Abstract
Background
The prospective associations between social isolation, loneliness, and health behaviors are uncertain, despite the potential importance of these relationships over time for outcomes including mortality.
Purpose
To examine the associations between baseline social isolation, baseline loneliness, and engagement in health behaviors over 10 years among older adults.
Methods
Data were from 3,392 men and women aged ≥52 years in the English Longitudinal Study of Ageing from 2004/2005 to 2014/2015. Modified Poisson regression was specified to estimate relative risks (RRs) and 95% confidence intervals for the associations between baseline social isolation, baseline loneliness, and consistent weekly moderate-to-vigorous physical activity, consistent five daily fruit and vegetable servings, daily alcohol drinking at any time point, smoking at any time point, and a consistently overweight/obese body mass index over the follow-up (all yes vs. no). Models were population weighted and adjusted for sociodemographic factors, health indicators, and depressive symptoms, with mutual adjustment for social isolation and loneliness.
Results
Socially isolated participants were less likely than non-isolated participants to consistently report weekly moderate-to-vigorous physical activity (RR = 0.86; 0.77–0.97) or five daily fruit and vegetable servings (RR = 0.81; 0.63–1.04). They were less likely to be consistently overweight or obese (RR = 0.86; 0.77–0.97) and more likely to smoke at any time point (RR = 1.46; 1.17–1.82). Loneliness was not associated with health behaviors or body mass index in adjusted models. Among smokers, loneliness was negatively associated with successful smoking cessation over the follow-up (RR = 0.31; 0.11–0.90).
Conclusions
Social isolation was associated with a range of health-related behaviors, and loneliness was associated with smoking cessation over a 10 year follow-up in older English adults.
Keywords: Social isolation, Health behaviors, Epidemiology, Health psychology, Aging
Social isolation is associated with a range of health-related behaviors and loneliness is associated with smoking cessation over a ten-year follow-up in older English adults.
Introduction
Social isolation and loneliness are problems frequently encountered by older adults, increasing in prevalence as people age [1–3]. Social isolation can be defined as a paucity of social contacts, while loneliness is described as the subjective experience of social isolation. Both have been associated with increased risks for poor self-reported health [4–6], depressive symptoms [7,8], cognitive decline [9–11], coronary heart disease and stroke [12,13], and all-cause mortality [14–16] among older men and women. Both are thought to influence health outcomes through direct biological mechanisms, as evidenced by their independent associations with increased inflammatory and stress biomarkers, as well as through health-related behavioral mechanisms [1,17–22]. Their respective relationships with the long-term persistence of health-related behaviors over time are less well understood, particularly in the context of aging. Older age is a time period in life when maintaining healthy lifestyle behaviors can become particularly challenging due to changing life circumstances including increasing risks of physical and cognitive impairments [23]. At the same time, healthy behaviors become increasingly important in later life for the maintenance of quality of life and well-being [24].
Social isolation is thought to influence health-related behaviors through the lack of social relationships that are maintained in situations of isolation [17,25,26]. Social relationships can serve to inhibit harmful or deviant behaviors and promote healthy behaviors through mechanisms of social control, engagement with others, and the provision of social support [17]. In the present study, we are particularly concerned with the health-related lifestyle behaviors of physical activity, fruit and vegetable intake, smoking, and alcohol consumption, along with body mass index (BMI). In the context of these behaviors, social control can act directly, though encouragements or reminders from family and friends to engage in desirable behaviors or to avoid deviant behaviors, and indirectly through behavioral cues to adhere to group-based social norms [26,27]. Social engagement with others can also directly affect behaviors when the engagements are health promoting in nature, such as exercise groups [17]. Social support could take the form of instrumental assistance with activities of daily living such as healthy meal preparation, or, similar to social control mechanisms, emotional and appraisal support for the maintenance of healthy behaviors [17,28]. However, social influence over health-related behaviors may in fact promote or damage health depending on the behavioral and leisure-time activity norms prevalent within a particular social group, the constraints of the physical and economic environments in which they operate, and the particular balance of demands and resources that the group members present [17,26,27].
Loneliness, as an affective experience of isolation, is also thought to have negative effects on health behaviors [29]. Importantly, loneliness may occur in the absence of social isolation, and socially isolated individuals do not always experience loneliness. This potential decoupling of loneliness and social isolation may be particularly common for older adults as reduced social network sizes are often expected and prepared for during aging [30]. There is relatively less theory on the mechanisms relating loneliness to health behavior than those relating social isolation to behavior, as much of loneliness’ effects on morbidity and mortality are thought to be mediated by chronic stress, dysregulation of coping mechanisms, cognitive dysfunction, and inflammation [2,29]. However, the negative effects of loneliness on mood might mediate its effects on behavior [29]. The relationship between loneliness and depression is generally accepted to be reciprocal [29,31], and social isolation may be a sufficient, but not necessary cause of both [1]. There is a weak-to-moderate positive correlation between social isolation and loneliness among in older adults populations, indicating that they overlap some but not all of the time [15,32]. Therefore, identifying the effects of social isolation and loneliness independently of one another on health-related outcomes is required to assess whether unique contributions are made by each, as well as the effects of each with and without depression accounted for due its possible role on the causal pathway between both constructs and health behavioral outcomes.
A body of cross-sectional literature demonstrates relationships between social isolation, loneliness, and a range of health behaviors among older adults, although they are rarely investigated in the same study or accounted for simultaneously in modeling. Among older adults, social isolation has been associated with having a poor diet [33,34], being physically inactive [20,34–36], problematic consumption of alcohol [34,36,37], and smoking [34,37]. In the Framingham Heart Study, obesity and heavy alcohol consumption have been shown to spread through family and friend networks over time, but so have positive behaviors related to substance use including smoking cessation and alcohol abstinence [38–40]. Greater social connectedness has also been associated with being physically active [37]. The empirical evidence for loneliness and health-related behaviors is more equivocal than for social isolation, although loneliness has been associated with physical inactivity, problematic alcohol consumption, overweight/obesity, and smoking [4,20,36,41–44].
Only one recent study, using data from adults aged ≥52 years in the English Longitudinal Study of Ageing (ELSA), has examined isolation and loneliness in concert in relation to physical activity and smoking, finding that both were independently associated with physical inactivity, but that isolation only was associated with smoking [20]. However, this study was cross-sectional and did not present the relationships of each construct with the persistence of health behaviors over time. The cross-sectional nature of existing evidence is a major limitation in this research area, as the effects of health behaviors on clinically defined outcomes are largely dependent on the persistence of behaviors over time. If social isolation or loneliness is associated with persistent engagement in behaviors such as physical activity, diet, smoking, and drinking over long periods of time, then the implications for health risks may be strong. However, the long-term associations between social isolation, loneliness, and health behaviors are uncertain. Given these two key limitations of existing literature, whether social isolation and loneliness represent independent risk factors for health behaviors over long time periods is uncertain. The simultaneous and balanced investigation of both constructs in relation to health is warranted to answer this question, which has direct implications for the types of interventions that may be developed to mitigate the effects of social isolation, loneliness, or both.
Assuming a normative regulatory role of social relationships over health behaviors, we hypothesize that social isolation will be associated with a lower likelihood of engaging in health-promoting behaviors over time among older adults. We hypothesize that loneliness will show associations in the same direction, although they may be of lesser magnitudes due to the potential presence of social control, engagement, and support from friends and family despite feelings of loneliness. The present paper therefore aims to investigate the longitudinal and independent relationships between baseline social isolation, baseline loneliness, and consistent weekly moderate-to-vigorous physical activity (MVPA), consistent five daily fruit and vegetable servings, daily alcohol drinking at any time point, smoking at any time point, and a consistently overweight/obese BMI over the follow-up over a 10 year period in a nationally representative cohort of older English adults.
Methods
Design
The ELSA is a population-based longitudinal cohort study of adults aged ≥50 years in England [45]. The cohort began in 2002/2003 based on a random stratified sample of households in England who participated in the Health Survey for England (n = 12,100, response rate = 66%). Data are collected through in-person home-based interviews, self-completion questionnaires every 2 years, and physical assessments with a trained nurse every 4 years. The study was approved by the London Multicentre Research Ethics Committee. Presently, data are available up to 2014/15.
Sample
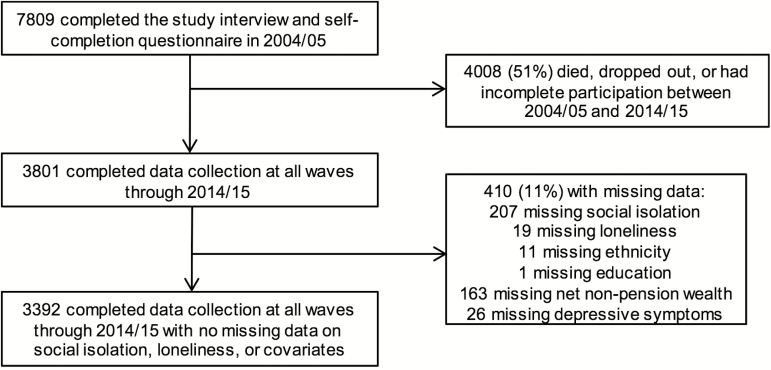
Eligible participants for this analysis were core ELSA participants who completed data collection from 2004/05 to 2014/15 with non-proxy interviews and had complete data on social isolation, loneliness, and covariates. Proxy interviews were conducted for participants who were cognitively impaired or institutionalized during data collection; these participants were excluded from the present analysis. The final analytic sample included 3,392 participants (Fig. 1).
Fig. 1.
Study flow diagram.
Measures
Social isolation
A five-item index of social isolation was computed [15,20]. Participants were assigned one point if they had less than monthly contact with each of children, other family members, and friends (any of meeting in-person, speaking on the telephone, or writing/emailing), if they did not belong to a social organization or club, or if they lived alone. Scores on the index ranged from 0 to 5, with higher scores indicating a greater degree of social isolation. As with previous ELSA analyses, scores were dichotomized at ≥2 versus <2 points to indicate high versus low social isolation [15,20]. While previous ELSA analyses have used marital status rather than living alone in the social isolation index, we exclude marital status to open up the possibility that someone can be married but still be isolated. Our recategorization may give a more precise of isolation based on actual living conditions, rather than on marital status.
Loneliness
Loneliness was measured using a three-item short form of the Revised University of California Los Angeles (UCLA) Loneliness Scale [46]. Items were questions such as ‘How often do you feel you lack companionship?’ with response options of ‘hardly ever or never’, ‘some of the time’, and ‘often’. Scores ranged from 3 to 9, with higher scores indicating greater loneliness. They were dichotomized at ≥6 versus <6 to indicate high versus low loneliness [15]. The scale showed good internal consistency, with a Cronbach’s alpha of 0.81.
Health behaviors
All health behaviors were categorized in a binary fashion according to UK public health recommendations and evidence on their associations with health outcomes in older adults, including risks of cardiovascular disease, cancers, and all-cause mortality [47–58].
MVPA was assessed in the study interview, where participants were questioned about the frequencies with which they participated in mild, moderate, and vigorous physical activities, with response options of ‘… more than once a week’, ‘once a week’, ‘one to three times a month’, and ‘hardly ever or never’. Participants were presented with a card showing examples of all three activity intensity levels. MVPA was coded dichotomously at each wave as moderate or vigorous intensity activity ≥once per week versus <once per week [47–49]. This MPVA measure has been validated in a subsample of ELSA participants against objective accelerometer measurements (Spearman r = 0.21; p =.002) and is predictive of all-cause mortality risk [48,52]. The outcome variable was maintaining weekly MVPA at all of six time points from 2004/05 to 2014/15 (yes vs. no).
Fruit and vegetable intake was assessed in the self-completion questionnaire from 2006/07 onward. In 2006/07 and 2008/09, participants were asked to tick off the numbers of various types of fruit and vegetable servings they had eaten in the past day. In 2010/11 through 2014/15, they were asked to write in a box the total number of fruit and of vegetable servings they had eaten in the past day. At each time point, the total number of fruit and vegetable servings consumed was calculated and dichotomized at <5 versus ≥5 per day, to reflect UK public health recommendations [51]. The median numbers of servings consumed at each time point were 4.3 (2006/07), 5.3 (2008/09), 5.0 (2010/11), 5.0 (2012/13), and 5.0 (2014/15). Hence, the five servings per day cutoff represents an approximate median split in intake at each follow-up time point. The outcome variable was consuming ≥5 servings daily at all of five time points from 2006/07 to 2014/15 (yes vs. no).
The frequency of consuming alcoholic drinks in the past 12 months was measured in the self completion questionnaire (‘almost every day’; ‘5 or 6 days a week’; ‘3 or 4 days a week’; ‘once or twice a week’; ‘once or twice a month’; ‘once every couple of months’; ‘once or twice a year’; ‘not at all in the last 12 months’). Those who reported drinking ‘almost every day’ in the past 12 months were coded as consuming alcohol daily, in order to capture heavy alcohol consumption [58]. The outcome variable was consuming alcohol daily at any time point from 2004/05 to 2014/15 (yes vs. no).
Smoking status was assessed in the study interview, where participants were asked at each wave whether they smoke cigarettes at all nowadays. Those who reported ‘yes’ to smoking nowadays were coded as smokers. Former smokers (prior to the study period) and never smokers were grouped together. The outcome variable for smoking status was being a smoker at any time point from 2004/05 to 2014/15 (yes vs. no). This variable captures long-term smokers and also ‘transitional’ smokers who intermittently made quit attempts followed by relapses over the study follow-up period.
Trained nurses measured BMI at 4 year intervals for a subset of the study population. BMI was classified at each time point as overweight or obese (BMI ≥ 25), or normal weight or underweight (BMI < 25). Very few participants were underweight (BMI < 18.5; n = 27). The outcome variable for BMI was consistently being overweight or obese in 2004/05, 2008/09, and 2012/13 (yes vs. no).
Covariates
Covariates, assessed in the study interview, were age group (52–59, 60–69, 70–79, ≥80), sex (male, female), marital status (single, married/living as married), net non-pension wealth in quintiles (quintiles were calculated stratified at age 65 to account for the effect of retirement on wealth), educational attainment (no qualifications, some education, degree level), ethnicity (white, non-white), limiting long-standing illness (yes, no), number of mobility impairments, presence of depressive symptoms according to scoring ≥3 on the eight-item Centre for Epidemiologic Studies Depression Scale (CES-D; yes, no) [15], and self-reported physician diagnosis of a range of chronic conditions: cancer, diabetes, heart disease, chronic lung disease, stroke, arthritis, and depression (all yes, no). An item on loneliness was removed from the CES-D scale to avoid overlap with the loneliness score, so that seven items remained in the scale [15].
Statistical Analysis
Characteristics of the sample were described according to baseline social isolation and baseline loneliness. A modified Poisson regression for binary outcome data with a log link function and robust error variance was used to estimate relative risks (RRs) and 95% confidence intervals (CIs) for the associations between baseline social isolation, baseline loneliness, and consistent weekly MVPA, consistent intake of five daily fruit and vegetable servings, daily alcohol drinking at any time point, smoking at any time point, and consistent overweight/obese BMI (all yes vs. no) over the follow-up [59]. Covariates were sequentially entered into models: Model Set 1 adjusted for age and sex, Model Set 2 additionally adjusted for sociodemographic factors (ethnicity, marital status, net non-pension wealth quintile, and educational attainment), and Model Set 3 additionally adjusted for health indicators (limiting long-standing illness, cancer, diabetes, heart disease, stroke, chronic lung disease, mobility impairment, and arthritis). In Model Set 4, social isolation and loneliness were mutually adjusted for. Model Set 5 additionally adjusted for depression and depressive symptom (CES-D) score to assess the role of mental health status in the results.
A subgroup analysis was conducted among baseline smokers (n = 383), where the relationships between each of social isolation and loneliness and successful smoking cessation (defined as reporting non-smoking from waves 2006/07 through 2014/15) were estimated in models adjusted for the same factors as in Model Set 4. Statistical weights were applied to all models to ensure that estimates represented the target general population. The ELSA wave 7 longitudinal weights were calculated as the inverse of the estimated probability of response to wave 7, multiplied by the wave 6 longitudinal weight and scaled to an average of 1. This iterative weighting calculation process means that the wave 7 longitudinal weight adjusts for non-response to the Health Survey for England and to each subsequent ELSA wave [60].
Three post hoc sensitivity analyses were run to further assess the relationships between social isolation, loneliness, and BMI: (a) removing all underweight participants (BMI <18.5 and <20), (b) stratifying models by age group to examine for effect modification by age (<65 vs. ≥65 and by decade), and (c) examining BMI at each time point to assess whether any particular time point might be driving the results. Two post hoc interaction analyses were also conducted, on the recommendation of the peer reviewers. The first examined whether an interaction existed between social isolation and loneliness, and the second examined whether the results differed between men and women. A final sensitivity analysis was conducted, using marital status rather than living situation (alone vs. not alone) in the social isolation index to be consistent with previous ELSA analyses [9,15,20]. All analyses were conducted using StataSE 13.1 (College Station, TX).
Results
Overall, 13% of participants (442/3,392) were classified as socially isolated (Table 1). Those who were socially isolated were more likely to be single, to have lower net non-pension wealth, and to have lower educational attainment than those who were not isolated (Table 1). Social isolation did not vary according to age, gender, ethnicity, or most baseline health conditions. However, compared with non-isolated participants, those who were socially isolated had a higher prevalence of chronic lung conditions (3% vs. 1%; p <.0001) and depressive symptoms (22% vs. 15%; p <.0001). In unadjusted chi-squared analyses, socially isolated participants were less likely to consistently report engaging in MVPA at least once weekly (41% vs. 53%; p <.0001) or consuming five daily fruit and vegetable servings (17% vs. 25%; p =.002); they were less likely to consistently be overweight or obese (55% vs. 66%; p <.0001), less likely to consume alcohol daily at any time point (35% vs. 43%; p =.01), and more likely to report smoking at any time point (22% vs. 12%; p <.0001).
Table 1.
Baseline Participant Characteristics According to Social Isolation, English Longitudinal Study of Ageing (ELSA), n = 3,392
| Baseline characteristic | Overall 3,392 (100%) | High social isolation 442/3,392 (13%) | Low social isolation 2,950/3,392 (87%) | p-value |
|---|---|---|---|---|
| Age group | .39 | |||
| 52–59 | 1,330 (39%) | 162 (37%) | 1,168 (40%) | |
| 60–69 | 1,299 (38%) | 167 (38%) | 1,132 (38%) | |
| 70–79 | 661 (19%) | 98 (22%) | 563 (19%) | |
| ≥80 | 102 (3%) | 15 (3%) | 87 (3%) | |
| Male | 1,487 (44%) | 207 (47%) | 1,280 (43%) | .17 |
| Marital status | <.0001 | |||
| Unmarried | 979 (29%) | 266 (60%) | 713 (24%) | |
| Married/living as married | 2,413 (71%) | 176 (40%) | 2,237 (76%) | |
| Net non-pension wealth quintile | <.0001 | |||
| 1 (poorest) | 449 (13%) | 107 (24%) | 342 (12%) | |
| 2 | 595 (18%) | 89 (20%) | 506 (17%) | |
| 3 | 683 (20%) | 89 (20%) | 594 (20%) | |
| 4 | 774 (23%) | 74 (17%) | 700 (24%) | |
| 5 (richest) | 891 (27%) | 83 (19%) | 808 (27%) | |
| Educational attainment | <.0001 | |||
| No qualifications | 907 (27%) | 150 (34%) | 757 (26%) | |
| Some education | 1,386 (41%) | 188 (43%) | 1,198 (41%) | |
| Degree level | 1,099 (32%) | 104 (24%) | 995 (34%) | |
| Ethnicity | .83 | |||
| Non-white | 35 (1%) | 5 (1%) | 30 (1%) | |
| White | 3,357 (99%) | 437 (99%) | 2,920 (99%) | |
| Limiting long-standing illness | 905 (27%) | 131 (30%) | 774 (26%) | .13 |
| Cancer | 81 (2%) | 9 (2%) | 72 (2%) | .60 |
| Diabetes | 178 (5%) | 31 (7%) | 147 (5%) | .07 |
| Heart disease | 75 (2%) | 7 (2%) | 68 (2%) | .34 |
| Chronic lung disease | 38 (1%) | 13 (3%) | 25 (1%) | <.0001 |
| Stroke | 48 (1%) | 6 (1%) | 42 (1%) | .91 |
| No. mobility impairments (mean; SD) | 1.67 (2.36) | 1.48 (2.1) | .36 | |
| Arthritis | 1,097 (32%) | 149 (34%) | 948 (32%) | .51 |
| Depression | 47 (1%) | 6 (1%) | 41 (1%) | .96 |
| Depressive symptoms | 540 (16%) | 97 (22%) | 443 (15%) | <.0001 |
| Health behaviors over the follow-upa | ||||
| Consistent weekly MVPA | 1,746 (52%) | 181 (41%) | 1,565 (53%) | <.0001 |
| Consistent five daily fruit & veg intake | 686 (24%) | 62 (17%) | 624 (25%) | .002 |
| Consistently overweight/obese BMI | 1,462 (65%) | 154 (55%) | 1,308 (66%) | <.0001 |
| Daily alcohol at any time point | 1,050 (42%) | 106 (35%) | 944 (43%) | .01 |
| Smoking at any time point | 449 (13%) | 96 (22%) | 353 (12%) | <.0001 |
MVPA moderate-to-vigorous physical activity; BMI body mass index.
aNumbers in the rows for the health behaviors may not sum to 3,392 due to missing outcome data.
Overall, 16% of participants (560/3,392) were classified as having a ‘high’ degree of loneliness. Social isolation and loneliness were weakly but significantly correlated (Spearman’s r = 0.13; p <.0001). Compared with those with ‘low’ loneliness, adults ‘high’ in loneliness were more likely to be older, to be female, to be single, to have less net non-pension wealth, to have lower educational attainment, and to be an ethnic minority (Table 2). Baseline health conditions varied more with loneliness than they did with social isolation; participants ‘high’ in loneliness had higher prevalence of limiting long-standing illnesses (40% vs. 24%; p <.0001), stroke history (3% vs. 1%; p =.005), arthritis (42% vs. 30%; p <.0001), and depressive symptoms (40% vs. 11%; p <.0001), and they had a greater number of mobility impairments, on average (2.44 vs. 1.32; p <.0001; Table 2). In unadjusted chi-squared analyses, adults ‘high’ in loneliness were less likely than those ‘low’ in loneliness to consistently report engaging in weekly MVPA (40% vs. 54%; p <.0001), less likely to be consistently overweight or obese (59% vs. 66%; p =.02), less likely to report drinking alcohol daily at any time point (34% vs. 43%; p =.02), and more likely to report smoking at any time point (16% vs. 13%; p =.02).
Table 2.
Baseline Participant Characteristics According to Loneliness, English Longitudinal Study of Ageing (ELSA), n = 3,392
| Baseline characteristic | Overall 3,392 (100%) | High loneliness 560/3,392 (16%) | Low loneliness 2,832/3,392 (84%) | p-value |
|---|---|---|---|---|
| Age group | .06 | |||
| 52–59 | 1,330 (39%) | 212 (38%) | 1,118 (39%) | |
| 60–69 | 1,299 (38%) | 198 (35%) | 1,101 (39%) | |
| 70–79 | 661 (19%) | 130 (23%) | 531 (19%) | |
| ≥80 | 102 (3%) | 20 (4%) | 82 (3%) | |
| Male | 1,487 (44%) | 192 (34%) | 1,295 (46%) | <.0001 |
| Marital status | <.0001 | |||
| Unmarried | 979 (29%) | 308 (55%) | 671 (24%) | |
| Married/living as married | 2,413 (71%) | 252 (45%) | 2,161 (76%) | |
| Net non-pension wealth quintile | <.0001 | |||
| 1 (poorest) | 449 (13%) | 115 (21%) | 334 (12%) | |
| 2 | 595 (18%) | 140 (25%) | 455 (16%) | |
| 3 | 683 (20%) | 120 (21%) | 563 (20%) | |
| 4 | 774 (23%) | 102 (18%) | 672 (24%) | |
| 5 (richest) | 891 (27%) | 83 (15%) | 808 (29%) | |
| Educational attainment | <.0001 | |||
| No qualifications | 907 (27%) | 205 (37%) | 702 (25%) | |
| Some education | 1,386 (41%) | 226 (40%) | 1,160 (41%) | |
| Degree level | 1,099 (32%) | 129 (23%) | 970 (34%) | |
| Ethnicity | .02 | |||
| Non-white | 35 (1%) | 11 (2%) | 24 (1%) | |
| White | 3,357 (99%) | 549 (98%) | 2,808 (99%) | |
| Limiting long-standing illness | 905 (27%) | 223 (40%) | 682 (24%) | <.0001 |
| Cancer | 81 (2%) | 10 (2%) | 71 (3%) | .31 |
| Diabetes | 178 (5%) | 33 (6%) | 145 (5%) | .45 |
| Heart disease | 75 (2%) | 19 (3%) | 56 (2%) | .04 |
| Chronic lung disease | 38 (1%) | 8 (1%) | 30 (1%) | .45 |
| Stroke | 48 (1%) | 15 (3%) | 33 (1%) | .005 |
| No. mobility impairments (mean; SD) | 2.44 (2.71) | 1.32 (1.99) | <.0001 | |
| Arthritis | 1,097 (32%) | 237 (42%) | 860 (30%) | <.0001 |
| Depression | 47 (1%) | 11 (2%) | 36 (1%) | .20 |
| Depressive symptoms | 540 (16%) | 226 (40%) | 314 (11%) | <.0001 |
| Health behaviors over the follow-upa | ||||
| Consistent weekly MVPA | 1,746 (52%) | 221 (40%) | 1,525 (54%) | <.0001 |
| Consistent five daily fruit & veg intake | 686 (24%) | 90 (21%) | 596 (25%) | .07 |
| Consistently overweight/obese BMI | 1,462 (65%) | 208 (59%) | 1,254 (66%) | .02 |
| Daily alcohol at any time point | 1,050 (42%) | 133 (34%) | 917 (43%) | .001 |
| Smoking at any time point | 449 (13%) | 91 (16%) | 358 (13%) | .02 |
MVPA moderate-to-vigorous physical activity; BMI body mass index.
aNumbers in the rows for the health behaviors may not sum to 3,392 due to missing outcome data.
Table 3 shows multivariable-adjusted associations between baseline social isolation and health behaviors over the 10 year follow-up. After adjusting for age and sex in Model Set 1, social isolation (high vs. low) was associated with reduced likelihoods of engaging in weekly MVPA (RR = 0.77; 95% CI: 0.68–0.87), consuming five daily fruit and vegetable servings (RR = 0.74; 95% CI: 0.58–0.95), being consistently overweight or obese (RR = 0.84; 95% CI: 0.75–0.94), and consuming alcohol daily at any time point (RR = 0.80; 95% CI: 0.68–0.95), and increased likelihood of smoking at any time point (RR = 1.84; 95% CI: 1.50–2.26). These RRs were moderately attenuated with adjustment for sociodemographic factors in Model Set 2, but all remained statistically significant except for daily alcohol consumption and fruit and vegetable intake, which was of borderline statistical significance (defined as upper limit of 95% CI between 1.00 and 1.05). Further adjustment for health indicators in Model Set 3, loneliness in Model Set 4, and depression and depressive symptoms in Model Set 5 negligibly altered the remaining RRs, indicating that they minimally influenced the relationship between social isolation and health behaviors reported over the follow-up (Table 3). The subgroup analysis of smokers showed that social isolation was not significantly associated with successfully quitting smoking over the follow-up (fully adjusted RR = 1.49; 95% CI: 0.75–2.97), although this estimate is imprecise due to the small number of smokers who successfully quit over the follow-up.
Table 3.
Population-weighted, Multivariable-adjusted Associations Between Social Isolation and Health Behaviors, English Longitudinal Study of Ageing (ELSA), 2004 to 2015
| Model | Longitudinal health behaviors | RRa (95% CI) High vs. low social isolation |
|---|---|---|
| Consistent weekly MVPA (n = 3,387) | ||
| 1 | Age + sex | 0.77 (0.68, 0.87) |
| 2 | Model 1 + sociodemographicsa | 0.85 (0.76, 0.97) |
| 3 | Model 2 + health indicatorsb | 0.86 (0.77, 0.97) |
| 4 | Model 3 + loneliness | 0.86 (0.77, 0.97) |
| 5 | Model 4 + depression and CES-D score | 0.86 (0.77, 0.97) |
| Consistent five daily fruit & veg intake (n = 2,858) | ||
| 1 | Age + sex | 0.74 (0.58, 0.95) |
| 2 | Model 1 + sociodemographicsa | 0.79 (0.62, 1.02) |
| 3 | Model 2 + health indicatorsb | 0.80 (0.62, 1.03) |
| 4 | Model 3 + loneliness | 0.80 (0.62, 1.04) |
| 5 | Model 4 + depression and CES-D score | 0.80 (0.62, 1.04) |
| Consistently overweight/obese BMI (n = 2,261) | ||
| 1 | Age + sex | 0.84 (0.75, 0.94) |
| 2 | Model 1 + sociodemographicsa | 0.85 (0.76, 0.95) |
| 3 | Model 2 + health indicatorsb | 0.86 (0.77, 0.96) |
| 4 | Model 3 + loneliness | 0.86 (0.77, 0.96) |
| 5 | Model 4 + depression and CES-D score | 0.86 (0.77, 0.97) |
| Daily alcohol at any time point (n = 2,524) | ||
| 1 | Age + sex | 0.80 (0.68, 0.95) |
| 2 | Model 1 + sociodemographicsa | 0.91 (0.77, 1.08) |
| 3 | Model 2 + health indicatorsb | 0.90 (0.76, 1.07) |
| 4 | Model 3 + loneliness | 0.90 (0.76, 1.07) |
| 5 | Model 4 + depression and CES-D score | 0.90 (0.76, 1.07) |
| Smoking at any time point (n = 3,389) | ||
| 1 | Age + sex | 1.84 (1.50, 2.25) |
| 2 | Model 1 + sociodemographicsa | 1.46 (1.18, 1.82) |
| 3 | Model 2 + health indicatorsb | 1.46 (1.17, 1.82) |
| 4 | Model 3 + loneliness | 1.47 (1.18, 1.83) |
| 5 | Model 4 + depression and CES-D score | 1.46 (1.17, 1.82) |
MVPA moderate-to-vigorous physical activity; CES-D Centre for Epidemiologic Studies Depression Scale; BMI body mass index.
aSociodemographic factors are ethnicity, marital status, net non-pension wealth quintile, and educational attainment.
bHealth indicators are limiting long-standing illness, cancer, diabetes, heart disease, stroke, chronic lung disease, mobility impairment, and arthritis.
Table 4 shows multivariable-adjusted associations between baseline loneliness and health behaviors over the 10 year follow-up. After adjusting for age and sex in Model Set 1, loneliness was significantly associated with reduced likelihoods of engaging in weekly MVPA (RR = 0.75; 95% CI: 0.66–0.84), drinking alcohol daily (RR = 0.83; 95% CI: 0.71–0.98), and increased likelihood of smoking at any time point (RR = 1.27; 95% CI: 1.02–1.58). It was borderline statistically significantly associated with consumption of five daily fruit and vegetable servings (RR = 0.82; 95% CI: 0.67–1.01) and being consistently overweight or obese (RR = 0.93; 95% CI: 0.85–1.02). After full adjustment for covariates, loneliness was not significantly associated with any of the health behaviors (Table 4). In the subgroup analysis of smokers, loneliness was negatively associated with successfully quitting smoking over the follow-up (fully adjusted RR = 0.31; 95% CI: 0.11–0.90).
Table 4.
Population-weighted, Multivariable-adjusted Associations Between Loneliness and Health Behaviors, English Longitudinal Study of Ageing (ELSA), 2004 to 2015
| Model | Longitudinal health behaviors | RRa (95% CI) High vs. low loneliness |
|---|---|---|
| Consistent weekly MVPA (n = 3,387) | ||
| 1 | Age + sex | 0.75 (0.66, 0.84) |
| 2 | Model 1 + sociodemographicsa | 0.84 (0.75, 0.94) |
| 3 | Model 2 + health indicatorsb | 0.94 (0.84, 1.04) |
| 4 | Model 3 + social isolation | 0.94 (0.84, 1.04) |
| 5 | Model 4 + depression and CES-D score | 0.97 (0.88, 1.09) |
| Consistent five daily fruit & veg intake (n = 2,858) | ||
| 1 | Age + sex | 0.82 (0.67. 1.01) |
| 2 | Model 1 + sociodemographicsa | 0.88 (0.71, 1.08) |
| 3 | Model 2 + health indicatorsb | 0.87 (0.70, 1.08) |
| 4 | Model 3 + social isolation | 0.87 (0.70, 1.08) |
| 5 | Model 4 + depression and CES-D score | 0.93 (0.75, 1.15) |
| Consistently overweight/obese BMI (n = 2,261) | ||
| 1 | Age + sex | 0.93 (0.85, 1.02) |
| 2 | Model 1 + sociodemographicsa | 0.93 (0.85, 1.02) |
| 3 | Model 2 + health indicatorsb | 0.92 (0.83, 1.01) |
| 4 | Model 3 + social isolation | 0.92 (0.83, 1.01) |
| 5 | Model 4 + depression and CES-D score | 0.92 (0.84, 1.02) |
| Daily alcohol at any time point (n = 2,524) | ||
| 1 | Age + sex | 0.83 (0.71, 0.98) |
| 2 | Model 1 + sociodemographicsa | 0.97 (0.83, 1.13) |
| 3 | Model 2 + health indicatorsb | 0.99 (0.84, 1.15) |
| 4 | Model 3 + social isolation | 0.99 (0.85, 1.16) |
| 5 | Model 4 + depression and CES-D score | 1.01 (0.86, 1.18) |
| Smoking at any time point (n = 3,389) | ||
| 1 | Age + sex | 1.27 (1.02, 1.58) |
| 2 | Model 1 + sociodemographicsa | 0.99 (0.78, 1.23) |
| 3 | Model 2 + health indicatorsb | 0.93 (0.74, 1.17) |
| 4 | Model 3 + social isolation | 0.91 (0.72, 1.15) |
| 5 | Model 4 + depression and CES-D score | 0.88 (0.69, 1.11) |
MVPA moderate-to-vigorous physical activity; CES-D Centre for Epidemiologic Studies Depression Scale; BMI body mass index.
aSociodemographic factors are ethnicity, marital status, net non-pension wealth quintile, and educational attainment.
bHealth indicators are limiting long-standing illness, cancer, diabetes, heart disease, stroke, chronic lung disease, mobility impairment, and arthritis.
The inverse relationships between social isolation, loneliness, and overweight/obesity were unexpected. Given that age modifies the relationship between BMI and health outcomes in elderly adults, whereby low BMI among adults over age 65 is predictive of poor health and increased mortality risk, we conducted three post hoc sensitivity analyses to further examine the role of BMI dynamics in our results. As shown in the Supplementary Material, removal of participants with low BMI (each of <18.5 and <20) did not affect the results, indicating that the inverse relationship we observed was not due to isolated participants being underweight. There was no evidence of effect modification by age group, either stratified at age 65 or by decade of life, indicating that the inverse relationship between BMI and health status in older adults did not influence the overall result. Finally, BMI category at any single time point did not appear to drive the results, indicating that potentially different trajectories of weight loss between the low versus high isolation groups did not affect the results. The sensitivity analyses for loneliness showed similar results (Supplementary Material).
There were no indications of statistical interactions between social isolation and loneliness in predicting the health behavior outcomes, with the following p-values for multiplicative interaction terms in the final models: p =.89 (MVPA), p =.88 (fruit and vegetable intake), p =.39 (BMI), p =.86 (alcohol consumption), and p =.16 (smoking). There was also no indication that gender moderated the relationships between either social isolation or loneliness with the health behavior outcomes (all p-value >.05). The results were also not significantly altered when marital status, rather than living alone, was included in the social isolation index (Supplementary Material). In this analysis, the RRs were somewhat smaller than in the original analysis, indicating that marital status may have a weaker association with health behavior than does living alone.
Discussion
In this longitudinal study of English adults aged ≥52 years over a 10 year period, social isolation was negatively associated with consistent engagement in weekly MVPA, consistent consumption of five daily fruit and vegetable servings, and being overweight or obese at any time point. It was positively associated with smoking at any time point. There was no association between social isolation and daily alcohol consumption over the 10 year follow-up. These relationships indicate that social isolation is associated with less desirable and inconsistent engagement in health-promoting behaviors over time among older adults. Loneliness was not associated with any health behaviors or overweight/obesity over the 10 year follow-up, although it was negatively associated with successful smoking cessation among smokers. The implications of loneliness for older smokers require investigation in other longitudinal studies with a greater number of smokers than were included in this study. Overall, our findings indicate that among the general population of older English adults, social isolation, but not loneliness, might have consequences for longer term patterns of health-related behaviors.
Our findings are consistent with studies that have found relationships between social isolation and physical activity, diet, smoking, and obesity [20,33–35,37,39] but inconsistent with those finding patterns of alcohol abuse and abstinence to be associated with isolation [36,40]. Our results are also consistent with other findings using the ELSA data, which found that social isolation (defined according to marital status, rather than living alone) was prospectively associated with declines in physical mobility and cognitive function, and risk of all-cause mortality [9,15,61]. The negative relationship with overweight/obesity that we observed was unexpected and may be due to uncaptured subclinical health conditions or restricted eating behaviors that would cause lower BMI among isolated or lonely adults [62]. Our findings are also inconsistent with those observing relationships between loneliness and health behaviors [4,20,41–44], especially one observing that baseline loneliness predicted reduced odds of physical activity over a 2 year follow-up in 229 older American adults [43]. These previous studies were all cross-sectional except for one and could not examine whether the observed relationships persisted over time. Differing methods of physical activity assessment across studies, such as differing scales of activity frequency, duration, or type, may also explain these inconsistent findings. No other studies have investigated social isolation or loneliness in relation to smoking cessation, as none have been able to longitudinally investigate smoking as an outcome. Only one other study has accounted for both social isolation and loneliness, also using the ELSA data in a cross-sectional analysis of the 2004/05 wave [20]. Our finding that smoking was associated with isolation, but not loneliness, is consistent with theirs, although they found that both loneliness and isolation were associated with reduced odds of weekly physical activity [20]. Overall, our findings indicate that longitudinal studies are necessary to understand the relationships between affective states and health-related behaviors.
In this large, population-representative sample of older English adults, our results support the notion that social isolation may lead to non-engagement in healthy behaviors [17]. Social isolation may reduce or remove any direct sense of obligation to stay well for loved ones, may exempt one from broader group-based social norms that promote health, and result in a lack of instrumental or emotional social support that can help promote healthy behaviors [17,25–28]. Future work should examine whether different modes of social connections, such as face-to-face, over the telephone, or online, have differential effects on influencing health behaviors over time. For older adults who are lonely, social connections may still be in place despite the unpleasant affective experience of feeling alone. Theoretical work emphasizes that the clinical outcomes of loneliness, including increased mortality risk, may be predominantly through non-behavioral mechanisms such as chronic stress, dysregulation of coping mechanisms, cognitive dysfunction, and systemic inflammation [2,29]. Among smokers, however, loneliness appeared to have a negative association with smoking cessation. An important consideration is that we did not have measures of social isolation, loneliness, or health behaviors from earlier in life. From a life course perspective, social relationships may influence health behaviors from childhood through older age, and we may be observing long-term social behavioral processes set into motion in earlier life [63]. Comparable evidence from early- and mid-life cohorts would help illuminate the progressive links between social relationships and health behaviors across the whole life course. For now, our results indicate that the health-related behavioral associations of social isolation may remain in place for periods of at least 10 year among older adults.
Although theoretical and empirical research in this area consistently point to social isolation effects on health behavior, reverse causality is possible in our findings. This is particularly true for smoking and alcohol consumption, due to their negative effects on social integration. Smoking is typically initiated early in life, and it might lead to social withdrawal and subsequent isolation over time through its adverse effects on mood [64]. Using data from the Framingham Heart Study, Christakis et al. have found that as smoking behavior has become less normative in the population over time, long-term smokers tend to get pushed to the peripheries of social networks [39]. Our results may have in part captured this reverse direction of association. We did observe that loneliness was negatively associated with smoking cessation among baseline smokers, although the number of participants who successfully quit without relapsing was small (n = 40), and the finding for social isolation was imprecise. Heavy alcohol consumption can also result in social withdrawal, although our alcohol measure had poor sensitivity to capture true heavy drinking, as it assessed frequency rather than volume of consumption. Furthermore, longitudinal research should examine the temporal dynamics of social isolation, loneliness, smoking cessation, and alcohol abuse in older adults.
A limitation of our study is that the health behaviors were assessed by self-report. Recall error would bias the RRs in a direction that would depend on whether it was random (bias towards the null) or differential according to loneliness or social isolation (bias in a direction that would depend on the overall direction of under- or over-estimates of behaviors in each group). Reassuringly, the overall frequencies of self-reported health behaviors in this study are similar to those reported in the population-representative Health Survey for England [65–67]. We categorized the health behaviors according to UK public health recommendations and evidence on their associations with health outcomes [47–58]. Although the response format for fruit and vegetable intake changed between 2008/09 and 2010/11, the median values at each time point were 5.0 or close to 5.0, meaning that the outcome variable approximately represents a median split in intake at each follow-up time point, regardless of the change in response format. Those who dropped out or died over the follow-up were more likely to be socially isolated and lonely at baseline than those who remained in the study (Supplementary Material). They were also more likely to be men, to have lower net non-pension wealth, to have no educational attainment, to be non-white, and to be in worse health than those who remained (Supplementary Material). This was addressed through the use of population-based longitudinal weights that iteratively accounted for non-response to the Health Survey for England and all waves of the ELSA in all statistical models to ensure the sample was representative of the target general population [60].
In conclusion, this study indicates that social isolation is associated with a range of health-related behaviors over a 10 year follow-up period among older English adults. Loneliness was not associated with any persistent health-related behaviors, although loneliness was negatively associated with smoking cessation among smokers. These findings require replication in other longitudinal cohorts of aging. These longitudinal findings were independent of a range of sociodemographic factors and health indicators, including functional mobility and depression. Our results support the notion that social isolation affects health outcomes such as mortality through behavioral pathways. On balance, the consistent evidence for poor health outcomes associated with social isolation and loneliness warrants the development of psychosocial interventions to improve social engagement and reduce feelings of loneliness among older adults. Future studies could examine the best possible ways to help isolated and lonely older adults to connect and stay connected with others in ways that help them to sustain health-promoting behaviors and overall health and well-being.
Supplementary Material
Supplementary material is available at Annals of Behavioral Medicine online.
Compliance with Ethical Standards
Funding The ELSA is funded by the National Institute of Aging in the USA (grant numbers 2RO1AG7644-01A1, 2RO1AG017644) and a consortium of UK government departments coordinated by the Economic and Social Research Council.
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards The authors Kobayashi and Steptoe declare that they have no conflict of interest. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Ethical Approval The London Multicentre Research Ethics Committee granted ethical approval for the ELSA (MREC/01/2/91).
Informed consent Informed consent was obtained from all participants.
Author Contributions LCK conceived of the study; LCK and AS designed the study; LCK conducted the statistical analysis and wrote the first draft of the manuscript; LCK and AS interpreted the results, revised the manuscript for important intellectual content, and approved of the final manuscript for submission. All authors had full access to all of the data (including statistical reports and tables) in the study and take full responsibility for the integrity of the data and accuracy of the statistical analysis.
References
- 1. Cacioppo JT, Hawkley LC, Norman GJ, Berntson GG. Social isolation. Ann N Y Acad Sci. 2011; 1231(1): 17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hawkley LC, Cacioppo JT. Aging and loneliness: Downhill quickly?Curr Dir Psychol Sci. 2007; 16(4): 187– 191. [Google Scholar]
- 3. McPherson M, Smith-Lovin L, Brashears ME. Social isolation in America: Changes in core discussion networks over two decades. Am Sociol Rev. 2006; 73(3): 353–375. [Google Scholar]
- 4. Stickley A, Koyanagi A, Roberts B, et al. Loneliness: Its correlates and association with health behaviours and outcomes in nine countries of the former Soviet Union. PLoS One. 2013; 8(7): e67978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kearns A, Whitley E, Tannahill C, Ellaway A. Loneliness, social relations and health and well-being in deprived communities. Psychol Health Med. 2015; 20(3): 332–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rico-Uribe LA, Caballero FF, Olaya B, et al. Loneliness, social networks, and health: A cross-sectional study in three Countries. PLoS One. 2016; 11(1): e0145264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cruwys T, Dingle GA, Haslam C, Haslam SA, Jetten J, Morton TA. Social group memberships protect against future depression, alleviate depression symptoms and prevent depression relapse. Soc Sci Med. 2013; 98(1): 179–186. [DOI] [PubMed] [Google Scholar]
- 8. Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychol Aging. 2006; 21(1): 140–151. [DOI] [PubMed] [Google Scholar]
- 9. Shankar A, Hamer M, McMunn A, Steptoe A. Social isolation and loneliness: Relationships with cognitive function during 4 years of follow-up in the English Longitudinal Study of Ageing. Psychosom Med. 2013; 75(2): 161–170. [DOI] [PubMed] [Google Scholar]
- 10. Bassuk SS, Glass TA, Berkman LF. Social disengagement and incident cognitive decline in community-dwelling elderly persons. Ann Intern Med. 1999; 131(3): 165–173. [DOI] [PubMed] [Google Scholar]
- 11. Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends Cogn Sci. 2009; 13(10): 447–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Holt-Lunstad J, Smith TB. Loneliness and social isolation as risk factors for CVD: Implications for evidence-based patient care and scientific inquiry. Heart. 2016; 102(13): 987–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. Heart. 2016; 102(13): 1009–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect Psychol Sci. 2015; 10(2): 227–237. [DOI] [PubMed] [Google Scholar]
- 15. Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci USA. 2013; 110(15): 5797–5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Berkman LF, Syme SL. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979; 109(2): 186–204. [DOI] [PubMed] [Google Scholar]
- 17. Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000; 51(6): 843–857. [DOI] [PubMed] [Google Scholar]
- 18. Loucks EB, Sullivan LM, D’Agostino RB Sr, Larson MG, Berkman LF, Benjamin EJ. Social networks and inflammatory markers in the Framingham Heart Study. J Biosoc Sci. 2006; 38(6): 835–842. [DOI] [PubMed] [Google Scholar]
- 19. Ford ES, Loucks EB, Berkman LF. Social integration and concentrations of C-reactive protein among US adults. Ann Epidemiol. 2006; 16(2): 78–84. [DOI] [PubMed] [Google Scholar]
- 20. Shankar A, McMunn A, Banks J, Steptoe A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 2011; 30(4): 377–385. [DOI] [PubMed] [Google Scholar]
- 21. Kiecolt-Glaser JK, Gouin JP, Hantsoo L. Close relationships, inflammation, and health. Neurosci Biobehav Rev. 2010; 35(1): 33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yang YC, McClintock MK, Kozloski M, Li T. Social isolation and adult mortality: The role of chronic inflammation and sex differences. J Health Soc Behav. 2013; 54(2): 183–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Clouston SA, Brewster P, Kuh D, et al. The dynamic relationship between physical function and cognition in longitudinal aging cohorts. Epidemiol Rev. 2013; 35(1): 33–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Peel NM, McClure RJ, Bartlett HP. Behavioral determinants of healthy aging. Am J Prev Med. 2005;28(3):298–304. [DOI] [PubMed] [Google Scholar]
- 25. Emmons KM, Barbeau EM, Gutheil C, Stryker JE, Stoddard AM. Social influences, social context, and health behaviors among working-class, multi-ethnic adults. Health Educ Behav. 2007; 34(2): 315–334. [DOI] [PubMed] [Google Scholar]
- 26. Tucker JS. Health-related social control within older adults’ relationships. J Gerontol B Psychol Sci Soc Sci. 2002; 57(5): P387–P395. [DOI] [PubMed] [Google Scholar]
- 27. Umberson D. Family status and health behaviors: Social control as a dimension of social integration. J Health Soc Behav. 1987; 28(3): 306–319. [PubMed] [Google Scholar]
- 28. Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Rimer BK, Viswanath K, eds. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed San Francisco: Jossey-Bass; 2008: 189–207. [Google Scholar]
- 29. Hawkley LC, Cacioppo JT. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010; 40(2): 218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009; 50(1): 31–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010; 25(2): 453–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cornwell EY, Waite LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP study. J Gerontol B Psychol Sci Soc Sci. 2009; 64 (Suppl 1): i38–i46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Locher JL, Ritchie CS, Roth DL, Baker PS, Bodner EV, Allman RM. Social isolation, support, and capital and nutritional risk in an older sample: Ethnic and gender differences. Soc Sci Med. 2005; 60(4): 747–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kharicha K, Iliffe S, Harari D, Swift C, Gillmann G, Stuck AE. Health risk appraisal in older people 1: Are older people living alone an “at-risk” group?Br J Gen Pract. 2007; 57(537): 271–276. [PMC free article] [PubMed] [Google Scholar]
- 35. Ramlagan S, Peltzer K, Phaswana-Mafuya N. Social capital and health among older adults in South Africa. BMC Geriatr. 2013; 13(1): 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shiovitz-Ezra S, Litwin H. Social network type and health-related behaviors: Evidence from an American national survey. Soc Sci Med. 2012; 75(5): 901–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Watt RG, Heilmann A, Sabbah W, et al. Social relationships and health related behaviors among older US adults. BMC Public Health. 2014;14: 533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007; 357(4): 370–379. [DOI] [PubMed] [Google Scholar]
- 39. Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008; 358(21): 2249–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rosenquist JN, Murabito J, Fowler JH, Christakis NA. The spread of alcohol consumption behavior in a large social network. Ann Intern Med. 2010; 152(7): 426–33, W141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lauder W, Mummery K, Jones M, Caperchione C. A comparison of health behaviours in lonely and non-lonely populations. Psychol Health Med. 2006; 11(2): 233–245. [DOI] [PubMed] [Google Scholar]
- 42. Dyal SR, Valente TW. A systematic review of loneliness and smoking: Small effects, big implications. Subst Use Misuse. 2015; 50(13): 1697–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: Cross-sectional & longitudinal analyses. Health Psychol. 2009; 28(3): 354–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Netz Y, Goldsmith R, Shimony T, Arnon M, Zeev A. Loneliness is associated with an increased risk of sedentary life in older Israelis. Aging Ment Health. 2013; 17(1): 40–47. [DOI] [PubMed] [Google Scholar]
- 45. Steptoe A, Breeze E, Banks J, Nazroo J. Cohort profile: The English longitudinal study of ageing. Int J Epidemiol. 2013; 42(6): 1640–1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Russell DW. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J Pers Assess. 1996; 66(1): 20–40. [DOI] [PubMed] [Google Scholar]
- 47. Friedenreich CM, Orenstein MR. Physical activity and cancer prevention: Etiologic evidence and biological mechanisms. J Nutr. 2002; 132(11 Suppl): 3456S–3464S. [DOI] [PubMed] [Google Scholar]
- 48. Hamer M, de Oliveira C, Demakakos P. Non-exercise physical activity and survival: English longitudinal study of ageing. Am J Prev Med. 2014; 47(4): 452–460. [DOI] [PubMed] [Google Scholar]
- 49. Samitz G, Egger M, Zwahlen M. Domains of physical activity and all-cause mortality: Systematic review and dose-response meta-analysis of cohort studies. Int J Epidemiol. 2011; 40(5): 1382–1400. [DOI] [PubMed] [Google Scholar]
- 50. World Health Organization. Global Recommendations on Physical Activity for Health. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 51. National Health Service. 5 A day [Internet]. NHS choices 2013. [accessed 2017 April 23]. Available from: http://www.nhs.uk/livewell/5aday/Pages/5ADAYhome.aspx.
- 52. Hamer M, Lavoie KL, Bacon SL. Taking up physical activity in later life and healthy ageing: The English longitudinal study of ageing. Br J Sports Med. 2014; 48(3): 239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: A comprehensive dose-response meta-analysis. Br J Cancer. 2015; 112(3): 580–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ford ES, Zhao G, Tsai J, Li C. Low-risk lifestyle behaviors and all-cause mortality: Findings from the National Health and Nutrition Examination Survey III Mortality Study. Am J Public Health. 2011; 101(10): 1922–1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: The EPIC-Norfolk prospective population study. PLoS Med. 2008; 5(1): e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kvaavik E, Batty GD, Ursin G, Huxley R, Gale CR. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: The United Kingdom health and lifestyle survey. Arch Intern Med. 2010; 170(8): 711–718. [DOI] [PubMed] [Google Scholar]
- 57. Ness AR, Powles JW. Fruit and vegetables, and cardiovascular disease: A review. Int J Epidemiol. 1997; 26(1): 1–13. [DOI] [PubMed] [Google Scholar]
- 58. NHS Choices. Alcohol units and guidelines: The lower risk daily guidelines [Internet]. Change 4 Life 2015. [accessed 2017 April 23]. Available from: http://www.nhs.uk/change4life/Pages/alcohol-lower-risk-guidelines-units.aspx.
- 59. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004; 159(7): 702–706. [DOI] [PubMed] [Google Scholar]
- 60. Littleford C, Hussey D, Begum N, Oskala A. Methodology. In: Banks J, Batty GD, Nazroo J, Steptoe A, eds. The Dynamics of Ageing: Evidence from the English Longitudinal Study of Ageing 2002–15 (Wave 7). London: Institute for Fiscal Studies; 2016. 141–170. [Google Scholar]
- 61. Shankar A, McMunn A, Demakakos P, Hamer M, Steptoe A. Social isolation and loneliness: Prospective associations with functional status in older adults. Health Psychol. 2017; 36(2): 179–187. [DOI] [PubMed] [Google Scholar]
- 62. Janssen I, Katzmarzyk PT, Ross R. Body mass index is inversely related to mortality in older people after adjustment for waist circumference. J Am Geriatr Soc. 2005; 53(12): 2112–2118. [DOI] [PubMed] [Google Scholar]
- 63. Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across life course. Annu Rev Sociol. 2010; 36(1): 139–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Glassman AH, Helzer JE, Covey LS, et al. Smoking, smoking cessation, and major depression. JAMA. 1990; 264(12):1546–1549. [PubMed] [Google Scholar]
- 65. Chaudhury M, Esliger D. Accelerometry in adults. In: Craig R, Mindell J, Hirani V, eds. Health Survey for England 2008. London: The Health and Social Care Information Centre; 2009. 59–78. [Google Scholar]
- 66. Fat LN. Adult cigarette smoking. In: Craig R, Mindell J, eds. Health Survey for England 2013. Leeds: The Health and Social Care Information Centre; 2013. 1–38. [Google Scholar]
- 67. Lifestyle Statistics Team. Statistics on alcohol: England, 2015 [Internet] Leeds; 2015. [accessed 2017 April 23]. Available from: http://www.hscic.gov.uk/catalogue/PUB17712/alc-eng-2015-rep.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.