Abstract
Background.
Fine needle aspiration cytology (FNAC) is an important diagnostic tool in a range of medical settings. It is fast, quick and an highly accurate diagnostic method and can be used, in settings with minimal laboratory infrastructures.
Methods.
In this report, we describe the experience in the use of FNAC since it is introduction in 1996 in the Anatomical Pathology Service of the Maputo Central Hospital (MCH), along with more detailed data referring to 2009–2010.
Results.
The number of FNAC analyses increased gradually from 269 (4.1% of all pathologic tests of the Service) in 1996, when it was introduced in Mozambique, to 3234 (17% of all tests) in 2010. Lymph nodes were the organs most frequently biopsied, followed by breast and soft tissues. Inflammatory conditions, especially tuberculosis, were the most frequent diagnoses (22.2% of the cases), followed by hyperplastic conditions (20.6%), benign tumors (13.4%) and malignant tumors (12.3%).
Conclusion.
Our results clearly demonstrate that even in an environment with poor laboratory resources, it is possible to establish a FNAC clinic that can provide a quick and precise diagnosis for clinicians to aid in early treatment interventions, especially in inflammatory diseases which were the majority of our cases.
Keywords: Fine needle aspiration cytology, lymph node, tuberculosis, Mozambique
INTRODUCTION
Fine Needle Aspiration Cytology
Fine needle aspiration cytology (FNAC) is an important diagnostic tool in different medical settings. It is a direct first-line approach to the evaluation of palpable and impalpable lesions, and is a quick and inexpensive when compared to conventional histology, especially in settings when only minimal laboratory infrastructures is available 1,2. For example, it is particularly useful for the diagnosis of tuberculosis, as well as the first approach in the investigation of lymphadenopathies in HIV-positive patients3–5, both conditions with high frequencies in developing countries. The great challenge is to train cytopathologists to bring the benefits of the technique, since the accurate diagnosis depends on procedures performed by well-trained professionals2,3. Pathologists can have an important role, not only in reading the smears, but also in performing the FNAC technique, since they can see the patient and perform a physical examination, which is important to improve the integration of clinical and pathological findings. In addition, it is possible to perform quick staining and rapid on site evaluation of the sample to assess its adequacy in real time and repeat the procedure immediately if necessary6.
Anatomic Pathology in Mozambique
Mozambique is located in Sub-Saharan Africa, with a population of approximately 24 million (Census 2009), distributed among 126 districts in 11 provinces. The preliminary results of the population census of 2017 show a growth of population to about 28 million inhabitants in 2017 (http://www.ine.gov.mz/operacoes-estatisticas/censos/censo-2007/censo-2017/divulgacao-os-resultados-preliminares-iv-rgph-2017/view). Life expectancy at birth was 56 years for men and 59 years for women in 2015 (World Health Statistics, 2015 - http://www.who.int/countries/moz/en/). HIV/AIDS prevalence in the country in very high and increased from 11.5% in 2009 to 13% in 20157,8.
In Mozambique until 2016 there were only three Anatomical Pathology services, one in each of the Central Hospitals of the country, namely, Maputo Central Hospital (MCH), Beira Central Hospital (BCH) and Nampula Central Hospital (NCH). These were responsible for diagnostic activities in the South, Center and North of the country, respectively. In 2017, a new pathology service was created in the Quelimane Central Hospital (QCH) in the central region of the country.
Since the beginning of the pathology resident training program in 1992, 13 pathologists have been trained. Of those, only one pathologist has moved outside of the country after the training and one currently is doing a PhD program. The remaining eleven Mozambican pathologists are working in the country in the public sector including performing FNA (7 in MCH, 2 in BCH, 1 in NCH and 1 in QCH). Moreover, there are five foreigner pathologists practicing in the country (two in MCH, one in BCH, one in NCH and one in QCH). These are working under a governmental cooperation agreement established in 1977 whereby each pathologist comes for a 3-year support mission and is replaced thereafter by another colleague.
CASE DESCRIPTION
The Anatomic Pathology Service of MCH
The Anatomical Pathology Service (APS) of MCH is the national reference service, carries out training activities for different levels of trainees, and conducts research activities in collaboration with national and foreign institutions. The resident program started in 1992. There is a 4-year local training program in Anatomical Pathology, which is complemented by a short training period (4 to 10 months) outside the country. In the end of the training program the pathology residents are submitted a national examination involving histopathology, autopsies and cytopathology and if approved they become independent practitioners. Currently, there are 7 residents enrolled in training programs and by our experience we expected all to stay working in the country. The activity of the service is based on clinical autopsies, histopathology and cytology, including exfoliative cytology and FNAC. The latter, was introduced in 1996 by Dr Hideki Yokohama, and in the same year a specific FNAC clinic was created in the service, with the technical support of Prof Fernando Schmitt from Medical Faculty of Porto University and Institute of Pathology and Molecular Immunology of the University of Porto (IPATIMUP), as part of a program supported by the Calouste Gulbenkian Foundation, Portugal.
Initially, clinicians performed the biopsy but the results were frequently non-satisfactory especially because the clinical information provided to the pathologists was not sufficient for a good clinical-pathological correlation. Additionally, the material collected was often insufficient or inadequate. After the FNAC clinic was implemented in the Anatomical Pathology Service, the pathologists were responsible for performing FNAC in all patients.
During the first year of this transition to the pathology service, the number of FNAC analyses was small and carried out twice weekly. Gradually, this method gained popularity and acceptance by the clinicians with a consequent increase in the number of requested FNAC. Currently the APS has a FNAC clinic working on a daily basis and under the responsibility of pathologists. Once per week, the sampling is ultrasound-guided with the support of the radiologists, for intraabdominal tumors, and for some thyroid and breast lesions. A maximum of 15 patients are scheduled per day. The FNAC team includes a pathologist, a resident, and a laboratory technician. The pathologists and the residents under their supervision perform the aspirations.
The standard procedures include the use of a 23-Gauge needle attached to a 10 ml syringe and a syringe pistol for aspiration. A 25-Gauge needle is used for biopsy of deeper masses. The smears were airdried and fixed in methanol and, then stained by May-Grunwald-Giemsa initially and now by Diff-Quick stain. The routine protocol for all lymph node biopsies is to add an additional Ziehl-Neelsen (ZN) stain for detection of acid-fast bacilli (AFB). Other ancillary stains, such as Grocott Methenamine Silver or Periodic Acid Schiff (PAS), are used whenever indicated.
Smears are stained following the end of FNAC clinic by the technician, who delivers them early afternoon to the residents. The residents study the cases and then discuss them later with the scheduled staff pathologists.
In this report, we provide the global numbers of FNAC cases in the period 1996–2010. In addition, we present a summary of the data of all consecutive FNAC performed in APS-MCH during the period of 2009–2010, which were retrospectively collected from the database.
This study was performed in accordance with national regulative law for the handling of biological specimens, the samples being exclusively available for the research purposes in retrospective studies as well as under the international Helsinki declaration.
RESULTS AND DISCUSSION
The MCH Experience in FNAC
Evolution of frequency and general sociodemographic characteristics
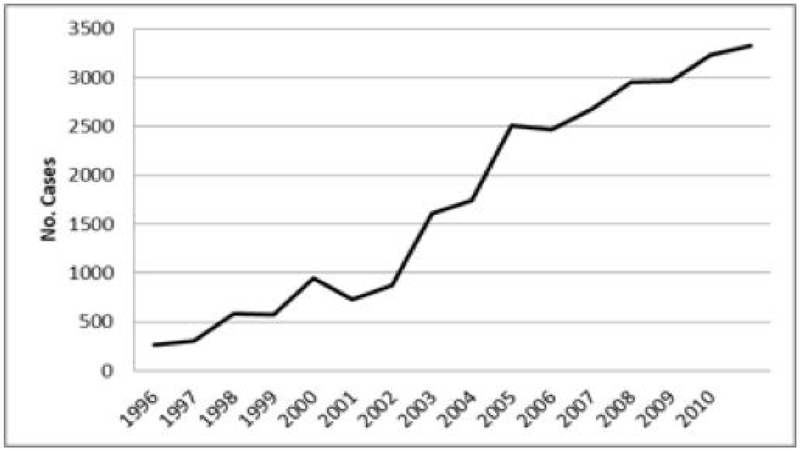
The number of FNAC analyses increased gradually from 269 (4.1% of all tests of the Service) in 1996, when it was introduced in Mozambique, to 3234 (17% of all tests) in 2010, emphasizing the increased importance of this technique in the APS-MCH (Figure 1). With the increasing number of cases, the FNAC clinics were schedule more frequently, and currently are performed daily, by both residents and pathologists.
Figure 1-.
Number of FNAC biopsies each year, since its introduction in the Anatomical Pathologic Service of the Maputo Central Hospital (MCH), 1996–2010.
Until 2016, the APS-MCH was the only public hospital that provided FNAC service in Maputo, and this contributed to the work overload of the few pathologists, who were at same time responsible for all histopathology, autopsy and cytopathology services. This illustrated the urgent need to train other health professionals to perform the technique to offset the burden on pathologists. In 2007 the High Institute of Health Science of Maputo (ISCISA) opened a 4-year course to train technicians of anatomical pathology, with a component of cytotechnology focused on cervical cancer screening program and FNAC practice. The objective of this training is to implement the FNAC techniques in the peripheral hospitals utilizing technicians who have had a period of training and assessment at APS-MCH. Finally, the resident program of APS-MCH includes training in the practical performance and diagnostic interpretation of FNAC from the second year of resident program.
Table 1 shows the socio-demographic characteristics of the patients who underwent FNAC during 2009–2010. Nearly two-thirds of the patients were women and 96.1% were black. Mean age was 32 ± 17.3 years (range: 1 month–92 years) and the most frequent age group was 24–35 years. FNAC of children (0–14 years old) accounted for 13.7% of the exams.
Table 1.
Sociodemographic data of the patients submitted to FNAC, MCH, 2009–2010
| Characteristics | N° | % |
|---|---|---|
| Gender | ||
| Female | 3786 | 64.3 |
| Male | 2094 | 35.6 |
| No Information | 5 | 0.1 |
| Race | ||
| Black | 5656 | 96.1 |
| Mixed | 161 | 2.7 |
| White | 32 | 0.6 |
| Others | 17 | 0.3 |
| No information | 19 | 0.3 |
| Age | ||
| 0–14 | 806 | 13.7 |
| 15–24 | 1134 | 19.3 |
| 25–34 | 1433 | 24.4 |
| 35–44 | 1000 | 16.9 |
| 45–54 | 800 | 13.6 |
| 55–64 | 376 | 6.4 |
| ≥ 65 | 288 | 4.9 |
| No Information | 48 | 0.8 |
FNAC – fine needle aspiration cytology; MCH-Maputo Central Hospital
Source of patients submitted to the FNAC clinic
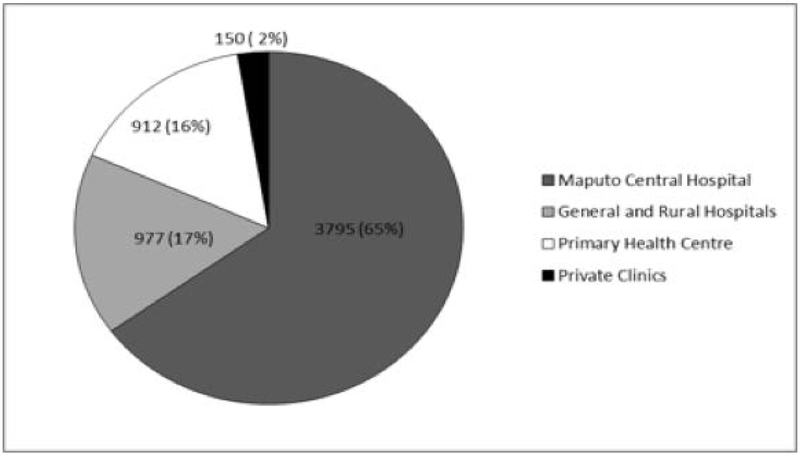
Although most of the patients came from MCH (64.5% of the FNAC analyses), approximately one-third of the biopsies were patients referred from general and rural hospitals or peripheral primary health centers (Figure 2). This demonstrates the importance of FNAC for a more precise diagnosis in patients from the peripheral centers, where surgical biopsy is not accessible9. Decentralization of the FNAC clinic will further increase the collection of samples in the peripheral hospitals and health centers and will provide a more robust basis for the diagnosis of diseases improving the standards of care for many patients who typically are diagnosed based on clinical assessment alone.
Figure 2.
Source of patients submitted to FNAC by health unit, number and percentage, 2009–2010.
Based on these assumptions, the first two units of cytology outside MCH were recently created in two general hospitals at the periphery, namely Mavalane and José Macamo General Hospitals. The collection of FNAC samples is supported by the technicians that were trained in the APS-MCH while pathologists continue performing FNAC two days a week in these units and reporting the slides from all patients.
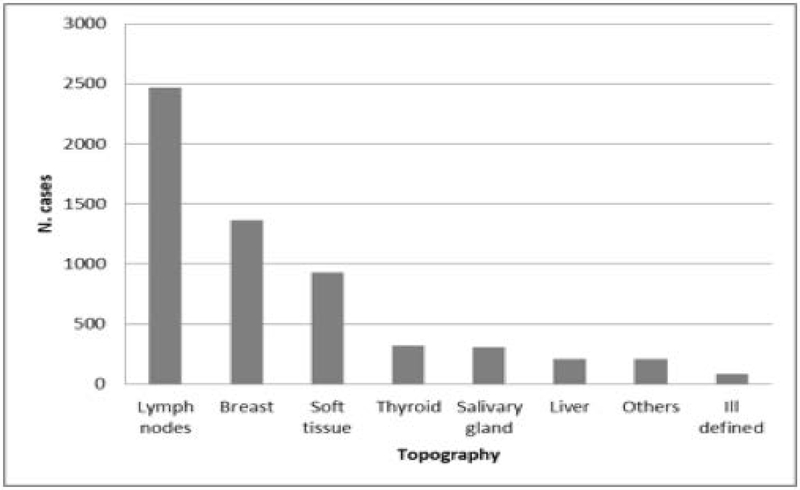
Anatomical sites and diagnosis
The frequency of anatomical sites is shown in Figure 3. Lymph nodes were the organs more frequently bioipsied, followed by breast and soft tissues (Figure 3).
Figure 3.
Distribution of FNAC by anatomical sites, 2009–2010.
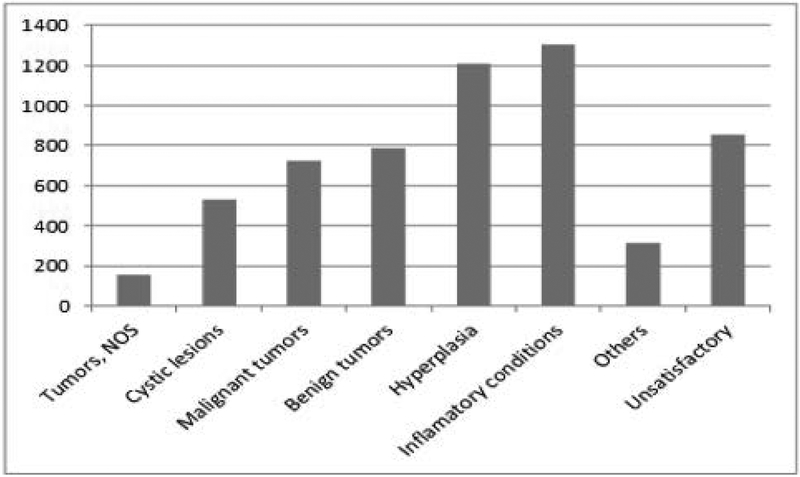
Inflammatory conditions were the most frequent diagnoses (22.2% of the cases), followed by hyperplastic conditions (20.6%), benign tumors (13.4%) and malignant tumors (12.3%) (Figure 4).
Figure 4.
Frequency of diagnose on FNAC, all organs, 2009–2010.
Within the inflammatory conditions, tuberculosis (TB) and granulomatous necrotizing inflammatory process compatible with tuberculosis accounted for 988 cases. In Mozambique, TB is a major cause of morbidity and mortality amongst vulnerable groups (young adults, children and HIV/AIDS patients) with a national estimated TB prevalence of 559/100 000 population. About 50% of the patients with TB in Mozambique are estimated to be HIV positive10. Approximately 10% of the TB reported cases in 2013 were extra pulmonary10. When considering FNAC in lymph nodes, tuberculosis was the most frequent diagnosis (Table 2), consistent with previously described studies in other developing countries3,5,14,15,16.. Lymphoid reactive hyperplasia was the second most frequent diagnosis in our series. In the series of Hirachand et al (2009) lymphoid hyperplasia was the most frequent diagnosis, whereas a malignant neoplasm was the most frequent diagnosis described by Mitra et al (2011) 16,17. Kaposi sarcoma was observed in 3.2%, lymphomas in 4.5% and metastasis in 2.5% of the cases. Although it was not possible to access HIV status in our study, the high frequency of lymph node tuberculosis, lympho-epithelial lesions in salivary glands, Kaposi sarcoma and some lymphomas, probably reflect an association with HIV4,11–13, which is highly prevalent in Mozambique7,8.
Table 2.
Frequency of diagnosis in lymph nodes and breast in FNAC, MCH, 2009–2010
| Diagnosis | Lymph nodes | Breast | ||
|---|---|---|---|---|
| N | % | N | % | |
| Non-specific inflammation | 264 | 10.7 | 53 | 3.9 |
| Tuberculosis/granulomatous and necrotizing inflammatory process consistent with tuberculosis | 825 | 33.5 | 16 | 1.2 |
| Lymphomas | 111 | 4.5 | 8 | 0.6 |
| Reactive Lymphoid hyperplasia | 668 | 27.1 | 0 | 0 |
| Lymphoepitelial lesions | 47 | 2.0 | Na | Na |
| Kaposi’s Sarcoma | 79 | 3.2 | 0 | 0 |
| Metastatic lesions | 52 | 2.1 | 0 | 0 |
| Cysts/fibrocystic changes | Na | Na | 89 | 6.6 |
| Fibradenoma | Na | Na | 372 | 27.4 |
| Epithelial proliferative lesions | Na | Na | 297 | 21.9 |
| Carcinoma | Na | Na | 143 | 10.5 |
| Other malignant tumors, NOS | Na | Na | 2 | 0.1 |
| Others | 104 | 4.2 | 184 | 13.6 |
| Unsatisfactory | 301 | 12.2 | 193 | 14.2 |
| Total | 2463 | 100.0 | 1357 | 100 |
Na – not applicable; NOS – not otherwise specified
In breast, fibroadenomas accounted for 27% of the cases. Epithelial proliferative lesion were the second most frequent diagnosis, observed in 22% of the cases. Diagnosis of breast carcinoma was found in 10.5% of the cases. Breast lesions compatible with tuberculosis were observed in 16 cases. Despite being a relatively uncommon manifestation of TB, breast tuberculosis needs to be suspected in countries with high prevalence of tuberculosis and HIV18.
Many studies have compared the role of FNAC and core needle biopsies (CNB) in the preoperative diagnosis of breast lesions, and the majority of these have been based on practice in developed countries. Although CNB seems to be the preferred method for the preoperative diagnosis of breast cancer19,20, FNAC is also a valuable method, especially when conducted by experienced cytopathologists. The cost of the CNB instrument is around U$2400 dollars in Mozambique and the single use needle is around 19 U$ dollars, and this is a major obstacle for its use in our country. Moreover, CNB leads to additional costs in the laboratory because requires histological processing, as well as increases the time for the diagnosis.
Given the limitations in materials and specialized human resources in our setting, CNB cannot be done, particularly in peripheral areas.
In soft tissues (n=936), the most frequent diagnoses were benign tumors (n=669) including lipomas. Sarcomas were diagnosed in 39 cases, and spindle-cell tumors without other specification in 95 cases. In twelve cases we diagnosed lymphomas and in 15 cases metastatic carcinomas.
FNAC of thyroid accounted for only 5% of all cases (n=314). Colloid/adenomatous goiter was the most frequent diagnosis (n=184), followed by follicular tumors (n=29 cases). There were also 12 carcinomas and 10 cases of thyroiditis. Despite the low number of cases when compared with others FNAC series, the distribution of the results is similar to those described in the literature21.
Lesions from salivary glands were also frequently sampled (n=308 cases, from which 195 were parotid). The most frequent diagnoses in salivary glands were lympho-epithelial lesions (n=112), mainly lympho-epithelial cysts. Michelow et al (2012) described a similar presentation in HIV infected patients in South Africa while in the study by Fakhry et al (2012), in France, benign tumors were the most frequent diagnoses in FNAC of parotid masses11,22. We also found 37 pleomorphic adenomas.
Of the 216 FNAC of liver performed 146 cases were hepatocellular carcinomas (HCC). There are a number of studies of cancer incidence in Maputo from six decades ago showing HCC as the most frequent cancer both in male and female, associated mainly with consumption of aflatoxins and Hepatitis B viral infection23. Data based on registry of APS-MCH showed that liver cancer remains one of the most frequent cancers in Mozambique, both in males and females24, occupying the third position in man (11%) and 5th position in women (4%). Prior to FNAC, most of the diagnoses were made clinically or during autopsy. Biopsies were not routinely performed. The frequency of HCC observed in our study is also high, showing the role of FNAC in the diagnosis of liver tumors25,26.
Abdominal masses accounted for 40 cases. Non-Hodgkin lymphomas were the most frequent diagnoses (n=10), followed by malignant tumors (n=15, of which 7 were metastatic lesions, and 6 were germ cell or blastoma tumors). Twenty-six cases underwent renal FNAC of which 23 were Wilms’ tumor in children.
In Figure 4 we show the most frequently diagnosed lesions by FNAC at MCH.
Unsatisfactory/inconclusive cases
In our study, the proportion of unsatisfactory smears in 2009–2010 was high (14%). This was unexpected, since the FNAC clinic is centred in the APS-HCM, and the biopsies were done by pathologists and residents in most of the cases. The unsatisfactory rate varies widely in the literature, but does not exceed 25%5, and depends on the experience of the personnel who perform the FNAC, the experience of the pathologist reading the smears, the location and nature of the mass to be sampled, and the accessibility of lesion and the assistance of ultrasound2,9,25. In our study, one of the main causes of unsatisfactory report was scant cellularity due to the small size of lesion (often less than 1 cm diameter). In addition, FNAC is often requested in cases without appropriate indications for instance very small lymph nodes; or cases with poor accessibility of the lesion. Another important constraint is the fact that only a small number of sample collections are done with ultrasound guidance, and many do not have previous evaluation by ultrasound because of the shortage of radiologists: there are only 7 in Maputo) MCH is the primary teaching hospital and as such, biopsy procedures performed by residents during their training period in the technique will have an increased number of cases without sufficient cellularity or with artefacts due to a poor smear technique or poor staining. Regular training in the FNA technique and the interpretation of slides for all personnel involved with a quality control system, needs to be done regularly and monitored2,3. At present moment, we were implementing a quality system to prepare our service for certification. One of the goals established is that in the first year of monitoring, the percentage of non-diagnostic specimen should not be higher than 10%. Additional training of the personnel will be implemented when these aims were not reached.
The advent of “one-stop” diagnostic services (with rapid on site evaluation (ROSE) and image-guided procedures, as well as liquid-based cytology6,27 will also improve the diagnostic yield. In a one-stop FNAC clinic, the cellularity of smears can be assessed at the time of the biopsy giving immediate feedback about the quality of the biopsy technique and the smears. ROSE offers improved training and reduction of insufficient rates and was a most important innovation that we introduced in 2012 within our FNAC clinic. It reduced the inadequate rate by offering repeat FNAC during the first visit, and the immediate feedback on sample quality is a way to reinforce good biopsy technique.
In the study of Ammanagi et al (2012) there was 14% of unsatisfactory smears (28/200 cases) at the first biopsy attempt, which was assessed by ROSE, mainly in thyroid, followed by breast and lymph nodes. After repeat FNAC in the same visit, adequate material was found in 24/28 cases6.
CONCLUSION
Our results clearly demonstrate that even in an environment with poor resources, it is possible to establish a FNAC clinic that can provide a quick and precise diagnosis for clinicians to aid in early treatment interventions, especially in inflammatory diseases as is evident in the majority of our cases. Despite the differences in the incidence of the diseases in the various populations and the frequency of organs biopsied, the general results in our study are similar to other series based on the practice of FNAC in European an American countries. After the first successful 15 years of experience in MCH, our goal is to disseminate the technique throughout the country, reinforce the training of technicians, residents and pathologists, and reduce the inadequate biopsy rates through ‘one-stop’ cytology clinics and establishing ROSE and when possible ultrasound-guided aspiration.
Acknowledgments:
The work of CC was supported by the National Institutes of Health (NIH) Fogarty International Center, and the Health Resources and Services Administration under the United States of America President’s Emergency Plan for AIDS Relief (PEPFAR), grant numbers R24TW008908 and R24TW008910. Co-funding was also received from the NIH Office of Research on Women’s Health and the Office of AIDS Research. The authors are grateful to all the members of the Department of Pathology of the MCH and other hospitals for their support to the Service as well as the Gulbenkian Foundation that supports the agreement between IPATIMUP and Universidade Eduardo Mondlane.
Footnotes
Disclosure: The authors declare that they have no disclaimers or conflict of interest to report.
REFERENCES
- 1.Orell S, Sterret GF, Whittaker D. FNAC. 4th Ed Philadelphia: USA:Elsevier; 2005; [Google Scholar]
- 2.Field AS, Geddie W, Zarka M, Sayed S, Kalebi A, Wright CA, Banjo A, Desai M, Kaaya E. Assisting Cytopathology training in medically under-resourced countries: Defining the problems and stablishing solutions. Diagn Cytopathol 2012;40:273–281 [DOI] [PubMed] [Google Scholar]
- 3.Wright CA, Pienaar JP, Marais BJ. Fine needle aspiration biopsy: diagnostic utility in resource-limited settings. Ann Trop Paediatr 2008;28:65–70; [DOI] [PubMed] [Google Scholar]
- 4.Sarma PK, Chowhan AK, Agrawal V, Agarwal V. Fine needle aspiration cytology in HIV-related lymphadenopathy: experience at a single centre in north India. Cytopathology 2010;21:234–239 [DOI] [PubMed] [Google Scholar]
- 5.Fatima S, Arshad S, Ahmed Z, Hasan SH. Spectrum of cytological findings in patients with neck lymphadenopathy – experience in a terciary care hospital in Pakistan. Asian Pac J Cancer Prev 2011;12:1873–1875 [PubMed] [Google Scholar]
- 6.Ammanagi AS, Dombale VD, Patil SS. On-site toluidine blue staining and screening improves efficiency of fine-needle aspiration cytology reporting. Acta Cytol 2012;56:347–351 [DOI] [PubMed] [Google Scholar]
- 7.INSIDA 2009, Relatório final Inquérito nacional de prevalência, riscos Comportamentais e Informação sobre o HIV e SIDA em Moçambique [Internet]. Moçambique: Ministério da Saúde, Instituto Nacional de Saúde Maputo, Moçambique; Instituto Nacional de Estatística Maputo, Moçambique; ICF Macro Calverton, MD, EUA; 2010. p. 310 Available from: https://dhsprogram.com/pubs/pdf/AIS8/AIS8.pdf [Google Scholar]
- 8.IMASIDA 2017, [Inquérito de Indicadores de Imunização, Malária e HIV/SIDA em Moçambique – IMASIDA 2015]. Moçambique: Ministério da Saúde (MISAU), Instituto Nacional de Estatística (INE), ICF Internacional; Rockville, Maryland, EUA: INS, INE e ICF International; 2017. [Google Scholar]
- 9.Erra S, Costamagna D. Fine-needle aspiration cytology for breast lesions and cytopathologic correlations. An Italian peripheral hospital experience with 440 cases (from 2000 to 2007). G Chir 2010;31:404–408 [PubMed] [Google Scholar]
- 10.World Health Organization. Global tuberculosis report 2014. Geneva: World Health Organization; 2014 [Google Scholar]
- 11.Michelow P, Dezube BJ, Pantanowitz L. Fine neelde aspiration of salivary gland masses in HIV-infected patients. Diagn Cytopathol 2012;40:684–690 [DOI] [PubMed] [Google Scholar]
- 12.Gamborino E, Carrilho C, Ferro J, Khan MS, Garcia C, Suarez MC, Yokoyama H, Schmitt FC. Fine-needle aspiration diagnosis of Kaposi’s sarcoma in a developing country. Diagn Cytopathol. 2000;23:322–325 [DOI] [PubMed] [Google Scholar]
- 13.Viegas SO, Ghebremichael S, Massawo L, Alberto M, Fernandes FC, Monteiro E, Couvin D, Matavele JM, Rastogi N, Correia-Neves M, Machado A, Carrilho C, Groenheit R, Källenius G, Koivula T. Mycobacterium tuberculosis causing tuberculous lymphadenitis in Maputo, Mozambique. BMC Microbiol. 2015. November 21;15:268. doi: 10.1186/s12866-015-0603-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mittal P, Handa U, Mohan H, Gupta V. Comparative evaluation of fine needle aspiration cytology, culture, and PCR in diagnosis of Tuberculous lymphadenitis. Diagn Cytopathol 2011;39:822–826 [DOI] [PubMed] [Google Scholar]
- 15.Majeed MM, Bukhari MM. Evaluation for granulomatous inflammation on fine needle aspiration cytology using special stains. Pathology Research International 2011, Article ID 851524, 8 pages [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirachand S, Lakhey M, Akhter J, Thapa B. Evaluation of fine needle aspiration cytology of lymph nodes in Kathmandu Medial College, Teaching hospital. Kathmandu Univ Med J (KUMJ) 2009;7:139–142 [DOI] [PubMed] [Google Scholar]
- 17.Mitra S, Ray S, Mitra PK. Fine needle aspiration cytology of supraclavicular lymph nodes: our experience over three-year period. J Cytol 2011;28:108–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Metha G, Mittal A, Verma S. Breast tuberculosis – clinical spectrum and management. Indian J Surg 2010;72:433–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hukkinen K, Kivisaari L, Heikkila PS, Von Smitten K, Leidenius M. Unsuccessful preoperative biopsies, fine needle aspiration cytology or core needle biopsy, lead to increased costs in the diagnostic workup in breast cancer. Acta Oncol 2008;47:1037–1045 [DOI] [PubMed] [Google Scholar]
- 20.Brancato B, Crocetti E, Bianchi S, Catarzi S, Risso GG, Bulgaresi P, Piscioli F, Scialpi M, Ciatto S, Houssami N. Accuracy of needle biopsy of breast lesions visible on ultrasound: audit of fine needle versus core needle biopsy in 3233 consecutive samplings with ascertained outcomes. Breast. 2012. 21:449–454. [DOI] [PubMed] [Google Scholar]
- 21.Paajanen I, Metso S, Jaatinen P, Kholová I. Thyroid FNA diagnostics in a real-life setting: Experiences of the implementation of the Bethesda system in Finland. Cytopathology. 2017. December 18. doi: 10.1111/cyt.12513 [DOI] [PubMed] [Google Scholar]
- 22.Fakhry N, Antonini F, Michel J, Penicaud M, Mancini J, Lagier A, Santini L, Turner F, Chrestian MA, Zanaret M, Dessi P, Giovanni A. Fine-needle aspiration cytology in the management of parotid masses: evaluation of 249 patients. Eur Ann Otorhinolaryngol Head Neck Dis 2012;129:131–135 [DOI] [PubMed] [Google Scholar]
- 23.Prates MD, Torres FO. A cancer survey in Lourenço Marques, Portuguese East Africa. J Natl Cancer Inst. 1965;35:729–757 [PubMed] [Google Scholar]
- 24.Lorenzoni C, Vilajeliu A, Carrilho C, Ismail MR, Castillo P, Augusto O, García-Basteiro AL, Sidat M, de Sanjosé S, Menéndez C, Ordi J. Trends in cancer incidence in Maputo, Mozambique, 1991–2008.PLoS One. 2015. June 25;10(6):e0130469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Swamy MCM, Arathi CA, Kodandaswamy CR. Value of ultrasonography-guided fine needle aspiration cytology in the investigative sequence of hepatic lesions with an emphasis on hepatocellular carcinoma. J Cytol 2011;28:178–184 Mallikarjuna et al, 2011; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mrzlijak A, Kardum-Skelin I, Cvrlje VC, Filipec-Kanizaj T, Sustercic D, Skegro D. Role of fine needle aspiration cytology in management of hepatocellular carcinoma: a single centre experience. Coll Antropol 2010;34:381–385 [PubMed] [Google Scholar]
- 27.Gerhard R, Schmitt FC: Liquid-based cytology in FNAB of breast lesions. Acta Cytol 2014;58:533–542. [DOI] [PubMed] [Google Scholar]