Abstract
Objectives
Although forecasting a positive future can be adaptive, it may not be when expectations are unmet. Our study examined whether such inaccurate expectations about future health status (overestimation) were maladaptive for older adults who commonly experience late life declines in physical functioning.
Method
We analyzed data from the nationally representative German Aging Survey (DEAS; 1996–2011; n = 2,539; age range 60–85 years) using multilevel growth models that assessed the influence of inaccurate health expectations on older adults’ physical functioning over a 9-year period.
Results
Overestimating future health status predicted reduced day-to-day physical functioning when age, gender, and self-rated health were controlled. A Time × Overestimation interaction indicated that the negative effects of overestimation on physical functioning became more pronounced over the 9-year period.
Discussion
Results suggest that repeatedly unmet health expectations may undermine motivational resources and accelerate late life declines in physical functioning.
Keywords: Expectation accuracy, Health, Perceived control, Physical functioning
Common wisdom suggests there are benefits to looking on the bright side. This perspective is supported by evidence that shows positive expectations facilitate adaptation for individuals across the life span (Rasmussen, Scheier, & Greenhouse, 2009; Scheier & Carver, 1993; see Gallagher, Lopez, & Pressman, 2013 for a study of >150,000 participants). However, few studies have considered the health implications of unmet (inaccurate) expectations. Being too confident about (overestimating) future health status may be maladaptive for older adults who commonly experience late life declines in physical functioning (Centers for Disease Control and Prevention, 2013).
Realistic or even pessimistic health expectations may be more adaptive if anticipating such losses helps older adults prepare for and adjust to these unavoidable challenges (Lang, Weiss, Gerstorf, & Wagner, 2013; Rothbaum, Weisz, & Snyder, 1982). Based on this premise, we examined whether overestimating future health status eroded day-to-day physical functioning in older adults using 9-year data from the nationally-representative German Aging Study (DEAS). We also assessed whether overestimation effects became stronger over time given that repeatedly unmet expectations may undermine motivational resources and accelerate declines in physical functioning.
The Consequences of Inaccurate Expectations
Past research points to the detrimental consequences of unmet expectations in multiple domains that include work, education, and close relationships among others (Biehle & Mickelson, 2012; Irving & Montes, 2009; Ots, 2013; Taris, Feij, & van Vianen, 2005). Most relevant to the present study is emerging evidence on how inaccurate expectations about the future relate to health and well-being. Past studies in this domain have examined discrepancies in current versus future life satisfaction (Lachman, Röcke, Rosnick, & Ryff, 2008; Lang et al., 2013), estimated versus actual risk of heart disease or stroke (Asimakopoulou, Skinner, Spimpolo, Marsh, & Fox, 2008; Ferrer et al., 2012), or current versus future physical self (Cheng, Fung, & Chan, 2009). Results of these studies suggest that overestimating future well-being is associated with less positive and more negative affect (Asimakopoulou et al., 2008; Lachman et al., 2008), reduced psychological well-being (Cheng et al., 2009), higher intima-media thickness (and thus an increased likelihood of developing atherosclerosis; Ferrer et al., 2012), and a higher risk of disability and mortality (Lang et al., 2013).
Collectively, this research implies that overestimation reflects a specific form of inaccurate expectations that may be maladaptive. However, little is known about the long-term consequences of these inaccurate expectations since the majority of past studies did not consider whether overestimation relates to changes in well-being over time (e.g., Asimakopoulou et al., 2008; Ferrer et al., 2012; Lachman et al., 2008). Longitudinal research by Cheng et al. (2009) and Lang et al. (2013) provides stronger evidence for the detriments of overestimation, but neither study examined whether overestimation effects became more pronounced with the passage of time. Given that repeatedly unmet expectations may be particularly damaging in late life, a more systematic approach is needed to assess whether the effects of overestimating future health become stronger over time. For example, an older adult who expects her health to remain unchanged but subsequently experiences a decline may be challenged to adjust her expectations. A possible consequence of repeatedly overestimating her future health (i.e., failure to adjust expectations) may include feelings of helplessness or resignation that can undermine health engagement. Thus, adjusting expectations may serve as a protective mechanism over time.
Lacking also is an examination of discrepancies between how older adults expect their general (global) health status to change relative to how it actually changes. Previous studies have assessed expectation inaccuracy with measures ranging from those that concern specific health events (estimated vs. actual risk of heart disease; Ferrer et al., 2012) to those that concern broad measures of future selves (current vs. future physical self; Cheng et al., 2009). The importance of older adults’ global health expectations (and their inaccuracy) is implied by a 4-year study that showed global health appraisals relate to perceived control, goal engagement, and mortality in late life (Menec et al., 1999). Thus, overestimating future (global) health status may have significant consequences in late life but this issue remains unexamined in the literature.
Our 9-year study extended previous research by examining whether inaccurate global health expectations (overestimation) eroded longitudinal physical functioning in a representative sample of older German adults. Based on past research that has consistently pointed to the detriments of overestimation, we hypothesized that overestimating future health status (vs. accurate estimation/underestimation) would predict reduced physical functioning (Asimakopoulou et al., 2008; Cheng et al., 2009; Ferrer et al., 2012; Lang et al., 2013; Lachman et al., 2008). Overestimation effects were expected to become stronger over time because expectations that are repeatedly unmet may be particularly detrimental in late life. Consistent overestimates of future health status may exacerbate the consequences of health declines if they undermine adjustment in older adults who are unprepared for these difficult losses (Lang et al., 2013; Rothbaum et al., 1982). Repeated failure to anticipate such declines may also erode perceptions of control that have been shown to facilitate adaptive health-related cognitions, emotions, and behaviors for those who face late life health challenges (Chipperfield et al., 2012, 2016; Gerstorf et al., 2014; Lang & Heckhausen, 2001; Zurlo, Yoon, & Kim, 2014).
Supplemental analyses were conducted to provide an initial longitudinal test of whether accurate estimation and underestimation had differential consequences for late life physical functioning. It is possible that underestimation could be less adaptive if it reflects a lack of self-knowledge and stems from a self-fulfilling prophecy in which unrealistically pessimistic expectations compromise important health behaviors (Levy, 2009; Ryff, 2014; Ryff & Singer, 2013). However, we did not expect differences between accurate estimation and underestimation based on the rationale that both reflect humble expectations about the future that may protect late life motivational resources (Lang et al., 2013). For older adults, the self-regulation (lowering) of expectations in this manner may engender an adaptive approach to health engagement that focuses on a realistic minimization of future losses rather than an unrealistic maximization of future gains (cf., Heckhausen et al., 2013). Regardless of whether such humble expectations turn out to be accurate or underestimated, they may help older adults cope with an uncertain future if they increase preparedness for eventual health declines and facilitate adjustment when losses occur (Morling & Evered, 2006; Norem & Cantor, 1986; Rothbaum et al., 1982).
This logic is supported by empirical evidence from a 1-year study of older adults (aged 60–92) that showed no differences in well-being between those who were accurate and those who underestimated their future selves (Cheng et al., 2009). However, our supplemental analyses allowed us to consider whether accurate estimation could potentially be more adaptive than underestimation. This possibility is suggested by one study that found adults across the life span (aged 24–75) who accurately estimated their future life satisfaction reported higher psychological well-being than those who underestimated future life satisfaction (Lachman et al., 2008).
Method
Participants
We examined our research questions using data from the scientific release of the German Ageing Survey (DEAS) provided by the Research Data Centre of the German Centre of Gerontology (DZA). A detailed summary of DEAS sampling procedures and study design can be found elsewhere (see Engstler & Schmiade, 2013; see also Curtis, Huxhold, & Windsor, in press). Briefly, the DEAS is an ongoing (1996–2011) nationally representative panel study of 40+ year old community-dwelling German adults stratified by age (40–54, 55–69, and 70–85 years old), gender, and geographical location (East/West). New baseline samples were assessed in 1996, 2002, and 2008 and all willing participants were reassessed in 2002, 2008, and 2011. Sample size was 4,838 in 1996, 5,194 in 2002 (3,670 new participants and 1,524 reassessed), 8,200 in 2008 (6,205 new participants and 1,995 reassessed), and 4,855 in 2011 (0 new and 4,855 reassessed).
Inclusion criteria for the present study were that participants (a) were 60+ years old at time of first interview and (b) had at least one rating of expected health change in 1996, 2002, or 2008 and a corresponding rating of actual health change at the following wave in 2002, 2008, or 2011 (e.g., 2002 overestimation = 1996 expected health change—2002 actual health change). In other words, 60+ year old participants were included in the present study if they had one or more overestimation scores. Participants could contribute a maximum of three scores (2002, 2008, and 2011) which enabled us to examine the association between overestimation and late life physical functioning over a 9-year period. In total, 2,539 participants between 60 and 85 years of age (M = 68.83; 45% female) who provided 3,180 observations were included in the analyses (see Table 1 for details).
Table 1.
Descriptive Statistics and Correlations (n = 2,539)
| Correlations | |||||||
|---|---|---|---|---|---|---|---|
| M (SD) or % | Range | 1 | 2 | 3 | 4 | 5 | |
| 1. Age | 68.83 (6.10) | 60–85 | – | ||||
| 2. Female | 45% | 0–1 | −.05* | – | |||
| 3. Health | 3.40 (0.72) | 1–5 | −.14* | −.01 | – | ||
| 4. Overestimation | 40% | 0–1 | .03 | .03 | −.31* | – | |
| 5. Physical Functioning | 75.22 (25.81) | 0–100 | −.29* | −.14* | .58* | −.27* | – |
Note: *p < .01.
Measures
Physical functioning (PF-10)
Physical functioning was assessed at each wave using the respective 10-item subscale (PF-10) of the Short-Form Health Survey (SF-36; Ware & Sherbourne, 1992). The PF-10 measured participants’ ability to perform 10 physical activities in daily life (e.g., walking one block, bathing). Scores ranged from 0 to 100 with higher scores reflecting better day-to-day physical functioning.
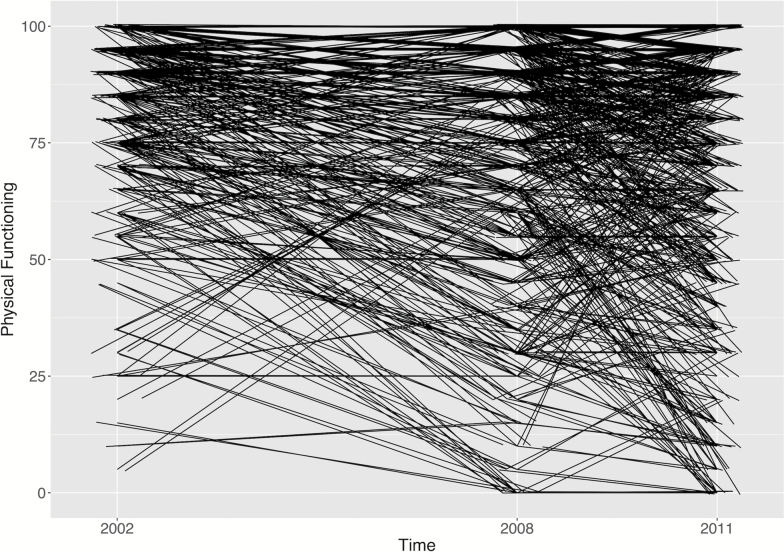
Previous research has established the reliability and validity of the PF-10 across diverse populations in more than 12 countries (see McHorney, Ware, & Raczek, 1993; McHorney, Ware, Lu, & Sherbourne, 1994; Ware, 2000; White, Wilson, & Keysor, 2011). Supporting its convergent validity in older populations, the PF-10 is a strong correlate of objective indicators of physical functioning such as balance (single limb stance; r = .42), gait speed (r = .75), and mobility (Timed Up and Go Test; r = −.70; see Bohannon & DePasquale, 2010; White et al., 2011). In line with previous research (α = .93; McHorney et al., 1994), the PF-10 was internally consistent at each wave (α2002 = .92, α2008 = .92, α2011 = .93) and showed acceptable stability over the present 3–6-year assessment intervals (test-retest r2002–2008 = .55, r2008–2011 = .72). See Figure 1 for a plot of individual PF-10 trajectories across measurement occasions. Note that trajectories have been “jittered” (raised by a minute, varying value) to facilitate visualization of overlapping lines (see Schilling et al., 2013).
Figure 1.
Individual trajectory plot of physical functioning across measurement occasions.
Health overestimation
Expected health change (EHC; “How do you expect your state of health to change in the future?”) and actual health change were assessed at each wave (AHC; “How has your state of health changed over the past 3/6 years?”; from 1996 to 2002, from 2002 to 2008, from 2008 to 2011). Both items were answered on a five-point scale (1 = will improve greatly or has improved greatly, 5 = will get much worse or has gotten much worse). Items were reverse coded and difference scores calculated by subtracting AHC from EHC for three time frames: 1996 (EHC)—2002 (AHC); 2002 (EHC)—2008 (AHC); and 2008 (EHC)—2011 (AHC). Positive scores indicated an overestimate of future health status (i.e., future health was expected to be better than it actually was 3 or 6 years later), zero indicated an accurate estimate of future health status, and negative scores reflected an underestimate of future health status. Difference scores were dichotomized based on conceptual, empirical, and statistical considerations and indicated whether participants had overestimated their health for each time frame (0 = accurately estimated or underestimated future health status, 1 = overestimated future health status).
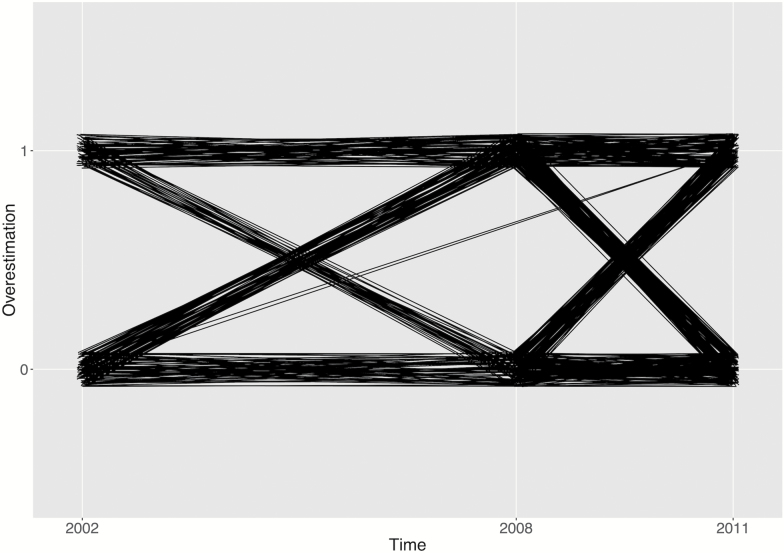
Conceptually, no differences were expected between accurate estimation and underestimation because both reflect humble expectations that should help older adults cope with uncertainty by facilitating preparedness and protecting motivational resources when losses occur (Lang et al., 2013; Norem & Cantor, 1986). Empirically, t tests showed that those who accurately estimated health did not differ from those who underestimated health with respect to the covariate measures of age, gender, or self-rated health (all ps > .50). Statistically, relatively few participants underestimated their future health status (15%) which results in disproportionate group sizes when older adults are separated into three categories (accurate estimation, underestimation, and overestimation). See Figure 2 for a plot of individual overestimation trajectories across measurement occasions. Trajectories have been “jittered” (raised by a minute, varying value) to facilitate visualization of overlapping lines (see Schilling et al., 2013).
Figure 2.
Individual trajectory plot of overestimation across measurement occasions (0 = accurate estimation/underestimation, 1 = overestimation).
Covariates
Chronological age (M = 68.83) at the first measurement point, gender (0 = male, 1 = female; 45% female), and self-rated health were included as covariates in the analyses. Self-rated health was assessed at each wave (“How would you rate your present state of health?”) using a five-point scale (1 = very good, 5 = very bad). The measures from 2002, 2008, and 2011 were reverse coded and a mean-weighted composite of self-rated health was generated with higher scores indicating better health over a 9-year period.
Results
Descriptive statistics and intercorrelations are reported in Table 1. Physical functioning was positively associated with better health (r = .58) and negatively associated with age (r = −.29) and being female (r = −.14). Overestimating future health was negatively associated with physical functioning (r = −.27). This indicates that overestimation was as strong a correlate of physical functioning as the sociodemographic factors (chronological age, gender).
Main Analyses
Multilevel growth models were estimated with Mplus 7 (Muthén & Muthén, 1998–2015) to assess change in physical functioning over a 9-year period. We estimated two-level models with measurement occasions (Level 1) nested within participants (Level 2). Health overestimation and time were included as time-varying (Level 1) predictors. A Time × Overestimation interaction was also included to assess whether longitudinal changes in physical functioning could be explained by overestimating future health status. The Level 1 equation that included the interaction term was specified as follows:
Gender, age, and self-rated health were included as time-independent (Level 2) predictors. Age and self-rated health were grand-mean centered. Level 1 intercepts and slopes were allowed to vary between participants. Level 2 equations that included the interaction term were specified as follows:
Table 2 shows the results of the main effect (Model 1) and interaction effect models (Model 2). Model 1 indicated that physical functioning was lower for those who were older (−.94), female (−7.31), and overestimated future health status (−4.85), whereas it was higher for individuals with better self-rated health (19.44). The time slope showed a linear decrease in physical functioning for each year since the first measurement (−.50). This indicates that functioning declined by 4.50 units for the average participant over the 9-year follow-up.
Table 2.
Multilevel Regression Growth Models Predicting Change in Physical Functioning (n = 2,539)
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| B | SE | B | SE | |
| Intercept | 83.93** | 0.86 | 82.74** | 0.97 |
| Time-Independent Predictors | ||||
| Age | −0.94** | 0.07 | −0.94** | 0.07 |
| Female | −7.31** | 0.75 | −7.34** | 0.75 |
| Health | 19.44** | 0.63 | 19.42** | 0.63 |
| Time-Varying Predictors | ||||
| Time | −0.50** | 0.11 | −0.32* | 0.12 |
| Overestimation | −4.85** | 0.78 | −1.72 | 1.59 |
| Time × Overestimation | −0.49* | 0.22 | ||
Note: *p < .05. **p < .01.
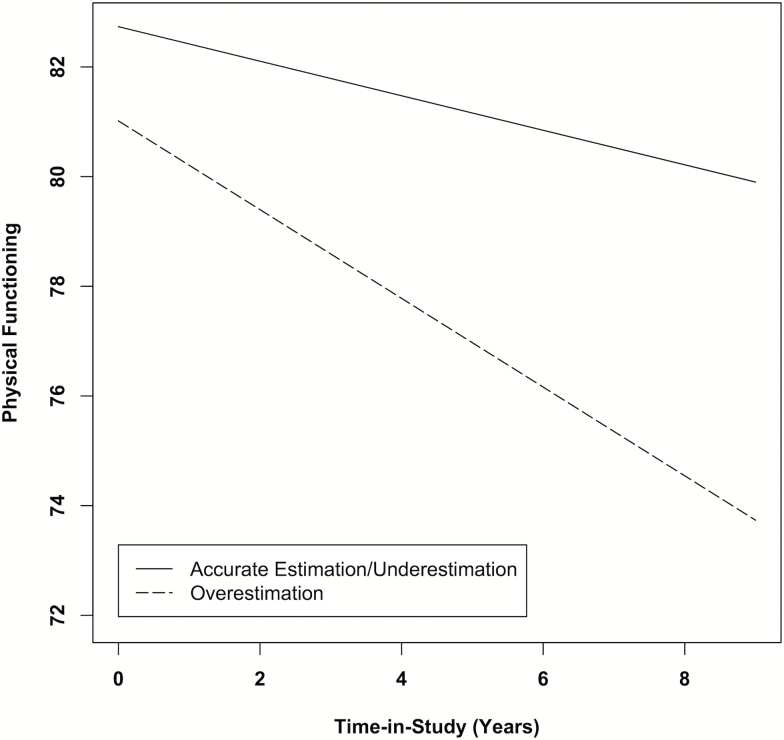
Model 2 revealed a significant Time × Overestimation interaction (−.49) that showed older adults who overestimated their future health status experienced more pronounced declines in physical functioning over time (see Figure 3). Simple slope analyses probed the interaction and showed the negative effect of overestimation on physical functioning became stronger at each successive wave: B = −1.72, SE = 1.59, p = .278 at Wave 1 (2002); B = −4.68, SE = 0.78, p < .001 at Wave 2 (2008); B = −6.17, SE = 0.97, p < .001 at Wave 3 (2011).
Figure 3.
The interaction of time and health overestimation on changes in physical functioning over a 9-year period.
We also probed the Time × Overestimation interaction by examining the effect of time on physical functioning for older adults who overestimated (vs. accurately estimated or underestimated) their future health. Simple slope analyses showed that time had a strong effect for those who overestimated health (B = −0.81, SE = 0.19, p < .001) in contrast to a small effect for those who accurately estimated or underestimated health (B = −0.32, SE = 0.12, p = .011). This indicates that functioning declined by 7.29 units for older adults who overestimated their future health over the 9-year follow-up (vs. a 2.88 unit decline for those who accurately or underestimated it).
Supplemental Analyses
Supplemental multilevel growth models examined whether accurate estimation and underestimation had differential consequences for physical functioning. Analyses were conducted using dummy-coded variables that reflected accurate estimation, underestimation, and overestimation (reference group = underestimation). As expected, Model 1 (main effect) results showed physical functioning did not differ between those who accurately estimated health and those who underestimated health (B = 0.12, SE = 0.94, p = .902). Model 1 results also indicated those who overestimated health had lower physical functioning than those who underestimated health (B = −4.89, SE = 1.07, p < .001). As expected, Model 2 (interaction) results showed there was no Time × Accurate Expectations interaction (B = 0.17, SE = 0.27, p = .520). This indicates that changes in physical functioning over time did not differ between those who accurately estimated health and those who underestimated health. Model 2 also revealed a significant Time × Overestimation interaction that showed those who overestimated health experienced more pronounced declines in physical functioning over time relative to those who underestimated health (B = −0.61, SE = 0.29, p = .036).
Supplemental growth models also assessed whether results from the main analyses were consistent when (a) overestimation was treated as a continuous variable (higher scores = greater overestimation), (b) an alternate overestimation measure was used that captured expected health change versus present state of health rated several years later (rather than expected health change vs. actual health change rated several years later), (c) several additional variables that may relate to overestimation and physical functioning were controlled, and (d) self-rated health was included as a time varying covariate.
Results of the continuous variable analyses were consistent with the main analyses and revealed a Model 1 overestimation main effect (B = −2.59, SE = 0.39, p < .001) and a Model 2 Time × Overestimation interaction (B = −0.22, SE = 0.11, p = .043). Findings from the alternate overestimation measure analyses (expected health change vs. present health) were also consistent and yielded a Model 1 overestimation main effect (B = −8.65, SE = 1.57, p < .001) and a marginal Model 2 Time × Overestimation interaction (B = −.79, SE = 0.42, p = .062). Results of the covariate analyses showed the Model 1 overestimation main effect (B range = −4.65 to −4.85, all ps < .001) and the Model 2 Time × Overestimation interaction remained significant when controlling for health behaviors such as physician visits (interaction B = −0.49, p = .025) and smoking (interaction B = −0.50, p = .026), as well as subjective age (interaction B = −0.51, p = .021), self-efficacy (interaction B = −0.69, p = .008), and a proxy variable for neuroticism (extent to which participants felt upset; interaction B = −0.50, p = .027). Findings were also consistent when self-rated health was included in the model as a time-varying covariate: Model 1 overestimation main effect (B = −3.74, p < .001), Model 2 Time × Overestimation interaction (B = −0.42, p = .035).
Discussion
Although forecasting a positive future can be adaptive, unmet expectations may pose a threat to adjustment. Particularly in late life, realistic or even pessimistic expectations about future health status may be beneficial if they help individuals to psychologically prepare for eventual declines and thereby soften the blow. Anticipating such declines may help to cope with uncertainty and facilitate adaptation if they enable older adults to accept and adjust to difficult losses before they occur (Morling & Evered, 2006; Rothbaum et al., 1982; see also Norem & Cantor, 1986).
Our findings support this logic in that failure to anticipate health declines (overestimation) was linked to reduced physical functioning when controlling for health status, age, and gender. These results support recent studies that underscore the importance of considering both the valence and accuracy of expectations (Cheng et al., 2009; Lang et al., 2013). Our study also extends previous research by showing that overestimation (expectation inaccuracy) had negative consequences for physical functioning across an extended time period that involved multiple assessments of both predictor and outcome variables.
Measuring overestimation (predictor) and everyday physical functioning (outcome) on several occasions enabled an initial test of whether overestimation effects change with time. Multilevel growth model results supported our hypotheses and showed that the detriments of overestimating future health status became more pronounced over a 9-year period. The negative effect of overestimation on physical functioning increased more than threefold during the course of the study (from B = −1.72 in 2002 to B = −6.17 in 2011). Stated differently, day-to-day physical functioning declined by 7.29 units for older adults who overestimated their future health (relative to 2.88 units for those who accurately or underestimated it). These results suggest health expectations that are repeatedly disconfirmed may be especially damaging in late life. Consistently unmet expectations may precipitate feelings of helplessness (perceived lack of control) that can erode motivational resources and exacerbate the negative consequences of deteriorating health (Abramson, Garber, & Seligman, 1980; Chipperfield, Perry, & Stewart, 2012).
Our results also contribute to a growing literature showing the benefits of humble expectations in late life (e.g., Asimakopolou et al., 2008; Cheng et al., 2009; Ferrer et al., 2012). We found that increasing age did not relate to more humble expectations (r = .03), which is in contrast to a small age-expectations correlation (r = −.15) reported by Lang et al. (2013) in a sample that encompassed the adult life span (18–98 years). This implies that a large age range is needed to capture an age gradient in expectations. Even so, it is notable that 40% of our 60–85-year-old sample overestimated their health across occasions (see Table 1). This suggests that a sizable minority of individuals do not develop humble expectations. Thus, many older adults may struggle to calibrate health expectations even after years of experience.
Lowering expectations about future health may be an important form of self-regulation for older adults who face the prospect of health declines (Centers for Disease Control and Prevention, 2013). The maintenance of realistic or somewhat pessimistic expectations may represent a low risk (safe) strategy that focuses on the minimization of future losses and thereby protects motivational resources (cf. Heckhausen et al., 2013). Such humble expectations may be adaptive whether or not they are accurate: If older adults’ expectations about health decline are inaccurate, the discrepancy is in their favor in that health is better than anticipated. If their expectations about decline are accurate, they had the foresight to anticipate these losses and may be better prepared for and able to adjust to poor health (Chipperfield, Hamm, Perry, & Ruthig, 2017; Rothbaum et al., 1982).
Our supplemental findings are consistent with this rationale in that they revealed no differences in physical functioning between older adults who accurately estimated their health and those who underestimated it. These results contribute to the expectation accuracy literature in that few studies have directly examined whether accurate estimation and underestimation have distinct consequences. Those that have were based on single-assessments of expectation accuracy, and the results were inconsistent: Lachman et al. (2008) found that accurate estimation was more adaptive than underestimation, whereas, consistent with our supplemental results, Cheng et al. (2009) found no differences between accurate estimation and underestimation.
Sample age may help to explain this discrepancy. Lachman et al.'s (2008) life-span sample was comprised of adults aged 24–75, whereas Cheng et al.’s (2009) sample was comprised of older adults aged 60–92 similar to our sample of 60–85-year olds. It could be that underestimation—which typically reflects more pessimistic expectations—is less adaptive in early and middle adulthood when opportunities to shape one’s development are at their peak (Heckhausen, Wrosch, & Schulz, 2010). Expecting too little (and overachieving) at this stage of the life span may undermine rather than sustain motivation (cf. Taylor & Brown, 1988). Underestimation may become more adaptive as individuals encounter increasing constraints in later life. In old age, underestimation (as well as accurate estimation) could protect motivational resources that are challenged by functional declines if such humble expectations help individuals focus on a realistic minimization of future losses (Heckhausen et al., 2013).
One caveat when interpreting our findings is that health status and physical functioning (PF-10) were self-reported rather than objectively assessed. However, previous research has established the reliability and validity of both these self-report measures. Systematic reviews and meta-analyses provide strong evidence for the validity of self-rated health and show it is an excellent predictor of all-cause mortality, even when controlling for objective health measures such as diagnosed diseases and functional abilities (DeSalvo, Bloser, Reynolds, He, & Muntner, 2006; Idler & Benyamini, 1997; see also Schnittker & Bacak, 2014). For instance, DeSalvo et al.’s (2006) meta-analysis revealed adults with “poor” self-rated health had a twofold higher risk of mortality than those with “excellent” health. Past studies have also consistently shown the PF-10 to be a valid measure of physical functioning that is a strong correlate of relevant objective indicators such as balance (single limb stance; r = .42), gait speed (r = .75), and mobility (Timed Up and Go Test; r = −.70; see Bohannon & DePasquale, 2010; Ware, 2000; White et al., 2011). Nonetheless, further research is needed to extend our study by examining whether the pattern of results is consistent for older adults who overestimate objective future health status.
A second caveat when interpreting our findings is that expectations and their accuracy may have changed multiple times during the present 3–6-year assessment periods. Future research should assess overestimation over shorter time intervals (e.g., monthly or annually) to better capture fine-grained adjustments that occur in day-to-day life. A final limitation is that personality variables such as neuroticism that may relate to overestimation and physical functioning were not available in the DEAS study. However, our findings were consistent when a rough proxy variable for neuroticism was controlled (extent to which participants felt upset).
Implications
The present study has implications for the development of treatment interventions for older adults who face age-related health declines. Some evidence suggests cognitive interventions designed to increase expectations about future health (e.g., attributional retraining) may help prevent late life physical decline (Sarkisian, Prohaska, Davis, & Weiner, 2007; see Perry, Chipperfield, Hladkyj, Pekrun, & Hamm, 2014 and Perry & Hamm, 2017 for reviews of attribution-based interventions). Our findings highlight the importance of incorporating an intervention component that encourages older adults to maintain modest expectations about potential health improvements. Such expectations about intervention efficacy may protect against disappointment when setbacks occur and produce more sustainable health benefits.
Funding
This work was supported by a Social Sciences and Humanities Research Council of Canada (SSHRC) Doctoral Fellowship, a SSHRC Michael Smith Foreign Study Supplement, and a SSHRC Postdoctoral Fellowship to J. M. Hamm; a Canadian Institutes of Health Research (MOP-130382) grant to J. G. Chipperfield; a SSHRC Insight Grant (435-2012-1143) and a Royal Society of Canada and Alexander von Humboldt Research Grant to R. P. Perry; and a VolkswagenStiftung Research Grant (Az. 86 759) to F. R. Lang. Study data are from the scientific release of the German Ageing Survey (DEAS), provided by the Research Data Centre (FDZDZA) of the German Centre of Gerontology (DZA).
References
- Abramson L. Y., Garber J., & Seligman M. E. P (1980). Learned helplessness in humans: An attributional analysis. In Garber J., & Seligman M. E. P. (Eds.), Human helplessness: Theory and applications (pp. 3–34). New York: Academic Press. [Google Scholar]
- Asimakopoulou K. G. Skinner T. C. Spimpolo J. Marsh S. & Fox C (2008). Unrealistic pessimism about risk of coronary heart disease and stroke in patients with type 2 diabetes. Patient Education and Counseling, 71, 95–101. doi:10.1016/j.pec.2007.12.007 [DOI] [PubMed] [Google Scholar]
- Biehle S. N. & Mickelson K. D (2012). First-time parents’ expectations about the division of childcare and play. Journal of Family Psychology: JFP, 26, 36–45. doi:10.1037/a0026608 [DOI] [PubMed] [Google Scholar]
- Bohannon R. W. & DePasquale L (2010). Physical Functioning Scale of the Short-Form (SF) 36: Internal consistency and validity with older adults. Journal of geriatric physical therapy (2001), 33, 16–18. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention.(2013). The state of aging and health in America 2013. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services. [Google Scholar]
- Cheng S. T. Fung H. H. & Chan A. C (2009). Self-perception and psychological well-being: The benefits of foreseeing a worse future. Psychology and Aging, 24, 623–633. doi:10.1037/a0016410 [DOI] [PubMed] [Google Scholar]
- Chipperfield J. G., Hamm J. M., Perry R. P., & Ruthig J. C (2017). Perceived control. In Robinson M. D. & Eid M. (Eds.), The happy mind: Cognitive contributions to well-being.New York: Springer. [Google Scholar]
- Chipperfield J. G. Newall N. E. Perry R. P. Stewart T. L. Bailis D. S. & Ruthig J. C (2012). Sense of control in late life: Health and survival implications. Personality & Social Psychology Bulletin, 38, 1081–1092. doi:10.1177/0146167212444758 [DOI] [PubMed] [Google Scholar]
- Chipperfield J. G., Perry R. P., & Pekrun R. H., Barchfeld P., Lang F. R., & Hamm J. M (2016). Paradoxical effects of perceived control on health behavior. PLoS One, 11, 1–16. doi:10.1371/journal.pone.0148921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chipperfield J. G., Perry R. P., & Stewart T. L (2012). Perceived control. In Ramachandran V. S. (Ed.), Encyclopedia of human behavior (2nd edn., pp. 42–48). San Diego, CA: Academic Press. doi:10.1016/B978-0-12-375000-6.00109-9 [Google Scholar]
- Curtis R. G., Huxhold O., & Windsor T. D (in press). Perceived control and social activity in midlife and older age: A reciprocal association? Findings from the German Ageing Survey. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73, 807-815. doi:10.1093/geronb/gbw070 [DOI] [PubMed] [Google Scholar]
- DeSalvo K. B. Bloser N. Reynolds K. He J. & Muntner P (2006). Mortality prediction with a single general self-rated health question. A meta-analysis. Journal of General Internal Medicine, 21, 267–275. doi:10.1111/j.1525-1497.2005.00291.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engstler H., & Schmiade N (2013). The German Ageing Survey (DEAS)—A longitudinal and time-series study of people in the second half of life. Schmollers Jahrbuch, Zeitschrift für Wirtschafts-und Sozialwissenschaften, 133, 97–107. doi:10.3790/schm.133.1.97 [Google Scholar]
- Ferrer R. A. Klein W. M. Zajac L. E. Sutton-Tyrrell K. Muldoon M. F. & Kamarck T. W (2012). Unrealistic optimism is associated with subclinical atherosclerosis. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 31, 815–820. doi:10.1037/a0027675 [DOI] [PubMed] [Google Scholar]
- Gallagher M. W. Lopez S. J. & Pressman S. D (2013). Optimism is universal: Exploring the presence and benefits of optimism in a representative sample of the world. Journal of Personality, 81, 429–440. doi:10.1111/jopy.12026 [DOI] [PubMed] [Google Scholar]
- Gerstorf D. Heckhausen J. Ram N. Infurna F. J. Schupp J. & Wagner G. G (2014). Perceived personal control buffers terminal decline in well-being. Psychology and Aging, 29, 612–625. doi:10.1037/a0037227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckhausen J. Wrosch C. & Schulz R (2010). A motivational theory of life-span development. Psychological Review, 117, 32–60. doi:10.1037/a0017668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckhausen J. Wrosch C. & Schulz R (2013). A lines-of-defense model for managing health threats: A review. Gerontology, 59, 438–447. doi:10.1159/000351269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E. L. & Benyamini Y (1997). Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38, 21–37. doi:10.2307/2955359 [PubMed] [Google Scholar]
- Irving G. P., & Montes S. D (2009). Met expectations: The effects of expected and delivered inducements on employee satisfaction. Journal of Occupational and Organizational Psychology, 82, 431–451. doi:10.1348/096317908X312650 [Google Scholar]
- Lachman M. E. Röcke C. Rosnick C. & Ryff C. D (2008). Realism and illusion in Americans’ temporal views of their life satisfaction: Age differences in reconstructing the past and anticipating the future. Psychological Science, 19, 889–897. doi:10.1111/j.1467-9280.2008.02173.x [DOI] [PubMed] [Google Scholar]
- Lang F. R. & Heckhausen J (2001). Perceived control over development and subjective well-being: Differential benefits across adulthood. Journal of Personality and Social Psychology, 81, 509–523. doi:10.1037/0022-3514.81.3.509 [DOI] [PubMed] [Google Scholar]
- Lang F. R., Weiss D., Gerstorf D., & Wagner G. G (2013). Forecasting life satisfaction across adulthood: Benefits of seeing a dark future?Psychology and Aging, 28, 249–261. doi:10.1037/a0030797 [DOI] [PubMed] [Google Scholar]
- Levy B. (2009). Stereotype embodiment: A psychosocial approach to aging. Current Directions in Psychological Science, 18, 332–336. doi:10.1111/j.1467-8721.2009.01662.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menec V. H. Chipperfield J. G. & Perry R. P (1999). Self-perceptions of health: A prospective analysis of mortality, control, and health. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 54, P85–P93. doi:10.1093/geronb/54B.2.P85 [DOI] [PubMed] [Google Scholar]
- McHorney C. A. Ware J. E. Jr, & Raczek A. E (1993). The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31, 247–263. doi:10.1097/00005650-199303000-00006 [DOI] [PubMed] [Google Scholar]
- McHorney C. A., Ware J. E., Lu J. F. R., & Sherbourne C. D (1994). The MOS 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care, 32, 40–66. doi:10.1097/00005650-199401000-00004 [DOI] [PubMed] [Google Scholar]
- Morling B. & Evered S (2006). Secondary control reviewed and defined. Psychological Bulletin, 132, 269–296. doi:10.1037/0033-2909.132.2.269 [DOI] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (1998-2015). Mplus user’s guide (7th ed.). Los Angeles: Muthén & Muthén. [Google Scholar]
- Norem J. K. & Cantor N (1986). Defensive pessimism: Harnessing anxiety as motivation. Journal of Personality and Social Psychology, 51, 1208–1217. doi:10.1037/0022-3514.51.6.1208 [DOI] [PubMed] [Google Scholar]
- Ots A. (2013). Third graders’ performance predictions: Calibration deflections and academic success. European Journal of Psychology of Education, 28, 223–237. doi:10.1007/s10212-012-0111-z [Google Scholar]
- Perry R. P., Chipperfield J. G., Hladkyj S., Pekrun R., & Hamm J. M (2014). Attribution-based treatment interventions in some achievement settings. In Karabenick S. & Urdan T. (Eds.), Motivational interventions (Vol. 18). Bingley, UK: Emerald Publishing. doi:10.1108/S0749-742320140000018000 [Google Scholar]
- Perry R. P. & Hamm J. M (2017). An attribution perspective on competence and motivation: Theory and treatment interventions. In Elliot A., Dweck C., & Yeager D. (Eds.), Handbook of competence and motivation (2nd Edition): Theory and applications. New York: Guilford Press. [Google Scholar]
- Rasmussen H. N. Scheier M. F. & Greenhouse J. B (2009). Optimism and physical health: A meta-analytic review. Annals of Behavioral Medicine: A publication of the Society of Behavioral Medicine, 37, 239–256. doi:10.1007/s12160-009-9111-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum F., Weisz J. R., & Snyder S. S (1982). Changing the world and changing the self: A two-process model of perceived control. Journal of Personality and Social Psychology, 42, 5–37. doi:10.1037/0022-3514.42.1.5 [Google Scholar]
- Ryff C. D. (2014). Psychological well-being revisited: Advances in the science and practice of eudaimonia. Psychotherapy and Psychosomatics, 83, 10–28. doi:10.1159/000353263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff C. D., & Singer B. H (2013). Know thyself and become what you are: A eudaimonic approach to psychological well-being. In Delle Fave A. (Ed.), The exploration of happiness (pp. 97–116). New York: Springer. doi:10.1007/978-94-007-5702-8_6 [Google Scholar]
- Sarkisian C. A. Prohaska T. R. Davis C. & Weiner B (2007). Pilot test of an attribution retraining intervention to raise walking levels in sedentary older adults. Journal of the American Geriatrics Society, 55, 1842–1846. doi:10.1111/j.1532-5415.2007.01427.x [DOI] [PubMed] [Google Scholar]
- Scheier M. F., & Carver C. S (1993). On the power of positive thinking: The benefits of being optimistic. Current Directions in Psychological Science, 2, 26–30. doi:10.1111/1467–8721.ep10770572 [Google Scholar]
- Schilling O. K. Wahl H. W. Boerner K. Reinhardt J. P. Brennan-Ing M. & Horowitz A (2013). Change in psychological control in visually impaired older adults over 2 years: Role of functional ability and depressed mood. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 68, 750–761. doi:10.1093/geronb/gbs118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittker J., & Bacak V (2014). The increasing predictive validity of self-rated health. PLoS One, 9, 1–11. doi:10.1371/journal.pone.0084933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taris R., Feij J. A., & van Vianen A. E (2005). Met expectations and supplies–values fit of Dutch young adults as determinants of work outcomes. The International Journal of Human Resource Management, 16, 366–382. doi:10.1080/0958519042000339552 [Google Scholar]
- Taylor S. E. & Brown J. D (1988). Illusion and well-being: A social psychological perspective on mental health. Psychological Bulletin, 103, 193–210. doi:10.1037/0033-2909.103.2.193 [PubMed] [Google Scholar]
- Ware J. (2000). SF-36 health survey update. Spine, 24, 3130–3139. doi:10.1097/00007632-200012150-00008 [DOI] [PubMed] [Google Scholar]
- Ware J. E. Jr, & Sherbourne C. D (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30, 473–483. doi:10.1097/00005650-199206000-00002 [PubMed] [Google Scholar]
- White D. K. Wilson J. C. & Keysor J. J (2011). Measures of adult general functional status. Arthritis Care & Research, 63, S297–S307. doi:10.1002/acr.20638 [DOI] [PubMed] [Google Scholar]
- Zurlo K. A. Yoon W. & Kim H (2014). Unsecured consumer debt and mental health outcomes in middle-aged and older Americans. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69, 461–469. doi:10.1093/geronb/gbu020 [DOI] [PubMed] [Google Scholar]