Abstract
Background:
Pectoralis major muscle (PMM) tendon ruptures are becoming more common. Multiple techniques for fixation of the avulsed tendon to its humeral insertion have been described. None of these techniques has been reviewed to compare outcomes in efforts to establish a first-line surgical technique.
Purpose:
To systematically review and analyze the data available in the literature to establish a clinically superior surgical technique and time frame in which surgery should occur.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic literature review was conducted. Only studies reporting the surgical techniques and outcomes of PMM repair were included. Data including patient age, injury mechanism, type and extent of the rupture, time from injury to surgery, surgical technique, outcome including complications, steroid use, location and year of publication, and activity level were extracted from the included studies. Statistical and descriptive analyses were conducted on the available literature.
Results:
Of 259 cases from studies that provided the timing of repair, 72.6% (n = 188) were repaired acutely, while the remaining were repaired more than 8 weeks after the injury. There was no statistical difference found in the outcomes of these repairs. There were 265 cases included in the statistical analysis comparing the outcomes of surgical techniques. The odds of an excellent/good outcome were significantly better for the transosseous suture (TOS) compared with the unicortical button (UCB) technique (odds ratio [OR], 6.28 [95% CI, 1.37-28.75]; P = .018) and also for the suture anchor (SA) compared with the UCB technique (OR, 3.40 [95% CI, 1.06-10.85]; P = .039). The odds of an excellent/good outcome were not significantly different when comparing the TOS, SA, and TOS with trough techniques to one another. The probability of complications was highest with the TOS with trough technique (12.0%), although the odds of having a complication were not statistically significant for any single technique compared with the others.
Conclusion:
The low quality of evidence available limited this review. There were no significant differences observed in the outcomes of PMM repair based on the timing of repair. The TOS and SA techniques had statistically significantly greater odds of resulting in an excellent/good outcome compared with the UCB technique, but 1 study that contributed to this analysis may have statistically skewed the results for the UCB technique. Therefore, all 3 surgical techniques are accepted options, and the best technique is that with which the surgeon is most proficient and comfortable. Comparative research with a greater level of evidence is needed to determine a definitive first-line surgical technique.
Keywords: pectoralis major, muscle, rupture, tendon, repair, surgery
The pectoralis major muscle (PMM) is a large muscle of the upper extremity that functions to adduct, forward flex, and internally rotate the humerus at the glenohumeral joint. The muscle is not considered to be necessary to perform activities of daily living but is utilized in athletics and labor-intensive work to produce maximal force in upper extremity movements.60 It is believed that the anatomy of the PMM tendon places it at risk of injury when the arm is positioned in extension of 30°.55 This is because the inferior fibers of the sternocostal head of the PMM are placed in more tension and are in a mechanically disadvantaged position at this amount of arm extension.41,55,60 This mechanism explains the common pattern of ruptures of the PMM tendon at its insertion at the proximal humerus, starting at the fibers inferiorly and extending superiorly when the muscle is eccentrically loaded in the extended, abducted, and externally rotated positions.
A PMM rupture has historically been a rarely reported injury. Tomčovčík et al77 reported that since the injury was first described in 1822 by Patissier up to December 2010, 447 cases have been reported in the literature. However, of these 447 cases, Tomčovčík et al77 reported that 283 were found to have been described in the literature after the year 2000. Originally described as a work-related injury, the increasing frequency in recent years is most likely related to an increase in athletic activities, especially weight lifting, in the modern population.41 Injuries occur most frequently in men aged 20 to 40 years and commonly occur in athletes who are anabolic steroid users while weight lifting.41,60 The tendon most commonly avulses from its insertion on the proximal humerus in the population younger than 30 years of age, and in those older than 30 years, the injury most often occurs as a rupture at the musculotendinous junction.55
In general, it is accepted that surgically repaired PMM ruptures have better outcomes in terms of strength, function, and cosmesis at the axillary fold.15,68,85 The opinion of the best timing of surgical repair or reconstruction of the tendon has less evidence, and although some literature favors acute surgical treatment of the PMM injury, the evidence is not sufficient to confirm these findings.25,39 Furthermore, there is a wide variety of techniques used in the repair and reconstruction of PMM ruptures. As of now, none of the techniques in the literature has shown biomechanical superiority over the others, although some may be easier or more comfortable for an individual surgeon.25,39 The current recommendation from the literature is that the technique used in the surgical treatment of PMM ruptures should depend on surgeon preference and ability.39 The purpose of this study was to perform a systematic review and meta-analysis of the current available literature to determine the technique with the best comparable clinical outcomes and the time frames in which these techniques may be the most effective.
Methods
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses; www.prisma-statement.org) guidelines were used in the design of this systematic review of the available literature. The PubMed, CINAHL, Scopus, OvidSP, and Cochrane databases were reviewed for English-language human studies published between the inception of the databases and August 2017. The following search terms and variations were used: “pectoralis major” OR “pectoralis major rupture” OR “pectoralis major surgery” OR “pectoralis major avulsion” OR “pectoralis major injury” OR “pectoralis major tendon” OR “pectoralis major muscle” OR “pectoralis major treatment” OR “pectoralis major repair.”
Studies of all levels of evidence that reported the operative techniques and clinical outcomes after PMM repair were included for review. Exclusion criteria included the following: (1) studies not specifying the type of technique and its associated outcome, (2) studies that were not in the English language (1 study written in Portuguese with a detailed abstract in English was included), (3) review articles, and (4) studies that evaluated nonoperative methods of treatment. Studies that were performed on cadaveric specimens or nonhumans as well as biomechanical studies were excluded from the statistical analysis but were reviewed as part of the literature. All abstracts were reviewed by the 2 authors (M.G. and J.E.J.) and evaluated with the aforementioned criteria in mind. The same authors then reviewed the full text of eligible studies to determine final inclusion. Reference lists and citations were cross-referenced for studies that met inclusion criteria but were not found through a direct search of the databases. Data were extracted by the same 2 authors from all the included studies using a standardized data form created at the onset of the study. Inconsistencies between the authors were resolved by a joint review of the content in question.
Classification Criteria
The Tietjen76 classification system is the most commonly recognized and used system to describe the extent and type of a PMM tendon injury. A modified system by Bak et al6 that adds further subclassifications was used in this study. Descriptions of these classifications can be found in Table 1.
TABLE 1.
Bak Classification of Pectoralis Major Muscle Tendon Injuries
| Type | Description |
|---|---|
| I | Sprain or contusion |
| II | Partial tear |
| III | Complete tear |
| A | Sternoclavicular origin |
| B | Muscle belly |
| C | Musculotendinous junction |
| D | Insertion |
| E | Bony avulsion from insertion |
| F | Muscle tendon substance |
The outcomes of procedures were categorized according to the Bak classification system,6 the most commonly used in the literature. The specifics of each classification type (excellent, good, fair, and poor) can be found in Table 2. In studies with outcomes that did not entirely fit the Bak classification, the best judgment was made by the authors as to which category the outcome belonged in based on the description of the measured outcomes in the original study. Of note, some studies reported that a number of good results would have been counted as excellent excluding the consideration of cosmesis.9
TABLE 2.
Bak Classification of Pectoralis Major Muscle Repair
| Outcome | Description |
|---|---|
| Excellent | The patient was pain-free, had full range of motion, had no cosmetic complaints, had symmetrical manual adduction strength or <10% isokinetic strength loss, and had returned to previous activities without restrictions. |
| Good | The patient had only slight functional impairment with slight restrictions in movement or strength, without cosmetic complaints, and with symmetrical manual adduction strength or a <20% isokinetic deficit. |
| Fair | There was an impairment of function that affected return to the desired activity; that is, there was pain or weakness on activity, or the cosmetic result was unsatisfactory. |
| Poor | Significant complications occurred, pain or restricted range of motion persisted, or there were significant cosmetic complaints from scarring or inadequate repair. |
Acute versus chronic repair is an important factor in determining the method of surgical treatment. Chronic injuries may be more difficult to repair and require the use of an autograft or allograft because of adhesions and tendon retraction.25,45 In the studies reviewed, we found different time frames for classifying repairs as acute or chronic; acute repair was classified as <3 weeks,1,15 <6 weeks,20,36,56,85 or <8 weeks.6,9,77 For consistency in this analysis, any repair ≤8 weeks was considered an acute repair.
Surgical Techniques
The type and extent of the rupture partly dictate the type of chosen repair technique. There are multiple variations and combinations of repair techniques to fixate the PMM tendon back to the humerus, but most fall into 1 of 3 general classes: transosseous suture (TOS) through a drill hole or bone tunnel with or without a bone trough, suture anchor (SA), and unicortical or bicortical button (UCB or BCB, respectively).25,60 There are limited reports of barbed bone staples and cancellous screws with spiked washers for fixation.19,27,45,77,86 In some cases, with significant tendon damage or retraction, an allograft or autograft may be used in conjunction with one of the aforementioned fixation techniques.45 Direct suturing of tendon ends has been performed for intratendinous type IIIC tears if there is sufficient healthy tissue attached to the insertion.1,25 Most techniques utilize high-strength nonabsorbable and absorbable sutures placed through the tendon or muscle in a locking configuration using Krackow, Kessler, or Mason-Allen techniques.39,45,56 To allow for the greatest mobilization and relaxation of the torn muscle, general anesthesia is typically preferred.39,45,56 Patients are commonly placed in the beach-chair or supine position and repaired through a deltopectoral or anterior axillary approach.1,25,60,68 The deltopectoral approach is more commonly used because it allows better visualization.39 Descriptions of the 3 general classes of repair follow.
TOS With Bone Trough Technique
The TOS with bone trough technique (Figure 1) involves creating a vertical trough over the insertional footprint of the PMM tendon and then making drill holes lateral to the trough. Sutures are placed in the tendon and then passed into the trough, out of the drill holes, and tied over the bone bridge.25,39,68 This technique is also performed without a bone trough and involves passing sutures through 2 sets of drill holes or bone tunnels.39
Figure 1.
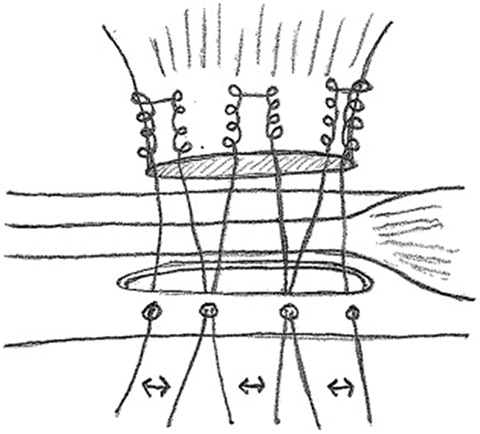
Transosseous suture with bone trough technique: right pectoralis major tendon. (Used with permission from Rabuck et al.63)
SA Technique
The SA technique (Figure 2) involves placing anchors that are preloaded with high-strength nonabsorbable sutures into the humerus over the insertional footprint of the PMM tendon. These sutures are then passed through the tendon to allow for the approximation and fixation of the tendon to its anatomic insertion on the humerus.25,41,45,63
Figure 2.
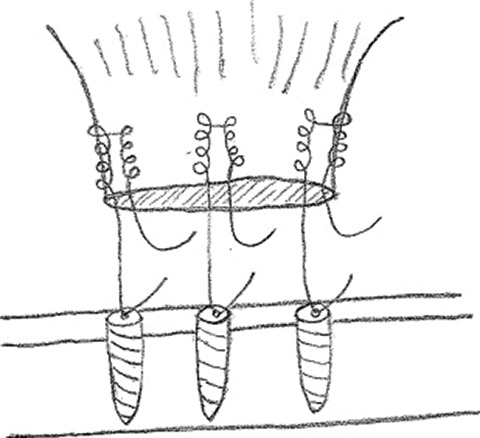
Suture anchor technique: right pectoralis major tendon. (Used with permission from Rabuck et al.63)
Cortical Button Technique
The UCB technique (Figure 3) involves drilling unicortical drill holes in the humerus over the insertional footprint of the PMM tendon. The buttons, preloaded with sutures, are placed through the drill holes, engaging the near cortex. The sutures are then run through the tendon.25,34,45,46,71 A similar technique using bicortical fixation with endobuttons has also been described.59,78
Figure 3.
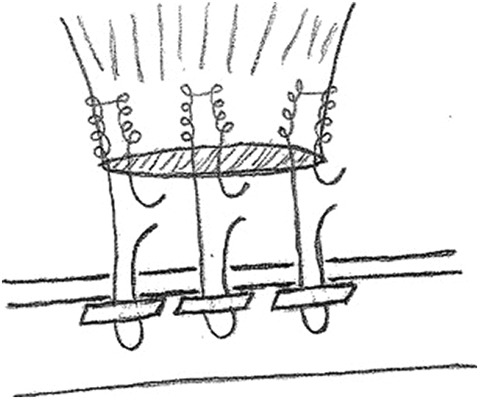
Unicortical button technique: right pectoralis major tendon. (Used with permission from Rabuck et al.63)
Statistical Analysis
Data were analyzed using JMP Pro (version 13.2.1; SAS Institute). Individual patient data from each study were used in a 1-stage approach to produce an overall summary effect of the techniques as an odds ratio (OR).74 Data were categorized as excellent/good or fair/poor based on the outcomes reported in the reviewed studies. This was done because of the low incidence of fair and poor outcomes reported and because of the ambiguity of reporting excellent versus good outcomes in the reviewed studies. Direct suturing of tendon ends was used for type IIIC PMM ruptures and was, with few exceptions, the main technique used to repair this type of tear. However, there is some ambiguity when classifying tears as type IIIC versus type IIID so both injuries were included in the analysis. Because of this and the limited use of some techniques, only the 4 most common surgical techniques (SA, UCB, TOS, and TOS with trough) for humeral fixation of either type IIID or IIIC tears were analyzed by nominal logistic regression for the overall probability and the odds of resulting in an excellent/good outcome. To avoid confounding of the data, all cases that used a variation of one of these most common techniques were not analyzed as part of the technique group corresponding to the common technique. Each technique was compared individually against the other 3 using a nominal logistic model to produce an OR, with an excellent/good outcome as the response of interest. Heterogeneity was assessed and interpreted by calculating the I 2 statistic as described by Higgins and Green.30 The likelihood of having a surgical complication in each of these techniques was evaluated in a similar manner.
The timing of the procedure, whether acute or chronic, was analyzed using chi-square analysis and the Fisher exact test. The probability of each outcome by the timing of the procedure, the odds of an excellent/good outcome, and the OR of acute versus chronic repair were determined using a 2-by-2 contingency table. Significance was set at P < .05.
Results
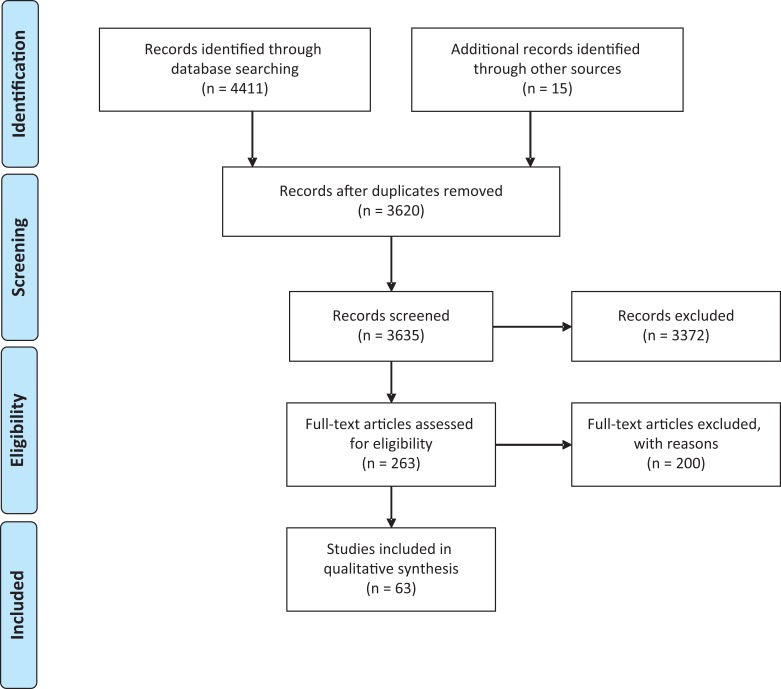
Our initial literature search yielded 4411 articles; after the elimination of duplicates and unrelated articles by an evaluation of titles, 263 full texts were evaluated. After applying our exclusion and inclusion criteria, 63 articles were deemed appropriate for inclusion in this analysis. A flowchart of study selection can be seen in Figure 4.
Figure 4.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of study selection.
The 63 included articles consisted of 1 comparative study,68 2 cohort studies,13,14 18 case series,§ and 42 case reports.∥ The articles comprised a total of 330 occurrences of a PMM tendon rupture that met inclusion criteria. These articles were published between 1941 and 2017 in 19 different locales. The bench press, along with other variations of weight lifting, was responsible for over 70% of the ruptures in articles that addressed the injury mechanism, and 3.6% (n = 12) of articles mentioned anabolic steroid use. All the patients were male, and reported ages ranged from 18 to 74 years, with a mean of 30.4 years and standard deviation of 9.7 years. Patients were professional athletes, amateur athletes, military personnel, and nonathletes. Of the articles that listed the type and extent of the tear, type IIID (75%) was most common, as shown in Table 3. Of the articles that listed head involvement, simultaneous ruptures of both the sternal and clavicular heads occurred 74% of the time and the sternal head only 26% of the time, and there was only 1 case of the clavicular head alone.
TABLE 3.
Incidence of Pectoralis Major Muscle Tendon Ruptures
| Bak Classification Type | Incidence, % |
|---|---|
| I | 0 |
| II | 0 |
| IIIA | 0 |
| IIIB | 1 |
| IIIC | 22 |
| IIID | 75 |
| IIIE | 1 |
| IIIF | <1 |
Of the articles that listed the patient surgical position, 82% mentioned the use of the beach-chair position, 10% the supine position, 4% the semi–beach-chair position, and 4% the semi-Fowler position. Of the articles that listed the surgical approach, a deltopectoral approach was mentioned 78% of the time, and an anterior axillary approach was mentioned in all other articles except 1 study, which mentioned a deltoid splitting approach. Nineteen (30.2%) of the articles reported the suture technique: Krackow technique, 42.1% (n = 8); Kessler technique, 21.1% (n = 4); box suture sliding technique, 5.3% (n = 1); Mason-Allen technique, 10.5% (n = 2); modified Mason-Allen technique, 5.3% (n = 1); interrupted mattress technique, 5.3% (n = 1); horizontal mattress technique, 5.3% (n = 1); and running-locking suture technique, 5.3% (n = 1). Forty-nine of the 330 repairs (15%) required the use of a graft. The types and outcomes are listed in Table 4.
TABLE 4.
Outcomes of Pectoralis Major Muscle Repair Based on Graft Typea
| Excellent/Good | Fair/Poor | Complications | |
|---|---|---|---|
| Semitendinosus/gracilis (n = 37; 76%) | 36 (97.3) | 1 (2.7) | 2 (5.4) |
| Achilles (n = 5; 10%) | 5 (100.0) | 0 (0.0) | 0 (0.0) |
| Tensor fasciae latae (n = 4; 8%) | 4 (100.0) | 0 (0.0) | 0 (0.0) |
| Patellar (n = 2; 4%) | 1 (50.0) | 1 (50.0) | 1 (50.0) |
| Semitendinosus (n = 1; 2%) | 1 (100.0) | 0 (0.0) | 0 (0.0) |
aData are shown as n (%).
Of the 259 cases from articles that listed the timing of repair, 72.6% (n = 188) were repaired acutely, and the remaining were repaired chronically; 169 (89.9%) of the acute repairs had excellent/good outcomes, and 64 of 71 (90.1%) total cases repaired chronically had excellent/good outcomes. The timing of repair was only specified in 12 of 18 complications. There were 9 (4.8%) complications after acute repairs that consisted of pulmonary embolism, biceps tendinitis, a rerupture, revision, persistent pain, transient medial cord plexopathy (n = 2), a keloid scar, and a widened scar. For chronic repairs, there were 3 (4.2%) complications that consisted of a hypertrophic scar, foreign body reaction, and superficial infection. There was no statistical significance found in chi-square analysis (χ2 = 0.003, P = .953) or the Fisher exact test (P = .604) for independence. The odds of an excellent/good outcome after acute repair versus chronic repair were 0.97 (95% CI, 0.39-2.42), which indicated that an excellent/good outcome was almost equally as likely for chronic or acute repair.
The 5 most reported surgical repair techniques were the UCB (n = 82; 24.8%), SA (n = 70; 21.2%), TOS (n = 63; 19.1%), TOS with trough (n = 50; 15.2%), and direct suturing of tendon ends back together (n = 30; 9.1%). The outcomes of these techniques are listed in Table 5. The remaining techniques were variations of the previously listed techniques in addition to other less commonly used techniques. These techniques only accounted for 10.6% (n = 35) of the 330 repairs, and they, along with their outcomes, are listed in Table 5. Of the 330 outcomes, 91.5% (n = 302) were excellent/good, and 8.4% (n = 28) were fair/poor. There were 18 (5.5%) complications after PMM repair, which are listed in Table 5.
TABLE 5.
Outcomes of Pectoralis Major Muscle Repair Based on Techniquea
| Total, n | Excellent/Good, n | Fair/Poor, n | Complications, n (%) | |
|---|---|---|---|---|
| TOS | 63 | 61 (Pr = .97) | 2 (Pr = .03) | 2 (3.2): persistent pain and superficial infection |
| TOS + cortical window | 2 | 2 | 0 | 0 |
| TOS + barbed bone staple | 1 | 1 | 0 | 0 |
| TOS + trough | 50 | 46 (Pr = .92) | 4 (Pr = .08) | 6 (12.0): superficial infection, wound dehiscence, 2 reruptures, paresthesia in third and fourth digits, and hypertrophic scar |
| UCB | 82 | 68 (Pr = .83) | 14 (Pr = .17) | 4 (4.8): pulmonary embolism, biceps tendinitis, reaction to FiberWire, and axillary nerve paresthesia |
| UCB + trough | 1 | 1 | 0 | 0 |
| SA | 70 | 66 (Pr = .94) | 4 (Pr = .06) | 5 (7.1): 2 transient medial cord plexopathies, keloid scar, and 2 reruptures |
| SA + trough | 8 | 8 | 0 | 0 |
| SA + screw and washer | 11 | 10 | 1 | 0 |
| Other | ||||
| Suturing | 30 | 28 | 2 | 0 |
| BCB + trough | 5 | 5 | 0 | 0 |
| BCB + tendon sliding | 1 | 1 | 0 | 0 |
| Screw and washer | 5 | 4 | 1 | 1 (20.0): hypertrophic scar |
| Suturing + mesh | 1 | 1 | 0 | 0 |
aBCB, bicortical button; Pr, probability of achieving the indicated outcome; SA, suture anchor; TOS, transosseous suture; UCB, unicortical button.
Overall, 265 cases were included in the statistical analysis comparing the outcomes of surgical techniques: 70 cases of the SA technique, 63 cases of the TOS technique, 50 cases of the TOS with trough technique, and 82 cases of the UCB technique. The probability of an excellent/good outcome was highest for the TOS technique (Pr = .97), and the probability of a fair/poor outcome was highest for the UCB technique (Pr = .17). The probabilities can be found in Table 5. The odds of an excellent/good outcome were significantly better for the TOS compared with the UCB technique (OR, 6.28 [95% CI, 1.37-28.75]; P = .018) and for the SA compared with the UCB technique (OR, 3.40 [95% CI, 1.06-10.85]; P = .039). The odds of an excellent/good outcome were not significantly different for the TOS compared with the SA technique (OR, 1.85 [95% CI, 0.33-10.45]; P = .49), the TOS compared with the TOS with trough technique (OR, 2.65 [95% CI, 0.47-15.11]; P = .27), the SA compared with the TOS with trough technique (OR, 1.43 [95% CI, 0.34-6.03]; P = .62), or the TOS with trough compared with the UCB technique (OR, 2.37 [95% CI, 0.73-7.65]; P = .15). I 2 was equal to 69.4%, which is consistent with a substantial amount of heterogeneity (50%-90%).30
Discussion
As PMM ruptures have become more common and the number of surgical repairs have increased, various repair techniques have been introduced, however the principles and goals of PMM repair are similar regardless of the technique used. The main goal is to utilize sutures to obtain anatomic reduction of the tendon back to its native footprint while avoiding injuries to the adjacent long head of the biceps and surrounding structures.25,45,60,71 A number of techniques for fixation of the avulsed tendon to its humeral insertion have been described, and the majority of techniques involve some variation of the TOS technique through drill holes or bone tunnels, the SA technique, and the UCB or BCB technique.25,41,45,60 None of these techniques has proven to be superior, and this review aimed to determine the technique with the best clinical outcomes. Additionally, there is debate as to whether outcomes are best when the rupture is repaired acutely or if the rupture can be repaired in a delayed procedure with similar or better outcomes. Thus, we also evaluated the outcomes of surgical cases in the literature based on whether the injury was acute or chronic to determine the best timing for repairing PMM ruptures.
Numerous studies have demonstrated that surgical repair provides the best outcomes in terms of satisfaction, strength, cosmesis, and return to sport, especially in the young and active athlete.¶ Our data support the idea that surgical outcomes are generally very good, with 91.5% of the 330 outcomes resulting in a Bak classification6 of excellent/good. Additional data that were gathered regarding PMM tendon ruptures coincided with the current understanding of the literature. Type IIID tears that involved both sternal and clavicular heads (74%) were the most common type and extent of tears in the results of this review, which is consistent with the types of PMM ruptures that have been reported historically.6,25,45,60,77 Weight lifting, specifically bench-press variations, and contact sports are the most reported causes of PMM tendon ruptures in the literature, and the findings of this review also confirmed this, with contact sports, the bench press, and other variations of weight lifting responsible for over 80% of ruptures.6,45,77 Anabolic steroid use had been listed as a risk factor for PMM ruptures because of the increased muscle strength disproportionate to the strength of the tendon, making it more susceptible to injury.1,6,25,45,56,57 Many of the previously published articles do not formally mention steroid use in patients; in the current review, it was reported in 12 of the 63 included studies. The results of this review showed that patients suffering from PMM ruptures were all male with a mean age of 30.4 years, which agrees with the demographics that have been previously reported in the literature.6,20,25,41,45,77 Table 6 lists details from the included articles.
TABLE 6.
Data From Included Studiesa
| Author (Year) | Study Type (LOE) | No. of Ruptures (Patients) | Patient Age (Mean), y | Activity Level | Injury Type (n) | Head Involvement of Tear (n) | Timing of Repair (n) | Surgical Technique (n) | Outcome (n) | Location of Publication | Complications, n |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Aarimaa et al1 (2004) | CS (4) | 33 (31) | 18-40 (28) | WL, AA, L | IIID (22), IIIC (11) | B/S | A (22), C (11) | TOS (10), SA (12), suturing (11) | E/G (30), F/P (3) | Finland | — |
| Alho2 (1994) | CR (4) | 1 | 28 | WL | IIID | B | C | TOS | E/G | England | — |
| Anbari et al3 (2000) | CR (4) | 1 | 34 | WL | IIID | S | C | TOS + trough | E/G | USA | — |
| Arciero and Cruser5 (1997) | CR (4) | 1 | 20 | WL | IIID | — | A | TOS + trough | E/G | USA | — |
| Bakalim7 (1965) | CR (4) | 1 | 24 | WL | IIID | B | — | TOS | E/G | England | — |
| Berson8 (1979) | CR (4) | 1 | 19 | AA | IIIC | S | A | TOS | E/G | USA | — |
| Cordasco et al9 (2017) | CS (4) | 35 | 23-59 (34.4) | PA, WL, AA | IIID (13), IIIC (22) | B (14), S (21) | A (35) | UCB (35) | E/G (22), F/P (13) | USA | 2: pulmonary embolism, biceps tendinitis |
| De Castro Pochini et al10 (2015) | CR (4) | 1 | 32 | PA | IIIB | — | — | Suturing | E/G | USA | — |
| De Castro Pochini et al11 (2012) | CS (4) | 6 | — (32.7) | WL | IIID/IIIC | B (6) | C (6) | UCB + S/G (6) | E/G (6) | England | 1: foreign body reaction after using FiberWire |
| de Castro Pochini et al12 (2007) | CR (4) | 1 | 30 | PA | IIID | B | A | SA + SW | E/G | England | — |
| de Castro Pochini et al13 (2010) | CH (2) | 10 | 27-47 (32.37) | WL, AA, PA | IIID (8), IIIC (1), IIIB (1) | B (10) | — | SA + SW (7) + S/G (3) | E/G (9), F/P (1) | USA | — |
| de Castro Pochini et al14 (2017) | CH (2) | 27 | — (29.9) | WL, AA | IIID (27) | — | — | UCB + S/G (27) | E/G (26), F/P (1) | Brazil | 1: pain, axillary nerve paresthesia and referred pain |
| Delport and Piper16 (1982) | CR (4) | 1 | 24 | PA | IIID | B | A | TOS | E/G | Germany | — |
| Dempewolf et al17 (2017) | CR (4) | 1 | 22 | PA | IIIC | B | A | UCB | E/G | USA | — |
| Dunkelman et al18 (1994) | CR (4) | 1 | 28 | AA | IIID | B | C | TOS | E/G | USA | — |
| Egan and Hall19 (1987) | CR (4) | 1 | 20 | WL | IIID | B | A | TOS + barbed bone staple | E/G | Canada | — |
| Garrigues et al21 (2012) | CS (4) | 19 (24) | 18-48 (34) | WL, AA, L | IIID (18), IIIC (1) | S (19) | A (17), C (2) | TOS (16), SA (3) | E/G (18), F/P (1) | USA | 5: TOS (persistent pain, superficial infection), SA (keloid, 2 transient medial cord plexopathies) |
| Griffiths and Selesnick23 (1997) | CR (4) | 2 | 42, 25 (33.5) | L, PA | IIID (1), IIIC (1) | B (2) | — | SA (2) | E/G (2) | USA | — |
| Guity et al24 (2014) | CS (4) | 24 (32) | 22-36 (26.9) | WL, AA | IIID (24) | B (24) | A (15), C (9) | TOS + trough (24) | E/G (21), F/P (3) | Asia | 4: superficial infection, wound dehiscence, 2 reruptures |
| Harvey et al28 (2008) | CR (4) | 1 | 34 | — | IIIB | — | C | Suturing + mesh | E/G | USA | — |
| He et al29 (2010) | CS (4) | 9 (12) | 19-54 (32) | WL, AA | IIID (3), IIIC (6) | B (6), S (3) | A (9) | TOS (3), suturing (6) | E/G (8), F/P (1) | China | — |
| Joseph et al31 (2003) | CR (4) | 1 | 21 | WL | IIID | B | A | SA + AC | E/G | USA | — |
| Joshi et al32 (2016) | CS (4) | 11 | 20-30 (25.5) | WL, AA | IIID (11) | B (4), S (7) | A (5), C (6) | SA (11) | E/G (10), F/P (1) | India | — |
| Kakwani et al33 (2007) | CS (4) | 13 | 21-35 (28.6) | WL, AA | IIID (10), IIIF (2), IIIE (1) | B (13) | A (13) | SA (13) | E/G (12), F/P (1) | Germany | 1: rerupture |
| Kang et al34 (2014) | CS (4) | 12 | — | PA, AA | — | — | — | UCB (12) | E/G (12) | USA | — |
| Li et al37 (2007) | CR (4) | 1 | 74 | — | IIID | B | A | SA | E/G | Europe (Amsterdam) | — |
| Mackenzie40 (1981) | CR (4) | 1 | 24 | AA | IIID | B | A | TOS | E/G | South Africa | — |
| Merolla et al43 (2009) | CS (4) | 5 | 23-40 (31) | WL, AA | IIID (5) | B (5) | A (5) | SA (5) | E/G (5) | Italy | — |
| Merolla et al44 (2015) | CS (4) | 12 | 23-45 (34.6) | WL, L, AA | IIID (12) | B (12) | A (8), C (4) | SA (8) + TFL (4) | E/G (12) | France | — |
| Naderi and Funk50 (2009) | CR (4) | 2 (1) | 28 | — | IIID/IIIC | B (2) | C (2) | SA + AC (1), suturing (1) | E/G (2) | UK | — |
| Pavlik et al53 (1998) | CS (4) | 7 | 23-35 (28.2) | WL, AA | IIID (2), IIIC (5) | — | A (6), C (1) | TOS (2), suturing (5) | E/G (7) | Germany | — |
| Pedrazzini et al54 (2017) | CR (4) | 1 | 39 | WL | IIID | B | A | SA | E/G | Italy | — |
| Prabhu et al59 (2017) | CR (4) | 1 | 29 | WL | IIID | B | A | BCB + tendon sliding | E/G | Netherlands | — |
| Quinlan et al62 (2002) | CR (4) | 2 | 25, 24 (24.5) | AA | IIID (2) | B (2) | C (2) | SW (2) | E/G (2) | England | — |
| Salamon et al66 (2015) | CR (4) | 1 | 32 | WL | IIID | B | C | SA + S/G | E/G | Croatia | — |
| Schachter et al67 (2006) | CR (4) | 1 (primary) | 26 | WL | — | — | A | SA | F/P | USA | 1: revision |
| Schachter et al67 (2006) | CR (4) | 1 (revision) | 26 | WL | — | — | C | TOS + trough + S/G | E/G | USA | — |
| Schepsis et al68 (2000) | CS (4) | 13 | 19-37 (29) | WL, AA | IIID/IIIC | — | A (6), C (7) | TOS + trough (13) | E/G (13) | USA | — |
| Scott et al69 (1992) | CR (4) | 1 | — | — | IIID | S | C | TOS | E/G | England | — |
| Shindle et al72 (2007) | CR (4) | 1 | 19 | — | — | S | C | Suturing | E/G | USA | — |
| Verfaillie and Claes81 (1996) | CR (4) | 1 | 45 | AA | IIIE | B | A | SW | E/G | USA | — |
| Vitali et al82 (2016) | CR (4) | 1 | 50 | WL | IIID | CL | C | SA + suturing (CL head to S head) | E/G | Italy | — |
| Warme and Whitaker83 (2004) | CR (4) | 1 | 34 | AA | IIID | S | A | TOS + trough | E/G | USA | — |
| Wheat Hozack et al84 (2013) | CR (4) | 1 | 29 | PA | IIID (S), IIIC (CL) | B | A | UCB | E/G | USA | — |
| Zafra et al86 (2005) | CR (4) | 2 | 20, 20 | WL | IIIC (2) | B (2) | C (2) | SW + P (2) | E/G (1), F/P (1) | Belgium | 1: hypertrophic scar |
| Zvijac et al87 (2011) | CR (4) | 2 (1) | 38 | AA | IIID (2) | B (2) | A (2) | TOS + trough (2) | E/G (2) | USA | — |
| Potter et al58 (2004) | CR (4) | 2 (1) | 40 | AA | IIID (2) | B (2) | C (2) | TOS (2) | E/G (2) | USA | — |
| Rijnberg and van Linge65 (1993) | CR (4) | 1 | 27 | WL | IIIC | B | — | Suturing | E/G | Germany | — |
| Pulaski and Chandlee61 (1941) | CR (4) | 1 | 67 | — | IIIC | B | A | Suturing | E/G | USA | — |
| Kretzler and Richardson36 (1989) | CS (4) | 16 | — (32.5) | WL, AA, L | — | B (15), S (1) | — | TOS (15), suturing (1) | E/G (16) | USA | — |
| Miller et al48 (1993) | CR (4) | 1 | 19 | AA | IIID | B | A | SA | E/G | USA | — |
| Park and Espiniella52 (1970) | CR (4) | 1 | 31 | — | IIIC | B | A | TOS | E/G | USA | — |
| Reut et al64 (1991) | CR (4) | 1 | 31 | WL | IIID | B | A | Suturing | E/G | USA | — |
| Wolfe et al85 (1992) | CS (4) | 7 | 18-43 (30.2) | WL, AA | IIIC (4), IIID (3) | — | A (5 [4 E/G, 1 F/P]), C (2 [2 E/G]) | TOS + trough (7) | E/G (6), F/P (1) | USA | 2: paresthesia in third and fourth digits, widened scar (acute) |
| Orava et al51 (1984) | CS (4) | 5 | 19-38 (27) | — | IIID (4), IIIE (1) | — | A (4), C (1) | TOS (5) | E/G (5) | Germany | — |
| Manjarris et al42 (1985) | CR (4) | 1 | 26 | WL | — | S | — | Suturing | E/G | USA | — |
| Urs and Jani79 (1976) | CR (4) | 1 | 25 | PA | IIID | B | A | TOS | E/G | USA | — |
| Michael et al47 (2013) | CS (4) | 3 | 23-40 (28.7) | WL | IIID (3) | B (3) | C (3) | SA + AC (3) | E/G (3) | USA | — |
| Shepard et al70 (2013) | CR (4) | 1 | 19 | AA | IIIE | B | A | UCB + trough | E/G | USA | — |
| Uchiyama et al78 (2011) | CS (4) | 5 | 23-33 (28.4) | WL, AA | IIID (5) | B (5) | A (5) | BCB + trough (5) | E/G (5) | England | — |
| Valeriote et al80 (2005) | CR (4) | 2 (1) | 22 | WL | IIID (2) | B (2) | C (2) | TOS + cortical window (2) | E/G (2) | USA | — |
| Tomčovčík et al77 (2012) | CR (4) | 1 | 36 | WL | IIID | B | A | SA | E/G | Slovakia | — |
| Moucharafieh49 (2007) | CS (4) | 8 | 24-36 | WL | — | B (8) | A (8) | SA + trough (8) | E/G (8) | Kerala | — |
| Kersch et al35 (1992) | CR (4) | 1 | 30 | AA | IIID | B | A | TOS | E/G | USA | — |
aA, acute; AA, amateur athlete; AC, Achilles graft; B, both; BCB, bicortical button; C, chronic; CH, cohort study; CL, clavicular; CR, case report; CS, case series; E/G, excellent or good; F/P, fair or poor; L, laborer; LOE, level of evidence; P, patellar graft; PA, professional athlete; S, sternal; SA, suture anchor; S/G, semitendinosus/gracilis graft; SW, screw and washer; TFL, tensor fasciae latae graft; TOS, transosseous suture; UCB, unicortical button; WL, weight lifter.
The results of this analysis show that all 4 commonly used fixation techniques are very successful, with each technique having over 80% probability of excellent/good outcomes. Both the TOS (OR, 6.28 [95% CI, 1.37-28.75]; P = .018) and SA (OR, 3.40 [95% CI, 1.06-10.85]; P = .039) techniques had significantly higher odds of an excellent/good outcome compared with the UCB technique. Otherwise, there was no statistical difference in the odds when comparing the outcomes of any single technique against the others.
These data showed that the UCB technique has the poorest outcomes of the 4 techniques. Of note however, 13 of the less favorable outcomes for the UCB technique came from the same case series,9 and only 1 fair/poor outcome was reported otherwise in the remaining 6 publications that reported the use of the UCB technique. Despite the excellent patient satisfaction and functional outcomes, the majority of the 14 patients with the less than favorable outcomes according to Bak classification were in the fair/poor group because of cosmetic concerns related to their incision or their mild chest asymmetry. With cosmesis removed from the scoring system, only 4 of the 14 would remain in the fair/poor group. Also, this study reported 63% of tears as type IIIC, which are commonly repaired with sutures, and humeral fixation in these cases may have been more difficult.9 Regardless of the causes that contributed to less than favorable outcomes for the UCB technique, this study may have misrepresented the true outcomes of this technique. Nonetheless, the TOS technique statistically had the best clinical outcomes, with the highest percentage of combined excellent/good outcomes (96.8%), the lowest percentage of combined fair/poor outcomes (3.2%), and the lowest percentage of complications (3.2%). The predicted probability of an excellent/good outcome with the TOS technique was 97%, which was the highest probability of all 4 common techniques. Statistically, the UCB technique produced the worst clinical outcomes, having the lowest percentage of combined excellent/good outcomes (82.9%) and the highest percentage of combined fair/poor outcomes (17.1%). The predicted probability of an excellent/good outcome was also the lowest based on the data (83%). The TOS with trough technique had the highest percentage of complications (12.0%).
The universally accepted technique of direct suturing of tendon ends for type IIIC tears produced comparable outcomes with respect to the other 4 techniques, but there were only 30 cases that reported this technique. Of these cases, 6.7% reported fair/poor outcomes but no complications, and the combined excellent/good outcomes (93.3%) were similar when compared with the humeral fixation techniques.
There are advantages and disadvantages to each repair technique. An advantage of the TOS with trough technique is that it allows for increased surface area contact of tendon to bone.27 It also has had the most clinical use and is relatively inexpensive compared with the SA and cortical button techniques.27,71 One disadvantage is that the technique requires some tendon trimming, leading to excessive tension, as the tendon is pulled into the trough, particularly in chronic cases or when there is significant tendon retraction.27 Another disadvantage of the TOS technique when it is used with the trough is that the trough likely violates the strongest area of bone in the proximal humerus.27 The biomechanical results of Hart et al27 support this fact, with half of their TOS specimens failing at the trough, while none of the SAs pulled out of the bone. Silverstein et al73 also reported a case of a humeral fracture at the site of the trough with the use of this technique. In addition, the creation of the trough or the use of a bur can lead to damage or weakening of the tendon insertions of the latissimus dorsi and teres major, which are in close proximity to the insertional footprint of the PMM.27 More significant dissection and soft tissue stripping are required to create the trough and drill holes during the TOS technique compared with the SA and UCB techniques.25,39,71 Finally, the TOS technique usually requires a longer procedure time and comes with all the known disadvantages associated with longer surgery.
In contrast, the SA and cortical button techniques usually take less time and require much less dissection and soft tissue stripping.27 Both the SA and cortical button techniques require less insult to the proximal humerus, likely decreasing the risk of humeral fractures. The disadvantages of both techniques are increased costs, potential host reactions to metal or biodegradable materials, and decreased tendon-to-bone contact area.27 Also, although a minor disadvantage, if a metal SA or cortical button is used, it can have a compromising effect on the quality of any further imaging that may be required.71
Recent studies have attempted to determine which repair technique is biomechanically superior.27,63,71,75 In 2011, Hart et al27 found no significant biomechanical difference between the TOS with trough and SA techniques. In 2012, Sherman et al71 compared the TOS, SA, and UCB repair techniques and the intact PMM tendon in cadaveric specimens. Once again, no significant biomechanical differences were seen. In 2015, Thomas et al75 used freshly slaughtered porcine humeri to compare the TOS with trough and UCB techniques. The study concluded that the UCB technique shows parity with the TOS with trough technique, with neither being clearly superior.75 In 2012, Rabuck et al63 compared the TOS with trough, SA, and UCB repair techniques. The TOS with trough technique was found to be the strongest repair technique in their study. However, the authors did state that one of the specimens using this technique sustained a proximal humeral fracture and that other modes of fixation may be preferred to avoid this significant complication. It is noted that Sherman et al71 did not use a bone trough and recorded no failures at the bone bridge in contrast to the other 3 studies,27,63,75 which did have failure in the bone where the trough was made. In summary, all 4 of the described repair techniques are effective at repairing a torn PMM tendon, and one does not appear to be definitively biomechanically superior.
Evaluating the results of this study and the other factors mentioned, the current evidence available, although substantially heterogeneous (I 2 = 69.4%), suggests that the UCB technique is the least likely to produce a favorable outcome based on the Bak classification and that the TOS and SA techniques are the ones that have produced the highest odds of a good/excellent outcome. The TOS with trough technique produced generally favorable outcomes, but the risk of complications is the highest with the use of the trough, although this was not statistically significant. Current evidence suggests that the benefit of the trough may not outweigh the risks associated with its use, especially because the outcomes of the technique without the trough were shown to have slightly higher, although not significant, odds of being excellent/good. Depending on the experience and skill of the surgeon, the TOS, UCB, and SA techniques are all reasonable options for surgical fixation of PMM ruptures based on the current literature available. Because the methodology of this analysis is for exploratory and not confirmatory purposes, there is a significant need for studies with higher levels of evidence to definitively confirm a superior technique.
Some of the literature is controversial when it comes to acute versus chronic repair producing superior outcomes. A number of authors have concluded that outcomes are better when the injury is acutely repaired.# Schepsis et al68 concluded that there was no significant difference in subjective or objective outcomes between patients repaired acutely versus chronically. Other authors have published case reports of excellent/good outcomes after chronic repair.2,26,31,38 As stated previously, this review classified acute repair as one occurring ≤8 weeks from the initial injury. This analysis found no statistical difference in outcomes in repairs that were performed acutely or in a delayed fashion (χ2 = 0.003, P = .953; Fisher exact test, P = .604). The outcomes between acute and chronic repairs were nearly identical, with all categories within 2% of each other, and the odds of an excellent/good outcome were almost the same (OR, 0.97 [95% CI, 0.39-2.42]). Although the outcomes were similar, the literature does show more potential difficulty and opportunity for worse outcomes after chronic repair.
In chronic repair or repair when direct tendon attachment is not plausible because of substantial tendon retraction, damage, or adhesions, the PMM tendon can be reconstructed using an autograft or allograft with various humeral fixation techniques.25,45 There have been multiple studies, some of which are included in our results,** that report the use of a variety of different grafts, which are listed in Table 4. It was difficult to denote a single graft type as superior because the combined excellent/good outcomes for repairs incorporating grafts were ≥96%. Also, other variables such as the humeral fixation technique differed between the grafts; 96% of all repairs that included a graft yielded excellent/good outcomes, with only a 6% (n = 3) complication rate. This was a slightly better rate and was comparable with repairs that did not incorporate a graft.
Limitations
The low level of evidence gathered from case reviews, case series, and case-control studies for most of the data limits the clinical application of the results of this analysis. Ideally, these studies would be blinded randomized controlled trials comparing each technique, but the current analysis reflects the data that are currently available on the topic. Publication bias is a significant limitation in the type of evidence used because there is a high likelihood in these cases that good outcomes are more likely to be reported and published in the literature, thus increasing the number of excellent/good outcomes and decreasing the rate of fair/poor outcomes. This bias alone could reflect better outcomes for one or all the techniques evaluated in this analysis.
The techniques were generalized into 4 classes, but many of the cases that used the same general techniques varied from other cases by minor but significant alterations in the techniques, such as the suture configuration, number of anchors or buttons, and location of drill holes. A biomechanical study of suture techniques performed by Gregory et al22 concluded that suture configuration has a profound effect on repair strength in PMM repair. Sherman et al71 came to the same conclusion in their study. Another limitation that greatly affects outcomes is the postoperative and rehabilitation course that each patient takes, as returning too early to previous activity levels or incomplete rehabilitation could contribute to a poor outcome outside the surgical technique itself. The time to follow-up may also significantly alter outcomes.
The elimination of non–English-language articles and articles lacking outcome specificity was a limitation, as it reduced the number of reported repairs. Articles were included from as early as 1941, and the surgical field has advanced through time, which has the potential to alter relative outcomes. The incidence of this type of injury has significantly increased in more recent years; thus, the majority of surgical cases included are from more recent publications. Cases that did not use the Bak classification system required authorial judgment to classify outcomes according to the Bak system, which was another limitation. Furthermore, the Bak injury classification and outcome classification are the most reported in the literature but still involve some ambiguity and rely on subjective interpretation. There was a substantial amount of heterogeneity (I 2 = 69.4%), which can be contributed to multiple factors already described, including bias, surgeon factors, subtle technique variability, and rehabilitation. Overall, the evidence in this analysis does help with synthesizing current reported results of the techniques commonly used; however, there needs to be comparative research with high levels of evidence to definitively conclude the superiority of one technique over the other as well as the optimal timing for surgical intervention.
Conclusion
Although PMM rupture is becoming more common and is also being studied more extensively, it is still relatively uncommon, with sparse publications discussing the clinical outcomes of specific surgical techniques. The results of this review agreed with most literature to date concerning the injury mechanism, injury type/extent, and age of patients. Our findings indicated that there is no significant difference in the outcomes based on the timing in which PMM repair occurred. The TOS and SA techniques had statistically significantly higher odds of resulting in an excellent/good outcome compared with the UCB technique. Because of the low levels of evidence of the studies reviewed, comparative research with a higher level of evidence needs to be conducted to determine a definitive first-line surgical technique. The most appropriate technique should still be that which the surgeon can perform most proficiently. PMM ruptures in the appropriate patient should be repaired regardless of timing, and the use of a graft is a reasonable option when necessary to facilitate repair.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.E.J. is a contracted writer for ScholarRx. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Aarimaa V, Rantanen J, Heikkila J, Helttula I, Orava S. Rupture of the pectoralis major muscle. Am J Sports Med. 2004;32(5):1256–1262. [DOI] [PubMed] [Google Scholar]
- 2. Alho A. Ruptured pectoralis major tendon: a case report on delayed repair with muscle advancement. Acta Orthop Scand. 1994;65(6):652–653. [DOI] [PubMed] [Google Scholar]
- 3. Anbari A, Kelly JD, 4th, Moyer RA. Delayed repair of a ruptured pectoralis major muscle: a case report. Am J Sports Med. 2000;28(2):254–256. [DOI] [PubMed] [Google Scholar]
- 4. Antosh IJ, Grassbaugh JA, Parada SA, Arrington ED. Pectoralis major tendon repairs in the active-duty population. Am J Orthop (Belle Mead NJ). 2009;38(1):26–30. [PubMed] [Google Scholar]
- 5. Arciero RA, Cruser DL. Pectoralis major rupture with simultaneous anterior dislocation of the shoulder. J Shoulder Elbow Surg. 1997;6(3):318–320. [DOI] [PubMed] [Google Scholar]
- 6. Bak K, Cameron EA, Henderson IJ. Rupture of the pectoralis major: a meta-analysis of 112 cases. Knee Surg Sports Traumatol Arthrosc. 2000;8(2):113–119. [DOI] [PubMed] [Google Scholar]
- 7. Bakalim G. Rupture of the pectoralis major muscle: a case report. Acta Orthop Scand. 1965;36(3):274–279. [DOI] [PubMed] [Google Scholar]
- 8. Berson BL. Surgical repair of pectoralis major rupture in an athlete: case report of an unusual injury in a wrestler. Am J Sports Med. 1979;7(6):348–351. [DOI] [PubMed] [Google Scholar]
- 9. Cordasco FA, Mahony GT, Tsouris N, Degen RM. Pectoralis major tendon tears: functional outcomes and return to sport in a consecutive series of 40 athletes. J Shoulder Elbow Surg. 2017;26(3):458–463. [DOI] [PubMed] [Google Scholar]
- 10. De Castro Pochini A, Andreoli CV, Ejnisman B, Maffulli N. Surgical repair of a rupture of the pectoralis major muscle. BMJ Case Rep. 2015;2015:BCR2013202292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. De Castro Pochini A, Ejnisman B, Andreoli CV, Cohen M. Reconstruction of the pectoralis major tendon using autologous grafting and cortical button attachment: description of the technique. Tech Shoulder Elbow Surg. 2012;13(3):123–127. [Google Scholar]
- 12. de Castro Pochini A, Ejnisman B, Andreoli CV, et al. Exact moment of tendon of pectoralis major muscle rupture captured on video. Br J Sports Med. 2007;41(9):618–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. de Castro Pochini A, Ejnisman B, Andreoli CV, et al. Pectoralis major muscle rupture in athletes: a prospective study. Am J Sports Med. 2010;38(1):92–98. [DOI] [PubMed] [Google Scholar]
- 14. de Castro Pochini A, Rodrigues MSB, Yamashita L, Belangero PS, Andreoli CV, Ejnisman B. Surgical treatment of pectoralis major muscle rupture with adjustable cortical button. Rev Bras Ortop. 2017;53(1):60–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. de CP, Andreoli CV, Belangero PS, et al. Clinical considerations for the surgical treatment of pectoralis major muscle ruptures based on 60 cases: a prospective study and literature review. Am J Sports Med. 2014;42(1):95–102. [DOI] [PubMed] [Google Scholar]
- 16. Delport HP, Piper MS. Pectoralis major rupture in athletes. Arch Orthop Trauma Surg. 1982;100(2):135–137. [DOI] [PubMed] [Google Scholar]
- 17. Dempewolf MJ, Grumet RC, Shepard MF, Kocher K, Munson E, Hostetter G. Pectoralis major tendon rupture in a professional baseball player. Current Orthopaedic Practice. 2017;28(2):235–237. [Google Scholar]
- 18. Dunkelman NR, Collier F, Rook JL, Nagler W, Brennan MJ. Pectoralis major muscle rupture in windsurfing. Arch Phys Med Rehabil. 1994;75(7):819–821. [PubMed] [Google Scholar]
- 19. Egan TM, Hall H. Avulsion of the pectoralis major tendon in a weight lifter: repair using a barbed staple. Can J Surg. 1987;30(6):434–435. [PubMed] [Google Scholar]
- 20. ElMaraghy AW, Devereaux MW. A systematic review and comprehensive classification of pectoralis major tears. J Shoulder Elbow Surg. 2012;21(3):412–422. [DOI] [PubMed] [Google Scholar]
- 21. Garrigues GE, Kraeutler MJ, Gillespie RJ, O’Brien DF, Lazarus MD. Repair of pectoralis major ruptures: single-surgeon case series. Orthopedics. 2012;35(8):e1184–e1190. [DOI] [PubMed] [Google Scholar]
- 22. Gregory JM, Klosterman EL, Thomas JM, et al. Suture technique influences the biomechanical integrity of pectoralis major repairs. Orthopedics. 2015;38(9):e746–e752. [DOI] [PubMed] [Google Scholar]
- 23. Griffiths GP, Selesnick FH. Rupture of the pectoralis major muscle: diagnosis and treatment. Phys Sportsmed. 1997;25(8):118–125. [DOI] [PubMed] [Google Scholar]
- 24. Guity M, Vaziri AS, Shafiei H, Farhoud A. Surgical treatment of pectoralis major tendon rupture (outcome assessment). Asian J Sports Med. 2014;5(2):129–135. [PMC free article] [PubMed] [Google Scholar]
- 25. Haley CA, Zacchilli MA. Pectoralis major injuries: evaluation and treatment. Clin Sports Med. 2014;33(4):739–756. [DOI] [PubMed] [Google Scholar]
- 26. Hanna CM, Glenny AB, Stanley SN, Caughey MA. Pectoralis major tears: comparison of surgical and conservative treatment. Br J Sports Med. 2001;35(3):202–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hart ND, Lindsey DP, McAdams TR. Pectoralis major tendon rupture: a biomechanical analysis of repair techniques. J Orthop Res. 2011;29(11):1783–1787. [DOI] [PubMed] [Google Scholar]
- 28. Harvey KP, Adair JD, Ali MA. Seat belt trauma: pectoralis muscle rupture and delayed mesh repair. J Trauma. 2008;64(3):831–833. [DOI] [PubMed] [Google Scholar]
- 29. He ZM, Ao YF, Wang JQ, Hu YL, Yin Y. Twelve cases of the pectoralis major muscle tendon rupture with surgical treatment: an average of 6.7-year follow-up. Chin Med J (Engl). 2010;123(1):57–60. [PubMed] [Google Scholar]
- 30. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. 2011. Available at: www.handbook.cochrane.org. Accessed January 12, 2018.
- 31. Joseph TA, Defranco MJ, Weiker GG. Delayed repair of a pectoralis major tendon rupture with allograft: a case report. J Shoulder Elbow Surg. 2003;12(1):101–104. [DOI] [PubMed] [Google Scholar]
- 32. Joshi D, Jain JK, Chaudhary D, Singh U, Jain V, Lal A. Outcome of repair of chronic tear of the pectoralis major using corkscrew suture anchors by box suture sliding technique. World J Orthop. 2016;7(10):670–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kakwani RG, Matthews JJ, Kumar KM, Pimpalnerkar A, Mohtadi N. Rupture of the pectoralis major muscle: surgical treatment in athletes. Int Orthop. 2007;31(2):159–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kang RW, Mahony GT, Cordasco FA. Pectoralis major repair with cortical button technique. Arthrosc Tech. 2014;3(1):e73–e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kersch T, Cirillo R, Fay M. Pectoralis tendon rupture in a water skier: a case report. Contemp Orthop. 1992;24:437–441. [Google Scholar]
- 36. Kretzler HH, Jr, Richardson AB. Rupture of the pectoralis major muscle. Am J Sports Med. 1989;17(4):453–458. [DOI] [PubMed] [Google Scholar]
- 37. Li WWL, De Jonge MC, Goslings C, Haverlag R, Ponsen K. Complete avulsion of the pectoralis major tendon: a case report. Eur J Trauma Emerg Surg. 2007;33(5):553–556. [DOI] [PubMed] [Google Scholar]
- 38. Lindenbaum BL. Delayed repair of a ruptured pectoralis major muscle. Clin Orthop Relat Res. 1975;109:120–121. [DOI] [PubMed] [Google Scholar]
- 39. Lipman A, Strauss E. Treatment of pectoralis major muscle ruptures. Bull Hosp Jt Dis (2013). 2016;74(1):63–72. [PubMed] [Google Scholar]
- 40. Mackenzie DB. Avulsion of the insertion of the pectoralis major muscle: a case report. S Afr Med J. 1981;60(4):147–148. [PubMed] [Google Scholar]
- 41. Magnussen RA, Jacobi M, Servien E. Pectoralis major rupture In: Kerkhoff GMMJ, Servien E, eds. Acute Muscle Injuries. New York: Springer; 2014:93–103. [Google Scholar]
- 42. Manjarris J, Gershuni DH, Moitoza J. Rupture of the pectoralis major tendon. J Trauma. 1985;25(8):810–811. [DOI] [PubMed] [Google Scholar]
- 43. Merolla G, Campi F, Paladini P, Porcellini G. Surgical approach to acute pectoralis major tendon rupture. G Chir. 2009;30(1-2):53–57. [PubMed] [Google Scholar]
- 44. Merolla G, Paladini P, Artiaco S, Tos P, Lollino N, Porcellini G. Surgical repair of acute and chronic pectoralis major tendon rupture: clinical and ultrasound outcomes at a mean follow-up of 5 years. Eur J Orthop Surg Traumatol. 2015;25(1):91–98. [DOI] [PubMed] [Google Scholar]
- 45. Merolla G, Paladini P, Campi F, Porcellini G. Pectoralis major tendon rupture: surgical procedures review. Muscles Ligaments Tendons J. 2012;2(2):96–103. [PMC free article] [PubMed] [Google Scholar]
- 46. Metzger PD, Bailey JR, Filler RD, Waltz RA, Provencher MT, Dewing CB. Pectoralis major muscle rupture repair: technique using unicortical buttons. Arthrosc Tech. 2012;1(1):e119–e125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Michael MA, Fowler JT, Owens BD. Allograft reconstruction of chronic pectoralis major tendon ruptures. J Surg Orthop Adv. 2013;22(1):95–102. [DOI] [PubMed] [Google Scholar]
- 48. Miller MD, Johnson DL, Fu FH, Thaete FL, Blanc RO. Rupture of the pectoralis major muscle in a collegiate football player: use of magnetic resonance imaging in early diagnosis. Am J Sports Med. 1993;21(3):475–477. [DOI] [PubMed] [Google Scholar]
- 49. Moucharafieh R. Pectoralis major tendon ruptures: repair using absorbable anchor sutures. J Orthop. 2007;4(4):e9. [Google Scholar]
- 50. Naderi NM, Funk L. Chronic bilateral pectoralis major ruptures and reconstruction with allograft. Injury Extra. 2009;40(12):267–269. [Google Scholar]
- 51. Orava S, Sorasto A, Aalto K, Kvist H. Total rupture of pectoralis major muscle in athletes. Int J Sports Med. 1984;5(5):272–274. [DOI] [PubMed] [Google Scholar]
- 52. Park JY, Espiniella JL. Rupture of pectoralis major muscle: a case report and review of literature. J Bone Joint Surg Am. 1970;52(3):577–581. [PubMed] [Google Scholar]
- 53. Pavlik A, Csepai D, Berkes I. Surgical treatment of pectoralis major rupture in athletes. Knee Surg Sports Traumatol Arthrosc. 1998;6(2):129–133. [DOI] [PubMed] [Google Scholar]
- 54. Pedrazzini A, Banchi M, Bertoni N, et al. Pectoralis major tendon rupture in a weight lifter: a rare case. Acta Biomed. 2017;88(1):86–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Pepe MD, Tucker BS, Basamania C. Pectoralis major repair In: Williams GR, Ramsey ML, Wiesel SW, eds. Operative Techniques in Shoulder and Elbow Surgery. Philadelphia: Wolters Kluwer Health; 2011:247–251. [Google Scholar]
- 56. Petilon J, Carr DR, Sekiya JK, Unger DV. Pectoralis major muscle injuries: evaluation and management. J Am Acad Orthop Surg. 2005;13(1):59–68. [DOI] [PubMed] [Google Scholar]
- 57. Pochini Ade C, Ferretti M, Kawakami EF, et al. Analysis of pectoralis major tendon in weightlifting athletes using ultrasonography and elastography. Einstein (Sao Paulo). 2015;13(4):541–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Potter BK, Lehman RA, Jr, Doukas WC. Simultaneous bilateral rupture of the pectoralis major tendon: a case report. J Bone Joint Surg Am. 2004;86(7):1519–1521. [DOI] [PubMed] [Google Scholar]
- 59. Prabhu J, Faqi MK, Alkhalifa F, Tayara BK, Awad RK. Repair of double head pectoralis major tendon avulsion into its native footprint using bi-cortical EndoButtons and tendon sliding technique. Open Orthop J. 2017;11:12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Provencher MT, Handfield K, Boniquit NT, Reiff SN, Sekiya JK, Romeo AA. Injuries to the pectoralis major muscle: diagnosis and management. Am J Sports Med. 2010;38(8):1693–1705. [DOI] [PubMed] [Google Scholar]
- 61. Pulaski EJ, Chandlee BH. Ruptures of the pectoralis major muscle. Surgery (USA). 1941;10(2):309–312. [Google Scholar]
- 62. Quinlan JF, Molloy M, Hurson BJ. Pectoralis major tendon ruptures: when to operate. Br J Sports Med. 2002;36(3):226–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Rabuck SJ, Lynch JL, Guo X, et al. Biomechanical comparison of 3 methods to repair pectoralis major ruptures. Am J Sports Med. 2012;40(7):1635–1640. [DOI] [PubMed] [Google Scholar]
- 64. Reut RC, Bach BR, Jr, Johnson C. Pectoralis major rupture: diagnosing and treating a weight-training injury. Phys Sportsmed. 1991;19(3):89–95. [Google Scholar]
- 65. Rijnberg WJ, van Linge B. Rupture of the pectoralis major muscle in body-builders. Arch Orthop Trauma Surg. 1993;112(2):104–105. [DOI] [PubMed] [Google Scholar]
- 66. Salamon R, Anić T, Nemec B, et al. Chronic rupture of pectoralis major muscle: a case report. Medicina Fluminensis. 2015;51(1):183–185. [Google Scholar]
- 67. Schachter AK, White BJ, Namkoong S, Sherman O. Revision reconstruction of a pectoralis major tendon rupture using hamstring autograft: a case report. Am J Sports Med. 2006;34(2):295–298. [DOI] [PubMed] [Google Scholar]
- 68. Schepsis AA, Grafe MW, Jones HP, Lemos MJ. Rupture of the pectoralis major muscle: outcome after repair of acute and chronic injuries. Am J Sports Med. 2000;28(1):9–15. [DOI] [PubMed] [Google Scholar]
- 69. Scott BW, Wallace WA, Barton MA. Diagnosis and assessment of pectoralis major rupture by dynamometry. J Bone Joint Surg Br. 1992;74(1):111–113. [DOI] [PubMed] [Google Scholar]
- 70. Shepard NP, Westrick RB, Owens BD, Johnson MR. Bony avulsion injury of the pectoralis major in a 19 year-old male judo athlete: a case report. Int J Sports Phys Ther. 2013;8(6):862–870. [PMC free article] [PubMed] [Google Scholar]
- 71. Sherman SL, Lin EC, Verma NN, et al. Biomechanical analysis of the pectoralis major tendon and comparison of techniques for tendo-osseous repair. Am J Sports Med. 2012;40(8):1887–1894. [DOI] [PubMed] [Google Scholar]
- 72. Shindle MK, Khosravi AH, Cascio BM, Deune EG, McFarland EG. Surgical treatment of a tear of the pectoralis major muscle at its sternal origin: a case report. J Bone Joint Surg Am. 2007;89(9):2040–2043. [DOI] [PubMed] [Google Scholar]
- 73. Silverstein JA, Goldberg B, Wolin P. Proximal humerus shaft fracture after pectoralis major tendon rupture repair. Orthopedics. 2011;34(6):222. [DOI] [PubMed] [Google Scholar]
- 74. Simmonds MC, Higgins JP. A general framework for the use of logistic regression models in meta-analysis. Stat Methods Med Res. 2016;25(6):2858–2877. [DOI] [PubMed] [Google Scholar]
- 75. Thomas W, Gheduzzi S, Packham I. Pectoralis major tendon repair: a biomechanical study of suture button versus transosseous suture techniques. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2617–2623. [DOI] [PubMed] [Google Scholar]
- 76. Tietjen R. Closed injuries of the pectoralis major muscle. J Trauma. 1980;20(3):262–264. [DOI] [PubMed] [Google Scholar]
- 77. Tomčovčík L, Morochovič R, Resutík R. Pectoralis major muscle rupture: more than 440 cases already reported. A review of the recent literature. European Journal of Orthopaedic Surgery & Traumatology. 2012;22(7):603–608. [Google Scholar]
- 78. Uchiyama Y, Miyazaki S, Tamaki T, et al. Clinical results of a surgical technique using endobuttons for complete tendon tear of pectoralis major muscle: report of five cases. Sports Med Arthrosc Rehabil Ther Technol. 2011;3:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Urs ND, Jani DM. Surgical repair of rupture of the pectoralis major muscle: a case report. J Trauma. 1976;16(9):749–750. [DOI] [PubMed] [Google Scholar]
- 80. Valeriote J, Purchase RJ, Kelly JD. Simultaneous bilateral pectoralis major muscle rupture. Am J Orthop (Belle Mead NJ). 2005;34(6):301–302. [PubMed] [Google Scholar]
- 81. Verfaillie SM, Claes T. Bony avulsion of the pectoralis major muscle. J Shoulder Elbow Surg. 1996;5(4):327–329. [DOI] [PubMed] [Google Scholar]
- 82. Vitali M, Naim Rodriguez N, Pedretti A, Saladino A, Fraschini G. Surgical treatment of a rare case of inveterate pectoralis major rupture: a case report. Chirurgia. 2016;29(3):95–98. [Google Scholar]
- 83. Warme WJ, Whitaker DC. Pectoralis major tendon avulsion from rappelling. Mil Med. 2004;169(2):151–154. [DOI] [PubMed] [Google Scholar]
- 84. Wheat Hozack MJ, Bugg B, Lemay K, Reed J; Canadian Pro Rodeo Sport Medicine. Tears of pectoralis major in steer wrestlers: a novel repair technique using the EndoButton. Clin J Sport Med. 2013;23(1):80–82. [DOI] [PubMed] [Google Scholar]
- 85. Wolfe SW, Wickiewicz TL, Cavanaugh JT. Ruptures of the pectoralis major muscle: an anatomic and clinical analysis. Am J Sports Med. 1992;20(5):587–593. [DOI] [PubMed] [Google Scholar]
- 86. Zafra M, Munoz F, Carpintero P. Chronic rupture of the pectoralis major muscle: report of two cases. Acta Orthop Belg. 2005;71(1):107–110. [PubMed] [Google Scholar]
- 87. Zvijac JE, Gampel B, Kiebzak GM. Simultaneous bilateral rupture of the pectoralis major tendons while exercising on the rings. Current Orthopaedic Practice. 2011;22(4):376–378. [Google Scholar]