Abstract
Purpose
The aim of the present experimental study was to evaluate the biomechanical behavior in different types of osteosynthesis (titanium screws, bioresorbable pins and miniplates) used in management of intracapsular condylar head fractures.
Method
Experimental models of the condylar head fractures were simulated on 15 dry human cadaveric mandibles. Osteotomized mandibles were randomly divided into three groups with different fixation systems used: 1) 15 mm long titanium screws, 2) 15 mm long bioresorbable pins Sonic Pins Rx, 3) T-shaped titanium miniplate and 7 mm long titanium screws. Mandibles were loaded in TIRAtest testing machine (Germany). The main types of deformations, including torsion, bending and shearing, were simulated to study the biomechanical characteristics of the fixation systems.
Results
Titanium bicortical screws demonstrated the highest stiffness in standard loading conditions. The fixation with bioresorbable pins showed lower stiffness in both frontal and sagittal loads. This is indicative of the fact that resorbable pins, which have numerous advantages for clinical usage, cannot provide adequately stable fixation in maximal masticatory loads. The mandibles fixed with T-shaped plate had the lowest stiffness.
Conclusion
Screw or pin fixation, regardless of the material used, was not resistant to rotational loads. On the contrary, the stiffness of T-shaped plates was quite significant. In real clinical conditions, if rotational displacements are not effectively compensated by irregularities in the fracture surface and precise repositioning of the bone fragments, combined use of miniplates and bicortical titanium screws or two screws can be beneficial.
Keywords: Condylar head, Osteosynthesis, Fracture, Biomechanics
1. Introduction
Mandibular condylar fractures are one of the most common types of mandibular fractures, ranging from 9.8% to 49% or more.1,2 Among them, high intracapsular fractures are considered to be the most unfavorable due to their complex anatomical and biomechanical relations, unsatisfactory clinical outcomes and challenging surgical approaches.3,4 The complications of intracapsular condylar fractures include extensive condylar deformation, occlusal disturbances, limitation of mandibular mobility, lateral deviation during mouth opening, malocclusion, pathological changes in the temporomandibular joint (TMJ), facial asymmetry, and ankylosis.5, 6, 7, 8 Indications for surgical treatment and its outcomes strongly depend on the type of the condylar head fracture. According to Neff et al. classification (2004, 2010), there are three types of intracapsular condylar fractures5,6: type A (a fracture line through the medial portion of the condylar head); type B (a fracture line through the lateral portion of the condylar head); type C (a fracture line is near the attachment of the lateral capsule). A number of authors recommend open reduction and internal fixation (ORIF) for condylar head fractures with ramus shortening (type B and C)6 as the above techniques are associated with lower risk of severe TMJ dysfunction, ankylosis, and early recovery of oral function.7, 8, 9 The aim of the surgical treatment for condylar head fractures is the correct reposition and stable fixation of the fragment in its normal anatomical position.5,10,11 Numerous surgical techniques using metallic or bioresorbable materials have been developed to ensure the reliable stability and strength of the condylar head osteosynthesis.12,13 They include Kirschner wires, bicortical titanium screw or pins, lag-screws, micro- and miniplates, resorbable screws and pins.3,12,14 Screw osteosynthesis of the condylar head is the most widely used technique because it can provide relatively good stability by minimally invasive surgical procedure. Screws for internal fixation of the intracapsular condylar fractures were first described by Rasse et al., followed shortly by Neff et al. who improved the technique and proved its efficacy in number of clinical and biomechanical studies.5,15,16 A number of authors have recently reported about the reliability and advantages of screw osteosynthesis as compared with other techniques of fixation.3,9,17 Several screw designs and insertion techniques have been offered in recent years. However, the optimal number (one, two or three), length (from 11 to 17 mm), direction (perpendicular to the fracture line, parallel to the long or horizontal axis of the condyle) and types of the screws are still discussed in the literature.3,5,17,18 Titanium screw osteosynthesis has a number of disadvantages, including the risk of malposition with perforation of the condylar head and exposure of the fixator after condylar remodeling, which may require screw removal.13 Other possible complication is fragmentation of the small fragment as a result of stresses applied when tightening the screw. Resorbable fixation is an alternative to titanium screws. The use of ultrasound-activated resorbable pins (SonicWeld®) minimizes the risk of the above complications and has some advantages from biological and technical points of view. Bioresorbable pins and screws were studied clinically and experimentally for their capability to ensure the stabile fixation in time-dependent process of their biodegradation.19 Some authors demonstrated no significant difference of pin osteosyntesis as compared with titanium screws in a sheep model.14 Despite this fact, there are few publications on biomechanical behavior of different fixation systems used for condylar head fractures. Further research is necessary for objective estimation and comparison of biomechanical properties of the fixators and their ability to provide rigid internal fixation and stability in functional load, which determine the clinical efficacy and long-term functional outcomes.
The aim of the present experimental study was to evaluate the biomechanical behavior of different types of osteosynthesis (titanium screws, bioresorbable pins and miniplates) used in management of intracapsular condylar head fractures.
2. Materials and methods
Experimental models of the condylar head fractures were simulated on 15 dry human cadaveric mandibles obtained from the Department of Anatomy, Bogomolets National Medical University. All the mandibles were free of lesions and had no signs of previous trauma or any surgery. For modeling of condylar head fractures, we used the Neff classification, which is most recognized and adopted by Strasbourg Osteosynthesis Research Group (SORG).5,6 In present study, type B condylar head fracture was reproduced by osteotomy of the mandibular head with steel disk and physiodispenser (W&H, Austria), rotating frequency 3000 rpm. The line of osteotomy began from the lateral pole of the condylar head and continued to the medial side of the condylar neck. When such a type of fracture occurs in clinical conditions, the medial bony segment dislocates medially, anteriorly, and inferiorly by lateral pterygoid muscle traction. This dislocation pattern may result in relevant ramus shortening and malocclusion. For this reason, type B condylar fracture in adults usually requires open reduction and internal fixation.20
Osteotomized mandibles were randomly divided into three groups with different fixation systems used. In group one (n = 6), after reposition of the fragments, the mandibles were fixed with 15 mm long titanium screw (Trimed, Germany, 2.0 mm system). The screws insertion and positioning was performed according to the standard protocol.7
In group two (n = 6), bioresorbable pins were employed to stabilize the fracture (15 mm long 2.1 mm diametr PDLLASonicPinsRx, KLS Martin, Germany). The pins were inserted and activated by SonicWeld Rx® device. Owing to the ultrasound-induced liquefaction, the bioresorbable pin penetrates into the bone and solidifies thus ensuring stable fixation achieved. In group three (n = 3), each mandible was fixed with T-shaped titanium miniplate and 7 mm long titanium screws (I-Plant, Ukraine, 1.6 system). The plate was placed onto the posterior slope of the condyle and across the fracture line.
In all the cases, we checked the position of screws inside the bone by standard X-ray tests.
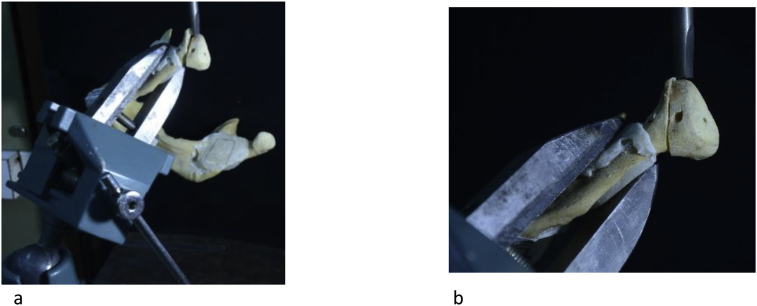
After the reduction and fixation of the fragments, mandibles were loaded in the TIRA-test (Germany) testing machine. The main patterns of the stress and strain state of the condyle were simulated taking into consideration the clinical data on functional loading and typical dislocations of the bone fragments in type B condylar fractures. A special appliance was used to immobilize the mandibles under force (Fig. 1). Further, the main types of deformations, including torsion in the horizontal plane, bending and shearing in sagittal and frontal planes, were simulated to study the biomechanical characteristics of the fixation systems (see Fig. 2).
Fig. 1.
A special appliance used to immobilize the mandibles under force.
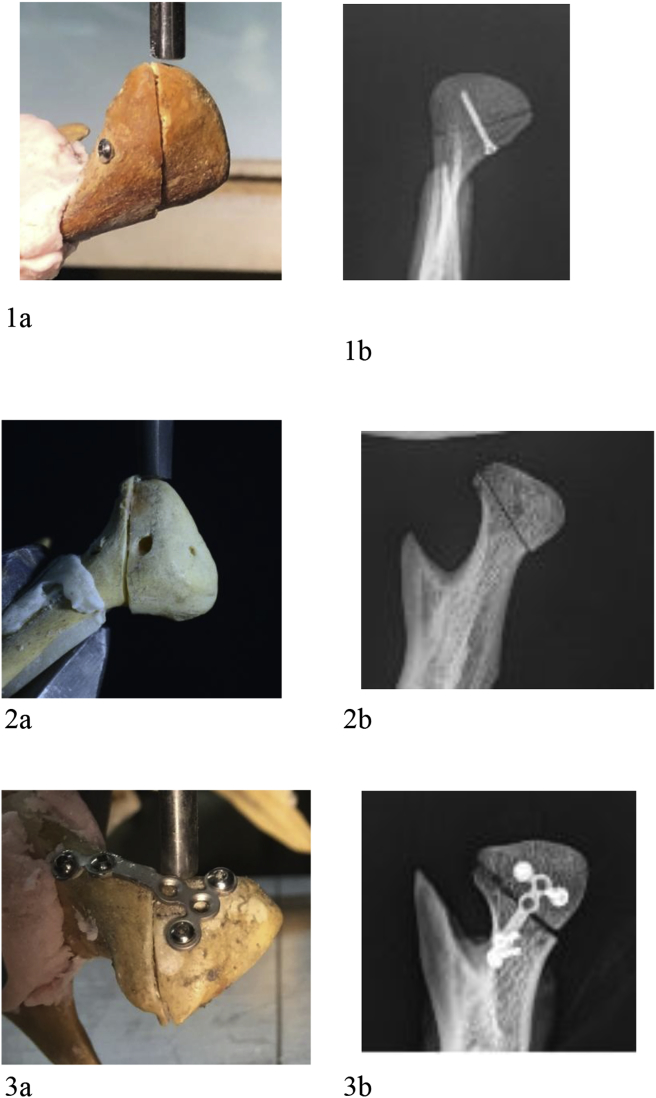
Fig. 2.
Experimental models and X-ray images of the condylar head fractures (type B by A. Neff, 2004) simulated on the dry human cadaveric mandibles and fixed with titanium screw (1a, 1b), bioresorbable pins (2a, 2b) and T-shaped plate (3a, 3b).
Each mandible was fixed in a standard position in the testing machine. Before the application of loading, 5 N (N/mm) of preload was applied for standardization of sagittal and frontal loading and 2.5 (N/mm) of preload for torsion deformation.
Sagittal and frontal loadings were created by vertical movement of the movable table of the testing machine and rigid steel rod connected to the dynamometer. The load was applied parallel to the fracture line at the lateral pole of the condylar surface. To apply a torsion load, a 1 mm-diameter metal ball was installed on the opposite side in the area of titanium plate hole to exclude other types of deformations. The load gradually increased in linear deformation range (up the limit of proportionality).The data were transmitted from the testing machine to the computer as a graph showing force and displacement. The stiffness was measured as the ratio of force (N) to deformation (mm). For torsion deformation, there was recorded a deformation diagram and stiffness was calculated by the ratio of the actual torque to the angle of torsion. After each loading, the samples were checked for irreversible plastic deformations.
The statistical analysis was carried out using SPSS package v.22 (SPSS, Inc., Chicago, IL, USA). The comparison between groups was performed with the nonparametric Mann-Whitney test, P < 0.05 considered significant.
3. Results
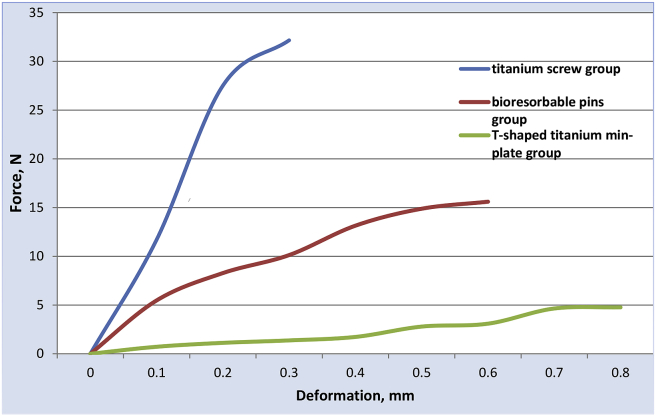
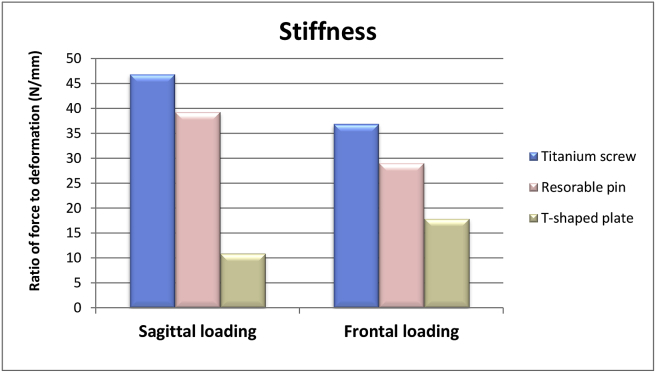
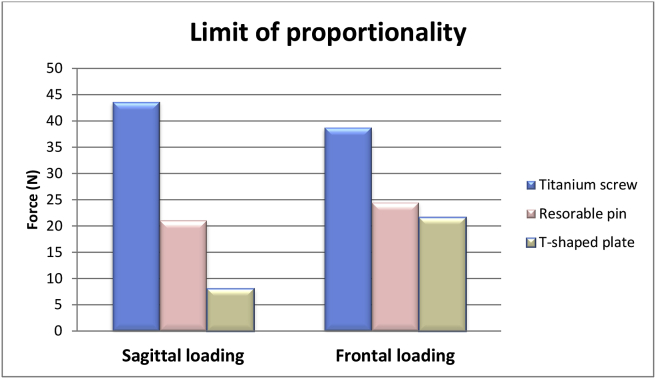
The general patterns of the bone –fixator system deformation under the gradually increased load are shown in Fig. 3. Group I (titanium screw fixation samples) (Fig. 4) had the highest stiffness. It was 46.9 ± 31,4 N/mm when the force was applied in the sagittal direction and 36.92 ± 20.34 N/mm – in the frontal direction. The fixation with bioresorbable pins demonstrated lower stiffness in both frontal (29.1 ± 9.03 N/mm) and sagittal loads (39.3 ± 16.6 N/mm). The lowest value of stiffness was found when the mandibles were fixed by T-shaped plate: 10.9 ± 10 N/mm – for sagittal and 17.9 ± 10.11 N/mm – for frontal loading. Mann-Whitney test for independent samples showed significant differences with group I (P > 0.05).At the same time, screw or pin fixation, regardless of the material used, was not resistant to rotational loads. Minimal stress caused the extreme deformations or breakdown of the fixation system. On the contrary, the stiffness of T-shaped plates was quite significant (an average value of 518.3 ± 111.9 N * mm/Rad). The limit of proportionality, reflecting the greatest stress that can be applied to the mandible without causing irreversible plastic deformation, was highest in group I and lowest in group III for both frontal and sagittal loads (Fig. 5). The maximum value of the limit of proportionality among all the mandibles tested was 98.5 N (group I) and it means that fixation system can easily resist non-mastication loads, but at maximal bite force, the plastic deformation of the system is possible.
Fig. 3.
General patterns of the deformation of different types of the condyle fixation system under the gradually increased load.
Fig. 4.
Comparison of stiffness value in different types of the condyle fixation.
Fig. 5.
Comparison of the limit of proportionality value in different types of the condyle fixation.
The biomechanical parameters of the samples within each group vary significantly, depending on the physical properties of the bone and anatomical shape of the condyle. It gives evidence that such factors as anatomical characteristics of the mandible and its architectonics, physical and mechanical properties of the bone and features of the fracture line can influence the biomechanical parameters of the internal fixation system more than type and material of the fixator.
4. Discussion
Surgical treatment of the condylar head fractures is still one of the most controversial issues in maxillofacial surgery.20 Such fractures, which account for 22–36% of all condylar fractures, are the most contentious regarding diagnosis and management due to the lack of evidence-based results and randomized controlled trials that have examined outcomes of different treatment strategies.2,3 A range of authors still recommend conservative treatment for high condylar fractures because open reduction of the bone fragments is a difficult intervention, which is often associated with the facial nerve injury, bleeding, and damage of the TMJ structures.2,10 The accuracy of the operation to a certain degree depends on the surgeon's experience and equipment used. However, closed reduction cannot provide the proper reposition in severe displaced or dislocated fractures or restore the normal height of the mandibular ramus.4 In adults, the main indications for surgical treatment are intracapsular fractures with reduction of ramus height (except for heavily comminuted fractures), or fractures in which the laterally dislocated ramus stump is out of the glenoid fossa.21 Randomized multi-entre studies reported better functional results after open reduction as compared with non-surgical treatment.9
Given the specific anatomy, functional loading of the mandibular head and other components of the temporomandibular joint (TMJ), the predominance of spongious bone in this zone, limited surgical space and visualization, an optimal fixation system remains the subject of discussion. The stress and strain state of the mandibular head changes substantially in different phases of the masticatory cycle and includes various types of deformations (tensile-compression, shear, bend and torsion in different planes). At the same time, a fixation system should ensure not only the stable holding of the fractured bone in the proper position, but also promote the normal biological processes in the postoperative period. Fixation elements should not cause significant damage to the spongious layer of the bone or other anatomical structures, including the lateral pterygoid muscle, vessels and nerves, intra-articular elements, etc.3,12
Among a large number of currently available types of fixators for treatment of the condylar head fractures, fixation with screws or pins of titanium or polymeric materials is the most widely technique used. It is minimally invasive, anatomically based and has a number of advantages over the use of traditional mini- or microplates.3,5,9,16,22
The data on the optimal number and orientation of screws are controversial. For example, Rasse at al., as well as Neff and his group recommended fixing the condylar head fracture with two titanium screws or resorbable pins, which should be placed at an angle to each other. According to Neff et al., 2004; Mengetal., 2010; Xinetal. 2014, to avoid lateral displacements and increase the rotational stability of the system, one screw should be placed perpendicular to the fracture line, and the other - parallel to the horizontal axis of the condylar process.5,16,20 Despite the certain biomechanical advantages of using two screws, fixing with one screw is often more advisable from anatomical and surgical points of view. Because of the small size of the mandibular head, its complex architectonics with a predominance of the spongious bone, there is a risk of the fragmentation due to the increased stress around the screw heads, exposure of the fixators during bone remodeling and related complications in the TMJ such as the destruction of the articular fossa.Yangetal. and Luo et al. in clinical trials showed the efficacy of one bicortical screw placed in proper position and provided the related biomechanical background.9,18,20,23
In recent years, resorbable pins have been offered to fix the condylar head fractures. Their main advantage is in the capability to reduce the risk of complications associated with the stress-shielding effect, condylar head resorption, perforation of the articular fossa or exposure of the pin during remodeling of the bone in the postoperative period.12,22 The ultrasound-aided placement of bioresorbable pins, does not create lateral loads that cause destruction of the bone when metal screws are inserted.3 Based on the clinical evidence, Müller-Richter et al. reported that when using the resorbable pins, the incidence of related complications (bleeding, limited mouth opening, pain in the area of the TMJ, etc.) was not significantly different from that of titanium screws.25 However, under the conditions of significant functional loads, their strength and reliability may be insufficient, especially over the course of pins biodegradation and their structural transformations in the postoperative period.
Therefore, the choice of the optimal material for the screws, their number and orientation, as well as the determination of clear indications for the use, remain the subject of scientific discussion.3,5,16,18,20
To resolve these issues appropriately, multi-center randomized clinical trials are required as well as systematic experimental studies of the biomechanical behavior of various types of fixators, including the reproduction of complex loading conditions of the mandibular condylar process and TMJ.
Our data give evidence that titanium bicortical screws placed in accordance with the recommendations of Guo S-s et al.7 had the highest rigidity and strength while loaded in sagittal and frontal planes. When applying titanium bicortical screws, the stability/rigidity of fixation was by 20% higher than that of resorbable pins, and almost 3-fold higher than that of a traditional T-shaped miniplate. The limit of proportionality was also higher than that of resorbable pins and plates by 44 and 63%, respectively. These results are consistent with the data reported by Schneider et al., 2011, who found the average shift strength of resorbable pins to be 310 N (range 117–600 N) in vitro tests. It was significantly lower than the values achieved with titanium screws (918 N), which also had strength three times higher than that of ultrasound-activated resorbable pins.24 However, a number of clinical and experimental studies found no statistically significant difference between the efficacy of titanium screws and resorbable pins in terms of the regenerate quality, rate of complications or the achieved functional result. According to our data, their rigidity and strength are insufficient to counteract the maximum masticatory load.14,22 This supports the opinion of some researchers that inter-maxillary fixation for two or more weeks is necessary in case of resorbable pins and screws fixation.11
By comparing the biomechanical parameters of traditional miniplates and titanium screws, we have confirmed the advantages of the latter for different types of shear deformation. These data are consistent with Neff et al., 2005.17 Taking into consideration other disadvantages and risks associated with the use of titanium miniplates, the data are indicative of the feasibility of the use only in limited cases. It is known that the use of titanium plates is associated with the need for longer incision, the larger space and fixation with at least two screws in the mandibular head, which results in impaired regeneration and blood supply to the bone. According to literary data, the rate of postoperative disorders of the TMJ in the application of titanium mini plates reaches more than 30%.15 At the same time, our findings show that only T-shaped plates were able to counteract the rotational displacement of fragments, which could not be achieved by fixing screws or pins. Neff et al., 2004 and other researchers demonstrated the failure of one screw to counteract the rotational displacement.5,12,14,19 However, in real clinical conditions, rotational displacements are effectively compensated by irregularities in the fracture surface, precise repositioning and the force of friction between the wound surfaces.
Furthermore, while comparing our findings with similar studies by Neff, 2004, Omezli, 2015, Schneider et al., 2012,5,11,14 which were performed on standardized polyurethane or animal jaws, we revealed significant variability in the biomechanical parameters of the fixator-bone system defined on the cadaver jaws (21.5 SD 93%). This suggests that in real clinical conditions, anatomical characteristics of the mandible and its architectonics, physical and mechanical properties of the bone and features of the fracture line can have a significant effect on the mechanical parameters of the fixator-bone system and determine the prognosis of surgical treatment to a greater extent than the selected type of fixator.
The present study has several limitations, which have to be pointed out. The number of samples included to the analysis was relatively small (3–6 in each group). Furthermore, the main findings cannot be directly transferred to human patients, as there are differences in physical and mechanical properties between dry cadaveric and vital bone tissue, the load patterns of the condylar head in mastication are more complicated and depend on its position inside the fossa, which can be the subject for the further investigations.
5. Conclusion
Titanium bicortical screws demonstrated the highest stiffness in standard loading conditions: 46.9 ± 31.37 N/mm when the forces were applied in sagittal direction and 36.92 ± 20.34 N/mm – in frontal direction. The fixation with bioresorbable pins showed lower stiffness in both frontal (29.07 ± 9.03 N/mm) and sagittal loads (39.3 ± 16.6 N/mm). This is indicative of the fact that resorbable pins, which have numerous advantages for clinical usage, cannot provide adequately stable fixation in maximal masticatory loads. The mandibles fixed with T-shaped plate had the lowest stiffness: 10.9 ± 10 N/mm for sagittal and 17.9 ± 10.11 N/mm for frontal loading. Screw or pin fixation, regardless of the material used, was not resistant to rotational loads. On the contrary, the stiffness of T-shaped plates was quite significant (an average value of 518.3 ± 111.9 N * mm/Rad). In real clinical conditions, if rotational displacements are not effectively compensated by irregularities in the fracture surface and precise repositioning of the bone fragments, combined use of miniplates and bicortical titanium screws or two screws can be beneficial.
Ethical approval
Ethical approval for this study was obtained from the Ethical Committee of Bogomolets National Medical University, Kyiv, Ukraine.
Conflicts of interest
The authors have none to declare.
References
- 1.Boffano P., Roccia F., Zavattero E. Maxillofacial Trauma (EURMAT) project: a multicentre and prospective study. J Cranio-Maxillo-Fac Surg. 2015;43(1):62–70. doi: 10.1016/j.jcms.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 2.Vashistha A., Singh M., Chaudhary M., Agarwal N., Kaure G. Comparison of 2 mm single locking miniplates versus 2 mm two non-locking miniplates in symphysis and parasymphysis fracture of mandible. J Oral BiolCraniofac Res. 2017;7(1):42–48. doi: 10.1016/j.jobcr.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luo S., Li B., Long X., Deng M., Cai H., Cheng Y. Surgical treatment of sagittal fracture of mandibular condyle using long-screw osteosynthesis. J OralMaxillofacSurg. 2011;69:1988–1994. doi: 10.1016/j.joms.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 4.Duan D.H., Zhang Y. A clinical investigation on disc displacement in sagittal fracture of the mandibular condyle and its association with TMJ ankylosis development. Int J Oral Maxillofac Surg. 2011;40(2):134–138. doi: 10.1016/j.ijom.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 5.Neff A., Muhlberger G., Karoglan M. Stability of osteosyntheses for condylar head fractures in the clinic and biomechanical simulation. Mund Kiefer Gesichtschir. 2004;8(2):63–74. doi: 10.1007/s10006-004-0529-9. [DOI] [PubMed] [Google Scholar]
- 6.Loukota R.A., Neff A., Rasse M. Nomenclature/classification of fractures of the mandibular condylar head. Br J Oral Maxillofac Surg. 2010;48(6):477e478. doi: 10.1016/j.bjoms.2009.08.036. [DOI] [PubMed] [Google Scholar]
- 7.Guo S-s, Zhou W-n, Wan L-z. Computer-aided design–based preoperative planning of screw osteosynthesis for type B condylar head fractures: a preliminary study. J Cranio-Maxillofacial Surg. 2015;44(2):167–176. doi: 10.1016/j.jcms.2015.11.013. [DOI] [PubMed] [Google Scholar]
- 8.Wysocki J., Reymond J., Krasucki K. Vascularization of the mandibular condylar head with respect to intracapsular fractures of mandible. J Cranio-Maxillo-Fac Surg. 2012;40(2):112–115. doi: 10.1016/j.jcms.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 9.Kolk A., Neff A. Long-term results of ORIF of condylar head fractures of the mandible: a prospective 5-year follow-up study of small-fragment positional-screw osteosynthesis (SFPSO) J Cranio-Maxillo-Fac Surg. 2015;43(4):452–461. doi: 10.1016/j.jcms.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Hlawitschka M., Eckelt U. Assessment of patients treated for intracapsular fractures of the mandibular condyle by closed techniques. J Oral Maxillofac Surg. 2002;60:784–791. doi: 10.1053/joms.2002.33246. [DOI] [PubMed] [Google Scholar]
- 11.Omezli M.M., Torul D., Polat M.E., Dayi E. Biomechanical comparison of osteosynthesis with poly-L-lactic acid and titanium screw in intracapsular condylar fracture fixation: an experimental study. Niger J Clin Pract. 2015;18:589–593. doi: 10.4103/1119-3077.158946. [DOI] [PubMed] [Google Scholar]
- 12.Wang W.H., Deng J.Y., Zhu J., Li M., Xia B., Xu B. Computer-assisted virtual technology in intracapsular condylar fracture with two resorbable long-screws. Br J Oral Maxillofac Surg. 2013;51:138–143. doi: 10.1016/j.bjoms.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 13.Abdel-Galil K., Loukota R. Fixation of comminuted diacapitular fractures of the mandibular condyle with ultrasound-activated resorbable pins. Br J Oral Maxillofac Surg. 2008;46:482–484. doi: 10.1016/j.bjoms.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 14.Schneider M., Seinige C., Pilling E. Ultrasound-aided resorbableosteosynthesis of fractures of the mandibular condylar base: an experimental study in sheep. Br J Oral Maxillofac Surg. 2012;50:528–532. doi: 10.1016/j.bjoms.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Rasse M. NeuereEntwicklungen der Therapie der Gelenkfortsatzbruche¨ der Mandibula (Recent developments in therapy of condylar fractures of the mandible) Mund Kiefer Gesichtschir. 2000;4:69–87. doi: 10.1007/s100060050175. [DOI] [PubMed] [Google Scholar]
- 16.Neff A., Kolk A., Deppe H., Horch H.-H. NeueAspektezurIndikation der operativenVersorgungintraartikulärer und hoher Kiefer-gelenkluxationsfrakturen. Mund Kiefer GesichtsChir. 1999;3:24–29. doi: 10.1007/s100060050088. [DOI] [PubMed] [Google Scholar]
- 17.Neff A., Kolk A., Meschke F., Deppe H., Horch H.H. Small fragment screws vs. plate osteosynthesis in condylar head fractures. Mund Kiefer Gesichtschir. 2005;9(2):80–88. doi: 10.1007/s10006-005-0600-1. [DOI] [PubMed] [Google Scholar]
- 18.Meng F.W., Liu Y.P., Hu K.J., Kong L. Use of a temporary screw for alignment and fix-ation of sagittal mandibular condylar fractures with lateral screws. Int J Oral Maxillofac Surg. 2010;39(6):548e553. doi: 10.1016/j.ijom.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 19.Pilling E., Mai R., Theissig F., Stadlinger B., Loukota R.A., Eckelt U. An experimental in vivo analysis of the resorption to ultrasound activated pins (Sonic weld®) and standard biodegradable screws (ResorbX®) in sheep. Br J Oral Maxillofac Surg. 2007;45:447–450. doi: 10.1016/j.bjoms.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Xin P., Jiang B., Dai J. Finite element analysis of type B condylar head fractures and osteosynthesis using two positional screws. J Cranio-Maxillo-Fac Surg. 2014;42(5):482–488. doi: 10.1016/j.jcms.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 21.Chrcanovic B.R. Open versus closed reduction: diacapitular fractures of the mandibular condyle. Oral Maxillofac Surg. 2012;16:257–265. doi: 10.1007/s10006-012-0337-6. [DOI] [PubMed] [Google Scholar]
- 22.McLeod N.M.H., Saeed N.R. Treatment of fractures of the mandibular condylar head with ultrasound-activated resorbable pins: early clinical experience. Br J Oral Maxillofac Surg. 2016;54(8):872–877. doi: 10.1016/j.bjoms.2016.05.027. [DOI] [PubMed] [Google Scholar]
- 23.Yang M.L., Zhang B., Zhou Q., Gao X.B., Liu Q., Lu L. Minimally-invasive open reduction of intracapsular condylar fractures with preoperative simulation using computer-aided design. Br J Oral Maxillofac Surg. 2013;51(3):29–33. doi: 10.1016/j.bjoms.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Müller-Richter U.D., Reuther T., Böhm H., Kochel M., Kübler A.C. Treatment of intracapsular condylar fractures with resorbable pins. J OralMaxillofacSurg. 2011;69:3019. doi: 10.1016/j.joms.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 25.Schneider M., Eckelt U., Reitemeier B. Stability of fixation of diacapitular fractures of the mandibular condylar process by ultrasound-aided resorbable pins (SonicWeld Rx® System) in pigs. Br J Oral Maxillofac Surg. 2011;49:297–301. doi: 10.1016/j.bjoms.2010.05.001. [DOI] [PubMed] [Google Scholar]