Abstract
Background:
Proximal hamstring avulsions cause considerable morbidity. Operative repair results in improved pain, function, and patient satisfaction; however, outcomes remain variable.
Purpose:
To evaluate the predictors of clinical outcomes after proximal hamstring repair.
Study Design:
Case series; Level of evidence, 4.
Methods:
We retrospectively reviewed proximal hamstring avulsions repaired between January 2014 and June 2017 with at least 1-year follow-up. Independent variables included patient demographics, medical comorbidities, tear characteristics, and repair technique. Primary outcome measures were the Single Assessment Numerical Evaluation (SANE), International Hip Outcome Tool–12 (iHOT-12), and Kerlan-Jobe Orthopaedic Clinic (KJOC) Athletic Hip score. Secondary outcome measures included satisfaction, visual analog scale for pain, Tegner score, and timing of return to sports.
Results:
Of 102 proximal hamstring repairs, 86 were eligible, 58 were enrolled and analyzed (67%), and patient-reported outcomes were available for 45 (52%), with a mean 29-month follow-up. The mean patient age was 51 years, and 57% were female. Acute tears accounted for 66%; 78% were complete avulsions. Open repair was performed on 90%. Overall satisfaction was 94%, although runners were less satisfied compared with other athletes (P = .029). A majority of patients (88%) returned to sports by 7.6 months, on average, with 72% returning at the same level. Runners returned at 6.3 months, on average, but to the same level 50% of the time and at a decreased number of miles per week compared to nonrunners (15.7 vs 7.8, respectively; P < .001). Postoperatively, 78% had good/excellent SANE Activity scores, but the mean Tegner score decreased (from 5.5 to 5.1). Acute tears had higher SANE Activity scores. The mean iHOT-12 and KJOC scores were 99 and 77, respectively. Endoscopic repairs had equivalent outcome scores to open repairs, although conclusions were limited given the small number of patients in the endoscopic group. Greater satisfaction was noted in patients older than 50 years (P = .024), although they were less likely to return to running (P = .010).
Conclusion:
Overall, patient satisfaction and functionality were high. With the numbers available, we were unable to detect any significant differences in functional outcome scores based on patient age, sex, body mass index, smoking status, medical comorbidities, tear grade, activity level, or open versus endoscopic technique. Acute tears had better SANE Activity scores. Runners should be cautioned that they may be unable to return to the same preinjury activity level after proximal hamstring repair.
Clinical Relevance:
When counseling patients with proximal hamstring tears, runners and those with chronic tears should set appropriate expectations.
Keywords: proximal, hamstring, repair, running
Proximal hamstring avulsions cause considerable morbidity.6,16 The nonoperative treatment of complete tears often results in intractable pain, atrophy, and weakness.6,18 Therefore, a surgical intervention is often recommended in athletic populations.
Operative repair of proximal hamstring avulsions has variable outcomes. Multiple studies have demonstrated improved strength and endurance, with a low risk of reruptures.18,19 Functionally, 76% to 100% of patients eventually return to sports, 55% to 100% return to their preinjury activity level, and 88% to 100% of patients are satisfied with surgical outcomes.1–3,5,7,18,19
There are limited data on who is most likely to have a favorable outcome after hamstring repair. While several studies have shown that repair of acute avulsions results in improved outcomes compared with chronic injuries, others have found no difference.3,11,17,19 There is also disagreement on how partial tears addressed surgically fare compared with complete tears.1,3 To our knowledge, there is minimal evidence regarding other predictors of successful treatment, including age, medical comorbidities, preoperative activity levels, and surgical technique.
The purpose of this study was to evaluate the predictors of clinical outcomes after proximal hamstring repair. The primary outcome measures were patient-reported functional scores. Secondary outcome measures included satisfaction, return to running or sports, and level of participation. We hypothesized superior outcomes for acute injuries, complete avulsions, patients younger than 50 years, and athletes of low-impact sports. We also hypothesized that endoscopic repair would have comparable outcomes with open repair based on the few patients available.
Methods
This was a retrospective review of data collected on proximal hamstring repairs performed at our institution between January 2014 and June 2017. This study was approved and monitored by our institutional review board.
Participants
All patients undergoing proximal hamstring repair during the study period were identified from a surgical database. Patients were included if they were diagnosed with a complete or partial proximal hamstring avulsion and had at least 12 months of follow-up. Patients were excluded if they were skeletally immature, had an avulsion fracture, had a previously repaired hamstring injury, required allograft reconstruction, or had subsequent extremity injuries or surgery (knee ligament, meniscectomy, etc).
Patients who met the inclusion criteria signed consent forms, were enrolled, and were sent an email with a link to complete an online survey via Google Forms. For those who did not respond after 1 month, a reminder telephone call was made, and a paper survey was mailed. One month later, we sent a subsequent email, and a second telephone call was made.
Patient demographics and medical comorbidities were obtained from the medical record. Clinical data including tear acuity, previous treatments, and return to running and sports were obtained from operative, physical therapy, and physician progress notes. Patient-reported outcome surveys included the Single Assessment Numerical Evaluation (SANE), visual analog scale for pain (VAS; 0-10), International Hip Outcome Tool–1210 (iHOT-12; 0-120), Kerlan-Jobe Orthopaedic Clinic (KJOC) Athletic Hip score14 (0-100), and overall satisfaction (1-5). Additional data collected at follow-up included preinjury and postinjury sports/activity levels (Tegner score) and complications. A SANE score of 90-100 was considered excellent, 75-89 good, 50-74 fair, and <50 poor. Tears were identified as partial (grade 2) or complete (grade 3) based on magnetic resonance imaging and were confirmed at the time of surgery. Surgical technique, acuity, and amount of tendon retraction were recorded. The surgical technique was based on the surgeon’s preference and was dictated in part by patient habitus, chronicity of the tear, and amount of retraction. Acute repair was classified as surgery within 6 weeks after the injury.
Surgical Procedure
Open Repair
In the prone position, an 8-cm horizontal incision was made in the gluteal crease. Cautious subcutaneous dissection was carried out to identify and protect the posterior femoral cutaneous nerve. The inferior gluteus maximus musculature was identified and then retracted superior and lateral. The sciatic nerve was identified, neurolysed, and protected throughout the case. Next, the hamstring sheath was identified and incised longitudinally, revealing the invested hamstring tendons. Characterization of the tear was noted. The ischial tuberosity was defined, bursectomy was performed, and the bone was then roughened with a Cobb elevator and rongeur. A double-loaded 2.3-mm Iconix (Stryker) or 4.5-mm PEEK Corkscrew (Arthrex) suture anchor was placed in the oblique lateral facet of the ischial tuberosity. A modified Krackow suture was then applied to the proximal hamstring tendons, and a tension-slide technique was used to bring the tendon down to the bone. Sufficiency of the repair was evaluated, and a second or third anchor was applied as needed. The suture ends were then placed through a 4.75-mm SwiveLock (Arthrex) and set proximally to complete double-row repair. Next, the wound was closed in layers, followed by the application of dressing.
Endoscopic Repair 9
In the prone position, a 4-cm incision was made in the gluteal crease. A 30° arthroscope was placed into the space between the gluteus maximus and the ischial tuberosity. Next, an accessory portal was placed, and a shaver was utilized to perform ischial bursectomy. The sciatic nerve was identified, neurolysed, and protected. The torn proximal hamstring tendons were identified and debrided. Once the ischial tuberosity was clearly defined, a 4-mm bur was utilized to prepare the bone. Next, 1 or 2 suture anchors, as described above, were placed under direct visualization (Figure 1). A suture-passing device was used to place the suture through the proximal hamstring tendons in a mattress fashion. The tension-slide technique was applied to bring the tendons down to the bone, and an arthroscopic knot was tied. A lateral-row SwiveLock anchor was placed, as described above. The wound was then closed and dressing applied.
Figure 1.
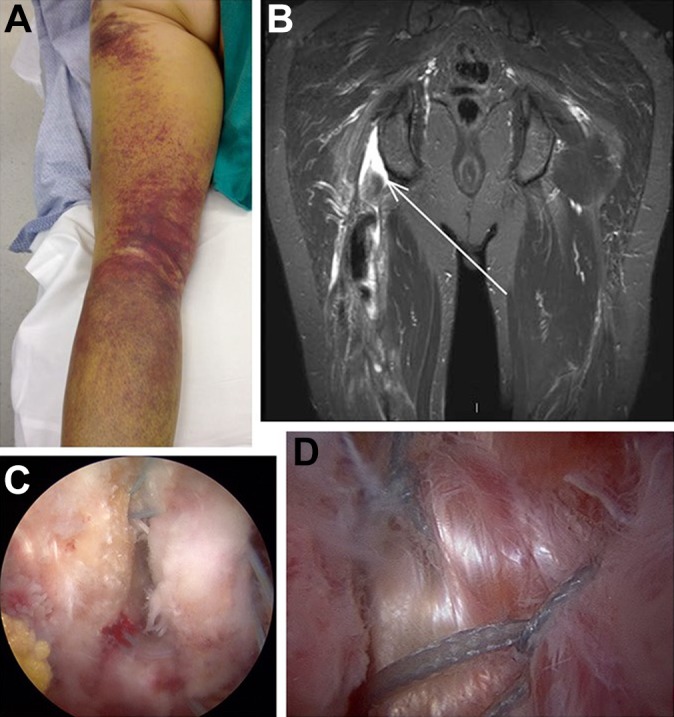
(A) Clinical presentation of a proximal hamstring tear. (B) Coronal magnetic resonance imaging demonstrating a complete avulsion. (C) Endoscopic view of suture anchor placement in the anatomic footprint on the ischium with sutures passed through the tendon. (D) Final repair construct after reduction.
Postoperative Care
For both open and endoscopic procedures, patients were initially restricted to partial weightbearing with crutches for 6 weeks, followed by unrestricted weightbearing, stretching, and closed chain exercises for the next 6 weeks. There was no limitation placed on range of motion. At 3 months, unrestricted strengthening was permitted, with gradual resumption of running, followed by sports or usual activities as strength improved.
Statistical Analysis
Descriptive statistics were performed using Excel (Microsoft). A sample size of 34 total patients was predicted using an alpha of 0.05, a beta of 0.20, and an effect size and standard deviation of 0.10 based on a previous study.3 Response data were analyzed using a nonparametric Pearson chi-square test for nominal categories (sex, race, acuity, grade, and technique). Pearson correlation and regression modeling were used to determine the relationship between the independent variables and outcome scores, VAS scores, time to return to running or sports, and level of activity. A multivariate model was employed to control for the endoscopic technique.
Results
A total of 102 hamstring repairs were performed by the senior authors (M.B.B., M.B.G.) during the study period. Sixteen patients were excluded: 2 underwent revision surgery for retears, 2 underwent allograft reconstruction, 5 underwent subsequent unrelated knee surgery during the follow-up, and 7 declined participation. There were 86 patients eligible for participation. Of these, 28 patients were unable to be reached or did not provide consent. Thus, 58 patients (67%) were enrolled; patient-reported outcomes were available for 45 patients (52%). The mean follow-up was 29 months (range, 12-48 months).
The mean patient age was 51 years (range, 17-77 years) (Table 1). Female patients accounted for 57%, and the mean body mass index (BMI) was 25 kg/m2. Eight patients attempted physical therapy before surgery, and 8 patients tried a platelet-rich plasma injection initially. Two patients had a contralateral proximal hamstring tear previously. The most common mechanism of injury was a fall or slip, followed by running; 48% of tears occurred during sports (Table 2).
TABLE 1.
Patient Demographics and Injury Characteristics (N = 58 Patients)a
| Demographics | |
| Age, y | 51.1 ± 12.0 |
| Body mass index, kg/m2 | 25.3 ± 4.4 |
| Sex, n (%) | |
| Male | 25 (43) |
| Female | 33 (57) |
| Surgical technique, n (%) | |
| Open | 52 (90) |
| Endoscopic | 6 (10) |
| Smoker, n (%) | 3 (5) |
| Thyroid disorder, n (%) | 4 (7) |
| Follow-up,b mo | 29.0 ± 9.9 |
| Injury characteristics | |
| Time to surgery,c d | 176 ± 356 |
| Right side, n (%) | 33 (57) |
| Amount of retraction, cm | 3.4 ± 2.7 |
| Tear grade, n (%) | |
| Complete (grade 3) | 45 (78) |
| Partial | 13 (22) |
| Acuity, n (%) | |
| Acute (<6 wk) | 38 (66) |
| Chronic | 20 (34) |
aData are presented as mean ± SD unless otherwise indicated.
bRange was 12 to 48 months.
cMean time to surgery was 20 days for acute injuries and 472 days for chronic injuries.
TABLE 2.
Mechanism of Injury
| Mechanism | n (%) |
|---|---|
| Fall or slip | 21 (36) |
| Sporting activity | 28 (48) |
| Running | 12 (21) |
| Water/snow skiing | 6 (10) |
| Surfing | 4 (7) |
| Lunges/strength training | 3 (5) |
| Other sport | 3 (3) |
| Atraumatic or unknown | 4 (7) |
| Other | 5 (9) |
Overall satisfaction was 94%, and the mean VAS pain score with activity was 1.6 (Table 3). The mean preoperative and postoperative Tegner scores were 5.5 and 5.1, respectively (P < .001). At a mean of 6.3 months, 82% of runners were able to return to running. At a mean of 7.6 months, 88% of patients were able to return to their usual sports or recreational activities, with 72% returning at the same level (n = 42/58). The mean iHOT-12 and KJOC scores were 99 and 77, respectively. There was excellent correlation between the iHOT-12 and KJOC scores (R 2 = 0.581).
TABLE 3.
Functional and Patient-Reported Outcomesa
| Functional outcomes (n = 58) | |
| Tegner scoreb | |
| Preoperative | 5.5 ± 1.0 |
| Postoperative | 5.1 ± 0.9 |
| Returned to running, n (%) | 37/45 (82) |
| Time to return to running, mo | 6.3 ± 3.8 |
| Returned to sports, n (%) | 50/57 (88) |
| Time to return to sports, mo | 7.6 ± 4.5 |
| Returned to same level, n (%) | 42/58 (72) |
| Patient-reported outcomes (n = 45) | |
| Overall satisfaction (1-5) | 4.7 ± 0.7 |
| VAS pain score with activity (0-10) | 1.6 ± 2.2 |
| SANE ADL scorec | |
| Preoperative | 60 ± 35 |
| Postoperative | 97 ± 7 |
| SANE Activity scored | |
| Preoperative | 32 ± 38 |
| Postoperative | 82 ± 24 |
| SANE Activity score, n (%) | |
| 90-100 | 26 (58) |
| 75-89 | 9 (20) |
| 50-74 | 6 (13) |
| <50 | 4 (9) |
| iHOT-12 score | 99 ± 16 |
| KJOC Athletic Hip score | 77 ± 19 |
aData are presented as mean ± SD unless otherwise indicated. ADL, Activities of Daily Living; iHOT-12, International Hip Outcome Tool–12; KJOC, Kerlan-Jobe Orthopaedic Clinic; SANE, Single Assessment Numerical Evaluation; VAS, visual analog scale.
bMean difference between preoperative and postoperative Tegner score = 0.4 (P < .001).
cMean difference between preoperative and postoperative SANE ADL score = 29.0 (P < .001).
dMean difference between preoperative and postoperative SANE Activity score = 39.4 (P < .001).
The median SANE Activity score postoperatively was 90, and 78% of patients reported good or excellent results. The SANE Activities of Daily Living and SANE Activity scores improved a mean of 29 and 39 points, respectively, from baseline (P < .001). Patients with excellent SANE Activity scores (≥90) were more likely to have acute tears (P = .037). Patients with SANE Activity scores <90 took longer to return to running (8.4 vs 5.0 months, respectively; P = .029) and sports (10.6 vs 5.8 months, respectively; P = .002), had more pain with activity (VAS score of 3.0 vs 0.6, respectively; P < .001), and had lower overall satisfaction (4.3 vs 4.9, respectively; P = .014) compared with those with SANE scores ≥90.
Age
For patients older than 50 years, there was significantly higher overall satisfaction compared with those aged ≥50 years (4.9 vs 4.3, respectively; P = .024). Those older than 50 years were less likely to return to running (P = .010); otherwise, there were no other functional differences related to age.
Acuity
Acute tears accounted for 66% of all tears. The mean time to surgery was 20 days for acute injuries and 472 days for chronic injuries. Chronic tears were more likely to be partial tears (P = .020), to occur more often in female patients (P = .044) and in patients with a lower weight and BMI (P = .010), and to occur less often during sports (P = .005). Patients with chronic tears more often had SANE Activity scores <90 (P = .037); otherwise, there were no significant differences in patient-reported outcomes or return to sports between acute and chronic repairs.
Grade
Complete (grade 3) tears were present in 78%. Partial tears were more likely to be chronic (P = .020), treated with physical therapy or platelet-rich plasma injections previously (P = .001), and repaired endoscopically (P = .005). No significant differences in patient-reported outcomes were identified between partial and complete tears.
Surgical Technique
Open repair was performed in 90% of patients. Patients with endoscopic repairs had very similar outcome scores compared with open repair; however, the study was not adequately powered to detect significant differences between these groups. Endoscopic repairs did well in terms of satisfaction, pain, complication rates, and patient-reported functional outcomes. Overall functional results were evaluated with the endoscopic repairs excluded as well as included, and there were no significant differences. With regard to the anchor type across all repairs, we did not observe any differences between all-suture and PEEK anchors in terms of functional outcomes.
Activity
Runners (n = 16) were less satisfied, on average, compared with other athletes (4.3 vs 4.8, respectively; P = .029). Runners returned to running 82% of the time but only returned to the same activity level 50% of the time (preinjury vs postinjury Tegner score of 6.3 vs 5.4, respectively; P < .001). This was significantly less compared with other sports (P = .018). Runners also returned at a lower number of miles per week, on average, compared with other athletes (15.7 vs 7.8, respectively; P < .001). Bicyclists, surfers, and water and snow skiers (n = 17) were able to return to their sports 87% of the time and at the same level of activity 81% of the time.
Comorbid Factors
There were no significant differences in functional outcome scores based on sex, BMI, smoking status, or other medical comorbidities, including thyroid disease, diabetes, or mood disorders.
Complications
The overall complication rate was 15%. One major complication (wound dehiscence requiring surgical debridement) and 8 minor complications were observed, including 3 minor wound infections, 2 complaints of unresolved numbness at the surgical site, and 4 patients reporting continued cramping, pain, or fatigue in the hamstrings, which inhibited activity. There were no reported sciatic nerve injuries postoperatively.
Discussion
To our knowledge, this is the first study to evaluate specifics regarding return to sports after proximal hamstring repair. Our hypothesis that acute tears and low-impact athletes would fare better was confirmed. Alternatively, age and tear grade were not significant factors in functional outcomes.
Multiple series have shown that surgically repaired proximal hamstring avulsions yield better functional results and patient-reported outcome scores and a higher rate of return to preinjury activities than patients treated nonoperatively.1–3,5,7,13,18,19 Bodendorfer et al3 found that satisfaction was much higher among patients treated operatively versus nonoperatively (93% vs 53%, respectively), with higher strength in the surgical group compared with the contralateral extremity (85% vs 64%, respectively).
Our overall findings were consistent with the existing literature.3,5,7,18,19 Patient satisfaction was high at 94%, and over 80% returned to running and sports, albeit at a lower level, on average. Excellent or good SANE Activity scores were reported by 78% postoperatively.
Acuity
In our cohort, acute injuries reported higher SANE Activity scores than chronic injuries. Several systematic reviews have found superior outcomes repairing acute injuries. Sarimo et al17 found better results for repairs performed at an average of 2.4 months compared with 11.7 months. Systematic reviews by Harris et al11 and Bodendorfer et al3 evaluated 300 and 795 hamstring repairs, respectively, and found that acute repairs (<4 weeks) had improved patient satisfaction, outcome scores, strength, and endurance and a higher rate of return to sports. Alternatively, a review by van der Made et al19 found no difference between acute and delayed procedures and attributed this to study selection differences.
Grade
While partial tears can often be managed nonoperatively initially, continued pain and weakness may impair athletic participation. Repair of partial hamstring tears results in good outcomes with a high rate of return to sports,12 although multiple studies have shown that repairs for complete injuries have higher patient-reported outcomes. Bodendorfer et al3 also found higher patient satisfaction and less pain, albeit a higher complication rate, among complete avulsion repairs. However, Barnett et al1 did find that partial tears had statistically better strength and endurance.
Surgical Technique
To our knowledge, no studies have directly compared outcomes between open and endoscopic techniques. Only technique articles have been published thus far without clinical outcomes.8,9 Endoscopic repair was safe and effective in this cohort. Broad, definitive conclusions cannot be made given the limited number of patients, however. Functional outcome scores were calculated both with and without endoscopic repairs. There were no statistical differences, which was expected given the same fixation technique under direct visualization, just through a smaller incision aided with endoscopy. For this reason, endoscopic repairs were included in the overall results.
Various means of fixation including suture anchors, drill tunnels, and unicortical buttons have all been described without clear benefit of one technique over another.4,18,19 We used a double-row technique with multiple suture anchors to re-create the native, broad area of contact between the tendon and the bone.15 Across all repairs, a comparison of implant types, all-suture versus PEEK, did not show any difference in outcomes.
Activity
Runners were overall less satisfied and less likely to return to their preinjury activity level compared with patients involved in other sports. They also returned at a lower number of miles per week, on average. Patients cited continued pain, weakness, cramping, and fatigue as the reason. This is likely because of scarring at the insertion site during healing, followed by high stress during high-impact activities. This effect was most pronounced in patients older than 50 years, as they were less likely to return to running.
Complications
The primary complication after hamstring repair is continued pain, weakness, or difficulty in returning to running or sports. Rerupture rates in the literature are typically low at <1% to 2%, and there were no failures in our cohort.3 In our study, approximately 12% were unable to return to sports, 28% were unable to return at the same level, and 38% reported pain, fatigue, or cramping with activities, although usually mild. While many patients report neurapraxia at the time of injury, with approximately 28% in 1 study,21 iatrogenic damage to the sciatic nerve is less common (<10%). An injury to the posterior femoral cutaneous nerve resulting in numbness to the posterior thigh is relatively common, with up to 20% in some cohorts,20,21 although it typically resolves. In our study, there were no sciatic nerve injuries, and 2 patients complained of unresolved posterior thigh numbness. Because of the location of the wound, healing can be a challenge. In our series, there were 3 patients with wound infections (5%), 1 of which required surgical debridement for dehiscence.
The strengths of this study include the large sample size, prospective collection of data, and use of validated patient-reported outcome measures. While other studies have published on return to activities, our study is the first to describe specifics regarding return to sports. This study has several important limitations. Patient follow-up was 67%, with patient-reported outcomes for only 52% (45 patients). Barnett et al1 evaluated 123 repairs, with functional outcomes reported for 92 patients. A better follow-up would have provided more robust analysis. Although return to running and sports provided an objective measure of functional outcomes, we had no objective measure of strength. A standard rehabilitation protocol was instituted; however, patients occasionally deviated from this and began running on their own as early as 2 months postoperatively. In the analysis, we recommend caution when interpreting data in subgroups that had few numbers (ie, smokers and thyroid disease). Endoscopic versus open repairs should also be cautiously evaluated because the endoscopic group was small and the study was not adequately powered for this analysis. Finally, patients participated in varying sports or activities and at various levels before surgery; thus, limited sport-specific conclusions were drawn from these data.
Conclusion
This is the first study to provide specifics regarding return to sports after proximal hamstring repair. Overall patient satisfaction (94%) and functionality were high. There were no significant differences in functional outcome scores based on age, sex, BMI, smoking status, medical comorbidities, tear grade, activity level, or surgical technique. Acute tears had better SANE Activity scores. Runners returned to their same preinjury level 50% of the time and at half as many miles. Based on the predictors described, patients should be appropriately counseled regarding return to their preinjury activity level after proximal hamstring repair.
Acknowledgment
The authors acknowledge Drew Watanabe for his assistance with data collection and processing.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: E.N.B. has received educational support from Smith & Nephew. N.E.M. has received educational support from Arthrex, Smith & Nephew, and DJO. M.B.G. has received royalties from Arthrex and is a consultant for Arthrex, Medacta, Ferring Pharmaceuticals, and Stryker. M.B.B. is a paid speaker/presenter for Arthrex and is a consultant for Stryker, MAKO Surgical, and Vericel. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Cedars-Sinai Institutional Review Board.
References
- 1. Barnett AJ, Negus JJ, Barton T, Wood DG. Reattachment of the proximal hamstring origin: outcome in patients with partial and complete tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):2130–2135. [DOI] [PubMed] [Google Scholar]
- 2. Birmingham P, Muller M, Wickiewicz T, Cavanaugh J, Rodeo S, Warren R. Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am. 2011;93(19):1819–1826. [DOI] [PubMed] [Google Scholar]
- 3. Bodendorfer BM, Curley AJ, Kotler JA, et al. Outcomes after operative and nonoperative treatment of proximal hamstring avulsions: a systematic review and meta-analysis. Am J Sports Med. 2018;46(11):2798–2808. [DOI] [PubMed] [Google Scholar]
- 4. Cain MT, Jones MC, Reed DN. A novel technique to repair acute and chronic proximal hamstring avulsions. Orthopedics. 2018;41(2):116–119. [DOI] [PubMed] [Google Scholar]
- 5. Chahal J, Bush-Joseph CA, Chow A, et al. Clinical and magnetic resonance imaging outcomes after surgical repair of complete proximal hamstring ruptures: does the tendon heal? Am J Sports Med. 2012;40(10):2325–2330. [DOI] [PubMed] [Google Scholar]
- 6. Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6(4):237–248. [DOI] [PubMed] [Google Scholar]
- 7. Cohen SB, Rangavajjula A, Vyas D, Bradley JP. Functional results and outcomes after repair of proximal hamstring avulsions. Am J Sports Med. 2012;40(9):2092–2098. [DOI] [PubMed] [Google Scholar]
- 8. Dierckman BD, Guanche CA. Endoscopic proximal hamstring repair and ischial bursectomy. Arthrosc Tech. 2012;1(2):e201–e207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Domb BG, Linder D, Sharp KG, Sadik A, Gerhardt MB. Endoscopic repair of proximal hamstring avulsion. Arthrosc Tech. 2013;2(1):e35–e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Griffin DR, Parsons N, Mohtadi NG, Safran MR, Multicenter Arthroscopy of the Hip Outcomes Research Network. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy. 2012;28(5):611–616. [DOI] [PubMed] [Google Scholar]
- 11. Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures: a systematic review. Int J Sports Med. 2011;32(7):490–495. [DOI] [PubMed] [Google Scholar]
- 12. Lempainen L, Sarimo J, Heikkila J, Mattila K, Orava S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med. 2006;40(8):688–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Orava S, Kujala UM. Rupture of the ischial origin of the hamstring muscles. Am J Sports Med. 1995;23(6):702–705. [DOI] [PubMed] [Google Scholar]
- 14. Papaliodis DN, Banffy MB, Limpisvasti O, et al. The development and validation of a subjective assessment tool for the hip in the athletic population. Am J Sports Med. 2017;45(11):2517–2523. [DOI] [PubMed] [Google Scholar]
- 15. Philippon MJ, Ferro FP, Campbell KJ, et al. A qualitative and quantitative analysis of the attachment sites of the proximal hamstrings. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2554–2561. [DOI] [PubMed] [Google Scholar]
- 16. Sallay PI, Friedman RL, Coogan PG, Garrett WE. Hamstring muscle injuries among water skiers: functional outcome and prevention. Am J Sports Med. 1996;24(2):130–136. [DOI] [PubMed] [Google Scholar]
- 17. Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med. 2008;36(6):1110–1115. [DOI] [PubMed] [Google Scholar]
- 18. Shambaugh BC, Olsen JR, Lacerte E, Kellum E, Miller SL. A comparison of nonoperative and operative treatment of complete proximal hamstring ruptures. Orthop J Sports Med. 2017;5(11):2325967117738551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van der Made AD, Reurink G, Gouttebarge V, Tol JL, Kerkhoffs GM. Outcome after surgical repair of proximal hamstring avulsions: a systematic review. Am J Sports Med. 2015;43(11):2841–2851. [DOI] [PubMed] [Google Scholar]
- 20. Wilson TJ, Spinner RJ, Krych AJ. Surgical approach impacts posterior femoral cutaneous nerve outcomes after proximal hamstring repair [published online October 6, 2017]. Clin J Sport Med. doi:10.1097/JSM.0000000000000514 [DOI] [PubMed] [Google Scholar]
- 21. Wilson TJ, Spinner RJ, Mohan R, Gibbs CM, Krych AJ. Sciatic nerve injury after proximal hamstring avulsion and repair. Orthop J Sports Med. 2017;5(7):2325967117713685. [DOI] [PMC free article] [PubMed] [Google Scholar]


