Abstract
Purpose
To describe a case of corneal ulceration associated with Nivolumab use.
Observations
An 80-year-old woman treated with Nivolumab for metastatic melanoma developed an intractable corneal ulcer in her left eye, refractory to all therapies – including surgery to cover the ulcer with a conjunctival flap – until topical prednisolone acetate was tried, which was curative.
Conclusions and importance
Nivolumab use may be associated with a form of steroid-responsive corneal ulceration.
Keywords: Cornea, Corneal ulcer, Nivolumab, Opdivo, Peripheral ulcerative keratitis
1. Introduction
Nivolumab is an immunomodulatory agent with a broadening list of indications including first-line medical treatment for metastatic melanoma and second line for non-small cell lung cancer.1 The drug is a monoclonal antibody that targets the PD-1 receptor, and it functions by upregulating the number and activity of circulating T-cells.2 Stemming from this mechanism, a number of “immune related adverse events” have been described, including polymyalgia rheumatica, insulin-dependent diabetes, and immune-related pneumonitis, colitis, myocarditis, hepatitis, nephritis, encephalitis, and others.2 Ocular side effects have also been reported including conjunctivitis, uveitis, and dry eye syndrome.2, 3, 4, 5 Here, we present a ocular adverse association with Nivolumab use – corneal ulceration – and describe its features, clinical behavior, and potential importance to oncologists as a harbinger of more serious systemic sequelae.
2. Case description
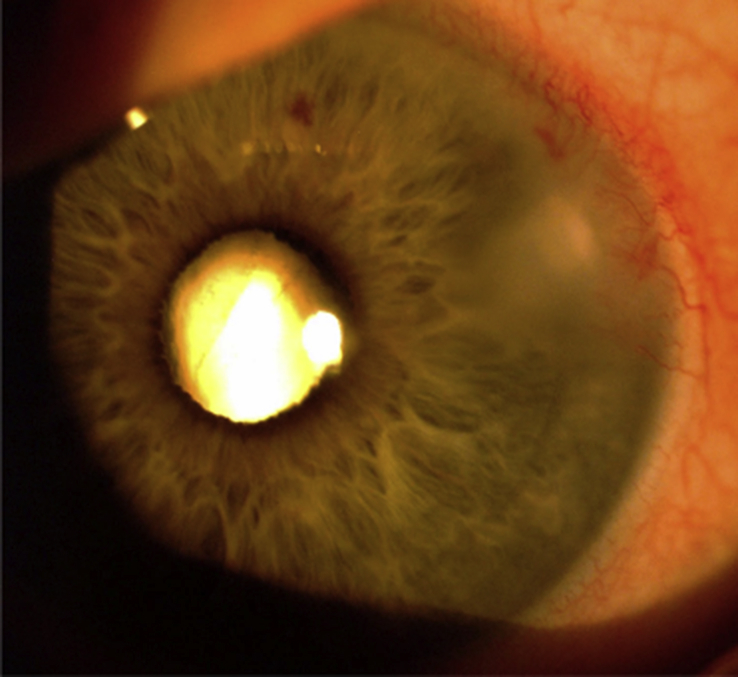
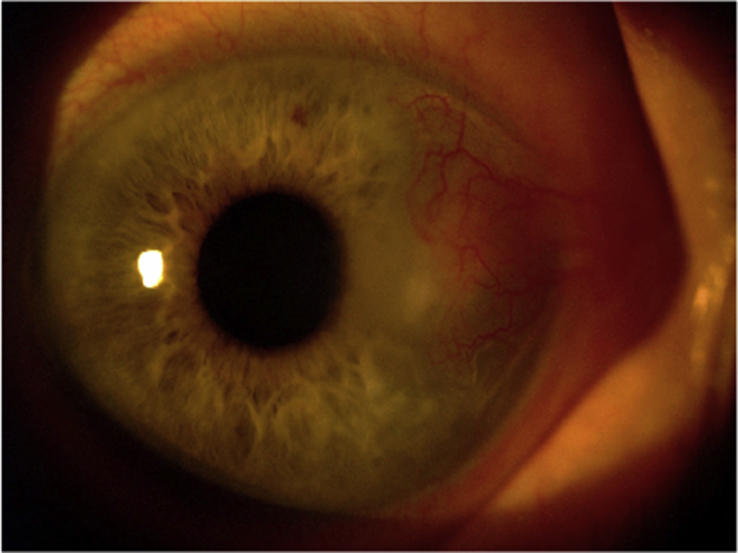
An 80-year-old white female with no past ocular history and a medical history significant for metastatic mucosal melanoma – treated initially with Nivolumab at the standard dosage (every-other-week infusions of 240mg for a duration of 4 months prior to seeing ophthalmological care) – presented to our clinic complaining of redness, pain, and decreased vision in her left eye of one-month's duration. On exam, her left eye manifested a best-corrected visual acuity (BCVA) of 20/40, moderate injection of the bulbar conjunctiva, and a limbus-involving corneal epithelial defect with underlying infiltrate (Fig. 1). The right eye was asymptomatic with a normal exam and a BCVA of 20/20. Bacterial and fungal cultures and HSV PCR were negative. Corneal sensation was normal bilaterally. Nevertheless, for suspected HSV-keratitis, ganciclovir ophthalmic gel (0.15%) was initiated five times daily in the left eye along with oral Valcyclovir 1 gm three times daily. Ten weeks of such treatment produced no improvement in the appearance of the ulcer, nor did one subsequent week of loteprednol etabonate ophthalmic gel (0.5%) applied twice daily, and – as a result of continuing pain– the patient underwent a conjunctival flap procedure along with corneal biopsy. The surgery itself was uneventful; at one day, week, and month postoperatively, the eye was comfortable and the flap appeared in good position. Meanwhile, the results of the corneal biopsy (including tissue gram stain, culture, and viral PCR for herpes simplex, zoster, and cytomegalovirus) were negative. However, by the two-month postoperative visit, the ulcer had recurred at the central edge of the conjunctival flap (Fig. 2). Viral and bacterial cultures were repeated, oral Valcyclovir at 1 gm three times daily was resumed (which had been discontinued after surgery), and topical ciprofloxacin (0.3%) ophthalmic solution was initiated at a frequency of one drop every hour around the clock. Three days later – with all cultures again negative, and the patient's signs and symptoms unimproved – a decision was made to stop all topical and oral therapy and instead proceed with topical prednisolone acetate ophthalmic solution (1%) four times daily. Four days later, the epithelial defect had completely healed; two weeks later, topical steroids were discontinued. Two months later, secondary to interstitial pneumonitis, declining pulmonary function, and the development of atrial fibrillation and brittle, insulin-dependent diabetes, Nivolumab infusions were halted (which were ongoing throughout the entirety of her ophthalmic treatment course). Through 12 months of subsequent follow-up, the patient's left eye has remained asymptomatic without evidence of ulcer recurrence.
Fig. 1.
Peripheral cornea ulcer.
Fig. 2.
Recurrent ulcer at the central edge of the conjunctival flap.
3. Discussion and conclusions
With Nivolumab rapidly increasing in popularity for a number of different malignancies, a number of inflammatory ocular side effects have been attributed to its use. These include conjunctivitis, anterior uveitis, immune retinopathy, endothelitis, and corneal allograft reaction with graft rejection.2, 3, 4, 5 Dry eye syndrome is believed to be the most common related ocular adverse event and, recently, Nguyen et al. described a severe example of which culminating in corneal perforation.6 Even more recently, Reddy et al. made the first report of Nivolumab associated retinopathy.7 Here, we describe Nivolumab associated corneal ulceration which appears to be immune, not exposure, related.
That our patient's ulcer arose at the corneal limbus, rather than in the inferior or interpalpebral cornea, suggests an inflammatory etiology, akin to a peripheral ulcerative keratitis, rather than an exposure keratopathy, as does the ulcer's unilaterality (and the paucity of dry-eye findings in the contralateral eye), its recurrence at the edge of the conjunctival flap, and its prompt resolution following the administration of topical prednisolone acetate (but, interestingly, not loteprednol etabonate). These findings also argue against a diagnosis of Rosacea-related keratitis, which has been reported to produce a sterile corneal ulceration.8
Although our initial suspicion was a herpetic keratitis based on the lesion's morphology, the patient's lack of response to extended medical (and surgical) therapy called this diagnosis into question, as did the multiple negative culture and biopsy results. Moreover, Nivolumab may actually be an effective treatment for herpetic keratitis, since it upregulates and activates the body's T-cell population, making our original diagnosis additionally unlikely and suggesting an etiology of true auto-immune keratitis.9 Whether our patient had a predisposition to developing ocular autoimmune problems is unknown, because the required laboratory investigations to inform upon that issue were not performed. However, it is possible that some individuals may be uniquely susceptible to such complications.
It is also noteworthy that our patient's systemic side effects of Nivolumab use which forced her to discontinue the medication crescendoed within four months of the appearance of her corneal ulcer. In patients with rheumatoid arthritis, peripheral ulcerative keratitis is often resistant to topical steroid therapy and is a well-known harbinger of severe morbidity and mortality risk. It is conceivable that peripheral ulceration in patients using Nivolumab likewise presages upcoming systemic events.10
4. Patient Consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Acknowledgments and disclosures
No funding or grant support.
No author has a financial or proprietary interest in any material or method mentioned.
All authors attest that they meet the current ICMJE criteria for Authorship.
References
- 1.Ramamurthy C., Godwin J.L., Borghaei H. Immune checkpoint inhibitor therapy: what line of therapy and how to choose? Curr Treat Options Oncol. 2017;18:33. doi: 10.1007/s11864-017-0476-y. [DOI] [PubMed] [Google Scholar]
- 2.Zimmer L., Goldinger S.M., Hofmann L. Neurological, respiratory, musculoskeletal, cardiac and ocular side-effects of anti-PD-1 therapy. Eur J Cancer. 2016;60:210–225. doi: 10.1016/j.ejca.2016.02.024. [DOI] [PubMed] [Google Scholar]
- 3.Richardson D.R., Ellis B., Mehmi I., Leys M. Bilateral uveitis associated with nivolumab therapy for metastatic melanoma: a case report. Int J Ophthalmol. 2017 18;10:1183–1186. doi: 10.18240/ijo.2017.07.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baughman D.M., Lee C.S., Snydsman B.E., Jung H.C. Bilateral uveitis and keratitis following nivolumab treatment for metastatic melanoma. Med Case Rep. 2017;3 doi: 10.21767/2471-8041.100044. pii: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le Fournis S., Gohier P., Urban T., Jeanfaivre T., Hureaux J. Corneal graft rejection in a patient treated with nivolumab for primary lung cancer. Lung Canc. 2016;102:28–29. doi: 10.1016/j.lungcan.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Nguyen A.T., Elia M., Materin M.A., Sznol M., Chow J. Cyclosporine for dry eye associated with nivolumab: a case progressing to corneal perforation. Cornea. 2016;35:399–401. doi: 10.1097/ICO.0000000000000724. [DOI] [PubMed] [Google Scholar]
- 7.Reddy M., Chen J.J., Kalevar A., Terribilini R., Agarwal A. Immune retinopathy associated with nivolumab administration for metastatic non-small cell lung cancer. Retin Cases Brief Rep. 2017 Nov 22 doi: 10.1097/ICB.0000000000000675. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Brouwer N., Haanen J., Jager M. Development of ocular Rosacea following combined ipilimumab and nivolumab treatment for metastatic malignant skin melanoma. Ocul Oncol Pathol. 2017;3:188–192. doi: 10.1159/000455150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jun H., Seo S.K., Jeong H.Y. B7-H1 (CD274) inhibits the development of herpetic stromal keratitis (HSK) FEBS Lett. 2005 7;579:6259–6264. doi: 10.1016/j.febslet.2005.09.098. [DOI] [PubMed] [Google Scholar]
- 10.Foster C.S., Forstot S.L., Wilson L.A. Mortality rate in rheumatoid arthritis patients developing necrotizing scleritis or peripheral ulcerative keratitis. Effects of systemic immunosuppression. Ophthalmology. 1984;91:1253–1263. doi: 10.1016/s0161-6420(84)34160-4. [DOI] [PubMed] [Google Scholar]