Abstract
Aims:
To examine child outcomes over time among mothers with perinatally depressed mood in rural South Africa (SA).
Methods:
A representative sample of consecutive births (470/493) in the OR Tambo District of the Eastern Cape of South Africa (SA) were recruited and were reassessed at five points over the course of the next two years: 85% were reassessed at 3 months, 92% at 6 months, 88% at 9 months, 91% at 12 months, and 88% at 2 years post-birth. Over time, the children of mothers with perinatally depressed mood (16%) were compared to children of mothers without depressed mood using multiple linear and logit regressions.
Results:
Mothers with perinatal depressed mood are significantly less likely to live with the child’s father or their in-laws (23% vs 35%), have household incomes above 2000 ZAR (154 USD) (31% vs 51%), and significantly more likely to have experienced IPV prior (19% vs. 9%) and during (32% vs. 20%) pregnancy compared to mothers without depressed mood. There are no differences in age, education, primipara, HIV status (29% seropositive), or alcohol use. Growth and developmental delays and motor and speech milestones through 24 months post-birth are similar for mothers with and without perinatal depressed mood.
Conclusions:
Despite increased economic and partner difficulties associated with perinatal depressed mood, infant outcomes are similar in mothers with and without depressed mood in rural South Africa.
Keywords: Depression, families, health outcomes, rural regions, women, children, low and middle income countries, South Africa
Introduction
The negative consequences of perinatal depression on mothers and their children are well-established in high income countries (HIC) (Brand, Brennan, 2009; Diego et al., 2004; Steer, Scholl, Hediger, Fischer,1992) and in more recent studies in low-and middle-income countries (LMIC) (Stein et al., 2014; Fisher et al., 2012). A recent meta-analytic review of the prevalence of perinatal depression globally (n = 17 countries) suggests prevalence rates of 5–30% in LMIC (Fisher et al., 2012). In South Africa, several studies in peri-urban settlements near Cape Town report high rates of perinatal depression with over 30% of pregnant women reporting depressive symptoms (Honikman, Van Heyningen, Field, Baron, Tomlinson, 2012; Rochat, Tomlinson, Bärnighausen, Newell, Stein, 2011; Rotheram-Borus et al., 2011). However, less is known about the rates of depression among pregnant women in rural areas.
In rural regions of LMIC, there are many challenges facing mothers. Maternal depression has been linked to poverty, age, prior history of mental health problems, having unintended children, and intimate partner violence (Fisher et al., 2012). In the Eastern Cape, poverty is pervasive and mothers often care for their children without their partners who migrate in search of work (Posel, Devey, 2006). Partner support is limited both financially and emotionally and intimate partner violence is also prevalent in this region (Nduna, Jewkes, Dunkle, Shai, 2010). With scarce employment opportunities and partner support, government assistance provided with the child support grant (CSG) is essential for all mothers. However, applying for this grant requires mothers to submit an application that includes their own identification documents and their child’s birth certificate to the nearest South African Social Security Agency office. This process can be difficult in geographically isolated areas such as the Eastern Cape, where mothers have large distances to travel and limited means of transportation. Considering the importance of this financial support in low-resource areas, we examine the time it takes mothers to obtain the CSG in the Eastern Cape.
Further, mothers living with HIV have been found to have higher rates of depression (Rotheram-Borus et al., 2011; Dyer, Stein, Rice, Rotheram-Borus, 2012; le Roux et al., 2013). In SA, pregnancy is the period during which young women are most likely to find out their HIV status – more than 98% of women will get tested for HIV while attending antenatal care (2013 National Antenatal Sentinel HIV Prevalence Survey). In the Eastern Cape, nearly one in three mothers will learn that they are HIV positive which places them and their child at lifelong risk for premature death and negative health outcomes (Rochat et al., 2006; Grapsa, Zaidi, Newell, 2013). Concurrently, 25% of mothers in peri-urban townships near Cape Town drink alcohol while pregnant (Rotheram-Borus et al., 2015; Tomlinson et al., 2014). Although alcohol use among pregnant mothers in rural areas is less understood, homemade alcohol is a common economic activity in this area (Fieldgate et al., 2013). This can serve as a source of household income and possibly increase the risk for use and dependency. In this study, we examined the structural, health, and risk factors between mothers reporting perinatally depressed and non-depressed moods in a South African rural setting.
Maternal depression affects the well-being of the mothers as well as their children. Low birth weight, shorter duration of breastfeeding, undernutrition, and diarrhea have been associated with maternal depression (Rahman Bunn, Lovel, Creed, 2007; Rahman, Malik, Sikander, Roberts, Creed, 2008; Rahman, Iqbal, Roberts, Husain, 2009). Children’s poor growth has been consistently linked to maternal depression in Southern Asian countries but has more inconsistent patterns in African nations (Patel, Rahman, Jacob, Hughes, 2004; Parsons, Young, Rochat, Kringelbach, Stein, 2012; Rahman et al., 2009). Depressed mothers living with HIV, even when children are uninfected with HIV, have children with poor growth (Stein et al., 2014). A recent meta-analysis reported a small but significant effect when assessing the influence of perinatal depression on cognitive functioning in children but a larger effect when considering postnatal maternal depression (Fisher et al., 2012).
This article examines the influence of perinatal depression on child outcomes through the first two years of life among a population cohort of mothers in a rural region in the Eastern Cape of South Africa. Having repeated assessments of this population cohort allowed us to examine multiple child outcomes over 24 months. We hypothesized that mothers experiencing perinatal depressed mood may have less structural resources (e.g., income, formal housing) and experience more risk (e.g., IPV, alcohol use). With these challenges, mothers with depressed mood may be less able to caretake for their children, resulting in developmental delays.
Methods
The study was conducted with approval of the Institutional Review Board of the Stellenbosch University (N12/08/046) and permission was granted by the Eastern Cape Department of Health to recruit in government health facilities.
Setting.
Zithulele Hospital in the King Sabata Dalindyebo (KSD) Sub-district of the OR Tambo District of the Eastern Cape of SA serves a population of approximately 130,000 and is the referral centre that provides training infrastructure for staff at 14 surrounding health clinics and it serves one of the two poorest municipalities in SA (BusinessTech, 2016).
Between January and April of 2013, a consecutive series of mothers giving birth at Zithulele Hospital and its 10 closest clinics were approached to participate in a birth cohort study. In addition, mothers who delivered at home (10.1%) or on the way to a health facility (3.2%) who sought follow-up care at one of these clinics were also approached. Mothers who travelled to the hospital from outside this catchment area to give birth at the hospital were excluded from the sample, due lack of funding for distant follow up. Voluntary informed consent was obtained from 95% of mothers (470/493 live births; 5% refusal/exclusion rate) and, in the case where the mother was less than 18 years old, consent was obtained from the adolescent mother and one of her parents/guardians. Mothers were approached while still in the hospital and interviewed in the first few days following birth. Mothers giving birth at clinics were assessed within the first week following birth; mothers giving birth at home were approached at the first post-natal clinic visit, and were in most cases assessed within the first two weeks of life. Mothers visit clinics as soon as possible after a home birth in order to secure a government Road to Health Card (RtHC). Not only is the RtHC a type of health passport and, therefore, an important health record, it also serves as proof of birth and is used to apply for a birth certificate, which is then used to apply for a child support grants (R250 per month in 2013) from the South African Social Security Agency (SASSA).
Mothers were reassessed at five points over the course of the next two years: 85% (n = 390/460) were reassessed at 3 months, 92% at 6 months (n = 420/456), 88% at 9 months (n = 410/454), 91% at 12 months (n = 411/450), and 88% at 2 years (n = 396/450) post-birth. Twenty-two infants died in the first year, two of whom were the second twin and are therefore not included in this analysis. No deaths were recorded the second year of the study.
Training.
Local, isiXhosa speaking women were trained as interviewers, using role play to train mock interviews and pilot interviews in the field over a six-week time period. Interviewers collected data on mobile phones which were pre-programmed with assessment questions by the Mobenzi mobile phone team (https://www.mobenzi.com/). The following measures were completed at each assessment point.
Maternal Measures at Birth:
Maternal depression was reported on the Edinburgh Postnatal Depression Scale (EPDS) (Cox, Holden, Sagovsky, 1987; Lawrie, Hofmeyr, De Jager, Berk, 1998). The EPDS has been translated and used across numerous cultural contexts (Husain et al., 2014; Patel et al., 2003; Shrestha, Pradhan, Tran, Gualano, Fisher, 2016) including South Africa (Rochat, Tomlinson, Newell, Stein, 2013; Tomlinson et al., 2014). In South Africa, the EPDS has demonstrated good internal reliability, with a Cronbach’s alpha of 0.87 (Hartley et al., 2011) and construct validity (De Bruin, Swartz, Tomlinson, Cooper, Molteno, 2004). We report both the mean scale score and identify mothers whose responses indicate probable depressive disorder (i.e., using a cut-off of >13 to indicate depressed mood) (Rochat et al., 2007). Structural resources were identified as education, employment, income, living with a partner, water on the premises, and electricity. Intimate partner violence (IPV) was self-reported at the baseline interview with four items adapted from Jewkes and colleagues (Jewkes, Levin, Penn-Kekana, 2002; 2003). Mothers were asked four items referring to the past 12 months: if they were slapped or had anything thrown at them; were pushed or shoved; were punched with a fist or another object; or were attacked or threatened with a weapon by their partner. Alcohol use. The frequency of drinking alcohol was assessed as 0, never drinking, and 1, having had at least one drink in the past three months. HIV status was self-reported by mothers at each assessment; maternal status is also reported on the mother’s antenatal card and their child’s government-issued Road-to-Health card. Number of antenatal visits. The percentage of mothers who completed the recommended number of antenatal appointments (four) was recorded. Alloparenting. Mothers self-reported whether they were the child’s primary caregiver at each assessment.
Child Measures Over Time.
Low birth weight was recorded for those infants born weighing less than 2500 grams. Weight and height were measured by trained and certified interviewers on measuring mats and on electronic scales which were recalibrated weekly. Children’s weight and height measures were then converted to z-scores based on the World Health Organization’s (WHO) age-adjusted norms (http://www.who.int/childgrowth/standards/en/). Growth at birth, 3, 6, 9,12, and 24 months is reflected in standardized scores (Z scores) for height-for-age (HAZ), weight-for-age (WAZ), and weight-for-length/height-for-age (WHZ). A z-score below −2SD was considered a serious health deficit, as being stunted ( > −2SD for HAZ) or malnourished ( > −2 SD for WAZ) (De Onis, Blössner, 2003). Received the child support grant. Whether or not the mother was receiving the South African child support grant (CSG) was recorded at birth, 3, 6, 9,12, and 24 months. Developmental Milestones. The gross motor developmental milestones of the WHO for children at 6 (WHO1), 9 (WHO3), 12 (WHO1–5) and 24 months (WHO1–6) were administered (Wijnhoven et al., 2004; Lansdown et al.,1996). These include six milestones that are fundamental to acquiring self-sufficient locomotion: sitting without support, hands-and-knees crawling, standing with assistance, walking with assistance, standing alone, and walking alone (De Onis et al., 2006). Tasks were coded as follows: if the milestones were completed (1), if the child refused or was unable to complete the task (0).
Analysis
The primary analysis compared maternal and child outcomes for mothers with (EPDS > 13) and without (EPDS </= 13) depressed moods at birth using mixed effects regression models, with mothers without depressed moods as the reference group. Logistic mixed effects regression models were used for binary outcomes and linear mixed effects regression models were used for continuous outcomes (i.e., age, education level, and number of household members). All models were adjusted for repeated measures, where appropriate, and a random participant effect to control for the longitudinal nature of the assessments was used. Longitudinal linear mixed effects regression models were used to compare child growth scores between children of mothers with and without depressed moods over the first two years of life and were adjusted for child sex and baseline household income. One HIV-positive child was omitted from the analyses. EPDS for one mother at birth was missing so this mother and her child were omitted from the analysis. The regression models were carried out using IBM SPSS Statistics (Version 20, Armonk, NY: IBM Corp).
Results
Table 1 summarizes the characteristics of the mothers with and without depressed mood at the point of recruitment at child-birth. There were 16% (73/468) of children born to mothers with perinatal depressed mood. Mothers with depressed moods were significantly less likely to be living with the child’s father or their in-laws (23% vs 35%, OR = 0.56, 95% C.I. = [0.31, 0.99], p = .05) and have household incomes above 2000 ZAR (31% vs 51%, OR = 0.43, 95% C.I. = [0.25, 0.74], p = .002). There were no significant differences amongst the mothers in age (M = 24.9 years, SD = 7.2), education (M = 8.6 years, SD = 2.4), if there was a water tank on site or electricity in the household (16%), number of people living in the household (M = 5.9, SD = 2.9), primipara (40%), having the recommended four antenatal clinic appointments (47%), HIV status (28% seropositive), or alcohol use (11% before learning about pregnancy and 7% after learning of pregnancy). However, mothers with depressed mood were more likely to experience IPV than mothers without depressed mood (B = 0.83, Std. Error = 0.34, 95% C.I. = [0.16,1.51], p = .016). Mothers were more likely to report IPV during pregnancy than prior whether they had depressed moods or not (B = 0.90, Std. Error = 0.15, 95% C.I. = [1.19,1.19], p < .001).
Table 1.
Differences between Baseline Characteristics at Birth by Mothers’ Depressed Mood
| No Depressed Mood (EPDS<13) | Depressed Mood(EPDS>13) | All Mothers | |
|---|---|---|---|
| N = 395 | N = 73 | N = 468 | |
| Demographic & Structural Characteristics | |||
| Mean age (SD) | 24.8 (7.1) | 25.4 (7.7) | 24.9 (7.2) |
| Mean highest education level (SD) | 8.6 (2.4) | 8.6 (2.4) | 8.6 (2.4) |
| Live With Father or Family* | 35% (139) | 23% (17) | 33% (94) |
| Monthly household income>2000Rand** | 51% (194/379) | 31% (21/68) | 48% (215/447) |
| Water Tank on Site | 17% (69) | 10% (7) | 16% (76) |
| Electricity | 17% (67) | 8% (6) | 16% (73) |
| Mean Household Members (SD) | 5.4 (2.8) | 6.0 (3.0) | 5.9 (2.9) |
| Intended to Apply for Child Support Grant | 97% (383) | 96% (70) | 97% (453) |
| Maternal Health | |||
| Mean EPDS | 6.1 (3.6) | 17.6 (3.3) | 7.9 (5.5) |
| Primipara | 40% (157) | 38% (28) | 40% (185) |
| Four+ Antenatal Clinic Appointments | 48%(132/275) | 38% (8/21) | 47% (140/296) |
| HIV Positive | 28% (110) | 30% (22) | 28% (132) |
| Alcohol and Domestic Violence | |||
| Alcohol Before Learning of Pregnancy | 11% (44) | 12% (9) | 11% (53) |
| Alcohol After Learning of Pregnancy | 6% (25) | 8% (6) | 7% (31) |
| Domestic Violence Previously* | 9% (37) | 19% (14) | 11% (51) |
| Domestic Violence During Pregnancy* | 20% (80) | 32% (23) | 22% (103) |
| Children Growth Measures | |||
| Mean HAZ Scores (SD) | −0.18 (1.15) | −0.08 (1.13) | −0.16 (1.14) |
| Mean WAZ Scores (SD) | −0.62 (0.99) | −0.46 (0.98) | −0.59 (0.99) |
| Mean WHZ Scores (SD) | −0.70 (1.31) | −0.46 (1.30) | −0.66 (1.31) |
| Low Birth Weight | 12% (39/330) | 9% (6/68) | 11% (45/398) |
Note. p values from linear (continuous variables) and logistic (binary) mixed effect regressions. Denominators shown for variables with missing data.
p < .05
p < .01
At birth, there were no significant differences in HAZ, WAZ, WHZ scores, or low birth weight children of mothers with and without depressed mood (11%).
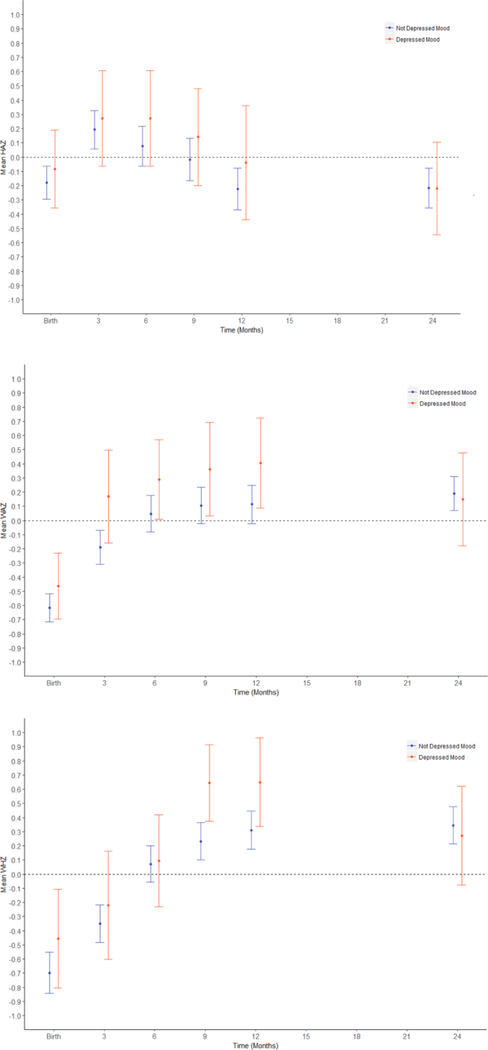
Table 2 summarizes the cumulative support for children over time by mothers’ depression. By 12 months, about 75% of all mothers had begun receiving the child support grant. However, by 24 months, mothers with depressed mood were significantly less likely to have obtained the child support grant than mothers without depressed mood (82% vs. 91%, OR = 0.43, 95% C.I. = [0.20, 0.94], p = .035). By 24 months, the majority of children had up-to-date immunizations, although immunization rates in this population were too low to ensure heard immunity for measles (Le Roux et al., 2017). In addition, children of mothers with and without depressed mood exclusively breastfeed at similar rates (8% for six months) and experience a similar rate of alloparenting by 24 months post-birth (34%). There were no significant differences between children of mothers with and without depressed mood in HAZ, WAZ, WHZ, low birth weight, stunting or malnourished scores, or in developmental motor, social, and speech milestones through 24 months post-birth. Overall, children’s WAZ and WHZ significantly increased over 24 months. WAZ increased from birth at three (Estimate = 0.46, S.E. = .05, p < .001, 95% C.I. = [0.38, 0.55]), six (Estimate = 0.71, S.E. = .05, p < .001, 95% C.I. = [0.60, 0.82]), nine (Estimate = 0.80, S.E. = .06, p < .001, 95% C.I. = [0.69, 0.92], 12 (Estimate = 0.74, S.E. = .06, p < .001, 95% C.I. = [0.62, 0.86], and 24 (Estimate = 0.78, S.E. = .06, p < .001, 95% C.I. = [0.67, 0.90]) months. WHZ increased from birth at three (Estimate = 0.34, S.E. = .06, p < .001, 95% C.I. = [0.17,0.51]), six (Estimate = 0.78, S.E. = .08, p = .004, 95% C.I. = [0.62,0.95]), nine (Estimate = 1.00, S.E. = .08, p < .001, 95% C.I. = [0.84, 1.16]), 12 (Estimate = 1.02, S.E. = .08, p < .001, 95% C.I. = [0.86, 1.19]), and 24 (Estimate = 1.01, S.E. = .08, p < .001, 95% C.I. = [0.85, 1.17]) months. However, the children’s HAZ increased from birth at three (Estimate = 0.38, S.E. = .07, p < .001 95% C.I. = [0.24, 0.52]) and six (Estimate = 0.28, S.E. = .07, p < .001, 95% C.I. = [0.14, 0.43]) months, but did not significantly change from birth at nine, 12, or 24 months (See Figure 1).1
Table 2.
Cumulative Support for Children over Time (months) by Mothers’ Depressed Mood Depressed Mood
| Depressed Mood EPDS>13 | Birth (N=468) | 3 months (N=389) | 6 months (N=417) | 9 months (N=399) | 12 months (N=408) | 24 months (N=395) | |
|---|---|---|---|---|---|---|---|
| Received Child Support Grant | No | -- | 37% | 67% | 76% | 79% | 91% |
| Yes | -- | 34% | 61% | 73% | 68% | 82% | |
| Exclusive Breastfeeding | No | -- | 21% (70/328) | 9% (31/351) | -- | -- | -- |
| Yes | -- | 18%(11/60) | 6% (4/66) | -- | -- | -- | |
| Up-to-date Immunizations | No | -- | 49% (148/305) | 70% (244/351) | 83% (255/308) | 74% (228/309) | 74% (224/304) |
| Yes | -- | 49% (26/53) | 79% (48/61) | 89% (50/56) | 68% (39/57) | 69% (34/49) | |
| Stunting HAZ < 2 SD | No | 7% | 3% | 6% | 6% | 8% | 8% |
| Yes | 6% | 5% | 3% | 9% | 9% | 6% | |
| MalnourishedWAZ < 2 SD | No | 10% | 4% | 6% | 3% | 4% | 3% |
| Yes | 10% | 3% | 0% | 3% | 4% | 2% | |
| WHZ < 2 SD | No | 18% | 9% | 4% | 3% | 4% | 3% |
| Yes | 16% | 13% | 6% | 0% | 2% | 6% | |
| WHO Gross MotorMilestones Completed | No | -- | -- | 88% (308/351) | 94% (318/337) | 76% (250/ 329) | 99% (334/339) |
| Yes | -- | -- | 89% (59/66) | 94% (58/62) | 73% (41/56) | 98% (55/56) |
Note: At birth, there were no immunizations. Denominators shown for variables with missing data.
Figure 1.
Growth of children (HAZ, WAZ, WHZ scores) from birth to 24 months by Mothers’ Depressed Mood at Birth. Longitudinal linear models were adjusted for household income, child gender, as well as living with the father or in-laws and IPV.
At 24 months post-birth, 8% of children were stunted, 3% of children were severely underweight for age, and 4% were wasted. Although the mean WAZ (mean difference = .18, p = .001, 95% C.I. = [0.07, 0.30] and WHZ (mean difference = .33, p < .001, 95% C.I. = [0.21, 0.46]) were significantly above the WHO norms at 24 months, the mean HAZ was significantly lower than the WHO norm (mean difference = −.22, p = .001, 95% C.I. = [−0.34, −0.09]), indicating stunted children who were for the most part not underweight.
Discussion
The rate of perinatal depression in the Eastern Cape (16%) is much lower than rates reported by previous research in rural, urban, and peri-urban areas in South Africa (>30%) (Honikman, Van Heyningen, Field, Baron, Tomlinson, 2012; Rochat, Tomlinson, Bärnighausen, Newell, Stein, 2011; Rotheram-Borus et al., 2011). Unlike evidence from HIC (Brand, Brennan, 2009; Diego et al., 2004; Steer et al.,1992)and in some LMIC (Stein et al., 2014; Fisher et al., 2012; Nasreen, Kabir, Forsell, Edhborg, 2011; Patel, DeSouza, Rodrigues, 2003), perinatal maternal depressed mood was not associated with negative growth outcomes for children in rural South Africa. The number of infants with low birth weights, as well as height and weight scores were consistent between children of mothers with and without perinatally depressed mood. These findings are consistent with a previous report on infant growth at 18 months among women who reported depressed mood two months after the birth of their child in periurban settlements outside of Cape Town, South Africa (Tomlinson, Cooper, Stein, Swartz, Molteno, 2006).
Children of mothers with and without perinatally depressed mood had similar growth rates and developmental outcomes. At two years, the rates of both stunted (8%) and malnourished (3%) children were much lower in the currently studied rural region than the national averages (27% and 12%, respectively) (State of the World’s Children, 2009). Mechanisms suggested to explain the effects of maternal depression on child development focus on individual deficits in caregiving (Stein et al., 2014). However, such deficits may be mitigated by the social connections rural living demands and more intact social structures when compared to peri-urban townships. (Patel, DeSouza, Rodrigues, 2003).
The rural environment may offer social protective factors in managing depression and other difficulties faced by women. Geographically isolated areas, such as those in the Eastern Cape, foster social connections among the inhabitants to support survival (Schatz, Madhavan, Williams, 2011). Less than half of all mothers in the current cohort have household incomes above 2000 ZAR (154 USD) and at least two years pass until most mothers secure a child support grant to support their children and themselves. Also, their relationships with their partners are unstable as only one in three pregnant women live with their partners or their partner’s families and one in five pregnant mothers experience violence by their partners. These challenges demand women to help each other for survival including caregiving children other than their own (Emmott, 2016; Rahman et al., 2003). One in three children experienced alloparenting in the current cohort. Further, mothers were also equally likely to breastfeed whether they reported depressed mood at birth or not. The more extreme poverty of rural communities may be associated with mothers, even those experiencing perinatal depressed mood, breastfeeding more because they have limited access to milk formula. Previous research in rural communities in South Africa and other LMICs suggest that social connections may mitigate the disruption caused by depression (Rahman et al., 2003). These connections are especially vital for mothers living in poor, rural areas with limited income, structural resources, and limited access to healthcare.
However, the influence of social support on maternal mental health in deeply rural areas of sub-Saharan Africa is not well understood (Rochat et al., 2006; Vyavaharkar et al., 2010). Results from previous studies suggest the importance of measuring different forms of social support as not all have positive associations with better mental health (Rochat et al., 2006). Specifically, among pregnant women in rural KwaZulu-Natal in South Africa, living away from a family or parental home is related to more depression (Vyavaharkar et al., 2010). However, qualitative results suggest that having an unsupportive partner and familial conflict, sometimes related to unwanted pregnancies or HIV status disclosure, results in elevated emotional stress and depressive symptoms among pregnant women (Vyavaharkar et al., 2010). However, the association between these sources of social support and mental health has not been studied in the Eastern Cape to date.
Limitations
Although social support may serve as a protective factor for women experiencing perinatal depression in rural SA, the current study did not assess or measure the types or degree of social support experienced by the mothers. However, previous research in rural regions of both HIC (Emmott, 2016) and LMIC (Rochat, Tomlinson, Bärnighausen, Newell, Stein, 2011) report associations between family and social support and reduced rates of ante-and postnatal depression. This highlights the need for future assessments to include measures of social support. Further, the current study assessed depressed mood at a single time-point, limiting the current analysis to maternal mood during the perinatal period. Although the EPDS has been found reliable and valid in South Africa (Hartley et al., 2011; De Bruin, Swartz, Tomlinson, Cooper, Molteno, 2004), it does not confirm a diagnosis of depression. Despite this limitation, the EPDS cut-off value of 13 serves as useful screening tool for depressed mood Kheirabadi, Maracy, Akbaripour, Masaeli, 2012). This efficient and inexpensive screening tool is especially useful in contexts, such as deeply rural areas, where clinical diagnoses are difficult and costly due to a lack of access to healthcare professionals. Although we focus on examining the influence of perinatal depressed mood, future examinations may also consider the potentially varying effects of prenatal, perinatal, and postnatal depressed mood (Tarabulsy et al., 2014) on maternal and child outcomes in deeply rural settings.
Conclusion
Despite the lower rates of depression among pregnant women in rural versus peri-urban South Africa (Honikman, Van Heyningen, Field, Baron, Tomlinson, 2012; Rochat, Tomlinson, Bärnighausen, Newell, Stein, 2011; Rotheram-Borus et al., 2011), mothers that experienced depressed mood perinatally faced even more deprivation than mothers without depressed mood. Mothers with perinatal depressed mood at the birth of their child had lower incomes, were less likely to live with their partner or their partner’s family and more likely to experience IPV. These results are consistent with previous findings linking poverty (Lund et al., 2010), marital status (Simon, 2002), and IPV (Tsai, Tomlinson, Comulada, Rotheram-Borus, 2016) to an increased risk of depression during pregnancy. Furthering our understanding of how social connections work in this region and how they can be encouraged to promote healthy life choices may be especially important for geographically isolated areas in SA and other LMIC.
Supplementary Material
Highlights.
16% of mothers report depressed mood in the rural Eastern Cape of South Africa
Perinatal depressed mood was associated with low income and interpersonal violence
Similar infant outcomes over the first two years despite maternal depressed mood
Acknowledgments.
This study was funded by the DG Murray Trust (South Africa), Philani (South Africa), and Ilifa Labantwana (South Africa)
Compliance with ethical standards/funding: This study was funded by the DG Murray Trust (South Africa), Philani (South Africa), NIH T32, and Ilifa Labantwana (South Africa).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: All authors declare no conflicts of interests.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was conducted with approval of the Institutional Review Board of the Stellenbosch University (N12/08/046) and permission was granted by the Eastern Cape Department of Health to recruit in government health facilities.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Availability of data and materials: Data can be made available upon request.
Longitudinal regression models were also run with maternal EPDS scores (continuous variable) and similar results were found for child growth over the first two years (see Appendix A).
References
- 2013. National Antenatal Sentinel HIV Prevalence Survey (https://www.health-e.org.za/2016/03/10/report-2013-national-antenatal-sentinel-hiv-prevalence-surey/). Accessed 19 Sep 2016.
- Brand SR, Brennan PA (2009). Impact of antenatal and postpartum maternal mental illness: Paediatrica, 95, 86–95. [DOI] [PubMed] [Google Scholar]
- Cox J, Holden JM, Sagovsky R (1987). Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry, 150(6), 782–786. [DOI] [PubMed] [Google Scholar]
- Dewing S, Tomlinson M, le Roux IM, Chopra, Tsai AC (2013). Food insecurity and its association with co-occurring postnatal depression, hazardous drinking, and suicidality among women in peri-urban South Africa. Journal of Affective Disorders, 150(2), 460–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bruin GP, Swartz L, Tomlinson M, Cooper PJ, Molteno C (2004). The factor structure of the Edinburgh Postnatal Depression scale in a South African peri-urban settlement. South African Journal of Psychology, 34(1), 113–21. [Google Scholar]
- De Onis M, Blössner M (2003). The World Health Organization global database on child growth and malnutrition: methodology and applications. International Journal of Epidemiology, 32(4), 518–526. [DOI] [PubMed] [Google Scholar]
- de Onis M, WHO Multicentre Growth Reference Study Group (2006). WHO Motor Development Study: windows of achievement for six gross motor development milestones. Acta Paediatrica, 95, 86–95. [DOI] [PubMed] [Google Scholar]
- Diego MA, Field T, Hernandez-Reif M, Cullen C, Schanberg S, Kuhn C (2004). Prepartum, postpartum, and chronic depression effects on newborns. Psychiatry: Interpersonal and Biological Processes, 67(1), 63–80. [DOI] [PubMed] [Google Scholar]
- Dyer TP, Stein JA, Rice E, Rotheram-Borus MJ (2012). Predicting depression in mothers with and without HIV: The role of social support and family dynamics. AIDS and Behavior, 16(8), 2198–2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmott E (2016). Access to Alloparents. Encyclopedia of Evolutionary Psychological Science, 1–4.
- Fieldgate I, Jeffrey R, Madinane M, Ebrahim Y, Soobyah L, Jordaan J (2013). Economic Impact of An Advertising Ban on Alcoholic Beverages For Industry Association for Responsible Alcohol Use. Econometrix (Pty) Ltd; Available online at: http://5737034557ef5b8c02c0e46513b98f90.cdn.ilink247.com/ClientFiles/econometrix/Econometrix/Company/Documents/Economic_Impact_of_an_Ad_Ban_Econometrix.pdf. 2013 Mar. [Google Scholar]
- Fisher J, Mello MCD, Patel V, Rahman A, Tran T, Holton S, Holmes W (2012). Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization, 90, 139–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley M, Tomlinson M, Greco E, Comulada WS, Stewart J, Le Roux I, Mbewu N, Rotheram-Borus MJ (2011). Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reproductive Health, 8(1), 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honikman S, Van Heyningen T, Field S, Baron E, Tomlinson M (2012). Stepped care for maternal mental health: a case study of the perinatal mental health project in South Africa. PLoS Medicine, 9(5), e1001222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husain N, Rahman A, Husain M, Khan SM, Vyas A, Tomenson B, Cruickshank KJ (2014). Detecting depression in pregnancy: validation of EPDS in British Pakistani mothers. Journal of Immigrant and Minority Health, 16(6), 1085–92. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Levin J, Penn-Kekana L. (2002). Risk factors for domestic violence: findings from a South African cross-sectional study. Social Science & Medicine, 55(9), 1603–17. [DOI] [PubMed] [Google Scholar]
- Jewkes RK, Levin JB, Penn-Kekana LA. (2003). Gender inequalities, intimate partner violence and HIV preventive practices: findings of a South African cross-sectional study. Social Science & Medicine, 56(1), 125–34. [DOI] [PubMed] [Google Scholar]
- Kheirabadi GR, Maracy MR, Akbaripour S, Masaeli N (2012). Psychometric properties and diagnostic accuracy of the edinburgh postnatal depression scale in a sample of Iranian women. Iranian Journal of Medical Sciences, 37(1), 32. [PMC free article] [PubMed] [Google Scholar]
- Lansdown RG, Goldstein H, Shah PM, Orley JH, Di G, Kaul KK, Kumar V, Laksanavicharn U, Reddy V (1996). Culturally appropriate measures for monitoring child development at family and community level: a WHO collaborative study. Bulletin of the World Health Organization, 74(3), 283. [PMC free article] [PubMed] [Google Scholar]
- Lawrie TA, Hofmeyr GJ, De Jager M, Berk M (1998). Validation of the Edinburgh Postnatal Depression Scale on a cohort of South African women. South African Medical Journal, 88(10), 1340–1344. [PubMed] [Google Scholar]
- Le Roux IM, Tomlinson M, Harwood JM, O’connor MJ, Worthman CM, Mbewu N, Stewart J, Hartley M, Swendeman D, Comulada WS, Weiss RE (2013). Outcomes of home visits for pregnant mothers and their infants: a cluster randomised controlled trial. AIDS (London, England), 27(9), 1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Roux K, Akin-Olugbade O, Katzen LS, Laurenzi C, Mercer N, Tomlinson M, Rotheram-Borus MJ (2017). Immunisation coverage in the rural Eastern Cape–are we getting the basics of primary care right? Results from a longitudinal prospective cohort study. South African Medical Journal, 107(1), 52–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C, Breen A, Flisher AJ, Kakuma R, Corrigall J, Joska JA, Swartz L, Patel V (2010).Poverty and common mental disorders in low and middle income countries: a systematicreview. Social Science Medicine, 71(3), 517–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maphalala Z, Pascoe M, Smouse MR (2014). Phonological development of first language isiXhosa-speaking children aged 3; 0–6; 0 years: A descriptive cross-sectional study. Clinical Linguistics Phonetics, 28(3), 176–194. [DOI] [PubMed] [Google Scholar]
- Nasreen HE, Kabir ZN, Forsell Y, Edhborg M (2010). Low birth weight in offspring of women with depressive and anxiety symptoms during pregnancy: results from a population based study in Bangladesh. BMC public health, 10(1), 515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nduna M, Jewkes RK, Dunkle KL, Shai NP, Colman I (2010). Associations between depressive symptoms, sexual behaviour and relationship characteristics: a prospective cohort study of young women and men in the Eastern Cape, South Africa. Journal of the International AIDS Society, 13(1), 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons CE, Young KS, Rochat TJ, Kringelbach M, Stein A (2012). Postnatal depression and its effects on child development: a review of evidence from low-and middle-income countries. British Medical Bulletin, 101(1). [DOI] [PubMed] [Google Scholar]
- Patel V, DeSouza N, Rodrigues M (2003). Postnatal depression and infant growth and development in low income countries: a cohort study from Goa, India. Archives of Disease in Childhood, 88(1), 34–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Rahman A, Jacob KS, Hughes M (2004). Effect of maternal mental health on infant growth in low income countries: new evidence from South Asia. BMJ, 328(7443), 820–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posel D, Devey R. (2006). The demographics of fathers in South Africa: an analysis of survey data, 1993–2002. Baba: men and fatherhood in South Africa, 38–52.
- Pronyk PM, Harpham T, Busza J, Phetla G, Morison LA, Hargreaves JR, Kim JR, Watts CH, Porter JD (2008). Can social capital be intentionally generated? A randomized trial from rural South Africa. Social Science Medicine, 67(10), 1559–1570. [DOI] [PubMed] [Google Scholar]
- Rahman A, Bunn J, Lovel H, Creed F (2007). Association between antenatal depression and low birthweight in a developing country. Acta Psychiatrica Scandinavica, 115(6), 481–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Iqbal Z, Harrington R (2003). Life events, social support and depression in childbirth: perspectives from a rural community in the developing world. Psychological Medicine, 33(7), 1161–1167. [DOI] [PubMed] [Google Scholar]
- Rahman A, Iqbal Z, Roberts C, Husain N (2009). Cluster randomized trial of a parent‐based intervention to support early development of children in a low‐income country. Child: Care, Health and Development, 35(1), 56–62. [DOI] [PubMed] [Google Scholar]
- Rahman A, Malik A, Sikander S, Roberts C, Creed F (2008). Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. The Lancet, 372(9642), 902–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Richest and Poorest Municipalities in South Africa. BusinessTech. (http://businesstech.co.za/news/wealth/127213/the-richest-and-poorest-municipalities-in-southafrica/). Accessed 19 Sep 2016.
- Rochat TJ, Richter LM, Doll HA, Buthelezi NP, Tomkins A, Stein A (2006). Depression among pregnant rural South African women undergoing HIV testing. JAMA, 295(12), 1373–1378. [DOI] [PubMed] [Google Scholar]
- Rochat TJ, Tomlinson M, Bärnighausen T, Newell ML, Stein A (2011). The prevalence and clinical presentation of antenatal depression in rural South Africa. Journal of Affective Disorders, 135(1–3), 362–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Richter L, Van Rooyen H, Van Heerden A, Tomlinson M ., Stein A, Rochat T, De Kadt J, Mtungwa N, Mkhize L, Ndlovu L (2011). Project Masihambisane: a cluster randomised controlled trial with peer mentors to improve outcomes for pregnant mothers living with HIV. Trials, 12(1), 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochat TJ, Tomlinson M, Newell ML, Stein A (2013). Detection of antenatal depression in rural HIV-affected populations with short and ultrashort versions of the Edinburgh Postnatal Depression Scale (EPDS). Archives of Women’s Mental Health, 16(5), 401–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Tomlinson M, Le Roux I, Stein JA (2015). Alcohol use, partner violence, and depression: a cluster randomized controlled trial among urban South African mothers over 3 years. American Journal of Preventive Medicine, 49(5), 715–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz E, Madhavan S, Williams J (2011). Female-headed households contending with AIDS-related hardship in rural South Africa. Health Place, 17(2), 598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon RW (2002). Revisiting the relationships among gender, marital status, and mental health. American Journal of Sociology, 107(4), 1065–1096. [DOI] [PubMed] [Google Scholar]
- Shrestha SD, Pradhan R, Tran TD, Gualano RC, Fisher JR (2016). Reliability and validity of the Edinburgh Postnatal Depression Scale (EPDS) for detecting perinatal common mental disorders (PCMDs) among women in low-and lower-middle-income countries: a systematic review. BMC Pregnancy and Childbirth, 16(1), 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- State of the World’s Children 2009. (https://www.unicef.org/sowc09/). UNICEF. Accessed 24 July 2018.
- Steer RA, Scholl TO, Hediger ML, Fischer RL (1992). Self-reported depression and negative pregnancy outcomes. Journal of Clinical Epidemiology, 45(10), 1093–1099. [DOI] [PubMed] [Google Scholar]
- Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, Pariante CM (2014). Effects of perinatal mental disorders on the fetus and child. The Lancet, 384(9956), 1800–1819. [DOI] [PubMed] [Google Scholar]
- Tanser F, Bärnighausen T, Grapsa E, Zaidi J, Newell ML (2013). High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science, 339(6122), 966–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarabulsy GM, Pearson J, Vaillancourt-Morel MP, Bussières EL, Madigan S, Lemelin JP, Duchesneau AA, Hatier DE, Royer F (2014). Meta-analytic findings of the relation between maternal prenatal stress and anxiety and child cognitive outcome. Journal of Developmental Behavioral Pediatrics, 35(1), 38–43. [DOI] [PubMed] [Google Scholar]
- Tomlinson M, Cooper PJ, Stein A, Swartz L, Molteno C (2006). Post‐partum depression and infant growth in a South African peri‐urban settlement. Child: Care, Health and Development, 32(1), 81–86. [DOI] [PubMed] [Google Scholar]
- Tomlinson M, O’Connor MJ, Le Roux IM, Stewart J, Mbewu N, Harwood J, RotheramBorus MJ (2014). Multiple risk factors during pregnancy in South Africa: the need for a horizontal approach to perinatal care. Prevention Science, 15(3), 277–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Tomlinson M, Comulada WS, Rotheram-Borus MJ (2016). Intimate partner violence and depression symptom severity among South African women during pregnancy and postpartum: population-based prospective cohort study. PLoS Medicine, 13(1), e1001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyavaharkar M, Moneyham L, Corwin S, Saunders R, Annang L, Tavakoli A (2010). Relationships between stigma, social support, and depression in HIV-infected African American women living in the rural Southeastern United States. Journal of the Association of Nurses in AIDS Care, 21(2), 144–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijnhoven TM, de Onis M, Onyango AW, Wang T, Bjoerneboe GE, Bhandari N, Lartey A, Al Rashidi B (2004). Assessment of gross motor development in the WHO Multicentre Growth Reference Study. Food and Nutrition Bulletin, S37–45 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.