the overlap between alcohol and cannabis were possible, but no specific data were available to adjust for the other specific drug classes (they were treated as “other drug” together).
Results
Estimating treatment demand
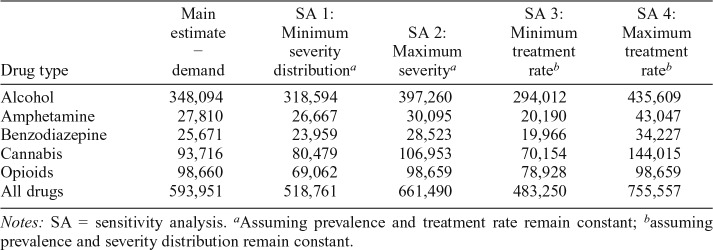
In the first instance, we report estimates without any adjustment for polydrug use. Table 4 provides the predicted demand for treatment for the main estimate and the four sensitivity analyses.
Table 4.
Predicted/modeled demand (number of people receiving treatment in the course of 1 year) main estimate and sensitivity analyses
| Drug type | Main estimate − demand | SA 1: Minimum severity distributiona | SA 2: Maximum severitya | SA 3: Minimum treatment rateb | SA 4: Maximum treatment rateb |
| Alcohol | 348,094 | 318,594 | 397,260 | 294,012 | 435,609 |
| Amphetamine | 27,810 | 26,667 | 30,095 | 20,190 | 43,047 |
| Benzodiazepine | 25,671 | 23,959 | 28,523 | 19,966 | 34,227 |
| Cannabis | 93,716 | 80,479 | 106,953 | 70,154 | 144,015 |
| Opioids | 98,660 | 69,062 | 98,659 | 78,928 | 98,659 |
| All drugs | 593,951 | 518,761 | 661,490 | 483,250 | 755,557 |
Notes: SA = sensitivity analysis.
Assuming prevalence and treatment rate remain constant;
assuming prevalence and severity distribution remain constant.
The main estimate predicted that the treatment demand would be for 593,951 people in Australia over 1 year (Table 4). As can be seen, the majority are for alcohol treatment (348,094: 58.6%). The sensitivity analyses revealed that the demand may be as low as 483,250 or as high as 755,557, depending on the choices about both severity distribution and treatment rate. The size of the difference in the ranges (in the order of 272,000 people) shows the importance of choosing the severity distribution and treatment rate parameters carefully. There is no objective evidence base to support one preferred distribution of severity and treatment rate over another. It relies on making expert judgments.
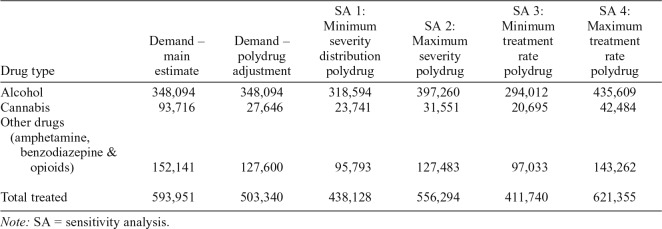
As expected, the adjustments for polydrug presentations resulted in lower overall estimate of demand (503,340)with a high estimate of 621,355 (based on SA 4), and a low estimate of 411,740 (SA 1; Table 5). Relative to the main demand estimate (593,951), the lowest estimate of 411,740 was predicated on modeling a lower treatment rate and accommodating a polydrug adjustment; and the highest estimate derived from the higher treatment rates.
Table 5.
Predicted/modeled demand estimate and sensitivity analyses taking into account polydrug use
| Drug type | Demand – main estimate | Demand – polydrug adjustment | SA 1: Minimum severity distribution polydrug | SA 2: Maximum severity polydrug | SA 3: Minimum treatment rate polydrug | SA 4: Maximum treatment rate polydrug |
| Alcohol | 348,094 | 348,094 | 318,594 | 397,260 | 294,012 | 435,609 |
| Cannabis | 93,716 | 27,646 | 23,741 | 31,551 | 20,695 | 42,484 |
| Other drugs (amphetamine, benzodiazepine & opioids) | 152,141 | 127,600 | 95,793 | 127,483 | 97,033 | 143,262 |
| Total treated | 593,951 | 503,340 | 438,128 | 556,294 | 411,740 | 621,355 |
Note: SA = sensitivity analysis.
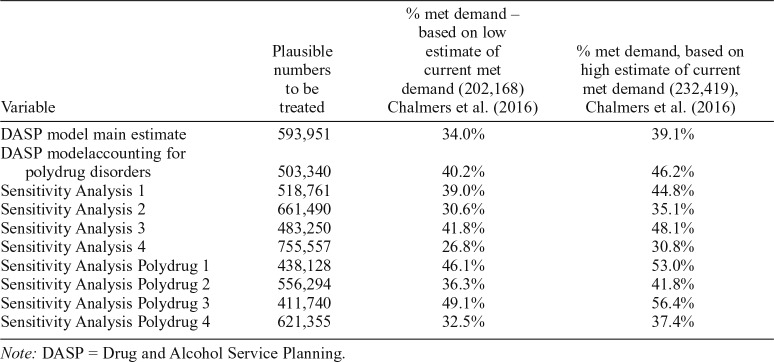
Comparison of the findings with estimates of current met demand
Chalmers et al. (2016) estimated that between 202,168 and 232,419 individuals received treatment in Australia in 2011/2012. This is the only comprehensive estimate of the met demand for Australia. Applying those figures to the total demand estimated here reveals that the proportion of demand currently being met ranges between 26.8% and 56.4% (Table 6). If this is translated into numbers of people, the additional number of people to be treated in any one year in Australia to meet predicted demand may be as high as 553,389 more people (that is if total demand = 755,557 less current met demand of 202,168) or as low as 179,321 more people (where total demand = 411,740 less met demand of 232,419).
Table 6.
Extent of potential met demand
| Variable | Plausible numbers to be treated | % met demand – based on low estimate of current met demand (202,168) Chalmers et al. (2016) | % met demand, based on high estimate of current met demand (232,419), Chalmers et al. (2016) |
| DASP model main estimate | 593,951 | 34.0% | 39.1% |
| DASP modelaccounting for polydrug disorders | 503,340 | 40.2% | 46.2% |
| Sensitivity Analysis 1 | 518,761 | 39.0% | 44.8% |
| Sensitivity Analysis 2 | 661,490 | 30.6% | 35.1% |
| Sensitivity Analysis 3 | 483,250 | 41.8% | 48.1% |
| Sensitivity Analysis 4 | 755,557 | 26.8% | 30.8% |
| Sensitivity Analysis Polydrug 1 | 438,128 | 46.1% | 53.0% |
| Sensitivity Analysis Polydrug 2 | 556,294 | 36.3% | 41.8% |
| Sensitivity Analysis Polydrug 3 | 411,740 | 49.1% | 56.4% |
| Sensitivity Analysis Polydrug 4 | 621,355 | 32.5% | 37.4% |
Note: DASP = Drug and Alcohol Service Planning.
Discussion
Planning for the appropriate amount of AOD treatment requires demand estimation. The work reported herein used a unique demand-based projection model to estimate the number of Australians who are appropriate for and would seek AOD treatment and then matched this against an estimate of met demand. Between 180,000 and 553,000 more people would be in treatment if demand were to be met; or stated differently, current met demand represents between 26.8% and 56.4% of the current Australian potential treatment population.
These modeled demand rates from the application of a unique and complex model should be higher than those reported for existing treatment utilization (effectively selfreported met demand). Andrews et al. (2004) reported a met demand rate between 8.1% (harmful) and 13.6% (dependence) for alcohol. More recent Australian estimates from the same survey source (the National Survey of Mental Health and Wellbeing) reported between 15.5% (harmful alcohol) and 52.4% (any drug dependence), with an average of 24% (Slade et al., 2009; Teesson et al., 2010, 2012). This suggests that the low modeled estimate (at 26.8%) is not unreasonable and accords with self-reported met demand.
Benchmarking the Australian results against estimates published from other developed countries suggests that, with the met demand falling between 27% and 56%, Australia has a relatively high rate of met demand. For other countries, estimates below or around 10% were reported for alcohol (Cohen et al., 2007; Drummond et al., 2005, 2009; Edlund et al., 2012), and a high estimate for alcohol use disorders was 22% (Kohn et al., 2004). For substance use disorders, the estimates ranged between 12% and 33% (Busch et al., 2013; McCollister & French, 2002; Mojtabai & Crum, 2013; Sareen et al., 2013; Spence, 2003; Sung et al., 2011). The figures reported herein are the first for Australia and contribute to this growing body of international literature regarding the size of the gap between met and unmet demand for AOD treatment.
As with any modeling work, there are many limitations, largely concerned with the series of assumptions that are required. The epidemiological prevalence data derived from 1997 and included both abuse and dependence diagnoses—arguably overestimating treatment need from the start. However, the inclusion of a mild severity category mitigated this. The average treatment rate across the model was 35% (excluding opioids), appearing quite modest. The sensitivity analyses address this, but it remains an open question for expert judgment. Gender was not included in the original DASP model—a limitation given the known differences in treatment seeking between males and females (Green, 2006). The published analysis of met demand (Chalmers et al., 2016) did not distinguish between drug classes, yet the predicted unmet demand will vary by drug class and by age group. The lack of detailed analyses of current met demand limits the opportunities for further analysis of the predicted demand, and more specific areas of high need. More generally, a limitation with this and other such models is that they are predicated on the existence of an identifiable and somewhat mature treatment service system, in which there are readily identifiable specialist services, evidence-based treatments are provided, and planning units are dedicated to determining the number, type, and spread of treatment services. This is rarely the case in developing countries (World Health Organization, 2017); hence, this population-based planning model is appropriate only for developed countries.
These analyses highlight that planning requires more than simply a quantitative model to predict demand. Consistent with all approaches to planning and needs assessment, multiple methods are required in order to gain a full picture of treatment gaps (Eagar et al., 2001). The perceptions of practitioners, clients, and the community are as important as the mathematical quantifications. Nonetheless, it is quite clear that there is a significant gap between the provision of AOD treatment in Australia and the existing demand for treatment. This gap represents a significant cost to society—not just in economic terms (where the burden of untreated substance use disorders is substantial; Collins & Lapsley, 2008), but also in terms of the physical and psychological effects (pain and suffering) that could be alleviated with the provision of treatment.
Acknowledgments
The DASP model was developed by the NSW MHDAO team (Judith Burgess, Alexander Canduci, Sue Hailstone, Anna Kollias, Harry Perlich, Ravneet Ram, Meredith Sims, Gavin Stewart, and Brian Woods). The Expert Reference Group for the DASP model development included Alison Ritter (Chair), Robert Ali, Meredythe Crane, Robyn Davies, Sarah Gobbert, Anthony Sievers, Helene Delany, Dennis Gray, James Hunter, Susan Alarcon, Tania Murray, Robert Batey, Debbie Kaplan, Nick Lintzeris, Dan Lubman, Lynne Magor-Blatch, Liz Davis, Elise Newton, Ashleigh Lynch, Garth Popple, Anita Reimann, and Myra Brown.
Footnotes
This work was commissioned and funded by the Australian Government Department of Health. Financial support was also provided by the Drug Policy Modelling Program core funds (Colonial Foundation Trust), and Professor Alison Ritter is a recipient of a National Health and Medical Research Council (NHMRC) Senior Research Fellowship (GNT102988). The Drug and Alcohol Service Planning (DASP) model was developed with funding from the Commonwealth Department of Health and Ageing and the New South Wales (NSW) Ministry of Health (Mental Health and Drug and Alcohol Office; MHDAO). The DASP model was developed by the NSW MHDAO team (Judith Burgess, Alexander Canduci, Sue Hailstone, Anna Kollias, Harry Perlich, Ravneet Ram, Meredith Sims, Gavin Stewart, and Brian Woods).
References
- Andrews G., Issakidis C., Sanderson K., Corry J., Lapsley H. Utilising survey data to inform public policy: Comparison of the costeffectiveness of treatment of ten mental disorders. British Journal of Psychiatry. 2004;184:526–533. doi: 10.1192/bjp.184.6.526. doi:10.1192/bjp.184.6.526. [DOI] [PubMed] [Google Scholar]
- Andrews G. the Tolkien II team. Tolkien II: A needs-based, costed, stepped-care model for mental health services: Recommendations, executive summaries, clinical pathways, treatment flowcharts, costing structures. Sydney, Australia: World Health Organization; 2006. [Google Scholar]
- Australian Bureau of Statistics. Mental health and wellbeing: Profile of adults, Australia, 1997. 1998a Retrieved from http://www.abs.gov.au/ausstats/abs@.nsf/ProductsbyReleaseDate/D5A0AC778746378FCA2574EA00122887. [Google Scholar]
- Australian Bureau of Statistics. National survey of mental health and wellbeing of adults: Users’ guide, 1997. 1998b Retrieved from http://www.abs.gov.au/AUSSTATS/abs@.nsf/allprimarymainfeatures/E1E464E508DB0948CA25755900126CE4?opendocument. [Google Scholar]
- Begg S., Vos T., Barker B., Stevenson C., Stanley L., Lopez A. Canberra, Australia: Australian Institute of Health and Welfare; 2007. The burden of disease and injury in Australia 2003 (Vol. PHE 82) [Google Scholar]
- Busch S. H., Meara E., Huskamp H. A., Barry C. L. Characteristics of adults with substance use disorders expected to be eligible for Medicaid under the ACA. Psychiatric Services. 2013;64:520–526. doi: 10.1176/appi.ps.201200011. doi:10.1176/appi.ps.201200011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centre for Mental Health. Mental health clinical care and prevention model: A population health model. MH-CCP Version 1.11. 2001 Retrieved from http://www.health.nsw.gov.au/mentalhealth/Documents/mh-ccp-v-1-11.pdf. [Google Scholar]
- Chalmers J., Ritter A., Berends L. Estimating met demand for alcohol and other drug treatment in Australia. Addiction. 2016;111:2041–2049. doi: 10.1111/add.13473. doi:10.1111/add.13473. [DOI] [PubMed] [Google Scholar]
- Chalmers J., Ritter A., Heffernan M., McDonnell G. Modelling pharmacotherapy maintenance in Australia: Exploring affordability, availability, accessibility and quality using a system dynamics modelling approach. Canberra: Australian National Council on Drugs; 2009. [Google Scholar]
- Cohen E., Feinn R., Arias A., Kranzler H. R. Alcohol treatment utilization: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2007;86:214–221. doi: 10.1016/j.drugalcdep.2006.06.008. doi:10.1016/j.drugalcdep.2006.06.00. [DOI] [PubMed] [Google Scholar]
- Collins D. J., Lapsley H. M. The costs of tobacco, alcohol and illicit drug abuse to Australian society in 2004/05. 2008 Retrieved from https://www.health.gov.au/internet/drugstrategy/publishing.nsf/Content/34F55AF632F67B70CA2573F60005D42B/$File/mono64.pdf. [Google Scholar]
- Degenhardt L., Bucello C., Calabria B., Nelson P., Roberts A., Hall W., McLaren J. What data are available on the extent of illicit drug use and dependence globally? Results of four systematic reviews. Drug and Alcohol Dependence. 2011;117:85–101. doi: 10.1016/j.drugalcdep.2010.11.032. doi:10.1016/j.drugalcdep.2010.11.032. [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Hall W. Patterns of co-morbidity between alcohol use and other substance use in the Australian population. Drug and Alcohol Review. 2003;22:7–13. doi: 10.1080/0959523021000059776. doi:10.1080/0959523021000059776. [DOI] [PubMed] [Google Scholar]
- Drummond C., Deluca P., Oyefeso A., Rome A., Scrafton S., Rice P. Scottish alcohol needs assessment. 2009 Retrieved from https://www.rcpsych.ac.uk/pdf/SANA%20report%206-8-09%20(2).pdf. [Google Scholar]
- Drummond C., Oyefeso A., Phillips T., Cheeta S., Deluca P., Perryman K., Christoupoulos A. Alcohol Needs Assessment Research Project (ANARP): The 2004 national alcohol needs assessment for England. 2005 Retrieved from http://webarchive.nationalarchives.gov.uk/20130123205210/ http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4122341. [Google Scholar]
- Druss B. G., Wang P. S., Sampson N. A., Olfson M., Pincus H. A., Wells K. B., Kessler R. C. Understanding mental health treatment in persons without mental diagnoses: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2007;64:1196–1203. doi: 10.1001/archpsyc.64.10.1196. doi:10.1001/archpsyc.64.10.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eagar K., Garrett P., Lin V. Health planning: Australian perspectives. Crows Nest, Australia: Allen & Unwin; 2001. [Google Scholar]
- Edlund M. J., Booth B. M., Han X. Who seeks care where? Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. Journal of Studies on Alcohol and Drugs. 2012;73:635–646. doi: 10.15288/jsad.2012.73.635. doi:10.15288/jsad.2012.73.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford W. E. Alcoholism and drug abuse service forecasting models: A comparative discussion. International Journal of the Addictions. 1985;20:233–252. doi: 10.3109/10826088509044908. doi:10.3109/10826088509044908. [DOI] [PubMed] [Google Scholar]
- Ford W. E. Perspective on the integration of substance user needs assessment and treatment planning. Substance Use & Misuse. 1997;32:343–349. doi: 10.3109/10826089709055854. discussion 351–357, 359–360. doi:10.3109/10826089709055854. [DOI] [PubMed] [Google Scholar]
- Ford W. E., Luckey J. W. Planning alcoholism services: A technique for projecting specific service needs. International Journal of the Addictions. 1983;18:319–331. doi: 10.3109/10826088309039351. doi:10.3109/10826088309039351. [DOI] [PubMed] [Google Scholar]
- Ford W. E., Schmittdiel C. J. Predicting alcoholism service needs from a National Treatment Utilization Survey. International Journal of the Addictions. 1983;18:1073–1084. doi: 10.3109/10826088309027371. doi:10.3109/10826088309027371. [DOI] [PubMed] [Google Scholar]
- Green C. A. Gender and use of substance abuse treatment services. Alcohol Research & Health. 2006;29:55–62. [PMC free article] [PubMed] [Google Scholar]
- Hall W., Teesson M., Lynskey M., Degenhardt L. The 12-month prevalence of substance use and ICD-10 substance use disorders in Australian adults: Findings from the National Survey of Mental Health and Well-Being. Addiction. 1999;94:1541–1550. doi:10.1046/j.1360-0443.1999.9410154110. [PubMed] [Google Scholar]
- Kip K. E., Peters R. H., Morrison-Rodriguez B. Commentary on why national epidemiological estimates of substance abuse by race should not be used to estimate prevalence and need for substance abuse services at community and local levels. American Journal of Drug and Alcohol Abuse. 2002;28:545–556. doi: 10.1081/ada-120006741. doi:10.1081/ADA-120006741. [DOI] [PubMed] [Google Scholar]
- Kohn R., Saxena S., Levav I., Saraceno B. The treatment gap in mental health care. Bulletin of the World Health Organization. 2004;82:858–866. doi:S0042-96862004001100011. [PMC free article] [PubMed] [Google Scholar]
- McAuliffe W. E., LaBrie R., Woodworth R., Zhang C., Dunn R. P. State substance abuse treatment gaps. American Journal on Addictions. 2003;12:101–121. doi:10.1111/j.1521-0391.2003.tb00609.x. [PubMed] [Google Scholar]
- McAuliffe W. E., Woodworth R., Zhang C. H., Dunn R. P. Identifying substance abuse treatment gaps in substate areas. Journal of Substance Abuse Treatment. 2002;23:199–208. doi: 10.1016/s0740-5472(02)00263-5. doi:10.1016/S0740-5472(02)00263-5. [DOI] [PubMed] [Google Scholar]
- McCollister K., French M. The economic cost of substance abuse treatment in criminal justice settings. Treatment of Drug Offenders: Policies and Issues. 2002:22–37. [Google Scholar]
- McKetin R., McLaren J., Kelly E., Hall W., Hickman M. Estimating the number of regular and dependent methamphetamine users in Australia. Sydney: National Drug and Alcohol Research Centre (NDARC); 2005. [Google Scholar]
- Mewton L., Slade T., McBride O., Grove R., Teesson M. An evaluation of the proposed DSM-5 alcohol use disorder criteria using Australian national data. Addiction. 2011;106:941–950. doi: 10.1111/j.1360-0443.2010.03340.x. doi:10.1111/j.1360-0443.2010.03340.x. [DOI] [PubMed] [Google Scholar]
- Mewton L., Slade T., Memedovic S., Teesson M. Alcohol use in hazardous situations: Implications for DSM-IV and DSM-5 alcohol use disorders. Alcoholism: Clinical and Experimental Research. 2013;37(Supplement 1):E228–E236. doi: 10.1111/j.1530-0277.2012.01881.x. doi:10.1111/j.1530-0277.2012.01881.x. [DOI] [PubMed] [Google Scholar]
- Mojtabai R., Crum R. M. Perceived unmet need for alcohol and drug use treatments and future use of services: Results from a longitudinal study. Drug and Alcohol Dependence. 2013;127:59–64. doi: 10.1016/j.drugalcdep.2012.06.012. doi:10.1016/j.drugalcdep.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., Harris M., Buckingham W., Whiteford H., Townsend-White C. International planning directions for provision of mental health services. Administration and Policy in Mental Health. 2007;34:377–387. doi: 10.1007/s10488-007-0116-0. doi:10.1007/s10488-007-0116-0. [DOI] [PubMed] [Google Scholar]
- Rush B. A systems approach to estimating the required capacity of alcohol treatment services. British Journal of Addiction. 1990;85:49–59. doi: 10.1111/j.1360-0443.1990.tb00623.x. doi:10.1111/j.1360-0443.1990.tb00623.x. [DOI] [PubMed] [Google Scholar]
- Rush B. Tiered frameworks for planning substance use service delivery systems: Origins and key principles. Nordisk Alkohol- & Narkotikatidskrift. 2010;27:617–636. doi:10.1177/145507251002700607. [Google Scholar]
- Rush B., Tremblay J., Behrooz R., Fougere C., Perez W. Development of a needs-based planning model for substance use services and supports in Canada: Interim report. 2012 Retrieved from http://www.sken.ca/wp-content/uploads/2014/11/Appendix%20A%20hyperlinks/link13%20Needs-Based%20Planning%20Project%20-%20Interim%20Report_04MAY12.pdf.
- Rush B., Tremblay J., Brown D. Development of a needs-based planning model to estimate required capacity of a substance use treatment system. Journal of Studies on Alcohol and Drugs. 2019;Supplement 18:51–63. doi: 10.15288/jsads.2019.s18.51. doi:10.15288/jsads.2019.s18.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush B., Urbanoski K. Estimating the demand for treatment for cannabis-related problems in Canada. International Journal of Mental Health and Addiction. 2007;5:181–186. doi:10.1007/s11469-007-9061-0. [Google Scholar]
- Sareen J., Henriksen C. A., Stein M. B., Afifi T. O., Lix L. M., Enns M. W. Common mental disorder diagnosis and need for treatment are not the same: Findings from a population-based longitudinal survey. Psychological Medicine. 2013;43:1941–1951. doi: 10.1017/S003329171200284X. doi:10.1017/S003329171200284X. [DOI] [PubMed] [Google Scholar]
- Schultz S. K., Arndt S., Liesveld J. Locations of facilities with special programs for older substance abuse clients in the US. International Journal of Geriatric Psychiatry. 2003;18:839–843. doi: 10.1002/gps.994. doi:10.1002/gps.994. [DOI] [PubMed] [Google Scholar]
- Shepard D. S., Strickler G. K., McAuliffe W. E., Beaston-Blaakman A., Rahman M., Anderson T. E. Unmet need for substance abuse treatment of adults in Massachusetts. Administration and Policy in Mental Health. 2005;32:403–426. doi: 10.1007/s10488-004-1667-y. doi:10.1007/s10488-004-1667-y. [DOI] [PubMed] [Google Scholar]
- Slade T., Johnston A., Teesson M., Whiteford H., Burgess P., Pirkis J., Saw S. The mental health of Australians 2: Report on the 2007 National Survey of Mental Health and Wellbeing. 2009 Retrieved from http://www.health.gov.au/internet/publications/publishing.nsf/Content/mental-pubs-m-mhaust2-toc. [Google Scholar]
- Spence R. Analysis model for planning chemical dependence treatment systems. Journal of Substance Abuse Treatment. 2003;24:175–181. doi: 10.1016/s0740-5472(03)00023-0. doi:10.1016/S0740-5472(03)00023-0. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National survey on drug use and health. 2010 https://www.samhsa.gov/data/sites/default/files/NSDUHNationalFindingsResults2010-web/2k10ResultsRev/NSDUHresultsRev2010.pdf U.S. Department of Health and Human Services, Center for Behavioral Health Statistics and Quality. Retrieved from: [PubMed] [Google Scholar]
- Sung H., Mahoney A., Mellow J. Substance abuse treatment gap among adult parolees: Prevalence, correlates, and barriers. Criminal Justice Review. 2011;36:40–57. doi:10.1177/0734016810389808. [Google Scholar]
- Teesson M., Hall W., Slade T., Mills K., Grove R., Mewton L., Haber P. Prevalence and correlates of DSM-IV alcohol abuse and dependence in Australia: Findings of the 2007 National Survey of Mental Health and Wellbeing. Addiction. 2010:2085–2094. doi: 10.1111/j.1360-0443.2010.03096.x. doi:10.1111/j.1360-0443.2010.03096.x. [DOI] [PubMed] [Google Scholar]
- Teesson M., Slade T., Swift W., Mills K., Memedovic S., Mewton L., Hall W. Prevalence, correlates and comorbidity of DSM-IV cannabis use and cannabis use disorders in Australia. Australian and New Zealand Journal of Psychiatry. 2012;46:1182–1192. doi: 10.1177/0004867412460591. doi:10.1177/0004867412460591. [DOI] [PubMed] [Google Scholar]
- Walters G. D. Spontaneous remission from alcohol, tobacco, and other drug abuse: Seeking quantitative answers to qualitative questions. American Journal of Drug and Alcohol Abuse. 2000;26:443–460. doi: 10.1081/ada-100100255. doi:10.1081/ADA-100100255. [DOI] [PubMed] [Google Scholar]
- World Health Organization. ATLAS on substance use 2017: Resources for the prevention and treatment of substance use disorders. 2017 http://www.who.int/substance_abuse/activities/fadab/msb_adab_2017_atlas_su_25June2017.pdf Retrieved from. [Google Scholar]