Abstract
Background
Arm levitation is an involuntary elevation of the upper limb, a manifestation of the alien-limb phenomenon. It has rarely been reported in Creutzfeldt–Jakob disease (CJD), less so as an initial manifestation
Case Report
We report a 56-year-old right-handed man with rapidly progressive gait ataxia and involuntary elevation of the left upper limb. During the next few weeks, the patient developed cognitive impairment, apraxia, visual hallucinations, and myoclonus. He met diagnostic criteria for CJD. We evaluated additional published cases of early-appearance of alien-limb phenomenon in the context of CJD; there were 22 such cases and alien-limb phenomenon was the first and exclusive manifestation in only five of them.
Discussion
Arm levitation may be a distinct presentation of CJD, appearing earlier than other clinical features.
Keywords: Arm levitation, alien-limb phenomenon, acute ataxia, Creutzfeldt–Jakob disease, movement disorders
Introduction
Creutzfeldt–Jakob disease (CJD) is an unusual neurodegenerative disease caused by accumulation of abnormally folded proteins (prions) with diffuse pathologic deposition, but a proclivity for the involvement of the striatum, thalamus, and cortical regions. The classic phenotype is characterized by rapidly progressive dementia associated with ataxia, myoclonus, and other movement disorders.1–3
Arm levitation is an involuntary elevation of the upper limb and is regarded as one of the manifestations of the alien-limb phenomenon (ALP), previously reported in CJD.4 Also, an acute or subacute presentation of ataxia in adults may rarely be the initial neurological presentation of CJD.5
In this article, we report a patient with sporadic CJD who presented with subacute ataxia and followed by arm levitation as initial manifestations. Moreover, we perform a comprehensive review of the literature about the phenomenology, classification, and associated neurological features of arm levitation in the context CJD patients.
Case report
Two months prior to presentation a 56-year-old right-handed male was evaluated in the emergency department for acute gait instability with ataxia suspected to represent a stroke. Brain magnetic resonance imaging (MRI) was normal. At the outpatient assessment, besides ataxia, he also exhibited levitation of the left arm (Video 1). Family history was unremarkable. Further questioning revealed he had exhibited progressive impairment of ataxia and cognition over the first month. On follow-up neurological examination, the patient was inattentive and disoriented to space and time. Cranial nerve examination was normal, except for spontaneous multidirectional nystagmus. There was moderate global ataxia. Over the following weeks, his gait progressively deteriorated. A repeat brain MRI was normal. Rheumatologic tests, autoimmune workup (celiac disease, thyroiditis, glutamic acid decarboxylase autoantibody), syphilis screen, and paraneoplastic antibodies panel were normal.
Video 1. Arm Levitation as Initial Neurological Manifestation of Creutzfeldt–Jakob Disease. The video shows gait ataxia with an involuntary elevation of the left arm (arm levitation). The patient had only mild cognitive impairment in this evaluation.
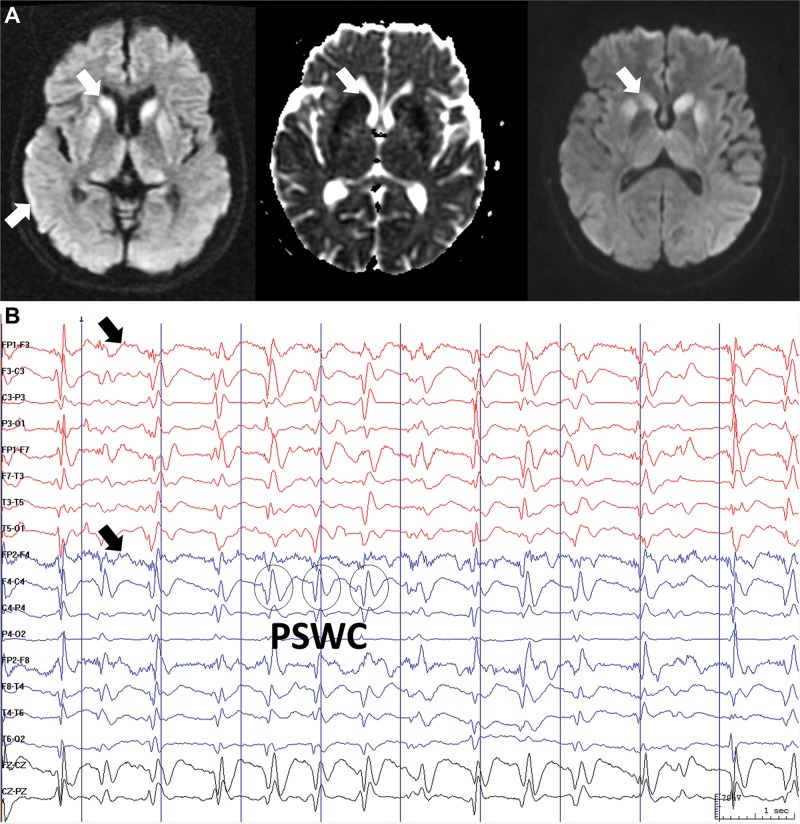
Over a 2-month period, ideomotor apraxia, visual hallucinations, dysphagia, rigidity, pyramidal features, and myoclonus with auditory stimuli exacerbation (startle myoclonus) appeared. A follow-up brain MRI showed diffusion restriction, predominantly in the right parietal cortex (cortical ribbon sign) and, caudate and putamen (Figure 1A). An electroencephalogram revealed diffuse delta activity, evolving to lateralized (right side) and diffuse periodic sharp wave complexes (Figure 1B). Cerebrospinal fluid (CSF) was normal, except for positive 14-3-3 protein. He met diagnostic criteria for CJD and died four weeks later. No autopsy was performed.
Figure 1. Brain Magnetic Resonance Images (MRI) and Electroencephalographic Recording (A) Axial diffusion-weighted brain MRI (left) shows hyperintense signal in the cortex, predominantly parietal, and bilateral striatum, which indicates restriction diffusion with low signal on the apparent diffusion coefficient (ADC) map (middle). Axial fluid-attenuated inversion recovery brain MRI (right) reveals gradual anteroposterior hyperintensity gradient on striatum, sparing posterior putamen. (B) Electroencephalographic recordings show disorganization of cerebral activity due to diffuse delta activity, evolving to lateralized and diffuse periodic sharp-wave complexes (PSWC).
Discussion
CJD can manifest with a range of movement disorders, including myoclonus, dystonia, tremor, parkinsonism, chorea, athetosis, and ballismus. The frequency of movement disorders in CJD depends on the distribution of the pathologically affected areas and increase significantly during disease progression.3 Early manifestations may be subtle or subclinical. A rapidly progressive ataxia should trigger an investigation for vascular, autoimmune, and infectious disorders.1,5 Subacute ataxia may only rarely represent the initial neurological presentation of CJD2.
Arm levitation is a rare neurological sign, mainly described in patients with vasculopathies (infarctions, hemorrhages), tumors, seizures, corticobasal syndrome, and progressive supranuclear palsy.2,3,6–8 MacGowan et al.4 were the first known to report ALP in CJD patients. They described two cases of neuropathologically established CJD who presented with ALP complaints in the absence of dementia.
ALP in CJD is of the posterior or sensory type (aimless movements, arm levitation), with high localizing value to the contralateral parietal lobe, unlike the frontal type (grasping reflex, manual groping, utilization behaviors, and perseveration) or the callosal type (intermanual conflict and manual interference with purposeful movements; a “disconnection syndrome”).7,9–12 Associated neurological features may include hemianesthesia, homonymous hemianopsia neglect, moderate-to-severe ataxia, visuomotor dissociation and/or visuospatial deficit.8,13 Patients typically deny ownership of the movements and engage personification of the limb.8 In CJD, the posterior ALP phenotype should be considered a sign of cortical dysfunction in the non-dominant parietal cortex.2,8 The mechanism of alien-limb generation may be dependent on the disruption in the integration of multimodal sensory processing signals to motor programming areas.2,6–8
We evaluated additional published cases of the early appearance of ALP in the context of CJD and their clinical features since the first description in 1997 by MacGowan et al.4 We summarize these 22 cases in Table 1. ALP was the first and exclusive manifestation in only five of them (22%). Most CJD patients exhibited a left ALP due to non-dominant parietal cortical involvement (72%). The most frequent associated deficits were sensory abnormalities and gait impairment, and the most common movement disorders were myoclonus and ataxia. No dementia was documented concomitantly ALP during the initial course of the disease (only two cases reported memory or cognitive impairment as concomitant manifestation), which may have contributed to a delay in ascertaining the diagnosis of CJD. Posterior and callosal phenotypes were similarly reported, and sometimes a mixed posterior-callosal phenotype was present, but no cases of an exclusively frontal ALP pattern were found.2,8
Table 1. Characteristics of Patients with Alien-limb Phenomenon as among the Initial Manifestations in Creutzfeldt–Jakob Disease.
| Case, Reference | Age, Handedness, Sex | ALP Side, Type† | Associated Deficits at Onset | Latency from ALP to diagnosis | MRI |
|---|---|---|---|---|---|
| 1, Rubin et al.2 | 73, R, man | L, NR | Disorientation, visual hallucinations | NR | Cortical T2 hyperintensity (DWI not done) |
| 2, Rubin et al.2 | 56, R, man | L, NR | Memory impairment, aphasia, tremor, sleep disturbance | NR | Normal |
| 3, Rubin et al.2 | 58, R, woman | R, NR | None | NR | Restricted diffusion in B striatum, and left cortex |
| 4, Rubin et al.2 | 69, R, man | L, NR | None | NR | Normal |
| 5, Rubin et al.2 | 71, R, woman | L, NR | Cognitive impairment, blurred vision | NR | No MRI |
| 6, Rubin et al.2 | 69, R, man | L, NR | Facial paresthesia, blurred vision | NR | No MRI |
| 7, Rubin et al.2 | 73, unknown, man | R, NR | Unknown | NR | Normal |
| 8, Rubin et al.2 | 56, unknown, woman | R, NR | Myoclonus, ataxia | NR | Restricted diffusion in B striatum and cortex |
| 9, Rubin et al.2 | 61, R, man | R, NR | Right arm jerking | NR | L > R parietal restricted diffusion |
| 10, Rubin et al.2 | 39, R, woman | R, NR | None | NR | Restricted diffusion in B striatum, L parietal cortex |
| 11, Rubin et al.2 | 56, R, man | L, NR | None | NR | B restricted diffusion, T2 hyperintensity of R posterior hemispheric cortex |
| 12, Rubin et al.2 | 71, L, woman | R, posterior and callosal | Gait instability | NR | Restricted diffusion, T2 hyperintensity of bilateral R > L parietal, occipital lobes |
| 13, Rubin et al.2 | 72, R, woman | L, NR | Myoclonus, behavioral changes | NR | Diffuse cortical restricted diffusion |
| 14, MacGowan et al.4 | 78, R, woman | L, callosal | L hemiparesis, sensory ataxia, and myoclonus | NR | Normal |
| 15, MacGowan et al.4 | 74, R, woman | L, callosal | Progressive weakness | 6 weeks | Mild cerebral atrophy |
| 16, Fogel et al.9 | 55, R, woman | L, callosal | Gait instability, falls, and limb ataxia | 1 month | Bilateral L > R restricted diffusion, T2 hyperintensity of B parietal cortex |
| 17, Inzelberg et al.12 | 70, R, man | L, posterior | Unsteady gait, frequent falls, and visual hallucinations | At least 6 weeks | Mild cerebral atrophy |
| 18, Oberndorfer et al.14* | 74, R, woman | L, posterior | L hand ataxia | 3 months | Non-diagnostic clues |
| 19, Anschel et al.15 | 65, R, man | L, callosal | None | 8 months | Restricted diffusion in R putamen, and bilateral R > L cortex |
| 20, Moreaud et al.16 | 70, unknown, woman | L, callosal | Upper limbs clumsiness | 6 months | B frontal and parietal atrophy, and cortical ribbon sign |
| 21, Kleiner-Fisman et al.17 | 73, R, man | L, posterior | L hand ataxia and clumsiness, L hemineglect, and unsteady gait | 4 weeks | Restricted diffusion in R caudate nucleus, and bilateral R > L cortex |
| 22, Avanzino et al.18 | 59, R, woman | L, posterior | L hand numbness | 2 weeks | Normal |
| 23, our case | 56, R, man | L, posterior | Gait instability and ataxia | 2 months | Right parietal cortex ribbon sign, Restricted diffusion in B striatum and R parietal cortex |
Abbreviations: ALP, Alien-limb Phenomenon; B, bilateral; CT, Computed Tomography; DWI, Diffusion-weighted Imaging; L, left; MRI, Magnetic Resonance Imaging; NR, Not Reported; R, right.
Familial CJD with neuropathology confirmation.
NR: Phenotypic description unavailable rendering ALP phenotype unclear.
In most arm levitation cases, gait instability or ataxia was present. The MRI findings almost invariably showed asymmetrical diffusion restriction in the striatum and parietal cortex. Of note, ALP has also been reported in pathology-confirmed familial CJD.13 The onset of arm levitation may precede the diagnosis of CJD by up to 16 weeks.2,7 Some patients have been phenotypically characterized as corticobasal syndrome, assumed to represent underlying corticobasal degeneration pathology, which is more frequent compared with CJD.2 However, the subacute presentation of arm levitation should raise suspicion for prion disease, particularly when associated with rapid onset dementia or ataxia,2,3,9 as in our case.
In conclusion, CJD must be considered in anyone presenting with arm levitation, classified as a posterior ALP, with or without associated acute or subacute ataxia.2,7,9,12
Acknowledgments
The authors are grateful to the patient and his family for trusting their care to us and for providing informed consent for this publication.
Footnotes
Funding: None.
Financial Disclosures: Dr. Espay has received grant support from the NIH, Great Lakes Neurotechnologies and the Michael J Fox Foundation; personal compensation as a consultant/scientific advisory board member for Abbvie, TEVA, Impax, Acadia, Acorda, Cynapsus/Sunovion, Lundbeck, and USWorldMeds; publishing royalties from Lippincott Williams & Wilkins, Cambridge University Press, and Springer; and honoraria from Abbvie, UCB, USWorldMeds, Lundbeck, Acadia, the American Academy of Neurology, and the Movement Disorders Society.
Conflicts of Interest: The authors report no conflict of interest.
Ethics Statement: All patients that appear on video have provided written informed consent; authorization for the videotaping and for publication of the videotape was provided.
References
- 1.Kim MO, Geschwind MD. Clinical update of Jakob-Creutzfeldt disease. Curr Opin Neurol. 2015;28:302–310. doi: 10.1097/WCO.0000000000000197. [DOI] [PubMed] [Google Scholar]
- 2.Rubin MN, Graff-Radford J, Boeve BF, Josephs KA, Aksamit AJ. The alien limb phenomenon and Creutzfeldt-Jakob disease. Parkinsonism Relat Disord. 2012;18:842–846. doi: 10.1016/j.parkreldis.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Maltête D, Guyant-Maréchal L, Mihout B, Hannequin D. Movement disorders and Creutzfeldt-Jakob disease: a review. Parkinsonism Relat Disord. 2006;12:65–71. doi: 10.1016/j.parkreldis.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 4.MacGowan DJL, Delanty N, Petito F, Edgar M, Mastrianni J, DeArmond SJ. Isolated myoclonic alien hand as the sole presentation of pathologically established Creutzfeldt-Jakob disease: a report of two patients. J Neurol Neurosurg Psychiatry. 1997;63:404–407. doi: 10.1136/jnnp.63.3.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mantokoudis G, Saber Tehrani AS, Newman-Toker DE. An unusual stroke-like clinical presentation of Creutzfeldt-Jakob disease: acute vestibular syndrome. Neurologist. 2015;19:96–98. doi: 10.1097/NRL.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 6.Carrilho PEM, Caramelli P, Cardoso F, Barbosa ER, Buchpiguel CA, Nitrini R. Involuntary hand levitation associated with parietal damage: another alien hand syndrome. Arq Neuro-Psiquiatr. 2001;59:521–525. doi: 10.1590/S0004-282X2001000400007. [DOI] [PubMed] [Google Scholar]
- 7.Graff-Radford J, Rubin MN, Jones DT, Aksamit AJ, Ahlskog JE, Knopman DS, et al. The alien limb phenomenon. J Neurol. 2013;260:1880–1888. doi: 10.1007/s00415-013-6898-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scepkowski LA, Cronin-Golomb A. The alien hand: cases, categorizations, and anatomical correlates. Behav Cogn Neurosci Rev. 2003;2:261–277. doi: 10.1177/1534582303260119. [DOI] [PubMed] [Google Scholar]
- 9.Fogel B, Wu M, Kremen S, Murthy K, Jackson G, Vanek Z. Creutzfeldt–Jakob disease presenting with alien limb sign. Move Disord. 2006;21:1040–1042. doi: 10.1002/mds.20858. [DOI] [PubMed] [Google Scholar]
- 10.Aboitiz F, Carrasco X, Schröter C, Zaidel D, Zaidel E, Lavados M. The alien hand syndrome: classification of forms reported and discussion of a new condition. Neurol Sci. 2003;24:252–257. doi: 10.1007/s10072-003-0149-4. [DOI] [PubMed] [Google Scholar]
- 11.Pappalardo A, Ciancio MR, Reggio E, Patti F. Posterior alien hand syndrome: case report and rehabilitative treatment. Neurorehabil Neural Repair. 2004;18:176–181. doi: 10.1177/0888439004269031. [DOI] [PubMed] [Google Scholar]
- 12.Inzelberg R, Nisipeanu P, Blumen SC, Carasso RL. Alien hand sign in Creutzfeldt- Jakob disease. J Neurol Neurosurg Psychiatry. 2000;68:103–104. doi: 10.1136/jnnp.68.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Josephs KAR, Rossor MN. Neurological sign: the alien limb. Pract Neurol. 2004;4:44–45. doi: 10.1111/j.1474-7766.2004.06-189.x. [DOI] [Google Scholar]
- 14.Oberndorfer S, Urbanits S, Lahrmann H, Jarius C, Albrecht G, Grisold W. Familial Creutzfeldt-Jakob disease initially presenting with alien hand syndrome. J Neurol. 2002;249:631–632. doi: 10.1007/s004150200077. [DOI] [PubMed] [Google Scholar]
- 15.Anschel DJ, Simon DK, Llinas R, Joseph JT. Spongiform encephalopathy mimicking corticobasal degeneration. Mov Disord. 2002;17:606–607. doi: 10.1002/mds.10166. [DOI] [PubMed] [Google Scholar]
- 16.Moreaud O, Monavon A, Brutti-Mairesse MP. Creutzfeldt-Jakob disease mimicking corticobasal degeneration: clinical and MRI data of a case. J Neurol. 2005;252:1283–1284. doi: 10.1007/s00415-005-0828-6. [DOI] [PubMed] [Google Scholar]
- 17.Kleiner-Fisman G, Bergeron C, Lang AE. Presentation of Creutzfeldt–Jakob disease as acute corticobasal degeneration syndrome. Mov Disord. 2004;19:948–949. doi: 10.1002/mds.20140. [DOI] [PubMed] [Google Scholar]
- 18.Avanzino L, Marinelli L, Buccolieri A, Trompetto C, Abbruzzese G. Creutzfeldt-Jakob disease presenting as corticobasal degeneration: a neurophysiological study. Neurol Sci. 2006;27:118–121. doi: 10.1007/s10072-006-0611-1. [DOI] [PubMed] [Google Scholar]