Abstract
Introduction:
Exclusive breastfeeding is the optimal mode of feeding for the first six months of a child’s life. Modifiable factors associated with increased breastfeeding, may be addressed through antenatal breastfeeding education. In Greece, the rates of exclusive breastfeeding remain rather low.
Aim:
The aim of the current study was to evaluate the effectiveness of a structured in-hospital midwife-led antenatal breastfeeding educational programme on breastfeeding knowledge and self-efficacy, attitudes towards breastfeeding and perceived-barriers of breastfeeding.
Patients and Methods:
This was a quasi-experimental study with two study groups: an intervention group (following a four-hour midwife-led antenatal breastfeeding programme) and a control group. All nulliparous women attending antenatal care at the tertiary hospital in Athens, Greece during May 2016–January 2017 were invited to participate, of which 203 nulliparous pregnant women took part. Demographic data forms, the Breastfeeding Self-efficacy Scale, the Iowa Infant Feeding Attitude Scale, the Breast Feeding Knowledge Questionnaire and the Perceived Breast Feeding Barriers Questionnaire were used for data collection.
Results:
Post-intervention, women in the intervention group had a more positive attitude towards breastfeeding (73.5% versus 66.1%, p<0.001), greater knowledge (14.6% versus 13.1%, p<0.001) and more breastfeeding self-efficacy (51.4% versus 45.6%, p<0.001) compared to the control group. Furthermore, they had significantly less perceived barriers regarding breastfeeding (27.4% versus 31.0%, p<0.001).
Conclusion:
The four-hour antenatal breastfeeding education intervention which occurred and was evaluated for the first time in the Greek female population was effective in increasing breastfeeding knowledge, self-efficacy and a positive attitude towards breastfeeding. The intervention was furthermore effective in lowering perceived breastfeeding barriers. This midwife-led antenatal breastfeeding education programme could be suitable for integration to routine antenatal care in health care services in Greece.
Keywords: Breast feeding, education, antenatal, attitudes, self efficacy
1. INTRODUCTION
The maternal and neonatal benefits of breastfeeding are extensively recorded (1-3) and exclusive breastfeeding for the first six months of a child’s life is recommended as the single largest potential intervention to prevent child mortality (4). To this end, the World Health Assembly (5) has set a global nutrition target, that in 2025 at least 50% of infants should be exclusively breastfeeding at six months of age. Although benefits are well known, developed countries keep on witnessing low breastfeeding rates (6). Globally only 38% of infants are exclusively breastfed at six months of age (7, 8).
In Greece, the initiation rates of breastfeeding are high (85-94%) (9, 10), but breastfeeding rates decrease rapidly over the next months; to 55% after the first month (11) and to 12-22% at the end of the sixth month (10, 11). Exclusive breastfeeding rates at six months of age range from 0,3-23,4% (10, 11-13). However, these data lack of standardization of definitions and methods used to monitor breastfeeding rates and duration making it difficult to compare these rates among other countries. Thus, according to a national data about breastfeeding, women in Greece seem to breastfeed exclusively at six months at only 0.7% (14). These rates are notably lower compared to national data of other countries, such as Denmark (17.2%), Spain (28.5%), Portugal (34.0%), Hungary (43.9%) or Slovakia (49.3%) (15).
The World Health Organization (WHO) has identified several leading factors that may contribute to low rates of exclusive breastfeeding; including societal beliefs favoring mixed feeding, hospital practices that are not supportive of breastfeeding and lack of knowledge among women and their partners (5). Furthermore, factors related to continued breastfeeding can be categorized into a) socio-demographic factors; b) biomedical factors and c) psycho-social factors such as breastfeeding attitude and self-efficacy. The psycho-social factors are especially important to clinical practice, as they may be modified.
Maternal breastfeeding self-efficacy is a significant psychometric factor that influences positively the breastfeeding rates (17, 18) and identifies high-risk mothers for discontinuing breastfeeding prematurely among varying maternal populations. Breastfeeding self-efficacy is associated with a mother’s perceived ability to breastfeed her baby, and is an important variable in breastfeeding duration as it expresses in advance a) the probable choice of the mother to breastfeed, b) the level of effort she is going to put, c) the negative or positive pattern of thoughts she is going to have, d) her emotional status while dealing with breastfeeding problems (19).
Although breastfeeding is a natural, physiologic process, it is also a learned behavior (20). Maternal knowledge about breastfeeding and breastfeeding attitudes are associated with longer duration of breastfeeding (21, 22) and intent (11, 23). Mothers who are positively predisposed to breastfeeding seem to maintain breastfeeding longer, regardless of whether they are exclusively breastfeeding (24). Also, mothers who find that it is more practical, healthy and less expensive to breastfeed, choose formula less often compared to mothers that regard breastfeeding to be troublesome and embarrassing (24). The predominance of formula feeding may be due in part to a lack of knowledge about the benefits of breastfeeding and the need for providing women with more information about the benefits of breast feeding has been identified (25). These modifiable factors associated with increased breastfeeding, i.e. knowledge and self-efficacy may be addressed through antenatal breastfeeding education (26).
However, the impact of an antenatal breastfeeding educational programme on these modifiable factors of breastfeeding knowledge, attitudes, self-efficacy and perceived barriers has not been evaluated in Greece, a country with exceptionally low exclusive breastfeeding rates at six months of age.
2. AIM
This paper describes and reports on an antenatal intervention to increase breastfeeding knowledge, self-efficacy and a positive attitude towards breastfeeding as well as lower perceived breastfeeding barriers.
3. PATIENTS AND METHODS
Our study applied a quasi-experimental and pre-to-post test-research design and was conducted in the largest maternity public hospital in Greece. This hospital provides a midwife-led antenatal education programme, which consists of five educational sessions about pregnancy, labour and the postpartum period. One of these five sessions is a 4-hour breastfeeding education class.
Participants were nulliparous pregnant women who were enrolled in the antenatal education classes and attended the breastfeeding session (intervention group) and pregnant women that did not attend any classes (control group). Both groups received routine maternity care at the outpatient maternity clinic. Nulliparous pregnant women, were included in the sample if they: a) were able to understand the Greek language so that they could fill in the questionnaires, b) were above 18 years old and c) were more than 32 weeks pregnant.
Women who were scheduled to attend the breastfeeding education classes between May 2016 and January 2017 were invited to participate in the study. During the recruitment period there were 12 breastfeeding classes scheduled and the final sample in the intervention group was 103 women (100% response rate among eligible women). Women in the control group, who were invited to participate in the study during their visit at the maternity outpatient department for routine care between May 2016 and October 2016, did not attend any breastfeeding classes before or during the study period. During the recruitment period, 140 eligible women were invited to participate and 40 refused, claiming lack of time due to their scheduled appointment. The final sample for the control group was 100 women (72% response rate among eligible women).
Women in the intervention group received and filled in the first questionnaire package just before attending the breastfeeding session and the second package one week later just before attending the next educational session. Women in the control group received and filled in the first questionnaire package whilst waiting for their routine antenatal check-up at the clinic and the second package one week later via a web-based survey platform. The surveys were self-administered, providing a more practical and relatively low-cost evaluation (27) and time was taken by the researcher to explain the surveys for participants. The women’s partners were not present when completing the forms at the hospital (both groups).
The intervention: A four-hour breastfeeding educational session
The four-hour breastfeeding educational session was led by a midwife and offered as an option to women receiving antenatal care at the tertiary hospital. It was not part of routine antenatal care but the class was free of charge. The breastfeeding session was adjusted to the WHO 10 Steps (28) and Baby Friendly Hospital Initiative fundamentals (29). The session emphasized obtaining competencies for latch and positioning, in addition to facing usual fears, worries, problems, and myths (30). Furthermore, to focus on the advantages of breastfeeding to mother, baby, and society and to meet specific needs in the early days of breastfeeding by proposing also resources for support. This session was supported by the hospital, which was in the process of becoming certified as Baby- Friendly (31). Participants received information on basic anatomy and physiology of milk production, the benefits of exclusive breastfeeding for the baby and mother, the importance of skin-to-skin contact the first hour and beyond, establishing breastfeeding and understanding milk supply, positioning and attachment, role of partners in breastfeeding, wrong thoughts and myths, common concerns and problem solving. All women were encouraged to outline their personal concerns and discuss them with the midwife and the other group members, thus building a support network. In order to accomplish the teaching goals, presentations, videos, group discussions, dolls and breast models were used.
3.1. Measures
Breastfeeding Self-Efficacy Scale
The Breastfeeding Self-Efficacy Scale-Short Form (BSES-SF) is an easy to use 14 item self-report instrument on a five-point Likert scale (32). The reliability estimates of the BSES-SF, including Cronbach’s alpha coefficient, inter-item correlations, and corrected item-total correlations, presented high internal consistency (32). The BSES-SF is an excellent measure of breastfeeding self-efficacy and is considered a unique tool to identify mothers likely to discontinue breastfeeding prematurely (33) and a measure to evaluate breastfeeding interventions and inform clinical practice (32). A scale format was chosen that presented all items positively (34). All scores are summed and higher scores indicate higher levels of breastfeeding self-efficacy (32). This version was easier to use in clinical context (32). The scale has been used not only during the postpartum period, but also during pregnancy, showing its predictive validity (35, 36).
Iowa Infant Feeding Attitude Scale
The Iowa Infant Feeding Attitude Scale (IIFAS) provides a reliable and valid assessment of attitudes toward different modes of infant feeding with Cronbach’s a 0.86. It is also predictive of breastfeeding intention and initiation in pregnant and postpartum women and breastfeeding duration among mothers who breastfeed (37). This tool could be used to stratify mothers in reference to their probability of breastfeeding, to evaluate changes in attitudes over time and the effectiveness of promoting interventions in altering attitudes to infant feeding (38). The IIFAS contains 17 items scored on a 5-point Likert-type scale and it is easy to use. Total attitude scores range from 17 to 85 with higher scores reflecting attitudes more positive to breastfeeding (37). IIFAS has been used widely in original and adapted formats as well (39).
Breastfeeding Knowledge Questionnaire
The Breastfeeding Knowledge Questionnaire, based on the WHO and UNICEF breastfeeding recommendations, was developed by Hala et al (40). The questionnaire consists of 15 items regarding the maternal and neonatal benefits of breastfeeding. The total score is calculated by summing the individual score of the 15 questions. The score ranges from 1-15, with the higher score reflecting a higher level of knowledge.
The Perceived Breast Feeding Barriers Questionnaire
The Perceived Breast Feeding Barriers Questionnaire was developed by Hala et al (40) and consists of 18 items. The total score is calculated by summing the individual scores of the 18 questions, with higher scores indicating more perceived barriers identified by mothers. The content validity of the Breastfeeding Knowledge Questionnaire and the Perceived Breast Feeding Barriers Questionnaire was determined by three experts (40). Assessment of the readability, reliability and culture congruence of these two study questionnaires was made by a pilot study (40).
The Socio-demographic Data Questionnaire
The Socio-demographic Data Questionnaire was designed by the authors and includes personal information, maternal history, breastfeeding experiences and intention.
3.2. Translation Procedures and Permissions
Permission to use and translate the following questionnaires (IIFAS, The Breast Feeding Knowledge Questionnaire, The Perceived Breast Feeding Barriers Questionnaire) was given to the researchers by their developers. In particular, the IIFAS was also assessed for validity and reliability. To maintain semantic equivalence to the original version of the questionnaires, we applied a back-translation method. The forward translation was done by a professional translator, and another professional translator, who was blind to the original English version, translated it back to English. After this procedure, the Greek translation was deemed semantically equivalent to the original version.
Permission to use the BSES-SF was obtained by its developer and a translated version of the questionnaire to Greek was provided by her.
3.3. Statistical analysis
Quantitative variables were expressed as mean values (SD), while qualitative variables were expressed as absolute and relative frequencies. Independent samples Student’s t-tests were used for the comparison of mean values between the control and intervention group. For the comparison of proportions chi-square and Fisher’s exact tests were used. Pearson correlations coefficients were used to explore the association of two continuous variables. Correlation coefficient between 0.1 and 0.3 were considered low, between 0.31 and 0.5 moderate and those over 0.5 were considered high. Repeated measurements analysis of variance (ANOVA) was adopted to evaluate the changes observed in all study scales among the two groups pre- and post-intervention. All reported p values are two-tailed. Statistical significance was set at p<0.05 and analyses were conducted using SPSS statistical software (version 19.0).
3.4. Ethical considerations
This study was approved by the Research and Ethics Committee of the Greek Hospital (6/20-04-2016). Informed consent was obtained from all participants, by informing them about the scope and the purpose of the study and also assuring them that they had the right to withdraw in any phase of the study with no compromise to the standard of care they received at the hospital. Confidentiality was also assured.
4. RESULTS
The study sample consisted of 203 women (100 in the control group and 103 in the intervention group). Socio-demographic and pregnancy related characteristics of the sample, stratified by control/intervention group are presented in Table 1. No statistically significant difference was found between the two groups at baseline.
Table 1. Sample characteristics of participants in the study (n=203). +Student’s t-test *Fisher’s exact test **Pearson’s x2 test.
| Group | |||
|---|---|---|---|
| Control | Intervention | ||
| (N=100) | (N=103) | ||
| N(%) | N(%) | P | |
| Age, mean (SD) | 32.3 (5.4) | 33.4 (3.8) | 0.094+ |
| BMI (before pregnancy), mean (SD) | 23.2 (4.7) | + | 0.720+ |
| Place of residence | |||
| Urban | 80 (84.2) | + | 0.120* |
| Semi-urban | 8 (8.4) | + | |
| Rural | 7 (7.4) | + | |
| Nationality | |||
| Greek | + | + | 0.234** |
| Other | + | + | |
| Educational status | |||
| Primary to high school | + | + | 0.557* |
| University | + | + | |
| Postgraduate studies | + | + | |
| Family status | |||
| Married | + | + | 0.589** |
| Single/ Divorced | + | + | |
| Husband’s age, mean (SD) | + | + | 0.090+ |
| Relationship with husband | |||
| Very bad/bad/ moderate | 8 (8.2) | + | 0.235** |
| Good | 5 (5.2) | + | |
| Very good | 84 (86.6) | + | |
| Gestational week, mean (SD) | 36 (3.5) | + | 0.229+ |
| Conception | |||
| Normal | 97 (98) | + | 0.280* |
| IVF | + | + | |
| Problems during pregnancy | 32 (37.6) | + | 0.131** |
| + | 2 (2.4) | + | 0.229* |
| Haemorrhage | 1 (1.2) | + | 0.369** |
| Infections | 3 (3.5) | + | 1.000* |
| Contractions | 8 (9.4) | + | 0.311** |
| Anemia | 3 (3.5) | + | 0.498** |
| Gestational diabetes | 8 (9.4) | + | 0.868** |
| Hypertension/Preeclampsia | 2 (2.4) | + | 1.000* |
| Other | 10 (11.8) | + | 0.291** |
| + | 33 (34) | + | 0.454** |
| + | 10 (10.2) | + | 0.078** |
| + | 38 (38.8) | + | 0.610** |
| Alcohol consumption during pregnancy | |||
| <Once/ month | 66 (91.7) | + | 0.083* |
| 1-3 times/month | 5 (6.9) | + | |
| Once/week | 1 (1.4) | + | |
| Mild somatic exercise during pregnancy for at least 30 minutes/day | 43 (44.3) | + | 0.507** |
Pre-intervention there were no significant differences between control and intervention group in any of the scales measuring attitudes, knowledge, self-efficacy and breastfeeding perceived barriers (Table 2). However, attitude towards breastfeeding, knowledge about breastfeeding and breastfeeding self-efficacy were improved significantly (p<0.001) among women in the intervention group but were unchanged in the control group (Table 2). Similarly, the score for perceived breastfeeding barriers was significantly lower in the intervention group (p<0.001) but unchanged among women in the control group (Table 2, Figure 1). Consequently, the degree of change in all study scales, differ significantly between the two groups as indicated by the significant interaction effect of the repeated measurements analyses.
Table 2. Changes in attitudes towards breastfeeding, breastfeeding knowledge, self-efficacy and perceived barriers pre and post intervention, stratified by intervention and control groups (n=203). *p-value for group effect; **p-value for time effect; ‡Repeated measurements ANOVA. Effects reported include differences between the groups in the degree of change over the follow-up period.
| Pre | Post | Change | ||||
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | P** | ‡ | ||
| IIFAS | Control group | 66.11 (7.87) | 66.14 (7.82) | + | 0.952 | <0.001 |
| Intervention group | 67.62 (5.85) | 73.59 (5.43) | + | <0.001 | ||
| P* | 0.121 | <0.001 | ||||
| Breastfeeding Knowledge Questionnaire | + | 13.05 (2.2) | 13.11 (2.24) | + | 0.729 | <0.001 |
| Intervention group | 12.94 (2.17) | 14.65 (0.74) | + | <0.001 | ||
| P* | + | <0.001 | ||||
| BSES-SF | + | 45.62 (12.36) | 45.65 (12.29) | + | 0.947 | <0.001 |
| Intervention group | 43.32 (9.54) | 51.4 (8.89) | + | <0.001 | ||
| P* | + | <0.001 | ||||
| Perceived Barriers Questionnaire | Control group | 31.09 (5.45) | 31.05 (5.45) | + | 0.928 | <0.001 |
| Intervention group | 31.68 (5.53) | 27.41 (5.95) | + | <0.001 | ||
| P* | + | <0.001 | ||||
Figure 1. Change in mean perceived barriers score for each study group (n=203).
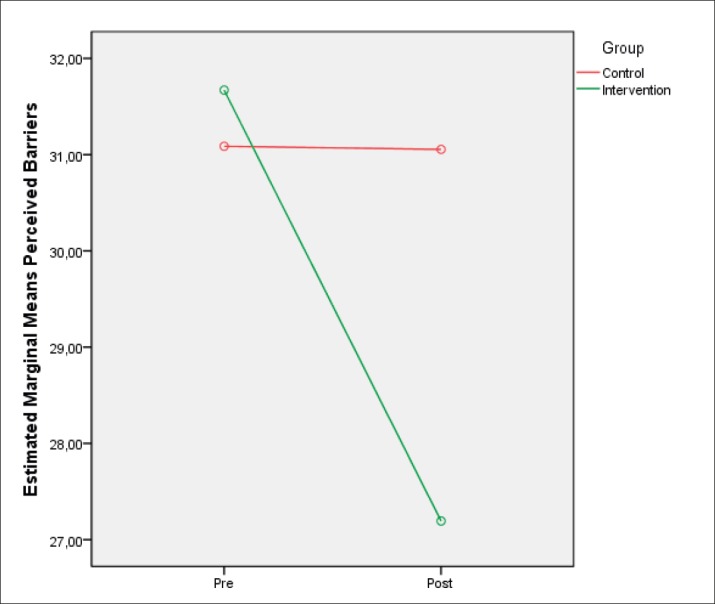
Table 3 shows the association of changes between the different study scales. A greater increase in the self-efficacy scale was found to be associated with a greater increase in both attitude and knowledge scales. On the contrary, a greater increase in attitude score was found to be associated with a greater decrease in perceived barriers scale.
Table 3. Pearson correlation coefficients to estimate changes in all study scales for the intervention group (n=103). *p<.05; **p<.01; ***p<.001.
| Change | |||
|---|---|---|---|
| Change | Knowledge | BSES-SF | Perceived Barriers Questionnaire |
| IIFAS | 0.21 | 0.24* | + |
| Breastfeeding Knowledge Questionnaire | 1.00 | 0.28* | + |
| BSES-SF | 1.00 | -0.16 | |
| Perceived Barriers Questionnaire | 1.00 | ||
5. DISCUSSION
Our quasi-experimental study showed that a four-hour structured, in-hospital, midwife-led, antenatal breastfeeding educational class, implemented between 32-37 weeks of pregnancy was effective in increasing participants’ breastfeeding knowledge, breastfeeding attitude, breastfeeding self-efficacy and in decreasing the breastfeeding perceived-barriers. These are all factors strongly related to extended breastfeeding (18, 21, 22, 24) and thus highly important modifiable factors when promoting continued breastfeeding. Similar to our findings, several other studies conclude that antenatal breastfeeding education has a positive effect on breastfeeding knowledge (41-44) and education in the antenatal period seems to be more effective in increasing exclusive breastfeeding, partial breastfeeding (10) and breastfeeding knowledge levels (45). Consistent with the above findings, research has also shown that antenatal education has a positive impact on breastfeeding attitudes (41, 42) and on breastfeeding self-efficacy (46, 47).
It was also noticeable that post-intervention the more the levels of knowledge, attitudes, and self-efficacy increased the more the perceived barriers decreased. A decline in breastfeeding is attributable primarily to perceived barriers of knowledge and attitude (48). According to our results, it is suggested that addressing barriers to breastfeeding through an educational programme may have the possibility to alter wrong thoughts concerning these barriers and lessen the perceived ones.
The strength of our study lies in the high response rate that ensured a large sample size (n=203). However, our study is not without limitations. The groups were not assigned in random and participants in the intervention group, who volunteered to participate may have been more positively predisposed to breastfeeding. Nevertheless, there was no significant difference between the two groups before the intervention. Moreover, participants were recruited by only one public maternity hospital in the city of Athens, thus limiting the generalizability of the findings. Though, this hospital serves pregnant women not only from the area of Athens but also from rural areas of Greece, with diverse cultural background and economic status, which makes the sample more representative for the Greek demographic.
6. CONCLUSION
The four-hour, midwife-led antenatal breastfeeding education class had a significant positive impact on breastfeeding knowledge, breastfeeding attitude, breastfeeding self-efficacy and breastfeeding perceived-barriers. This is a low-cost intervention with significant benefits, which occurs and is evaluated firstly in a Greek tertiary public maternity service and is recommended for integration to routine antenatal care as part of a strategy to reach the WHO’s target of 50% exclusive breastfeeding at six months, aiming in increasing the existing low rate in Greece as well.
Acknowledgments:
We are grateful to all the women who participated in this study.
Author’s contribution:
MI, KL, PP, ST gave substantial contribution to the conception or design of the work. MI, ST gave substantial contribution of data. All authors gave substantial contribution to the acquisition, analysis, or interpretation of data for the work. All authors had a part in article preparing for drafting or revising it critically for important intellectual content, and all authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Financial support and sponsorship:
None.
Conflict of interest:
There are no conflicts of interest.
REFERENCES
- 1.Ziegler AG, Wallner M, Kaiser I, Rossbaue M, Harsunen MH, Lachmann L, et al. Long-term protective effect of lactation on the development of type 2 diabetes in women with recent gestational diabetes mellitus. Diabetes. 2012;61(12):3167–3171. doi: 10.2337/db12-0393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ballard O, Ardythe L. Human milk composition: nutrients and bioactive factors. Paediatric Clinics of North America. 2013;60(1):49–74. doi: 10.1016/j.pcl.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carling SJ, Demment MM, Kjolhede CL, Olson CM. Breastfeeding duration and weight gain trajectory in infancy. Pediatrics. 2015;135(1):111–119. doi: 10.1542/peds.2014-1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS. Bellagio Child Survival Study Group. How many child deaths can we prevent this year? The Lancet. 2003;362(9377):65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Global Nutrition Targets 2025: Breastfeeding Policy Brief. 2014. [June 2018]. from ( http://apps.who.int/iris/bitstream/10665/149022/1/WHO_NMH_NHD_14.7_eng.pdf)
- 6.Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, Group TLBS. Why invest, and what it will take to improve breastfeeding practices? The Lancet. 2016;387(10017):491. doi: 10.1016/S0140-6736(15)01044-2. [DOI] [PubMed] [Google Scholar]
- 7.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child under nutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. World Health Statistics. 2013. [March 2018]. from ( www.who.int/gho/publications/world_health_statistics/2013/en/)
- 9.Bakoula C, Nicolaidou P, Veltista A, Prezerakou A, Moustaki M, Kavadias G, et al. Does exclusive breastfeeding increase after hospital discharge? A Greek study. Journal of Human Lactation. 2007;23(2):165–173. doi: 10.1177/0890334407300384. [DOI] [PubMed] [Google Scholar]
- 10.Bouras G, Mexi-Bourna P, Bournas N, Christodoulou C, Daskalaki A, Tasiopoulou I, et al. Mothers’ expectations and other factors affecting breastfeeding at six months in Greece. Journal of Child Health Care. 2013;17(4):387–396. doi: 10.1177/1367493512468358. [DOI] [PubMed] [Google Scholar]
- 11.Theofilogiannakou M, Skouroliakou M, Gounaris A, Panagiotakos D, Markantonis SL. Breast-feeding in Athens, Greece: factors associated with its initiation and duration. Journal of Pediatric Gastroenterology and Nutrition. 2006;43(3):379–384. doi: 10.1097/01.mpg.0000228104.97078.bb. [DOI] [PubMed] [Google Scholar]
- 12.Ladomenou F, Kafatos A, Galanakis E. Risk factors related to intention to breastfeed, early weaning and suboptimal duration of breastfeeding. Acta Paediatrica. 2007;96(10):1441–1444. doi: 10.1111/j.1651-2227.2007.00472.x. [DOI] [PubMed] [Google Scholar]
- 13.Vassilaki M, Chatzi L, Bagkeris E, Papadopoulou E, Karachaliou M, Koutis A, et al. Smoking and caesarean deliveries: major negative predictors for breastfeeding in the mother–child cohort in Crete, Greece (Rhea study) Maternal & child nutrition. 2014;10(3):335–346. doi: 10.1111/j.1740-8709.2012.00420.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaki E, Papamichael D, Sarafidou J, Panagiotopoulos T, Antoniadou-Koumatou I. Athens, Greece: 2009. National Survey of Prevalence and Determinants of Maternal Breastfeeding. Report of the Institute of Children’s Health/National School of Public Health – Sector of Children’s Health. (article in Greek) [Google Scholar]
- 15.Bosi ATB, Eriksen KG, Sobko T, Wijnhoven TM, Breda J. Breastfeeding practices and policies in WHO European region member states. Public health nutrition. 2016;19(4):753–764. doi: 10.1017/S1368980015001767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu Y, Zhang Z, Ling Y, Wan H. Impact of intervention on breastfeeding outcomes and determinants based on theory of planned behavior. Women and Birth. 2017;30(2):146–152. doi: 10.1016/j.wombi.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 17.Blyth RJ, Creedy DK, Dennis CL, et al. Breastfeeding duration in an Australian population: the influence of modifiable antenatal factors. Journal of Human Lactation. 2004;20(1):30–38. doi: 10.1177/0890334403261109. [DOI] [PubMed] [Google Scholar]
- 18.Inoue M, Binns CW, Otsuka K, Jimba M, Matsubara M. Infant feeding practices and breastfeeding duration in Japan: a review. International Breastfeeding Journal. 2012;7(1):15. doi: 10.1186/1746-4358-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dennis CL. Theoretical underpinnings of breastfeeding confidence: a self-efficacy framework. Journal of Human Lactation. 1999;15(3):195–201. doi: 10.1177/089033449901500303. [DOI] [PubMed] [Google Scholar]
- 20.Whitney EN, Rolfes SR. Cengage Learning; 2018. Understanding nutrition. [Google Scholar]
- 21.Kang NM, Choi YJ, Hyun T, Lee JE. Associations of Breastfeeding Knowledge, Attitude and Interest with Breastfeeding Duration: A Cross-sectional Web-based Study. J Korean Acad Nurs. 2015;45(3):449–458. doi: 10.4040/jkan.2015.45.3.449. [DOI] [PubMed] [Google Scholar]
- 22.Mi N, Ji Y, Eun J. Associations of Breastfeeding Knowledge, Attitude and Interest with Breastfeeding Duration. Journal of Korean Academy of Nursing. 2015;45(3):449–458. doi: 10.4040/jkan.2015.45.3.449. [DOI] [PubMed] [Google Scholar]
- 23.Scott JA, Kwok YY, Synnott K, Bogue J, Amarri S, Norin E, et al. A comparison of maternal attitudes to breastfeeding in public and the association with breastfeeding duration in four European countries: Results of a cohort study. Birth. 2015;42(1):78–85. doi: 10.1111/birt.12138. [DOI] [PubMed] [Google Scholar]
- 24.Cox KN, Giglia RC, Binns CW. The influence of infant feeding attitudes on breastfeeding duration: evidence from a cohort study in rural Western Australia. International Breastfeeding Journal. 2015;10(1):25. doi: 10.1186/s13006-015-0048-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sciacca JP, Dube DA, Phipps BL, Ratliff MI. A breast feeding education and promotion program: effects on knowledge, attitudes, and support for breast feeding. Journal of Community Health. 1995;20(6):473–490. doi: 10.1007/BF02277064. [DOI] [PubMed] [Google Scholar]
- 26.Svensson J. Antenatal breastfeeding education: Strategies for midwives. Women and Birth. 2015;28:S29. [Google Scholar]
- 27.Lorig K, Stewart A, Ritter P, Lynch J, Gonzalez V, Laurent D. Sage; 1996. Outcome measures for health education and other health care interventions. [Google Scholar]
- 28.World Health Organization. Geneva: 1998. Evidence for the ten steps to successful breastfeeding (WHO/CHD/98.6) [Google Scholar]
- 29.World Health Organization, United Nations Children’s Fund. Geneva: 2009. Baby-Friendly Hospital Initiative: revised, updated and expanded for integrated care. [PubMed] [Google Scholar]
- 30.Shealy KR, Li R, Benton-Davis S, Grummer-Strawn LM. The CDC guide to breastfeeding interventions. 2005.
- 31.UNICEF. Implementation Guidance. Protecting, promoting and supporting Breastfeeding in facilities providing maternity and newborn services: the revised Baby-Friendly Hospital Initiative. 2018.
- 32.Dennis CL. The breastfeeding self-efficacy scale: Psychometric assessment of the short form. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2003;32(6):734–744. doi: 10.1177/0884217503258459. [DOI] [PubMed] [Google Scholar]
- 33.Gregory A, Penrose K, Morrison C, Dennis CL, MacArthur C. Psychometric properties of the Breastfeeding Self-Efficacy Scale-Short Form in an ethnically diverse UK sample. Public Health Nursing. 2008;25(3):278–284. doi: 10.1111/j.1525-1446.2008.00705.x. [DOI] [PubMed] [Google Scholar]
- 34.Dennis CL, Faux S. Development and psychometric testing of the Breastfeeding Self-Efficacy Scale. Research in Nursing and Health. 1999;22(5):399–409. doi: 10.1002/(sici)1098-240x(199910)22:5<399::aid-nur6>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 35.Creedy DK, Dennis CL, Blyth R, Moyle W, Pratt J, Vries SM. Psychometric Characteristics of the Breastfeeding Self-Efficacy Scale: Data From an Australian Sample. Res Nurs Health. 2003;26(2):143–152. doi: 10.1002/nur.10073. [DOI] [PubMed] [Google Scholar]
- 36.Saljughi F, Savabi EM, Kohan S, Ehsanpour S. Promoting Breastfeeding Self-efficacy through Role-playing in Pregnant Women. Int J Pediatr. 2016;4(7):2061–2068. [Google Scholar]
- 37.Mora ADL, Russell DW, Dungy CI, Losch M, Dusdieker L. The Iowa infant feeding attitude scale: analysis of reliability and validity. Journal of Applied Social Psychology. 1999;29(11):2362–2380. [Google Scholar]
- 38.Twells LK, Midodzi WK, Ludlow V, Murphy-Goodridge J, Burrage L, Gill N, et al. Assessing infant feeding attitudes of expectant women in a provincial population in Canada: Validation of the Iowa infant feeding attitude scale. Journal of Human Lactation. 2016;32(3):NP9–NP18. doi: 10.1177/0890334414559647. [DOI] [PubMed] [Google Scholar]
- 39.Casal CS, Lei A, Young SL, Tuthill EL. A critical review of instruments measuring breastfeeding attitudes, knowledge, and social support. Journal of Human Lactation. 2017;33(1):21–47. doi: 10.1177/0890334416677029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hala S, Afaf M, Afnan S, Wadaa A. Breastfeeding knowledge, Attitude and Barriers among Saudi Women in Riyadh. Journal of Natural Sciences Research. 2013;3(12) ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) [Google Scholar]
- 41.Huang MZ, Kuo SC, Avery MD, Chen W, Lin KC, Gau ML. Evaluating effects of a prenatal web-based breastfeeding education programme in Taiwan. J Clin Nurs. 2007;16(8):1571–1579. doi: 10.1111/j.1365-2702.2006.01843.x. [DOI] [PubMed] [Google Scholar]
- 42.Arsin A, Arsunan S, Muh S. The effect of education lactation on breastfeeding behavior infant 0-6 months in Kendari Indonesia. Public Health of Indonesia. 2016;2(2):100–111. [Google Scholar]
- 43.Kronborg H, Maimburg RD. Væth M. Antenatal training to improve breast feeding: A randomised trial. Midwifery. 2012;28(6):784–790. doi: 10.1016/j.midw.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 44.Kani MF. A Study to Assess The Effectiveness of Structured Teaching Programme on Exclusive Breastfeeding Among the Primi Antenatal Mothers in A Selected Hospital, Tumkur. International Journal of Scientific Research. 2016;5(1):222–223. [Google Scholar]
- 45.Ugurlu M, Yavan T. The Effectiveness of Breastfeeding Education: An Integrative Review. Journal of Behavioral Health. 2016;5:182–190. [Google Scholar]
- 46.Noel-Weiss J, Rupp A, Cragg B, Bassett V, Woodend AK. Randomized controlled trial to determine effects of prenatal breastfeeding workshop on maternal breastfeeding self-efficacy and breastfeeding duration. Journal of Obstetric, Gynecologic and Neonatal Nursing. 2006;35(5):616–624. doi: 10.1111/j.1552-6909.2006.00077.x. [DOI] [PubMed] [Google Scholar]
- 47.Lin SS, Chien LY, Tai CJ, Lee CF. Effectiveness of a prenatal education programme on breastfeeding outcomes in Taiwan. Journal of Clinical nursing. 2008;17(3):296–303. doi: 10.1111/j.1365-2702.2006.01927.x. [DOI] [PubMed] [Google Scholar]
- 48.Roby JL, Woodson KS. An evaluation of a breast-feeding education intervention among Spanish-speaking families. Social work in health care. 2005;40(1):15–31. doi: 10.1300/j010v40n01_02. [DOI] [PubMed] [Google Scholar]


