Abstract
Prostate cancer is third common malignancy in men of old age (average 65 years) in Myanmar. Currently, serum PSA and bone scan are the markers of choice. Because of the evidence-based, promising success of 68Ga-PSMA PET-CT and 177Lu-PSMA theranostics in prostate cancer worldwide, 99mTc-PSMA SPECT-CT imaging and 177Lu-PSMA therapy has launched as a stepping-stone of theranostics in Myanmar with the available facilities. Twelve cases of prostate cancer patients were imaged with 600 MBq of 99mTc-PSMA I+S SPECT-CT. Four metastatic castration resistant prostate cancer (MCRPC) patients with abnormal result were treated with 177Lu-PSMA. The protocol consists of 6–8 GBq of 177Lu-PSMA, three successive doses at interval of 4–6 weeks. Post-therapy SPECT-CT imaging was done. All treated patients were improved by free of bone pain, and fall/rise in serum PSA level. Two patients with extensive skeletal metastases succumbed to complications. The results are well documented and present at the multidisciplinary conferences for clinical awareness. Theranostics in prostate cancer with available facilities is an additional boon to our health care professionals to upgrade cancer management in Myanmar. This paper provides the technology with cost effectiveness and benefit to prostate cancer patients of Myanmar.
Keywords: Theranostics, SPECT-CT, PET-CT, PSMA, Lutetium-177, Prostate cancer
Long Journey to Theranostics, from the Beginning
Myanmar (the then called Burma) inaugurated nuclear medicine service for her people’s health care system since 1963. It happened after Dr. Soe Myint’s pioneering effort under guidance of the Government of Myanmar in collaboration with International Atomic Energy Agency (IAEA). Radioisotope department was founded at the Yangon General Hospital (YGH) as a separate specialty, after the visit of Dr. E. H. Belcher, the then head of Divisions of Life Sciences, IAEA and the first IAEA expert service of Dr. R. Hoschl from Czechoslovakia in June 1965 (Fig. 1).
Fig. 1.
Department of Nuclear Medicine, Yangon General Hospital: past (1963) and present (2015)
Second IAEA expert mission, Dr. L. Kertez from Hungary, developed radiopharmacy techniques in 1974. Imaging followed it with OHIO Nuclear Gamma Camera donated by the Japanese Government in March 1975. IAEA expert, Dr. R. D. Piyasena from Sri Lanka, inaugurated in vitro section in 1982. Ministry of Health, Government of Myanmar and IAEA, has played a pivotal role in the development and sustainability of nuclear medicine services in Myanmar since then. Radioactive 131I was the drug of choice in diagnosis and therapy of thyrotoxicosis and differentiated thyroid cancer patients (very primitive theranostics).
PET-CT has become the only powerful diagnostic tool in medicine globally since year 2000. It detects metabolic activity as well as anatomical localization. The first dream came in after attending the IAEA organized project planning meeting on “Tumour Imaging (SPECT-CT & PET-CT) using radioisotopes”, RAS/6/042, Chiba, Japan, in April 2005. The Ministry of Health, Government of Myanmar, has put the tremendous and relentless effort to set up PET-CT and cyclotron at the Department of Nuclear Medicine, YGH during 3-year project (2012–2015). It was a huge, tremendous, adventurous, and challenging project for the developing country like Myanmar.
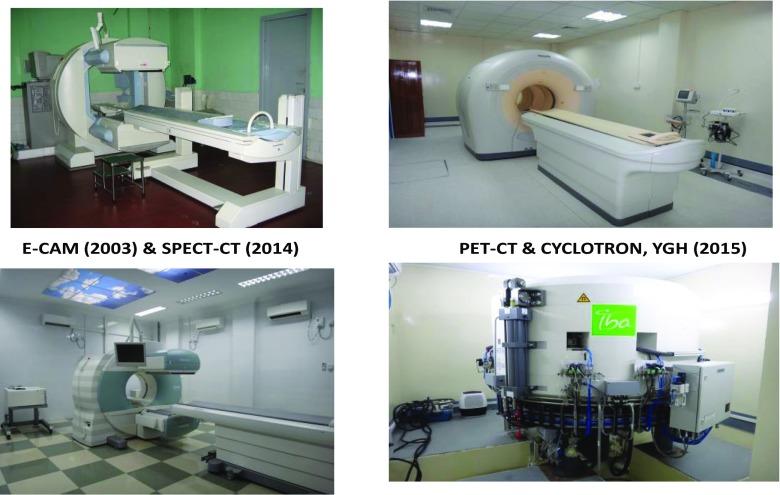
PET-CT imaging provides effective tool to cancer patients in accurate diagnosis, staging, restaging, and management. The referring physician sooner and later acknowledges PET/CT as a great boon to upgrade health care system. The Department of Nuclear Medicine, YGH, has been traveling a long journey from rectilinear scanner (1979) to SPECT-CT and PET-CT (2014–2015) (Figs. 2 and 3). It was the only center throughout the country of about 50 million population until 1998. By now, the country owns 4 departments in public, 1 in defense service, and 2 in private hospitals.
Fig. 2.
A long journey of nuclear medicine in Myanmar from rectilinear scanner (1979) to SPECT-CT and PET-CT (2014–2015)
Fig. 3.
Infrastructures at Department of Nuclear Medicine, Yangon General Hospital
Another dream came in after attending the IAEA organized pre-coordination meeting of RAS/0/063 “Regional meeting on project design of PRRT”, VIC, Vienna, Austria in February 2013.
In Myanmar, the incidence of prostate cancer is 4.3 per 100,000 population and third most common cancer among men of old age (average 65 years). Prostate cancer is the fourth most common malignancy worldwide. Serum PSA is the marker of choice with highest positive predictive value. Regarding staging of the disease, ultrasonography, CT, MRI, and 99mTc-MDP SPECT-CT bone scintigraphy have advised as choices of investigations. Currently, 68Ga-PSMA and 177Lu-PSMA theranostics is evidence-based, promising success in the management of prostate cancer worldwide [1]. As the gallium-68 generator is not available in Myanmar, 99mTc-PSMA I+S and 177Lu-PSMA theranostics with the available facilities (SPECT-CT) has inaugurated as a stepping-stone in 2017 [2].
This pilot study is the dawn of theranostics in Myanmar. Myanmar is one of the developing countries in Asia and Pacific region. The people could not afford costly high-tech imaging studies for diagnosis and therapy. 99mTc-PSMA I+S imaging for prostate cancer diagnosis is a non-invasive, cost effective, and provides an additional boon to our health care system. The study has been beneficial to prostate cancer management in both public and private hospitals.
The Ministry of Health, Government of Myanmar in collaboration with IAEA and a number of international organizations, has been playing a great role in strengthening and sustainability of nuclear medicine services throughout the country.
Clinical Study
Twelve cases of prostate cancer patients were imaged with 600 MBq of 99mTc-PSMA I+S SPECT-CT. The radiopharmaceutical labeling, quality control, and imaging protocol were done according to the vendor’s guideline. Four metastatic castration-resistant prostate cancer (MCRPC) patients were treated with 177Lu-PSMA after abnormal 99mTc-PSMA I+S SPECT-CT imaging at the nuclear medicine department of a private clinics, PERFECT Myanmar Molecular Imaging and Therapy Center (PERFECT MMITC). One out of these 4 cases had already taken 68Ga-PSMA PET-CT imaging in abroad. These two imaging results were processed to compare. Informed consents were obtained from all treated patients prior to the study. Therapy protocol was trained hands-on and guided by a well-experienced expert from abroad. Patients were treated with 6 to 8 GBq of 177Lu-PSMA each patient for three doses at interval of 4 weeks. Placing ice packs over both parotid regions was done before, during, and after 177Lu therapy. Total dose for each patient was 18 to 24 GBq. Post-therapy SPECT-CT imaging was done on the next day. 177Lu-PSMA labeling, radiopharmaceutical administration, and radiation protection practice guided by the expert was followed systematically. Dosimetry of 177Lu-PSMA for these patients had not done yet. Follow-up studies up to 3 successive doses were done.
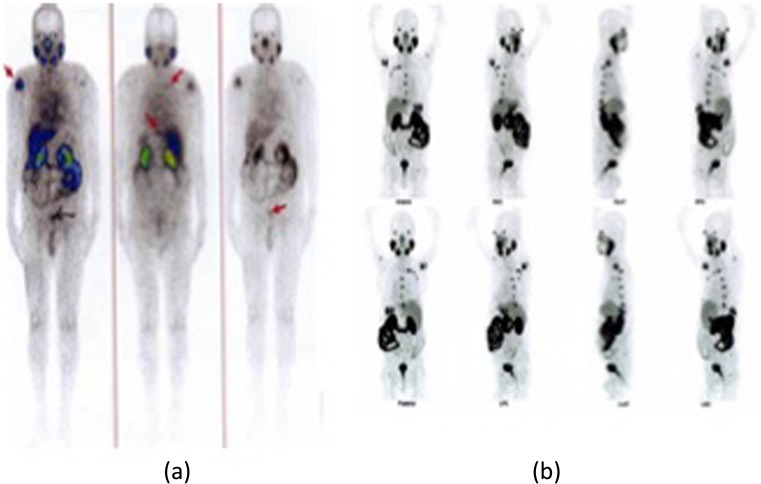
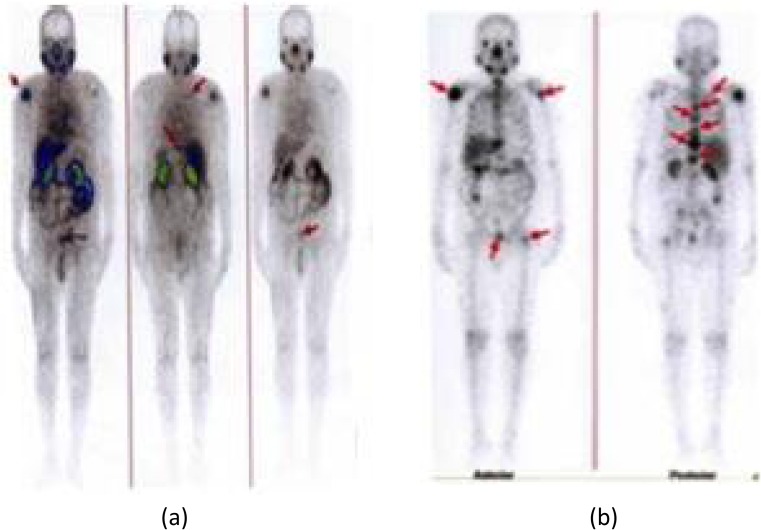
The two images of 99mTc-PSMA SPECT-CT and 68Ga-PSMA PET-CT are comparable (Fig. 4). No abnormal 99mTc-PSMA radiotracer uptake is seen at normal serum PSA level, and normal bone scan. Multiple skeletal and soft tissue radiotracer uptakes are seen in patients with raised serum PSA level, abnormal bone scan, and bone pain. Four MCRPC patients out of these patients with abnormal scan result were treated with 177Lu-PSMA. The outcome of the patient after each 177Lu-PSMA therapy was improved by free of bone pain, fall in serum PSA level in two cases, and serum PSA level rising after each successive doses in another two cases [3]. Those two cases with poor response to therapy, though they gained quality of life, succumb 2 and 8 weeks after third dose due to complications, such as chest infection in one case of 96 years old and anemic heart failure in another case of 76 years old. These two cases already had multiple extensive skeletal metastases with rising PSA level. The results are well documented and present at the multidisciplinary conferences for clinical awareness (Fig. 5 and Tables 1 and 2).
Fig. 4.
Comparison between 99mTc-PSMA I+S SPECT/CT (a) and 68Ga-PSMA PET/CT (b) images
Fig. 5.
Theranostics −99mTc-PSMA I+S imaging (a) and 177Lu-PSMA post-therapy imaging (b)
Table 1.
Baseline demography of four metastatic castration-resistant prostate cancer patients
| Patient | Age (years) | Hb% | PSA level (total) | Bone metastasis | Soft tissue metastasis | Bone pain |
|---|---|---|---|---|---|---|
| 1 | 76 | 10.6 g/dl | 23.16 ng/ml | + | + | + |
| 2 | 56 | 11 g/dl | 58 ng/ml | + | + | + |
| 3 | 96 | 10.7 g/dl | 512 ng/ml | + | + | + |
| 4 | 68 | 11 g/dl | 32 ng/ml | + | + | + |
Table 2.
Review of three successive 177Lu-PSMA therapies
| Patient | Hb% after 177Lu dose | Serum PSA level baseline and after 177Lu dose | Bone pain | Outcome |
|---|---|---|---|---|
| 1 | 9.0 g/dl, 8.7, 8.2 | 48.1 ng/ml, 96.35, 110.4 | _ | Expired |
| 2 | 10.6 g/dl, 10.4, 11.2 | 58 ng/ml, 19, 5.0 | _ | Improved |
| 3 | 10.0 g/dl, 9.5, 8.5 | 1785 ng/ml, > 5000, > 10,000 | _ | Expired |
| 4 | 10.5 g/dl, 10.2, 11.0 | 11.0 ng/ml, 10.5, 4.0 | _ | Improved |
No serious adverse effects and no significant changes in WBC, liver function test and renal function after 177Lu therapy of two responsive cases. But, some effects on hematopoietic system in two advanced cases with multiple extensive skeletal metastases of this small study (reduction in Hb% and platelets count) need blood transfusion and expired after late-effect complications. These two patients also showed raised PSA level significantly after each therapy (resistance to therapy). It can be explained by heterogeneity of PSMA receptor activity within the tumor population that some sites will not respond to treatment and will manifest as disease progression [4]. But, all treated cases had remarkably free of bone pain and improve in quality of life [5] (Table 2).
Conclusion/Suggestion
Although PET-CT and 18F-FDG is available at the public hospital (Department of Nuclear Medicine, YGH), Ga-68 generator is still out of reach because of budgetary constraint. Therefore, 99mTc PSMA I+S SPECT-CT prostate cancer imaging followed by 177Lu PSMA therapy (theranostics) inaugurated at the private center (PERFECT MMITC) in Yangon, Myanmar [2].
Theranostics in Myanmar by now is high cost and could not reach to the poor sufferer. Affordability is a big issue of theranostics. Myanmar health care system has not yet practiced reimbursement program for high costly regime like these, but free of charge for almost all of the services in public hospitals throughout the country. Ministry of Health and Sports, Government of Myanmar, is responsible for all the health issues of its people. It is promoting private sector to share the service these days and private hospitals throughout the country are actively participating in this business by the guidance and expert services of local and international professionals. But, we still need to activate moving further forward to promote and sustainability of this service (theranostics) among the patients and the health care professionals.
Finally, this small pilot study provides information about theranostics in prostate cancer with available facilities. It is cost effective and beneficial tool to our health care professionals as well as cancer patients to upgrade cancer management in Myanmar (Table 3).
Table 3.
Cost effectiveness
| Cost (USD) | Cost (Kyats) | Availability | |
|---|---|---|---|
| 68Ga-PSMA | > 1000.00 | 1500,000.00 | 68Ga generator not available |
| 99mTc-PSMA | 250.00 | 350,000.00 | Easily available |
Acknowledgements
The author would like to express kind appreciation to Dr. Tin Maung Thein, Dr. Thiri Kyi Phyu, Mr. Win Maung (Physicist), and all the staffs of PERFECT MMITC who are actively involved in this pilot study. I convey my sincere thanks to Mr. Kyaw Min Thet who makes photoshop editing of figures in this paper.
Conflict of Interest
Kyin Myint, Tin Maung Thein, Thiri Kyi Pyhu, and Win Maung declare no conflict of interest.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of national research committee.
Informed Consent
Informed consent was obtained from individual patient included in this study according to the protocol approved by the ethical committee and kept confidential.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kyin Myint, Phone: +9595003475, Email: kmnumed@gmail.com.
Tin Maung Thein, Phone: +959977332655, Email: drtinmaungthein.86@gmail.com.
Thiri Kyi Phyu, Phone: +959965098663, Email: a.kyiphyu@gmail.com.
Win Maung, Phone: +959976478268, Email: w.maung67@gmail.com.
References
- 1.Rahbar K, Bode A, Weckesser M, Avaramovic N, Claesener M, Stegger L, et al. Radioligand therapy with 177Lu-PSMA-617 as a novel therapeutic option in patients with metastatic castration resistant prostate Cancer. Clin Nucl Med. 2016;41:522–528. doi: 10.1097/RLU.0000000000001240. [DOI] [PubMed] [Google Scholar]
- 2.Robu S, Schottelius M, Eiber M, Maurer T, Gschwend J, Schwaiger M, et al. Preclinical evaluation and first patient application of 99mTc-PSMA-I&S for SPECT imaging and radioguided surgery in prostate cancer. J Nucl Med. 2017;58:235–242. doi: 10.2967/jnumed.116.178939. [DOI] [PubMed] [Google Scholar]
- 3.Soydal C, Ozkan E, Akyurek S, Kucuk NO. Marked response to 177Lu prostate- specific membrane antigen treatment in patient with metastatic prostate cancer. Clin Nucl Med. 2016;41:159–160. doi: 10.1097/RLU.0000000000001058. [DOI] [PubMed] [Google Scholar]
- 4.Emmett L, Willowson K, Violet J, Shin J, Blanksby A, Lee J. Lutetium-177 PSMA radionuclide therapy for men with prostate cancer: a review of the current literature and discussion of practical aspects of therapy. J Med Radiat Sci. 2017;64:52–60. doi: 10.1002/jmrs.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahbar K, Schmidt M, Heinzel A, Eppard E, Bode A, Yordanova A, et al. Response and tolerability of a single dose of 177Lu-PSMA-617 in patients with metastatic castration resistant prostate cancer: a multicenter retrospective analysis. J Nucl Med. 2016;57:1334–1338. doi: 10.2967/jnumed.116.173757. [DOI] [PubMed] [Google Scholar]