Abstract
Introduction:
The method of carrying out PTB is one of the most controversial topics of modern perinatology, because there are no clear and undeniable works and studies that would in any case support vaginal delivery (VD) or delivery to the cesarean section (CS).
Aim:
To determine more frequent mode of delivery in different groups of birth weights and degrees of prematurity from single and twin pregnancies. To determine the degree of vitality of premature born vaginal delivery (VD) in relation to the cesarean section (CS) in different degrees of prematurity from single and twin pregnancies.
Patients and methods:
Research has retrospective cohort character. Data were collected from the databases of University Clinic of Gynecology and Obstetrics Tuzla for the period of five years (January 1st, 2012–December 31st, 2016). The study included newborns of both genders, gestational age from 24 to 37 weeks of gestation (WG) in singleton and twin pregnancies.
Results:
Out of 19506 births, 1350 (6.92%) were preterm birth (PTB). Singleton PTB was 1180 (87.40%), and the twins were 170 (12.59%). Vaginal delivery (VD) was born 788 (58.37%). Cesarean section (CS) was born 562 (41.63%). There was statistically significant association between the mode of delivery (MD) in singleton and twins pregnancy in all three subgroups of birth weight (BW) 1000-1499, 2000-2499 and >2500 grams in 33-37 WG. In this group was more frequent VD than CS mode of singleton delivery, and CS than VD mode of twins delivery. In contrast to newborn with BW 1500-1999 grams (chi-square = 23.16, P <0.0001) in same gestational period where was more frequent CS than VD (OR: 2.56, 95% CI: 1.71-3,85). Apgar score (AS) at first and five minute 5-7 and 8-10 in the period 28-32 and 33-37 was a statistically significant frequent in VD and singletons in contrast to CS and twins.
Conclusion:
VD was more frequent in the higher WG, as well as the higher AS in singletons in contrast to twins delivery.
Keywords: Pregnancy, Twins, Cesarean section
1. INTRODUCTION
Preterm birth (PTB) is defined delivery came before 37 weeks of gestation (WG). The problem of PTB is a high percentage of infant mortality due to immaturity of the lungs, as well as neurological damage. The incidence of PTB in the range of 5 to 18% (1, 2). There are two divisions of PTB, according to etiology which are medically indicated and spontaneous (idiopathic), and according to WG is stratified into mild preterm (33-37 WG), very preterm (28-32 WG) and extremely preterm (<28 WG) (2, 3, 4).
Spontaneous preterm birth (SPTB) includes idiopathic PTB and preterm premature rupture of membranes (PPROM); it does not include medical indicated PTB (4, 5). There is significant variation in the way that PTB is diagnosed, managed and treated at the international level (4, 6). Numerical assessment of the vitality of the newborn is carried out on the basis Apgar score (AS) (7).
The method of carrying out PTB is one of the most controversial topics of modern perinatology, because there are no clear and undeniable works and studies that would in any case support vaginal delivery (VD) or delivery to the cesarean section (CS) (8).
2. AIM
The first aim of this study is to determine more frequent mode of delivery in different groups of birth weights and degrees of prematurity from single and twin pregnancies.
The second aim of this study is to determine the degree of vitality of infants born VD in relation to the CS born in different degrees of prematurity from single and twin pregnancies.
3. PATIENTS AND METHODS
Research has retrospective cohort character. We retrospectively collected data from the databases of University Clinic of Gynecology and Obstetrics Tuzla for the period of five years (January 1st, 2012–December 31st, 2016). Out of 19506 births, 1350 (6,92%) were PTB. Singleton PTB was 1180 (87,40%), and the twins were 170 (12,59%).
Including criteria was newborns of both genders, gestational age from 24 to 37 WG. Exclusion criteria included stillbirths and terminations of pregnancy due to lethal fetal anomalies.
All newborns included in the study are divided in one of three groups based on the gestational age: mild preterm (33-37 WG); b) very preterm (28-32 WG); c) extremely preterm (<28 WG).
According to the gestational age were formed subgroups of birth weight (BW) (< 999 grams, 1000-1449 grams, 1500-1999 grams, 2000-2499 grams,> 2500 grams), for each of the three basic groups. All prematures are subdivided into additional subgroups singleton and gemels. The difference observed between the groups was tested by Pearson’s Chi-Squared and Fischer’s exact test with the level of significance of 0.05. Calculations were performed using Epi Info 7 program.
4. RESULTS
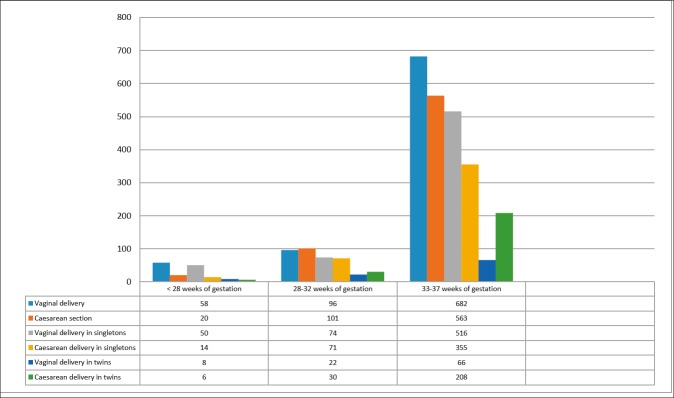
Vaginal delivery (VD) was born 788 (58,37%), of which 740 (93,90%) were singleton, and twins 48 (6,09%). Cesarean section (CS) was born 562 (41,63%), of which 440 (78,29%) singleton and 122 (21,70%) twins. Of the 170 twin pregnancies, 122 (71,76%) were completed by CS. Before the 28 WG, there were 71 (5,25%) births, before 32 WG 171 (12,66%) births and between 32-37 WG was 1108( 82,07%) births (Figure 1).
Figure 1. Distribution of preterm births by weeks of gestation and mode of delivery in singletons and twins.
Mode of delivery (MD), VD or CS, was no statistically significant for newborn with BW <999 g, none of the three periods of gestation. There was no statistically significant correlation between the MD in singleton and twins pregnancy in <28 WG (chi-square = 1.20, P = 0.274). MD, VD or CS, was no statistically significant for newborn in any group by BW, in gestational periods <28 and 28-32 WG.
There was a statistically significant correlation between the MD and newborn with BW 1000-1499 grams (chi-square = 10.56, P = 0.0012), BW 2000-2499 grams (chi-square = 10.56, P = 0.0012) and BW >2500 grams (chi-square = 62.73, P <0.0001) in 33-37 WG. In this group was more frequent VD than CS MD. In contrast to newborn with BW 1500-1999 grams (chi-square = 23.16, P <0.0001) in same gestational period where was more frequent CS than VD MD ( OR: 2.56, 95% CI: 1.71-3,85).
There was statistically significant association between the MD in singleton and twins pregnancy in all four subgroups of BW in 33-37WG. In this group was more frequent VD than CS mode of singleton delivery, and CS than VD mode of twins delivery (Table 1).
Table 1. Mode of delivery in correlation to birth weight (BW) and weeks of gestation (WG) in singleton (S) and twins (T) delivery, Vaginal delivery (VD), Caesarean section (CS).
| BW WG | VD | CS | χ2 | P | OR | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
| <999 | N=59 | N= 33 | ||||||
| <28 | 47 | 18 | 0.34 | 0.562 | 0.47 | 0.10-2.36 | ||
| 28-32 | 11 | 14 | 0.09 | 0.770 | 0.80 | 0.35-1.87 | ||
| <28 | S | T | S | T | 1.20 | 0.274 | 2.44 | 0.70-8.43 |
| 39 | 8 | 12 | 6 | |||||
| 28-32 | 11 | 0 | 13 | 1 | Fisher | 0.56 | - | - |
| 1000-1499 | N=48 | N= 64 | ||||||
| <28 | 10 | 1 | 1.10 | 0.295 | 4.17 | 0.50-34.74 | ||
| 28-32 | 30 | 39 | 0.87 | 0.351 | 0.72 | 0.40-1.30 | ||
| 33-37 | 8 | 24 | 10.56 | 0.0012 | 3.75 | 1.61-9.73 | ||
| 28-32 | 23 | 7 | 29 | 10 | 0.00 | 1.000 | 1.13 | 0.37-3.44 |
| 33-37 | 7 | 1 | 13 | 11 | 1.6 | 0.206 | 5.92 | 0.63-56.85 |
| 1500-1999 | N=88 | N= 118 | ||||||
| 28-32 | 42 | 38 | 0.53 | 0.465 | 1.29 | 0.73-2.28 | ||
| 33-37 | 45 | 80 | 23.16 | <0.0001 | 2.56* | 1.71-3.85 | ||
| 28-32 | 27 | 15 | 22 | 16 | 0.13 | 0.722 | 1.31 | 0.53-3.23 |
| 33-37 | 34 | 11 | 45 | 35 | 3.82 | 0.05 | 2.4 | 1.07-5.41 |
| 2000-2499 | N=168 | N= 204 | ||||||
| 28-32 | 11 | 8 | 0.87 | 0.351 | 0.72 | 0.40-1.30 | ||
| 33-37 | 157 | 195 | 10.56 | 0.0012 | 3.75 | 1.61-9.73 | ||
| 28-32 | 11 | 0 | 7 | 1 | Fisher | 0.842 | - | - |
| 33-37 | 131 | 26 | 118 | 77 | 20.99 | <0.0001 | 3.29 | 1.93-5.70 |
| >2500 | N=473 | N= 265 | ||||||
| 33-37 | 471 | 263 | 62.73 | <0.0001 | 2.55 | 2.02-3.21 | ||
| 33-37 | 444 | 27 | 179 | 84 | 89.02 | <0.0001 | 7.77 | 4.87-12.39 |
AS at first minute <4 was not dependent on the MD in the period <28 WG (chi-square = 0, P = 1) neither in the 28-32 WG (chi-square = 0.11, P = 0.744). AS <4 in 33-37 WG was more frequent in VD than CS MD ( OR=0.416, 95%CI: 0.24-0.69) and in singletons. AS 5-7 and 8-10 in the period 28-32 and 33-37 was a statistically significant frequent in VD for singletons. AS< 4 after 5 minutes was not correlate with MD in any period of gestation for singletons and twins. AS 5-7 after 5 minutes in the period 28-32 WG and 33-37 WG was a statistically significant frequent in VD and singletons. AS 8-10 after 5 minutes in the period 33-37 WG was 2.63 more frequent for VD and singletons (Table 2).
Table 2. Mode of delivery according to weeks of gestation (WG) and Apgar scor (AS) in singleton (S) and twins (T) delivery, Vaginal delivery (VD), Caesarean section (CS).
| WG AS | VD | CS | χ2 | P | OR | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
| AS <4 1' | N=113 | N= 106 | ||||||
| <28 | 54 | 19 | 0.00 | 1.000 | 0.71 | 0.02-7.82 | ||
| 28-32 | 33 | 38 | 0.11 | 0.744 | 0.87 | 0.48-1.56 | ||
| 33-37 | 26 | 49 | 12.18 | 0.0005 | 0.416 | 0.24-0.69 | ||
| <28 | S | T | S | T | 1.58 | 0.209 | 2.65 | 0.63-10.51 |
| 46 | 8 | 13 | 6 | |||||
| 28-32 | 25 | 8 | 30 | 8 | 0.001 | 0.748 | 0.83 | 0.23-2.97 |
| 33-37 | 25 | 1 | 32 | 17 | 7.25 | 0.007 | 13.28 | 1.79-576.8 |
| AS 5-7 1' | N=87 | N= 162 | ||||||
| <28 | 4 | 1 | 0.00 | 1.000 | 1.33 | 0.12-69.07 | ||
| 28-32 | 15 | 33 | 6.86 | 0.009 | 0.38 | 0.18-0.80 | ||
| 33-37 | 68 | 128 | 36.93 | <0.0001 | 0.38 | 0.27-0.52 | ||
| 28-32 | 11 | 4 | 25 | 8 | 0.00 | 1.000 | 0.88 | 0.18-4.87 |
| 33-37 | 56 | 12 | 81 | 47 | 6.80 | 0.009 | 2.71 | 1.27-6.10 |
| AS 8-10 1' | N=636 | N= 406 | ||||||
| 28-32 | 48 | 20 | 7.65 | 0.006 | 2.37 | 1.27-4.44 | ||
| 33-37 | 588 | 386 | 55.42 | <0.0001 | 2.87 | 2.15-3.84 | ||
| 28-32 | 38 | 10 | 16 | 14 | 4.63 | 0.031 | 3.33 | 1.09-10.21 |
| 33-37 | 535 | 53 | 242 | 144 | 113.86 | <0.0001 | 6.00 | 4.18-8.69 |
| AS <4 5' | N=91 | N= 62 | ||||||
| <28 | 47 | 19 | 1.28 | 0.257 | 0.22 | 0.005-1.78 | ||
| 28-32 | 24 | 23 | 0.17 | 0.842 | 1.13 | 0.56-2.30 | ||
| 33-37 | 20 | 20 | 0.21 | 0.649 | 0.82 | 0.41-1.62 | ||
| <28 | 41 | 6 | 13 | 6 | 2.10 | 0.149 | 3.15 | 0.79-13.91 |
| 28-32 | 22 | 2 | 19 | 4 | 0.24 | 0.622 | 2.32 | 0.29-27.8 |
| 33-37 | 19 | 1 | 16 | 4 | 0.91 | 0.339 | 4.75 | 0.40-246.00 |
| AS 5-7 5' | N=54 | N= 113 | ||||||
| 28-32 | 18 | 36 | 6.24 | 0.013 | 0.42 | 0.20-0.84 | ||
| 33-37 | 30 | 77 | 1.31 | 0.250 | 0.75 | 0.46-1.20 | ||
| 28-32 | 11 | 7 | 29 | 7 | 1.46 | 0.227 | 0.38 | 0.09-1.62 |
| 33-37 | 26 | 4 | 43 | 34 | 7.66 | 0.006 | 5.13 | 1.55-21.91 |
| AS 8-10 5' | N=691 | N= 509 | ||||||
| <28 | 5 | 1 | 0.001 | 0.97 | 1.79 | 0.18-89.18 | ||
| 28-32 | 54 | 42 | 3.67 | 0.055 | 1.81 | 0.99-3.31 | ||
| 33-37 | 632 | 466 | 28.07 | <0.0001 | 2.63 | 1.81-3.86 | ||
| 28-32 | 41 | 13 | 71 | 30 | 0.31 | 0.577 | 1.33 | 0.59-3.10 |
| 33-37 | 571 | 61 | 296 | 170 | 114.61 | <0.0001 | 5.38 | 3.85-7.56 |
5. DISCUSSION
Our study showed that most frequent mode of delivery (MD) in preterm birth (PTB) in singleton pregnancies was vaginal delivery (VD). VD may be a MD in case of vertex presentation and when the delivery progresses normally, cesarean section (CS) are not recommended for fetuses in vertex presentation. Today, there is often a doubt in the benefit of the CS for neonatal outcome in spontaneous preterm birth (SPTB), even in a group of infants with extremely low birth weight (BW) (8, 9, 10). When complicated by breech presentation the delivery seems to be best performed by the CS (10, 11). Retrospective cohort study carried out by Niles et al suggested that CS delivery of breech prematures had a protective effect on neonatal mortality compared to VD (12). Routine CS is not recommended only because of prematurity (8, 10, 11, 13). Systematic review performed by Dagenais C et al suggested that on the safest MD for extremely preterm vertex/non-vertex presentation twins found very limited existing evidence, without significant differences in neonatal death and severe brain injury in relation to MD (14-15).
Systematic assisted VD is not recommended during PTB. Use of vacuum is possible after 34 WG when cranial vertex ossification is considered satisfactory, unlike forceps, where many studies have suggested that it does not benefit in PTB (8). Although it has long been suggested that episiotomy at birth may reduce the risk of fetal injury, recent studies do not recommend the systematic use of episiotomy in case of PTB (13,8).
The incidence of low AS is inversely linearly related to BW, and it is affected by gestational age. Low AS may receive only because of immaturity. However, there are no consistent data on the significance of the AS in preterm infants (7).
Hegyi et al in their study concluded that low AS (<3 at 1 minute and <6 at 5 minutes) was significantly associated with BW, gestational age and MD (16).
Incidence PTB in our study is even in a mild decrease when compared with PTB in other European countries (5.4–11.4%) (17-18, 20). Kuehn reported an even higher incidence of PTB (13%) in the USA (21).
In study Schaaf et al incidence of PTB in singleton pregnancies by WG was <28-0.35% , 28-32-0.6 %, 33-37-5.1% (18), and 5.4% in study Barros et al (22). In our study was <28 WG-0.33% (N=64), 28-32WG-0.74% (N=145), 33-37 WG-4.98% (N= 971) which correlates with above mentioned studies.
The proportion of CS due to prematurity (< or = 37th WG) is about 34% in Westphalia-Lippe; in our study 41.63 % (N=562/1350), which is higher, immature preterm infants (< or = 32nd week of gestation) are delivered by CS is approximately 60% (median) in our clinic 42.56 % (N=103/242), which is lower (23). In study Sun et al CS rate was 52.9%, which is higher than in our study (17). In study Barros et al the CS rate in the late preterm group 34-36 WG was (39.1%), in our clinic ratio between VD and CS was 41.42 % (N=459/1108) for CS in the late preterm group 33-37 WG, which is slightly higher in our study (22). CS rates in very preterm birth (28–31 weeks) also showed a wide range (49–88%) amongst ten developed European regions in coincidence with our study where CS rate in group 28-32 WG was 50.29% ( N=86/171) (24). Roemer study was shown that for PTB in general (< or = 37th WG) lower the mortality rate between the 1st and 7th days of life for the higher incidence VD in contrast to immature preterm infants (< or = 32nd WG) show no significant correlation between MD and mortality rate(23).
In study Dietl J et al the CS rate of very preterm infants (1500 g, ≤ 32 WG) increased from 28% during the period 1977-1982 to 87% during the period 1982-1987 (P < 0.005), accompanied by an increase in survival rate from 63% to 70% (25). In our study we investigated the incidence of the CS rate of very preterm infants (1500 g, ≤ 32 weeks’ gestation) in the period from 2012 to 2016, it was 48.61% (N=35/72), which is significantly less compared to study Dietl et al. (25).
The strength of this study is the sample size and the standardized data collection, despite the retrospective nature of the analysis.
Our data have several limitations. The study had a retrospective nature of data collection, which was subject to a potential risk of incorrectly completed records.
This is the first study to date aiming MD in PTB in B&H. Nevertheless, it is an important finding that in our study, the prevalence of different stages of singleton and twins PTB is relatively reduced when compared to other published series in world and in our country (20, 19, 18, 17).
A prospective study of planned method of delivery is recommended to further explore this finding. Therefore, these findings should be confirmed in larger studies.
We believe that our data compel future research in this field, in order to better understand the MD in PTB.
6. CONCLUSION
Vaginal delivery was more frequent in the higher weeks of gestation, as well as the higher Apgar score in singletons in contrast to twins delivery.
Author’s contribution:
Anis Cerovac gave substantial contributions to the conception or design of the work in acquisition, analysis, or interpretation of data for the work. Each author had a part in article preparing for drafting or revising it critically for important intellectual content. Each author gave final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Financial support and sponsorship:
None.
Conflict of interest:
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization (WHO) Geneva, Switzerland: WHO; 2018. Feb, Preterm birth. [updated 2018 Feb 19; cited 2018 Aug 9]. Available from: http://www.who.int/news-room/fact-sheets/detail/preterm-birth. [Google Scholar]
- 2.Ananth CV, Vintzileos AM. Epidemiology of preterm birth and its clinical subtypes. J Matern Fetal Neonatal Med. 2006;19:12, 773–782. doi: 10.1080/14767050600965882. [DOI] [PubMed] [Google Scholar]
- 3.Moutquin JM. Classification and heterogeneity of preterm birth. BJOG. 2003;110:130. doi: 10.1016/s1470-0328(03)00021-1. -doi:3.10.1046/j.1471-0528.2003.00021. [DOI] [PubMed] [Google Scholar]
- 4.Di Renzo GC, Roura LC, Facchinetti F, et al. Guidelines for the management of spontaneous preterm labor: identification of spontaneous preterm labor, diagnosis of preterm premature rupture of membranes, and preventive tools for preterm birth. J Matern Fetal Neonatal Med. 2011;24:5, 659–667. doi: 10.3109/14767058.2011.553694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grgić G. Preterm birth. Tuzla: PrintCom; 2011. Etiological factors of preterm birth; pp. 17–33. [Google Scholar]
- 6.Harding JE, Pang J, Knight DB, et al. Do antenatal corticosteroids help in the setting of preterm rupture of membranes? Am J Obstet Gynecol. 2001 Jan;184(2):131–139. doi: 10.1067/mob.2001.108331. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics, Committee on Fetus and Newborn; American College of Obstetricians and Gynecologists and Committee on Obstetric Practice. The Apgar score. Pediatrics. 2006 Apr;117(4):1444–1447. [Google Scholar]
- 8.Grgić G, et al. Preterm birth. Tuzla: PrintCom; 2011. Method of guiding of preterm delivery; pp. 111–122. [Google Scholar]
- 9.Sentilhes L, Sénat MV, Ancel PY, et al. Prevention of spontaneous preterm birth: Guidelines for clinical practice from the French College of Gynaecologists and Obstetricians (CNGOF) Eur J Obstet Gynecol Reprod Biol. 2017 Mar;210:217–224. doi: 10.1016/j.ejogrb.2016.12.035. [DOI] [PubMed] [Google Scholar]
- 10.Alfirevic Z, Milan SJ, Livio S. Caesarean section versus vaginal delivery for preterm birth in singletons. Cochrane Pregnancy and Childbirth Group. 2013 Sep 12; doi: 10.1002/14651858.CD000078.pub3. doi. 10.1002/14651858. CD000078.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Solum T. Management of the extreme premature delivery. J Perinat Med. 1991;19(Suppl 1):317–320. [PubMed] [Google Scholar]
- 12.Niles KM, Barrett JFR, Ladhani NNN. Comparison of cesarean versus vaginal delivery of extremely preterm gestations in breech presentation: retrospective cohort study. J Matern Fetal Neonatal Med. 2017 Nov 20;:1–6. doi: 10.1080/14767058.2017.1401997. [DOI] [PubMed] [Google Scholar]
- 13.Mottet N, Riethmuller D. Mode of delivery in spontaneous preterm birth. J Gynecol Obstet Biol Reprod. 2016 Nov;45(10):1434–1445. doi: 10.1016/j.jgyn.2016.09.021. [DOI] [PubMed] [Google Scholar]
- 14.Dagenais C, Lewis-Mikhael AM, Grabovac M, et al. What is the safest mode of delivery for extremely preterm cephalic/non-cephalic twin pairs? A systematic review and meta-analyses. BMC Pregnancy Childbirth. 2017 Nov 29;17(1):397. doi: 10.1186/s12884-017-1554-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vergani P, Locatelli A, Ratti M, et al. Predictors of adverse perinatal outcome in twins delivered at < 37 weeks. J Matern Fetal Neonatal Med. 2004 Dec;16(6):343–347. doi: 10.1080/14767050400018254. [DOI] [PubMed] [Google Scholar]
- 16.Hegyi T, Carone T, Anwar M, et al. The Apgar score and its components in the preterm infant. Pediatrics. 1998;101:77–81. doi: 10.1542/peds.101.1.77. [DOI] [PubMed] [Google Scholar]
- 17.Sun L, Yue H, Sun B, et al. Estimation of birth population-based perinatal-neonatal mortality and preterm rate in China from a regional survey in 2010. J Matern Fetal Neonatal Med. 2013;26:16, 1641–1648. doi: 10.3109/14767058.2013.794208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schaaf J, Mol B, Abu-Hanna A, et al. Trends in preterm birth: singleton and multiple pregnancies in the Netherlands, 2000-2007. BJOG. 2011;118:1196–1204. doi: 10.1111/j.1471-0528.2011.03010.x. [DOI] [PubMed] [Google Scholar]
- 19.Tough S, Svenson L, Johnston D, et al. Characteristics of Preterm Delivery and Low Birthweight Among 113,994 Infants in Alberta: 1994-1996. Can J Public Health. 2001 Jul-Aug;92(4):276–280. doi: 10.1007/BF03404960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hudic I, Stray-Pedersen B, Skokic F, et al. Low Preterm Birth Rate With Decreasing Early Neonatal Mortality in Bosnia and Herzegovina During 2007-2014. Mater Sociomed. 2016 Feb;28(1):32–35. doi: 10.5455/msm.201628.32-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuehn BM. Scientists probe the role of clinicians in rising rates of late preterm birth. J Am Med Assoc. 2010;303:1129–1136. doi: 10.1001/jama.2010.296. [DOI] [PubMed] [Google Scholar]
- 22.Barros J, Clode N, Gracia L. Prevalence of Late Preterm and Early Term Birth in Portugal. Acta Med Port. 2016 Apr;29(4):249–253. doi: 10.20344/amp.6523. http://dx.doi.org/10.20344/amp.6523. [DOI] [PubMed] [Google Scholar]
- 23.Roemer VM. Considerations and observations on management of premature labor. Gynakol Geburtshilfliche Rundsch. 1998;38(3):131–142. doi: 10.1159/000022251. [DOI] [PubMed] [Google Scholar]
- 24.Zeitlin J, Di LD, Blondel B, et al. Variability in caesarean section rates for very preterm births at 28- 31 weeks of gestation in 10 European regions: results of the MOSAIC project. Eur J Obstet Gynecol Reprod Biol. 2010;149:147–152. doi: 10.1016/j.ejogrb.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 25.Dietl J, Arnold H, Haas G, et al. Delivery of very premature infants: does the caesarean section rate relate to mortality, morbidity, or long-term outcome? Arch Gynecol Obstet. 1991;249(4):191–200. doi: 10.1007/BF02390387. [DOI] [PubMed] [Google Scholar]