Abstract
Faith and public health partnerships offer promise to addressing health disparities but examples that incorporate African Americans and Latino congregations are lacking. Here we present results from developing a multi-ethnic, multi-denominational faith and public health partnership to address health disparities through community-based participatory research (CBPR), focusing on several key issues: 1) the multi-layered governance structure and activities to establish the partnership and identify initial health priority (obesity); 2) characteristics of the congregations recruited to partnership (n=66); and 3) the lessons learned from participating congregations’ past work on obesity that informed the development of a multi-level, multi-component, church-based intervention. Having diverse staff with deep ties in the faith community, both among researchers and the primary community partner agency, was key to recruiting African American and Latino churches. Involvement by local health department and community health clinic personnel provided technical expertise and support regarding health data and clinical resources. Selecting a health issue – obesity – that affected all subgroups (e.g., African Americans and Latinos, women and men, children and adults) garnered high enthusiasm among partners, as did including some innovative aspects such as a text/email messaging component and a community mapping exercise to identify issues for advocacy. Funding that allowed for an extensive community engagement and planning process was key to successfully implementing a CBPR approach. Building partnerships through which multiple CBPR initiatives can be done offers efficiencies and sustainability in terms of programmatic activities, though long-term infrastructure grants, institutional support, and non-research funding from local foundations and health systems are likely needed.
Keywords: church-based health promotion, community partnerships, African Americans, Latinos, health disparities, community-based participatory research
INTRODUCTION
Although there has been substantial progress in improving overall population health in the United States (U.S.) over the last several decades, racial and ethnic inequalities in a variety of health outcomes have not changed considerably in this same period [1]. African Americans and Latinos have substantially higher burdens and poorer outcomes than whites on a number of health conditions, including cardiovascular health [2], diabetes [3], cancer [4–7], HIV [8], and obesity [9]. The causes of disparities are complex and involve reduced access to quality healthcare [10–12] and reduced utilization of healthcare including important primary preventive services, even after controlling for insurance status [10, 11]. Implementation of the Affordable Care Act has reduced racial-ethnic disparities in health insurance coverage, especially in states where Medicaid was expanded, but substantial disparities remain [13]. Additional factors contributing to disparities may include medical distrust, poor physician-patient interactions related to cultural differences in communication styles, and negative expectations about the medical encounter given past experiences [14, 15]. In addition, neighborhood socioeconomic disadvantage and racial segregation have been found to be associated with increased mortality and morbidity [16–18].
This complex set of potential causes of disparities suggests that solutions must also be multifaceted and include participation from community-based organizations as well as health care providers and public health agencies. One option for addressing disparities is through partnerships between public health providers and faith-based organizations (FBOs). Local health departments and community clinics typically play a major role in promoting health, especially in underserved neighborhoods, but recent research highlights profound cuts to this sector, including substantial reductions in core funding and staffing [19]. Partnerships can increase the capacity of health departments and the broader public health community to provide public health services [20]. The need to develop such partnerships is high since recent research suggests that collaborations between religious congregations (a key type of FBO at the community level) and health departments are rare and underutilized, with only about 20% of all congregational partnerships involving government agencies [21].
Religious congregations are credible, stable entities that have significant reach within underserved neighborhoods as well as a history of providing and supporting social services, including health promotion and care. There are currently an estimated 300,000 religious congregations in the U.S. [22], and national surveys have found that about half of all adults attend religious services at least monthly [23]. African Americans and Latinos are more likely to self-identify as religious than the general population [24, 25]. Congregations provide physical infrastructure and complex social networks that can be leveraged for health promotion and services. Further, according to the 2012 National Congregations Study, an estimated 87% of congregations provided social services either formally or informally [26], up from 58% in 1998 and 82% in the 2006-2007 [27, 28], and 57% of congregations engaged in some type of health program [29]. Minority congregations in particular are often viewed as trusted resources by their members [30–32] and can help provide culturally sensitive programs to improve health.
Over the past several decades, there has been increasing interest in the role that congregations can play in community health promotion. Reviews of church-based health interventions have found that most have focused on African American churches and have involved limited numbers of churches and denominations [33, 34]. Further, most efforts to engage congregations in health promotion have been initiated to focus on a particular health issue, yet approaches that engage congregations around reducing disparities more generally are needed because of how pervasive disparities are among certain minority communities and the complex factors driving them [35].
Here we describe our experience developing a multi-ethnic, multi-denominational faith and public health partnership to address health disparities. Specifically, we focus on several key aspects of the development of this partnership: 1) the multi-layered governance structure and activities to establish the partnership and identify initial health priorities; 2) characteristics of the congregations involved in the partnership; and 3) the development of a multi-level, multi-component, church-based intervention. The activities described herein spanned a period of approximately 18 months: 10-12 months for partnership development and consensus-building about the health focus and 6-8 months for intervention development.
Our approach is guided by established approaches to community-based and church-based research as well as the socio-ecological framework. First, we followed principles of community-based participatory research (CBPR), in which community stakeholders were involved in all phases of the research and participated in shared decision-making regarding the research focus, goals, and methods [36]. Second, our congregation-based approach draws upon prior research, which suggests that repeated interactions beginning with the invitation to participate and moving through each stage of the project also help build trust and strengthen partnerships [35]. Our focus on pastors and other church leaders recognizes, as past work has, that their influence on congregational attitudes in general and toward health programs in particular can be critical to the success of those programs [37–39]. Finally, the development of our multi-level, multi-component congregation-based intervention draws heavily on the socio-ecological theory, which posits that health is influenced by multiple levels (intrapersonal, interpersonal, organizational, physical and social environment, and policy) [40].
METHODS
Context
Our partnership development focused on religious congregations and public health organizations in South Los Angeles (LA), an area that is overwhelmingly African American and Latino (95% in 2017). It is important to note the changing proportion of each of these groups over the last part of the 20th century and into the 21st century, during which African Americans went from the majority to a minority (28% African American in 2017 vs. 68% Latino), mostly through moving out of the area. However, African American churches retain a strong presence in South LA and many congregants commute back for worship and other church activities. Partnerships to address health in South LA must therefore involve representatives of both communities, and interventions targeting this community must consider its social context. Yet there are few organizations that bring together African American and Latino faith leaders in South LA; even within the race-ethnic groups, faith-based associations rarely cut across denominations. Further, although faith-based and public health leaders have been convened to address specific health issues, they have not focused on addressing disparities more generally.
Table 1 provides an overview of Service Planning Area 6, the LA County designation for the area in South LA. Compared to the county overall, our study area has higher proportions of Latinos and African Americans and immigrants, lower socio-economic status (lower levels of education, higher levels of poverty and unemployment), and worse health-related outcomes across various measures (obesity, HIV, mortality, and healthcare access). Almost all South LA has also been designated as a medically underserved area and health professional shortage area (see https://datawarehouse.hrsa.gov/tools/analyzers/muafind.aspx). This means that the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services has found that this community has too few primary care medical, dental and mental health providers, high infant mortality, as well as high poverty or a high elderly population.
Table 1:
Demographic Health Disparity Information for Service Planning Area (SPA) 6 iSouth LA)
| Characteristic | South LA SPA (#6) | LA County/All SPAs |
|---|---|---|
| POPULATION | ||
| Race/Ethnicity | ||
| Latino (%) | 68.2 | 48.4 |
| African American (%) | 27.4 | 8.5 |
| White (%) | 2.4 | 28.3 |
| Asian/Pacific Islander (%) | 1.9 | 14.6 |
| American Indian/Alaskan Native (%) | 0.1 | 0.2 |
| Percent of adults who were not bom in the US | 51.9 | 16.3 |
| Percent of adults that speak mostly Spanish at home | 48.8 | 12.5 |
| Education | ||
| Less than high school graduate | 41.6 | 22.4 |
| High school graduate | 25.7 | 21.5 |
| > High school | 32.6 | 56.1 |
| Unemployed | 13.6 | 10.2 |
| Percent of population with household incomes <100% FPL | 33.6 | 18.4 |
| HEALTH INFORMATION | ||
| Percent of adults who are obese (BMI ≥ 30.0) | 34.1% | 23.5% |
| Incidence of HIV (ages 13+) – annual new cases per 100,000 | 35.1 | 24.3 |
| All-cause mortality (age-adjusted per 100,000 population) | 726.6 | 593.5 |
| Percent of adults who reported difficulty access medical care | 32.5% | 23.6% |
Source: LA County Key Indicators of Health 2017
Partnership Structure
The primary partners include Los Angeles Metropolitan Churches (LAM), a non-profit organization that aims to increase congregations’ capacity to influence policy, and the RAND Corporation, a non-profit research organization that aims to influence policy. Specifically, LAM’s mission is to develop the capacity of member congregations and religious and community leaders in the greater Los Angeles area to achieve policy change in the communities where they live, work and worship. RAND and LAM received a community planning grant from the National Institute of Minority Health and Health Disparities (NIMHD) as part of their CBPR initiative to develop this partnership. LAM staff involved in the partnership included the executive director and two part-time faith organizers hired through our grant, one African American pastor and one Latino pastor. (LAM also has several other staff working on different initiatives). The RAND team included researchers with backgrounds in public health, health policy, survey research, and clinical psychology; researchers were also diverse across gender, race/ethnicity (African American, Latino, Asian, and Caucasian) and language (English-Spanish).
Two clergy leaders also formed part of the core operating and served as co-chairs of the Partnership Steering Committee, which included 10-12 faith leaders and two important public health leaders – one, the area health officer for South Los Angeles from the county health department and the other, the executive director of the network of community health centers serving South Los Angeles. The Steering Committee met regularly to shape the development of the partnership and specific project goals and methods. The faith-based leaders of the Steering Committee played key roles in helping reach out to the churches in their respective associations to solicit their participation in the partnership and its activities (e.g., needs assessment, selection of a health condition for focused attention, formative research, intervention pilot). LAM served as the lead convening agency in organizing and hosting meetings of the Steering Committee. The public health leaders of the Steering Committee played key roles in helping leverage assets from their organizations and networks to support the work of the partnership – for example, the health department providing data on community health needs and community clinics provided staff to help collect biometric data on congregants. The research members of the Steering Committee played key roles in providing technical and substantive expertise and leveraging relevant resources available at RAND and though external funding.
Initial Partnership Research Activities
We conducted several research activities early in the partnership to help identify health priorities and design our church-based intervention. RAND researchers and LAM staff collaborated to conduct all research activities. First, we asked each congregation that wanted to participate in the partnership to complete a Church Information Form (CIF), which provided information about congregation size, demographics, and experience with health programming. We aimed to recruit 60-80 congregations as this was deemed sufficient to give us a range of congregational types (African American and Latino of various denominations and sizes) but also to be manageable for engaging congregations in on-going partnership activities. Second, we conducted community expert interviews, which consisted of 16 semi-structured interviews to identify facilitators and barriers to faith and health partnerships, especially those involving diverse racial and ethnic groups. We used this information to identify best practices for the operation of our own partnership. Third, we implemented an extensive consensus-building process to identify the partnership’s initial health focus. This included conducting 14 community meetings hosted by Steering Committee members over a 3-4-month period to review community health data and generate a list of priority health concerns. Subsequently, we conducted a formal consensus-building process over a 1-2 month period using ExpertLens, a novel on-line iterative system and methodology developed by RAND researchers [41]. This involved having partnership members rate health conditions on various criteria, review their rankings in comparison to others and engage in discussion, and then re-rate the health conditions (we implemented an on-line and in-person versions of this process to enhance participation among partnership members). Finally, once obesity was selected as the priority health issue, we interviewed partners who had experience with church-based obesity programs and worked with community partners to design a multi-level, multi-component intervention to pilot with several partner churches. (The details of the community expert interviews and ExpertLens activities are reported elsewhere; here we focus on the description of partner churches from the CIF data, past partner experiences with church-based obesity programs, and the development of our multi-level, multi-component church-based intervention).
In terms of the costs associated with such partnerships, most of the grant funding was used for portions of researcher and LAM staff time for those working on the project. However, there were several other types of costs associated with the partnership, including consultant payments to the clergy co-chairs, food for Steering Committee meetings and all other partnership meetings, and small incentive payments for attending Steering Committee meetings and participation in the ExpertLens process. In addition, grant funding was used to provide incentive payments to congregations that participated in the intervention pilot, food and financial incentives for church members that participated in the intervention pilot, and stipends for community data collectors, some of whom were from partnership churches.
RESULTS
Description of Partner Churches
A total of 66 churches completed a CIF; most (>90%) of these were completed by the pastor or associate minister; the rest were completed by health ministry coordinators or other church staff. There were 41 predominantly (≥ 60%) African American and 21 predominantly Latino congregations in the partnership (2 congregations reported mixed composition and 2 did not report race-ethnicity of congregants; see Table 2 for characteristics by predominant race-ethnicity of the congregation). African American congregations tended to have a smaller average size than the Latino churches, although the variability was greater among the Latino churches, with several very large Catholic congregations and the rest small Protestant congregations. Because on average Latino churches were much larger, the total number of people associated with the 21 Latino churches (over 20,505) was larger than the total number associated with the 41 African American churches (16,109). Among the Latino churches, most congregants were reported to speak Spanish as their primary language.
Table 2.
Characteristics of partnership churches by predominant race-ethnicity of congregants (n=62)
| Congregational Characteristic | African American Churches (n = 41) Mean or % (SD) | Latino Churches (n = 21) Mean or % (SD) | p-value |
|---|---|---|---|
| Congregation size and reach | |||
| Total number of persons associated with congregation | 402.7 (841.1) | 1025.8 (1949.5) | 0.1851 |
| Total number of persons who attend congregation at least monthly | 243.0 (97.3) | 498.1 (160.8) | 0.1598 |
| Total number of persons associated with partner congregations | 16,109 | 20,515 | |
| Race-ethnicity of regular congregants (%) | |||
| African American | 89.7 (12.3) | 28.0 (30.8) | 0.0003 |
| Latino | 8.4 (8.7) | 89.5 (16.4) | <.0001 |
| Other | 6.8 (8.2) | 6.3 (5.3) | 0.9023 |
| Primary language of regular congregants (%) | |||
| English | 96.5 (5.9) | 39.6 (28.8) | <.0001 |
| Spanish | 6.9 (5.4) | 71.5 (24.8) | <.0001 |
| Other | 5.0 (5.8) | -- | -- |
| Gender of regular congregants (%) | |||
| Female | 67.2 (13.7) | 61.7 (6.8) | 0.0364 |
| Male | 32.9 (13.6) | 38.3 (6.8) | 0.0392 |
| Age of regular congregants (%) | |||
| < 18 years old | 16.1 (10.0) | 26.9 (16.3) | 0.0103 |
| 18–40 years old | 25.2 (16.0) | 27.2 (14.2) | 0.6299 |
| 41–64 years old | 31.1 (16.7) | 29.3 (14.8) | 0.6850 |
| 65 years or older | 28.8 (21.6) | 14.1 (13.0) | 0.0027 |
| Education of regular adult congregants (%) | |||
| ≤ 6th grade | 14.9 (18.5) | 24.0 (20.3) | 0.1518 |
| Completed 7-11th grade | 17.6 (20.0) | 23.9 (18.6) | 0.2889 |
| Completed high school or GED | 45.8 (22.7) | 40.8 (18.4) | 0.4333 |
| Attended or completed college | 35.8 (27.9) | 18.9 (18.4) | 0.0237 |
| Regular congregants with annual incomes <$45,000 (%) | 58.5 (27.6) | 75.5 (21.1) | 0.0182 |
| Staffing (mean) | |||
| Number of full-time, paid staff | 1.8 (1.3) | 4.2 (5.4) | 0.1520 |
| Number of part-time, paid staff | 3.2 (2.0) | 3.5 (2.8) | 0.7066 |
| Number of volunteer staff | 12.8 (19.0) | 16.8 (30.9) | 0.6321 |
| Health programming (%) | |||
| Has health ministry, committee, or group | 48.8 | 28.6 | 0.1312 |
| Involved in health-related activities (past 3 yrs) | 80.5 | 52.4 | 0.0208 |
| Most common health programs (%) | |||
| 1. Diabetes | 46.3 | 42.9 | 0.7982 |
| 2. Cancer | 53.7 | 19.1 | 0.0084 |
| 3. High blood pressure | 43.9 | 28.6 | 0.2479 |
| 4. Nutrition | 36.6 | 42.9 | 0.6380 |
In addition to race-ethnicity and language, there were several other differences between African American and Latino churches in our partnership. African American churches tended to have a higher proportion of regular congregants who were female, 65 years or older, and attended or completed college than Latino churches. Latino churches tended to have a higher proportion of congregants who were <18 years old and low-income (<$45,000 annual household income). African American churches were more likely to report having implemented health programs in the past 3 years, though among the top 4 types of programs across all churches, only cancer programs were more common among African American churches than Latino (similar proportions of each had implemented diabetes, high blood pressure, and nutrition programs).
Partner Interviews about Church-based Obesity Programs
Among the 66 congregations completing a CIF, 31 (47%) indicated that they had done some prior health programming around obesity and/or related issues (high blood pressure, heart disease, stroke prevention, nutrition or exercise). Of the 31, we successfully completed 17 (55%) telephone screener interviews with the pastor or church designee to obtain more detailed information about these activities to select a purposive sample for qualitative interviews. We selected 12 congregations for semi-structured interviews to learn more about their obesity-related programming. We completed semi-structured interviews with 10 (83%) of these churches, of which 4 were Latino Catholic, 2 were Latino Protestant, 1 was a mixed Latino and African American Protestant, and 3 were African American Protestant. Seven informants held clergy roles (pastor, deacon, etc.), while 3 were lay staff members.
In terms of why congregations get involved in addressing obesity, diabetes and related issues, most interviewees said they had observed the need for this in their congregation and/or community. Some also shared personal struggles with a related health condition. All also mentioned that their efforts aligned with congregational priorities to pursue a holistic approach to well-being, which included spiritual, physical, and mental health.
Common health activities in congregations consisted of a combination of recurring and special events such as cooking classes, nutrition classes, encouragement from the pulpit, and health fairs and screenings. Overall education and awareness raising regarding the importance of healthy eating were common goals. Most informants said that the content usually did not include a spiritual component per se. However, clergy and lay leaders were involved in helping implement the activities across all sites – external collaborators mostly provided in-kind and financial support. Congregations did report getting outside assistance for professional services such as screenings. Volunteers were also critical for implementation, and participation by specific church groups and ministries was noted as important for consistency.
Interviewees noted several challenges to implementing church-based health activities. First, some congregants may feel that funds directed towards health activities are being taken from the spiritual mission. Second, getting people to attend activities that are not adjacent to normally scheduled church services can be difficult, especially if congregants live far from the church. Finally, lack of consistent resources for health programming was cited as a consistent problem, as was maintaining interest and participation, given the number of activities already being conducted in and by congregations.
Factors that facilitate church-based health programs were also noted. An internal champion helps push the program forward and consistency in activities and scheduling can help build a critical mass of participants. Clergy support as well as promotion by the church and church members through announcements and word of mouth are important. Further, some sort of financial support is often needed, for example, funds to pay a physical activity instructor.
In terms of church culture and food, respondents described how food is integral to church life, and that some churches are already looking to serve healthier food. But it is important to develop specific policies and engage the culinary group (or those who prepare congregational meals). Respondents also indicated that overall there has been less of a focus on physical activity in church-based programs. Concerns about personal safety and lack of time were identified as the biggest barriers to being active in urban environments.
Intervention Development and Components
Parallel to our partner interviews, we also conducted monthly meetings over 4-5 months with an ad-hoc Intervention Development Working Group involving the RAND-LAM research team and approximately 12-15 community partners. All partnership members were welcomed to participate; however, we also did outreach to faith and public health members with experience doing faith-based obesity programs. In these meetings, we reviewed components of prior church-based obesity interventions and established through consensus the principles and potential activities for our intervention. Further, we discussed the pathways through which our intervention would help create a health promoting environment at the church.
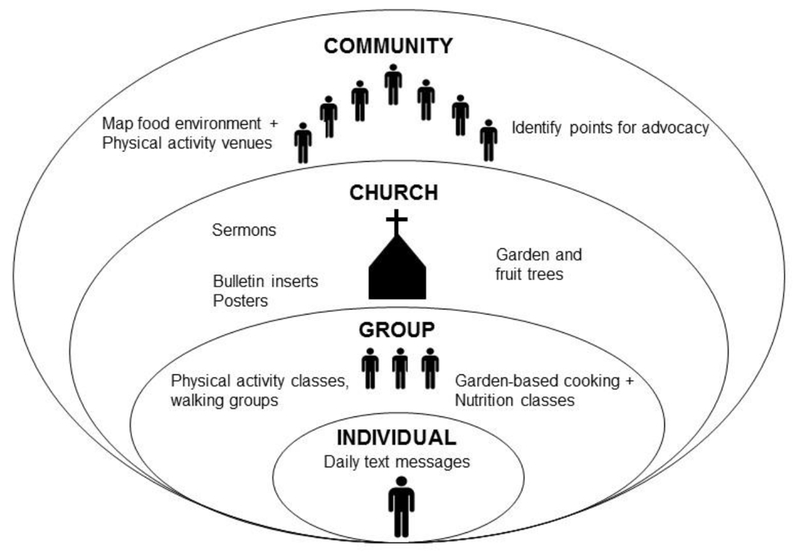
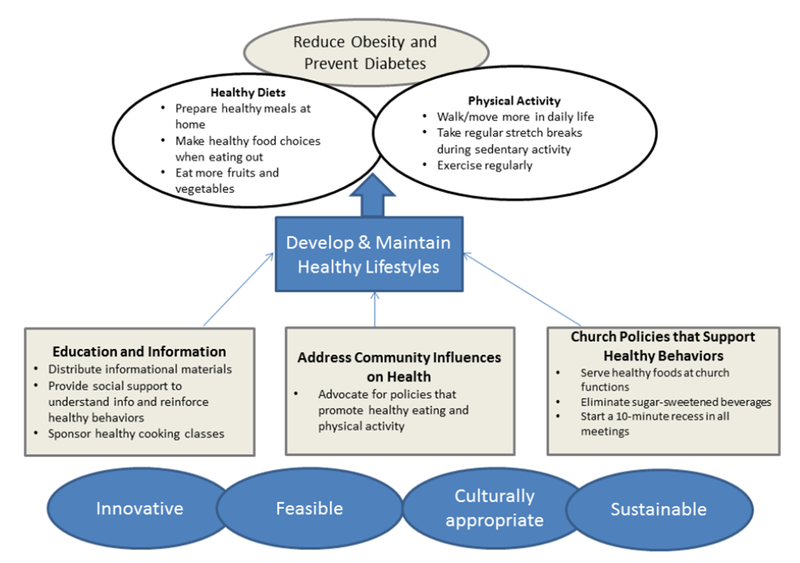
Figure 1 provides an overview of the framework that emerged from this Working Group. Underlying the framework are the principles guiding our intervention – i.e., that it be innovative (e.g., offering something new over previous church-based interventions), feasible, culturally appropriate, and sustainable. We also identified three pathways through which our intervention would influence dietary and physical activity behaviors of congregants: 1) education and information; 2) church policies that support healthy behaviors; and 3) addressing community influences on health (in the surrounding community).
Figure 1:
Partnership-developed Framework for Developing Church-based Obesity Prevention Programs
The framework then guided the identification of specific intervention components and activities, considering the underlying principles and partner resources. Figure 2 outlines the four levels of the socio-ecological framework targeted by our intervention and within each level identifies examples of activities. The only activity that was truly at the individual level was a texting/emailing component by which participants received daily health living tips aimed to reinforce the messages being transmitted in group activities and church-wide activities. The planned group activities included garden-based cooking and nutrition classes and physical activity classes based on participant preference (e.g., Zumba, yoga, walking groups). The planned church-wide activities included sermons on the importance of healthy eating and physical activity, bulletin inserts and posters, vegetable garden and fruit trees, and implementing church policies about food and physical activity (e.g., offering healthier options at congregation events, implementing regular, brief movement breaks into congregational meetings). But for longer term and broader community change, our intervention also had a community mapping component, whereby local food and physical activity resources were systematically assessed and then discussed with congregational leaders and members to then develop advocacy around issues of most concern to the congregation. After developing the intervention, we selected 6 congregations from the partnership (2 large Latino Catholic congregations and 4 small-to-mid-sized African American Protestant congregations) matched in 3 pairs and randomly assigned churches to intervention and wait-list control to pilot test the intervention.
Figure 2:
Intervention components at various levels of the socio-ecological framework
DISCUSSION
We found it feasible to recruit congregations to participate in a multi-ethnic faith and public health research partnership aimed at reducing health disparities more broadly. To our knowledge, ours is the first broader research partnership to report substantial involvement by both African American and Latino congregations from the outset. In describing the development of the Bronx Health REACH Coalition, Kaplan et al. noted early concerns about the initiative being identified with African American churches and the coalition’s realization that, to change this, addressing Spanish language needs were critical [42, 39]. Our team included a bilingual Latino faith organizer and bilingual project manager from the start (plus two of the 4 main investigators on the project are bilingual). Still, we also faced challenges in getting all types of congregations represented. For example, we have Latino Catholic churches (of which all are large as is common in Los Angeles), but among the Latino Protestant, we only have small congregations, even though there are some large mega churches. Similarly, we do not have any very large African American congregations. Some of this may be because the project’s main community partner, LAM, has historically focused on organizing networks among small and mid-sized African American churches. Further, our extensive experience in Los Angeles suggests that there are challenges in recruiting larger “mega” churches, both African American and Latino, to health initiatives given the demand that these organizations face in serving their large congregations and the difficulty of reaching congregational decision makers.
In addition to the lack of representation by the very large (mega) Protestant Latino and African American churches, the diversity among our partner congregations – in terms of denomination, size, and socio-demographics of members – made it challenging to engage them. For example, we had to conduct some of our broader partnership meetings in English and Spanish. Educational status varied widely – from less than high school to college and professional – and thus comfort level with on-line vs. in-person communication and research procedures. Our Community Steering Committee members played key roles in convening stakeholders from their networks for the consensus-building process and it worked well to have them host group lunch meetings (paid for by the grant). The two part-time faith organizers from LAM (one African American and one bilingual Latino) provided one-one-one follow-up and were essential to our success in recruiting over 60 congregations. Engaging that number of congregations required a variety of strategies – small and large group in-person group meetings and email/on-line interactions.
Diversity notwithstanding, we did find some common themes – both in the previous health initiatives implemented by these congregations as well as their ideas for the intervention we developed collaboratively. First, obesity was a common concern among all congregations, as evidenced by the results of our consensus-building process and the fact that just under half the congregations indicated that they had done some prior health programming around obesity and/or related issues. Although we considered prioritizing other, less addressed health issues, we decided to focus on obesity because interest was high for addressing this issue and most church-based programs have not implemented activities across the socio-ecological framework. Second, there were approaches that could work across a range of congregational types, such as community gardens and cooking classes and working with culinary committees to implement environmental changes. Church-wide and church environmental strategies were considered a key element, as in the evidence-based intervention known as Body & Soul [43]. In addition, pastoral influence was also emphasized, as has been identified by multiple faith-based health initiatives [39, 44–46].
Our intervention had several more novel aspects. First, a physical activity component was included since fewer faith-based interventions addressing obesity have included both dietary and physical activity components [47–51]. However, partner churches did have variability in terms of having available space for group classes. Second, a texting / email messaging component was included because community partners wanted this technological innovation used and we found only one published article of a church-based intervention using it (in a prostate cancer intervention among African American men) [52]. Community mapping was included given the importance of socio-ecological approaches and that few church-based studies have explicitly addressed the broader community environment [53, 54].
We must emphasize the nature of our funding, a community planning grant from NIMHD, which allowed us to fully implement a CBPR approach. This funding enabled our sustained outreach and partnership recruitment process that resulted in a diverse set of congregations and public health partners and allowed us to conduct an extended partnership- and consensus-building process to select the priority health issue and co-design a multi-level church-based intervention to address it. And we should note that our community partner (LAM) and several of the team’s investigators had worked previously with faith communities and public health organizations in South Los Angeles, so we were not starting from scratch. Our hope was that this partnership infrastructure (LAM, African American and Latino congregations, public health organizations, and RAND researchers) could support multiple CBPR initiatives, i.e., not just the initially-defined obesity focus. To fully implement and sustain CBPR initiatives, sustained funding through long-term infrastructure grants and institutional support are likely needed. The CDC-funded Prevention Research Centers are one example of these types of long-term infrastructure funding [55]. Other types of non-research funding from local foundations and health systems can help community partners supplement and sustain their involvement. Therefore, one focus of the partnership should be on developing a diverse set of funding sources that can support research and non-research community health initiatives.
Faith and public health partnerships to address health disparities hold great promise and multiethnic and multidenominational or multi-faith initiatives are becoming increasingly important in today’s diverse urban societies. Rather than building such partnerships separately for each CBPR research initiative or health topic, developing a partnership that can serve as infrastructure for multiple research initiatives is ideal and can help improve efficiencies since the added cost of doing CBPR can be substantial [56]. However, such approaches require funding for the community relationship-building and planning processes. Diverse partnerships need additional human capital resources to engage a broad range of partners. Starting with the issue of most concern to the community partners and learning from their past work in this area can help garner enthusiasm, build on existing assets, and result in a culturally- and contextually-appropriate intervention.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
This study was supported by the National Institute of Minority Health and Health Disparities of the National Institutes of Health under Award Number R24MD007943 (PI: Derose). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The Authors acknowledge the important role played the LAM Faith Organizers, Rev. Jawane Hilton and Rev. Juan Sarmiento, in recruiting churches to the partnership, and the broad and sustained contributions of other members of the Community Steering Committee, especially Rev. Rosalynn Brooks, Rev. John Cager, Rev. Walter Contreras, Jaime Huerta, Rev. Martin Garcia, Dr. Jan King, Rev. Felipe Martinez, Bp. Gwendolyn Stone, Nina Vaccaro, and Bp. Craig Worsham.
COMPLIANCE WITH ETHICAL STANDARDS
The study was approved by the RAND Human Subjects Projection Committee. Informed consent was obtained from all individual participants included in the study.
Contributor Information
Kathryn P. Derose, RAND, 1776 Main St, Santa Monica, CA 90401, Tel: (310) 393-0411, ext. 6302, derose@rand.org.
Malcolm V. Williams, RAND.
Cheryl Branch, Los Angeles Metropolitan Churches.
Karen R. Flórez, CUNY Graduate School in Public Health and Health Policy.
Jennifer Hawes-Dawson, RAND.
Michael A. Mata, Azusa Pacific Seminary.
Clyde W. Oden, Bethel AME Church.
Eunice C. Wong, RAND.
REFERENCES
- 1.Frieden TR. Foreword. CDC Health Disparities and Inequalities Report - United States, 2013. MMWR Morb Mortal Wkly Rep 2013;62(Suppl 3): 1–2. [PubMed] [Google Scholar]
- 2.Gu A, Yue Y, Desai RP, Argulian E. Racial and ethnic differences in antihypertensive medication use and blood pressure control among US adults with hypertension: The National Health and Nutrition Examination Survey, 2003 to 2012. Circ Cardiovas Qual Outcomes. 2017; 10(1). doi: 10.1161/circoutcomes.116.003166. [DOI] [PubMed] [Google Scholar]
- 3.Spanakis EK, Golden SH. Race/ethnic difference in diabetes and diabetic complications. Curr Diab Rep. 2013;13(6):814–23. doi: 10.1007/sl1892-013-0421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zonderman AB, Ejiogu N, Norbeck J, Evans MK. The influence of health disparities on targeting cancer prevention efforts. Am J Prev Med. 2014;46(3 Suppl l):S87–97. doi: 10.1016/j.amepre.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jackson CS, Oman M, Patel AM, Vega KJ. Health disparities in colorectal cancer among racial and ethnic minorities in the United States. J Gastrointest Oncol. 2016;7(Suppl 1):S32–43. doi: 10.3978/j.issn.2078-6891.2015.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Keefe EB, Meltzer JP, Bethea TN. Health disparities and cancer: racial disparities in cancer mortality in the United States, 2000–2010. Front Public Health. 2015;3:51. doi: 10.3389/fpubh.2015.00051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harper SB, Lynch J. Selected comparisons of measures of health disparities: a review using databases relevant to healthy people 2010 cancer-related objectives. US Department of Health and Human Services, National Institutes of Health, National Cancer Institute: Department of Epidemiology B, and Occupational Health; 2007. [Google Scholar]
- 8.Gant Z, Dailey A, Hu X, Johnson AS. HIV care outcomes among Hispanics or Latinos with diagnosed HIV infection - United States, 2015. MMWR Morb Mortal Wkly Rep 2017;66(40): 1065–72. doi: 10.15585/mmwr.mm6640a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong RJ, Chou C, Ahmed A. Long term trends and racial/ethnic disparities in the prevalence of obesity. J Community Health 2014;39(6):1150–60. doi: 10.1007/sl0900-014-9870-6. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality. 2010. National healthcare quality and disparities reports. Rockville, MD: http://archive.ahrq.gov/research/findings/nhqrdr/nhqrdr10/qrdr10.html. Accessed March 11 2018. [Google Scholar]
- 11.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured - Findings from a national sample. Med Care. 2002;40(l):52–9. [DOI] [PubMed] [Google Scholar]
- 12.Institute of Medicine (US). Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 13.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA. 2015;314(4):366–74. doi: 10.1001/jama.2015.8421. [DOI] [PubMed] [Google Scholar]
- 14.Cooper-Patrick L, Gallo J, Gonzales J, Vu H, Powe N, Nelson C et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–9. [DOI] [PubMed] [Google Scholar]
- 15.Doescher M, Saver B, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000;9(10):1156–63. [DOI] [PubMed] [Google Scholar]
- 16.Boardman JD, Saint Onge JM, Rogers RG, Denney JT. Race differentials in obesity: the impact of place. J Health Soc Behav. 2005;46(3):229–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kawachi I Income inequality and health In: Berkman LF, Kawachi I, editors. Social Epidemiology. Oxford: Oxford University Press; 2000. [Google Scholar]
- 18.Kawachi I, Kennedy BP. Socioeconomic determinants of health: health and social cohesion: why care about income inequality? BMJ. 1997;314(7086):1037–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willard R, Shah GH, Leep C, Ku L. Impact of the 2008-2010 economic recession on local health departments. J Public Health Manag Pract. 2012;18(2):106–14. doi: 10.1097/PHH.0b013e3182461cf2. [DOI] [PubMed] [Google Scholar]
- 20.Wholey DR, Gregg W, Moscovice I. Public health systems: a social networks perspective. Health Serv Res. 2009;44(5 Pt 2):1842–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barnes PA, Curtis AB. A national examination of partnerships among local health departments and faith communities in the United States. J Public Health Manag Pract. 2009;15(3):253–63. [DOI] [PubMed] [Google Scholar]
- 22.Chaves M Congregations in America. Cambridge, MA: Harvard University Press; 2004. [Google Scholar]
- 23.Idler EL, Musick MA, Ellison CG. Measuring multiple dimensions of religion and spirituality for health research: conceptual background and findings from the 1998 General Social Survey. Res Aging. 2003;25(4):327–65. [Google Scholar]
- 24.Pew Research Center. Religious Landscape Study. Washington, DC: 2014. http://www.pewforum.org/religious-landscape-study/. Accessed February 27 2018. [Google Scholar]
- 25.Taylor RJ, Mattis J, Chatters LM. Subjective religiosity among African Americans: a synthesis of findings from five national samples. J Black Psychol. 1999;25(4):524–43. doi: 10.1177/0095798499025004004. [DOI] [Google Scholar]
- 26.National Congregations Study. Religious Congregations in the 21st Century America 2015. http://www.soc.duke.edu/natcong/Docs/NCSIII_report_final.pdf. Accessed April 17 2018.
- 27.Chaves M, Anderson SL. Continuity and change in American congregations: introducing the second wave of the National Congregations Study. Sociol Relig 2008;69(4):415–40. [Google Scholar]
- 28.Chaves M, Tsitsos W. Congregations and social services: what they do, how they do it, and with whom. Nonprofit Volunt Sect Q. 2001;30(4):660–83. doi: 10.1177/0899764001304003. [DOI] [Google Scholar]
- 29.Williams MV, Haas A, Griffin BA, Fulton BR, Kanouse DE, Bogart LM et al. Predictors of the existence of congregational HIV programs: similarities and differences compared with other health programs. Am J Health Promot. 2015;29(6):e225–35. doi: 10.4278/ajhp.130531-QUAN-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor RJ, Chatters LM. Black and White differences in religious participation: a multisample comparison. J Sci Study Relig. 1996;35(4):403–10. [Google Scholar]
- 31.Anderson RN. Deaths: leading causes for 2000. Natl Vital Stat Rep 2002;50(16). [PubMed] [Google Scholar]
- 32.Lasater TM, Becker DM, Hill MN, Gans KM. Synthesis of findings and issues from religious-based cardiovascular disease prevention trials. Ann Epidemiol 1997;7(S7):S546–S53. [Google Scholar]
- 33.DeHaven MJ, Hunter IB, Wilder L, Walton JW, Berry J. Health programs in faith-based organizations: are they effective? Am J Public Health. 2004;94(6):1030–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–34. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- 35.Goldmon M, Roberson JT Jr., Carey T, Godley P, Howard DL, Boyd C et al. The data collection/data distribution center: building a sustainable African-American church-based research network. Prog Community Health Partnersh. 2008;2(3). [DOI] [PubMed] [Google Scholar]
- 36.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health,. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 37.Cadge W, Ecklund E. Religious service attendance among immigrants: evidence from the new immigrant survey-pilot. Am Behav Sci. 2006;49(11):1574. [Google Scholar]
- 38.De Marco M, Weiner B, Meade SA, Hadley M, Boyd C, Goldmon M et al. Assessing the readiness of black churches to engage in health disparities research. J Natl Med Assoc 2011;103(9-10):960–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaplan SA, Ruddock C, Golub M, Davis J, Foley R Sr., Devia C et al. Stirring up the mud: using a community-based participatory approach to address health disparities through a faith-based initiative. J Health Care Poor Underserved. 2009;20(4):1111–23. doi: 10.1353/hpu.0.0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sallis JE, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J. An ecological approach to creating active living communities. Annu Rev Public Health. 2006;27:297–322. doi: 10.1146/annurev.publhealth.27.021405.102100. [DOI] [PubMed] [Google Scholar]
- 41.Dalal S, Khodyakov D, Srinivasan R, Straus S, Adams J. ExpertLens: a system for eliciting opinions from a large pool of non-collocated experts with diverse knowledge. Technol Forecast Soc Change. 2011;78(8):1426–44. doi: 10.1016/j.techfore.2011.03.021. [DOI] [Google Scholar]
- 42.Kaplan SA, Calman NS, Golub M, Ruddock C, Billings J. The role of faith-based institutions in addressing health disparities: a case study of an initiative in the Southwest Bronx. J Health Care Poor Underserved. 2006;17(2 Suppl):9–19. doi: 10.1353/hpu.2006.0088. [DOI] [PubMed] [Google Scholar]
- 43.Resnicow K, Campbell M, Carr C, McCarty F, Wang T, Periasamy S et al. Body and soul: a dietary intervention conducted through African-American churches. Am J Prev Med. 2004;27(2):97–105. doi: 10.1016/j.amepre.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 44.Campbell MK, Resnicow K, Carr C, Wang T, Williams A. Process evaluation of an effective church-based diet intervention: body & soul. Health Educ Behav. 2007;34(6):864–80. doi: 10.1177/1090198106292020. [DOI] [PubMed] [Google Scholar]
- 45.Derose KP, Mendel PJ, Palar K, Kanouse DE, Bluthenthal RN, Castaneda LW et al. Religious congregations’ involvement in HIV: a case study approach. AIDS Behav. 2011;15(6):1220–32. doi: 10.1007/s10461-010-9827-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Payan DD, Florez KR, Bogart LM, Kanouse DE, Mata MA, Oden CW et al. Promoting health from the pulpit: a process evaluation of HIV sermons to reduce HIV stigma and promote testing in African American and Latino churches. J Health Commun 2017:1–10. doi: 10.1080/10410236.2017.1384352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Resnicow K, Taylor R, Baskin M, McCarty F. Results of Go Girls: a weight control program for overweight African-American adolescent females. Obes Res Clin Pract. 2005;13(10):1739–48. doi: 10.1038/oby.2005.212. [DOI] [PubMed] [Google Scholar]
- 48.Resnicow K, Jackson A, Blissett D, Wang T, McCarty F, Rahotep S et al. Results of the healthy body healthy spirit trial. Health Psychol 2005;24(4):339–48. doi: 10.1037/0278-6133.24.4.339. [DOI] [PubMed] [Google Scholar]
- 49.Samuel-Hodge CD, Keyserling TC, Park S, Johnston LF, Gizlice Z, Bangdiwala SI. A randomized trial of a church-based diabetes self-management program for African Americans with type 2 diabetes. Diabetes Educ 2009;35(3):439–54. doi: 10.1177/0145721709333270. [DOI] [PubMed] [Google Scholar]
- 50.Winett RA, Anderson ES, Wojcik JR, Winett SG, Bowden T. Guide to health: nutrition and physical activity outcomes of a group-randomized trial of an Internet-based intervention in churches. Ann Behav Med. 2007;33(3):251–61. doi: 10.1080/08836610701358045. [DOI] [PubMed] [Google Scholar]
- 51.Wilcox S, Parrott A, Baruth M, Laken M, Condrasky M, Saunders R et al. The faith, activity, and nutrition program: a randomized controlled trial in African-American churches. Am J Prev Med. 2013;44(2):122–31. doi: 10.1016/j.amepre.2012.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Le D, Holt CL, Saunders DR, Wang MQ, Coriolan A, Savoy AD et al. Feasibility and acceptability of SMS text messaging in a prostate cancer educational intervention for African American men. Health Informatics J. 2016;22(4):932–47. doi: 10.1177/1460458215598636. [DOI] [PubMed] [Google Scholar]
- 53.Campbell MK, Motsinger BM, Ingram A, Jewell D, Makarushka C, Beatty B et al. The North Carolina Black Churches United for better health project: intervention and process evaluation. Health Educ Behav 2000;27(2):241–53. [DOI] [PubMed] [Google Scholar]
- 54.Campbell MK, Demark-Wahnefried W, Symons M, Kalsbeek WD, Dodds J, Cowan A et al. Fruit and vegetable consumption and prevention of cancer: the Black Churches United for Better Health project. Am J Public Health. 1999;89(9):1390–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.White-Cooper S, Lewis EY, Greene-Moton E, Grunbaum JA, Gray B. Community engagement in prevention research: The Centers for Disease Control and Prevention’s Prevention Research Centers’ National Community Committee. Prog Community Health Partnersh. 2009;3(1):73–81. doi: 10.1353/cpr.0.0047. [DOI] [PubMed] [Google Scholar]
- 56.Hoeft TJ, Burke W, Hopkins SE, Charles W, Trinidad SB, James RD et al. Building partnerships in community-based participatory research: budgetary and other cost considerations. Health Promot Practice 2014;15(2):263–70. doi: 10.1177/1524839913485962. [DOI] [PMC free article] [PubMed] [Google Scholar]