Abstract
Background:
The medial ulnar collateral ligament (UCL) insertion of the elbow has been shown to extend distally beyond the sublime tubercle. The contribution to valgus stability of the distal aspect of the footprint is unknown.
Purpose/Hypothesis:
The purpose of this study was to determine the contribution of each part of the UCL footprint to the elbow valgus stability provided by the UCL. It was hypothesized that the distal two-thirds of the ulnar UCL footprint would not contribute significantly to valgus stability provided by the UCL.
Study Design:
Descriptive laboratory study.
Methods:
Fifteen cadaveric arms were dissected to the capsuloligamentous elbow structures and potted. A servohydraulic load frame was used to place 5 N·m of valgus stress on the intact elbow at 30°, 60°, 90°, and 120° of flexion. The UCL insertional footprint was measured and divided into thirds (proximal, middle, and distal). One-third of the UCL footprint was elevated off the bone (leaving the ligament in continuity), and the elbow was retested at the same degrees of flexion. This was repeated until the entire UCL footprint on the ulna was sectioned. Each elbow was randomized for how the UCL would be sectioned (sectioning the proximal, then middle, and then distal third or sectioning the distal, then middle, and then proximal third). Ulnohumeral joint gapping (millimeters) was recorded with a 3-dimensional motion capture system using physical and virtual markers. Two-group comparisons were made between each sectioned status versus the intact condition for each flexion angle.
Results:
When the UCL was sectioned from distal to proximal, none of the ligaments failed prior to complete sectioning. When the UCL was sectioned from proximal to distal, 3 of the 6 ligaments failed after sectioning of the proximal third, while 2 more failed after the proximal and middle thirds were sectioned. Of the specimens with the distal third of the ligament sectioned first, no significant differences were found between intact, distal third cut, and distal plus middle thirds cut at all flexion angles.
Conclusion:
The middle and distal thirds of the insertional footprint of the UCL on the ulna did not significantly contribute to gap resistance at 5 N·m of valgus load. The proximal third of the footprint is the primary resistor of valgus load.
Clinical Relevance:
This cadaveric biomechanical study demonstrated that the middle and distal thirds of the native UCL insertion onto the ulna did not significantly contribute to valgus resistance at the elbow. When a UCL reconstruction is performed, the proximal third of the UCL insertion may be the most clinically important portion of the ligament to reconstruct.
Keywords: ulnar collateral ligament (UCL), elbow, valgus, biomechanics, stability, cadaver
The ulnar collateral ligament (UCL) of the elbow has been increasingly studied over the past 10 years because of an increase in the number of UCL injuries sustained by professional and amateur baseball players.6,7,11,12,20,22 The UCL is composed of 2 bundles that cross the ulnohumeral joint, anterior and posterior, and is the primary soft tissue restraint to valgus stress at the elbow.30–32 The anterior bundle, which originates on the anteroinferior aspect of the medial epicondyle and inserts onto the sublime tubercle and UCL ridge of the ulna, has been shown to provide the majority of resistance to valgus stress at the elbow and can be further divided into anterior and posterior bands.5,30,35 These bands function in reciprocal fashion such that the anterior band is taut from 30° to 90° of elbow flexion, whereas the posterior band is taut from 90° to 120°.
The sublime tubercle, onto which the UCL inserts, is approximately 5.5 mm distal to the articular surface (although the most proximal extent of the UCL insertion averages 2.8 mm distal to the articular surface).17 Early studies found that the UCL had a relatively short insertion onto the ulnar sublime tubercle, and because of this, ulnar collateral ligament reconstruction (UCLR) techniques called for placement of a tunnel only a few millimeters distal to the articular surface.13,17,24,34 However, more recent studies have described the UCL ridge, which extends distally beyond the sublime tubercle for approximately 24.5 mm and is the insertion site for the distal-most fibers of the UCL.22 This new anatomic finding raises the question of whether the ulnar fixation point in UCLR should be moved more distally to restore native anatomic and biomechanical features.28 Although significant attention has focused on the ulnar footprint of the UCL, the literature lacks any evaluation of the functional contribution of each part of this ulnar UCL footprint to resistance of valgus stress. No study to date has specifically tested the function of the distal aspect of the UCL footprint to determine how much, if any, this contributes to valgus stability of the elbow. If the distal third of the ulnar UCL footprint contributes a significant amount of resistance to valgus stress, it may mean that the ulnar tunnel for a UCLR should be moved more distal and could explain the unfavorable rates of return to sport (RTS) and failure following UCLR.4,14,18,20,26,28
The purpose of this study was to determine the contribution of the proximal, middle, and distal aspects of the ulnar UCL footprint to valgus stability at the elbow. We hypothesized that the middle and distal thirds of the ulnar insertion of the UCL would not significantly contribute to valgus stability at the elbow and that the proximal third of the footprint would provide the majority of the stability.
Methods
Fifteen fresh-frozen cadaveric upper extremities were used for this study after ethics committee approval was obtained. No pairs of cadaveric arms were used for this study. Each specimen was thawed and carefully dissected in the same manner by a single author (B.J.E.) to reduce the chance of bias as a result of dissection technique. The elbows were thawed for dissection, were refrozen, and then thawed for testing. The average age of the cadavers was 61 years (range, 46-69 years). There were 9 right and 6 left elbows, all from male donors. The upper extremities were dissected down to the capsuloligamentous structures of the elbow (Figure 1). The humerus was cut at 20 cm from the ulnohumeral articulation. The ulna and radius were also cut 20 cm from the ulnohumeral articulation. The ulna and radius were potted into a cylinder cast by use of Bondo filler and resin (3M), and this was repeated for the humerus (Figure 2). Care was taken to keep moist gauze wrapped around the capsuloligamentous elbow structures at all times. The elbows were then refrozen until testing.
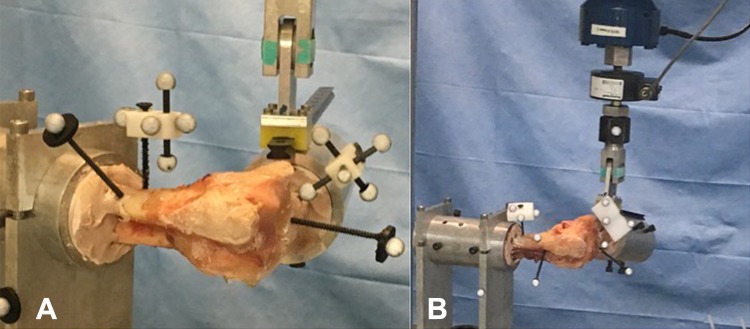
Figure 1.
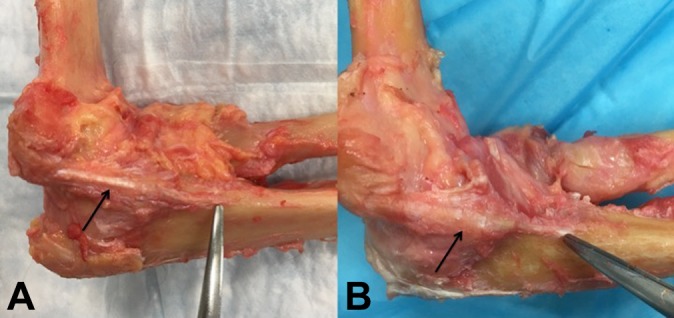
Images demonstrating the ulnar collateral ligament (UCL) in 2 of the cadaveric specimens (black arrows). Notice the distal extent of the UCL footprint on the ulna marked by the tip of the dissecting scissors in both images.
Figure 2.
(A) Image demonstrating the testing setup. (B) Image demonstrating placement of the markers on the cadaver as well as the machine. A valgus force was applied.
Testing
Each elbow was thawed overnight before testing. The specimens were mounted in custom fixtures on a servohydraulic load frame (Figure 2), and the length of the UCL attachment site on the ulna was measured with a digital caliper. This length was measured from the ulnohumeral joint line extending distally (Table 1). One author (B.J.E.) performed all measurements to reduce the risk of bias. Prior to performing these recorded measurements, this author used 3 different prepared cadavers and performed 5 measurements of each UCL insertion length on each of these 3 cadavers to assess intraobserver reliability (intraobserver reliability was >0.9, indicating excellent reliability). The UCL footprint of each cadaveric specimen was measured, and marks were made to delineate the ends of the footprint and the extents of each third (proximal, middle, and distal thirds) (Figure 3). The focus of this study was the proximal to distal attachment site of the UCL. The medial to lateral width and the overall surface area of the attachment did not factor into the decision on where to section the ligament because the ligament tapers as it inserts distally, making it difficult to distinguish between the anterior and posterior bands of the anterior bundle.
TABLE 1.
Measurements of Ulnar Collateral Ligament Length (mm) of 3 Cadaveric Specimens
| Cadaver 1 | Cadaver 2 | Cadaver 3 | |
|---|---|---|---|
| First measurement | 28.3 | 31.5 | 30.9 |
| Second measurement | 28.4 | 31.5 | 30.9 |
| Third measurement | 28.4 | 31.5 | 30.9 |
| Fourth measurement | 28.3 | 31.5 | 30.8 |
| Fifth measurement | 28.4 | 31.5 | 30.8 |
| Average | 28.4 | 31.5 | 30.9 |
| SD | 0.0415 | 0.0158 | 0.0217 |
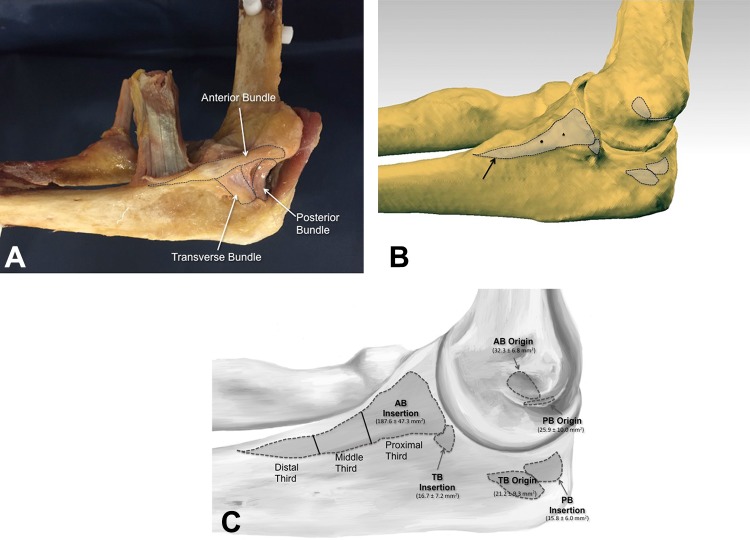
Figure 3.
(A) Image of a previously dissected cadaveric specimen with the ulnar collateral ligament (UCL) insertions of each bundle onto the ulna dotted out. (B) A computer-generated image of the origin and insertion footprints of the UCL. Notice the long insertion of the anterior bundle onto the ulna (black arrow). (C) Computer-generated image showing the insertion areas of the various bundles and how the UCL was divided into proximal, middle, and distal thirds for this study. AB, anterior bundle; PB, posterior bundle; TB, transverse bundle.
Four retroreflective markers were placed on both the radius and the ulna to facilitate 3-dimensional (3D) tracking of the bones with a motion capture camera system (Cortex; Motion Analysis Corp) (Figure 2B). A pointer was used to indicate locations on either side of the joint line. These virtual markers coupled with the physical markers were used to calculate and directly measure medial gapping under valgus stress. A valgus load was then applied to the elbow at 30°, 60°, 90°, and 120° of flexion with an intact UCL at 2 mm/s until a 5-N·m moment was achieved. Load and piston displacement were recorded throughout the test along with the 3D coordinates of all physical and virtual markers. Failure was defined as complete avulsion or rupture of the ligament at any point along its course.
The specimens were randomized to have the UCL sectioned from proximal to distal or from distal to proximal. Starting from the middle was not feasible. Sectioning was performed with a scalpel, releasing the fibers of the ligament from its ulnar insertion in a subperiosteal fashion. When specimens were sectioned from proximal to distal, the proximal third was elevated off of the ulna while the UCL was left intact (thereby removing the attachment of the UCL to bone of the proximal third, but leaving the ligament intact to test the middle and distal thirds). Each elbow was tested in 4 total states: (1) intact, (2) with either the distal or proximal third of the ulnar footprint sectioned, (3) with either the distal or proximal two-thirds of the ulnar footprint sectioned, and (4) with the UCL completely sectioned. In each of these states, the elbow was tested at 30°, 60°, 90°, and 120° of flexion. Continuity of the ligament was assessed after each test. Therefore, each specimen was tested a total of 16 times. The amount of gapping at the ulnohumeral joint against 5 N·m was measured and recorded for each state. A valgus moment of 5 N·m was selected based on previously published study protocols reporting it as a nondestructive moment while generating measurable joint gapping.9,10,33
Statistical Analysis
The data were not distributed normally, and therefore the Friedman repeated-measures analysis of variance on ranks with Student-Newman-Keuls method was used for pairwise comparisons of gap. Statistical significance was set at P < .05.
Results
No significant differences were found in footprint length between the groups of specimens with the distal third cut first (33.4 ± 3.4 mm) versus the group with the proximal third cut first (36.1 ± 2.0 mm) (P = .10). As well, no significant differences of ulnohumeral joint gapping (in millimeters) were found between groups when they were tested with the UCL completely intact or completely resected at any of the tested flexion angles (intact: 30°, P = .86; 60°, P = .09; 90°, P = .61; 120°, P = .82; full resection: 30°, P = .61; 60°, P = .54; 90°, P = .38; 120°, P = .10), indicating that the groups were similar.
Evaluation of the specimens with the proximal third of the ligament insertion sectioned first showed that 50% (3/6 specimens) failed during testing via avulsion of the UCL after the proximal third was cut. Two additional specimens failed after the proximal and middle thirds of the insertional footprint were sectioned. Hence, only 1 specimen with the proximal third sectioned first made it through the testing protocol before failure (complete UCL rupture with no end point on testing) (Table 2).
TABLE 2.
Gapping (mm) of Specimens That Were Sectioned From Proximal to Distala
| One-Third Sectioned | Two-Thirds Sectioned | All Sectioned | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Specimen | 30° | 60° | 90° | 120° | 30° | 60° | 90° | 120° | 30° | 60° | 90° | 120° |
| p1 | 4.4 | 3.6 | 1.1 | 0.3 | 4.7 | 4.1 | 2.4 | 0.5 | 4.9 | 3.7 | 1.2 | 0.7 |
| p2 | 5.3 | 2.3 | 2.8 | 3.1 | 17.7 | 4.4 | 5.3 | 3.5 | 18.7 | 10.2 | 7.9 | 10.4 |
| p3 | 7.3 | 11.4 | 1.7 | 0.6 | 9.6 | 8.2 | 2.2 | 0.7 | 12.7 | 9.2 | 2.5 | 0.6 |
aOf the proximal first specimens, 3 did not have complete tissue rupture (p1, p2, p3), and the changes in gap for these 3 specimens are shown in this table. At 30° of flexion, all 3 specimens exceeded the clinically acceptable gap increase level of 3.5 mm with only the proximal third of the ligament cut. At 60° of flexion, 2 of 3 specimens exceeded 3.5 mm with only the proximal third of the ligament cut.
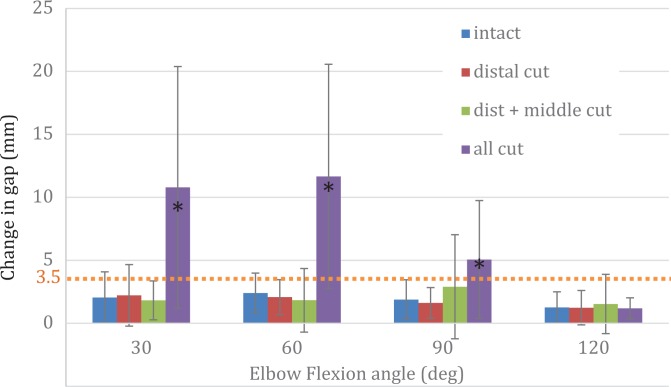
Evaluation of the specimens with the distal third of the ligament sectioned first revealed no significant differences between intact, distal third cut, and distal and middle thirds cut at all flexion angles (Figure 4). Once the proximal third was sectioned, leaving no ligament, gapping significantly increased at 30°, 60°, and 90° of flexion. At 120° of flexion, no significant difference in gapping was seen with any amount of ligament sectioning.
Figure 4.
Changes in gapping for the specimens in which the ulnar collateral ligament was sectioned from distal to proximal. The dotted line represents the clinically acceptable level of gap increase. Error bars indicate standard deviation. *Statistically significant difference compared with the other conditions (P < .05).
Discussion
With the increase in elbow UCL injuries to professional and amateur baseball players, the UCL has become one of the most studied ligaments in the body. Our hypothesis was confirmed, as the majority of resistance to valgus stress was provided by the proximal third of the ulnar UCL footprint, and relatively little resistance was provided by the middle and distal thirds of the ulnar UCL footprint.
The ligamentous anatomic features of the medial elbow have been extensively studied.23,29–32 The primary soft tissue restraints to valgus stress are the flexor-pronator mass (specifically the flexor carpi ulnaris), UCL, and joint capsule.25,29 The UCL is composed of 3 distinct bundles—anterior, posterior, and transverse. The transverse bundle does not cross the ulnohumeral joint and thus is not a valgus stabilizer of the elbow. The anterior and posterior bundles originate at the medial epicondyle, and as the primary restraint against valgus stress through most of the functional flexion angles of the elbow, the anterior bundle inserts at the ulnar sublime tubercle. Although the insertion site was once thought to be relatively small, recent evidence has shown that the insertion of the UCL is broader than previously reported. Farrow et al22 performed a quantitative analysis of the UCL ulnar footprint to determine its relationship to the sublime tubercle of the ulna. The investigators used 10 cadavers and 100 osseous specimens to measure the length of the anterior band of the UCL ulnar attachment as well as the entire ligament length. Using computed tomography scans, the investigators also measured the length of the osseous ridge of the ulna, which extends distally from the sublime tubercle. Farrow et al22 found the average length of the UCL ulnar soft tissue footprint to be 29.2 mm. They also identified an osseous ridge, present in all specimens, with an average length of 24.5 mm that extended distally from the sublime tubercle to the medial aspect of the ulnar insertion of the brachialis muscle tendon. This was the first study to report the extended ulnar attachment of the UCL.
More recently, Camp et al8 performed a quantitative anatomic analysis of the UCL complex using 10 cadavers. The authors found the average surface area of the anterior bundle to be 324.2 mm2, with an origin footprint of 32.3 mm2 and an elongated insertional footprint length of 29.7 mm. These results are similar to those of the current study, as the average ulnar footprint length of the UCL was 34 mm. However, no study has evaluated what, if any, contribution to valgus resistance is provided by the middle and distal aspect of the ulnar UCL footprint.
Several proven techniques are available for UCLR, including the modified docking, modified Jobe, American Sports Medicine Institute (ASMI) modification, double docking, and others.1–3,16,18,21 These techniques often afford overhead athletes better than an 80% RTS rate, and previous studies have found no significant difference in RTS rate between techniques.4,19,20,36 Unfortunately, some athletes are unable to return to sport and some do return but retear their graft and require a revision UCLR.15,26,27 Hence, although the results are adequate, a significant amount of room for improvement remains. One of the ways to improve outcomes may be to slightly alter the surgical technique based on the new anatomic information about the UCL.
The premise of all UCLR techniques is that a ligament graft is used to re-create the UCL and is fixed in a variety of ways. Regardless of the technique, the reconstructed ulnar attachment site for the UCL is commonly placed less than 1 cm distal to the ulnohumeral joint. Hence, most current reconstruction techniques aim to re-create the proximal third of the UCL footprint. However, some authors now advocate that this insertion site should be moved distally during UCLR.28 Despite this, no prior study has evaluated the contribution of the middle and distal aspects of the UCL to determine whether the ulnar tunnel or socket in conventional UCLR techniques is placed in the ideal position to re-create the function of the UCL. If the middle and distal aspects of the UCL contributed significantly to valgus stability of the elbow, this could indicate that the ulnar tunnel or socket should be moved slightly more distal. However, the current investigation found that the middle and distal aspects of the UCL did not significantly contribute to valgus stability of the elbow.
One possible explanation for these findings is the general shape of the UCL ulnar insertion; it is wider proximally and narrows distally. Hence, the larger surface area attached in the region of the sublime tubercle likely contributes more to valgus stability than the thin piece that extends distally, simply because more fibers are attached proximally. Although proximal placement of the ulnar tunnel or socket near the sublime tubercle during UCLR appears biomechanically sound, future studies are needed to evaluate more anatomic graft placement that re-creates the patient’s native anatomic features and optimizes healing potential in order to further understand this complex ligament and determine whether a stronger construct exists.
Limitations
This study is a biomechanical cadaveric study and as such is subject to the limitations of working with cadaveric specimens. Although every effort was made to keep the UCL properly hydrated during testing, it is possible that the ligament became desiccated during testing. A standardized potting and testing protocol was used in an attempt to eliminate differences in testing parameters between elbows. Three of the 6 specimens in which the proximal third of the UCL was elevated off of the ulna failed before the middle and distal thirds could be sectioned.
Conclusion
The middle and distal thirds of the insertional footprint of the UCL on the ulna did not significantly contribute to gap resistance at 5 N·m of valgus load. The proximal third of the footprint is the primary resistor of valgus load.
Footnotes
One or more of the authors has declared the following potential conflicts of interest or source of funding: A surgeon-in-chief grant at the Hospital for Special Surgery was provided to help pay for the cadaveric specimens used in this study. B.J.E. has received research support from Synthes and educational support from Smith & Nephew. C.L.C. has received educational support and hospitality payments from Arthrex, Stryker, and Zimmer. D.W.A. has received educational support and hospitality payments from Arthrex and Stryker. S.H.C. is a consultant for Pivot Medical, Smith & Nephew, and Stryker; receives royalties from Blue Belt Technologies; and has stock/stock options in CyMedica Orthopedics and Stryker. J.S.D. has received research support from Arthrex; is a consultant for Arthrex, DePuy, Horizon Pharma, Merck Sharp & Dohme, Trice, and Wright Medical; receives royalties from Linvatec and Wolters Kluwer Health–Lippincott Williams & Wilkins; and is a paid speaker/presenter for Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hospital for Special Surgery (IRB No. 14010).
References
- 1. Andrews JR, Jost PW, Cain EL. The ulnar collateral ligament procedure revisited: the procedure we use. Sports Health. 2012;4(5):438–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med. 1995;23(4):407–413. [DOI] [PubMed] [Google Scholar]
- 3. Bowers AL, Dines JS, Dines DM, Altchek DW. Elbow medial ulnar collateral ligament reconstruction: clinical relevance and the docking technique. J Shoulder Elbow Surg. 2010;19(suppl2):110–117. [DOI] [PubMed] [Google Scholar]
- 4. Cain EL, Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. [DOI] [PubMed] [Google Scholar]
- 5. Callaway GH, Field LD, Deng XH, et al. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997;79(8):1223–1231. [DOI] [PubMed] [Google Scholar]
- 6. Camp CL, Conte S, D’Angelo J, Fealy SA. Epidemiology of ulnar collateral ligament reconstruction in Major and Minor League Baseball pitchers: comprehensive report of 1429 cases. J Shoulder Elbow Surg. 2018;27(5):871–878. [DOI] [PubMed] [Google Scholar]
- 7. Camp CL, Dines JS, van der List JP, et al. Summative report on time out of play for Major and Minor League Baseball: an analysis of 49,955 injuries from 2011 through 2016. Am J Sports Med. 2018;46(7):1727–1732. [DOI] [PubMed] [Google Scholar]
- 8. Camp CL, Jahandar H, Sinatro AM, Imhauser CW, Altchek DW, Dines JS. Quantitative anatomic analysis of the medial ulnar collateral ligament complex of the elbow. Orthop J Sports Med. 2018;6(3):2325967118762751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ciccotti MG, Siegler S, Kuri JA II, Thinnes JH, Murphy DJ. Comparison of the biomechanical profile of the intact ulnar collateral ligament with the modified Jobe and the docking reconstructed elbow: an in vitro study. Am J Sports Med. 2009;37(5):974–981. [DOI] [PubMed] [Google Scholar]
- 10. Cohen SB, Woods DP, Siegler S, Dodson CC, Namani R, Ciccotti MG. Biomechanical comparison of graft fixation at 30 degrees and 90 degrees of elbow flexion for ulnar collateral ligament reconstruction by the docking technique. J Shoulder Elbow Surg. 2015;24(2):265–272. [DOI] [PubMed] [Google Scholar]
- 11. Conte S, Camp CL, Dines JS. Injury trends in Major League Baseball over 18 seasons: 1998-2015. Am J Orthop (Belle Mead NJ). 2016;45(3):116–123. [PubMed] [Google Scholar]
- 12. Conte SA, Fleisig GS, Dines JS, et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43(7):1764–1769. [DOI] [PubMed] [Google Scholar]
- 13. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes: treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74(1):67–83. [PubMed] [Google Scholar]
- 14. Dines JS, ElAttrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35(12):2039–2044. [DOI] [PubMed] [Google Scholar]
- 15. Dines JS, Yocum LA, Frank JB, ElAttrache NS, Gambardella RA, Jobe FW. Revision surgery for failed elbow medial collateral ligament reconstruction. Am J Sports Med. 2008;36(6):1061–1065. [DOI] [PubMed] [Google Scholar]
- 16. Dodson CC, Thomas A, Dines JS, Nho SJ, Williams RJ III, Altchek DW. Medial ulnar collateral ligament reconstruction of the elbow in throwing athletes. Am J Sports Med. 2006;34(12):1926–1932. [DOI] [PubMed] [Google Scholar]
- 17. Dugas JR, Ostrander RV, Cain EL, Kingsley D, Andrews JR. Anatomy of the anterior bundle of the ulnar collateral ligament. J Shoulder Elbow Surg. 2007;16(5):657–660. [DOI] [PubMed] [Google Scholar]
- 18. Erickson BJ, Bach BR, Jr, Cohen MS, et al. Ulnar collateral ligament reconstruction: the Rush experience. Orthop J Sports Med. 2016;4(1):2325967115626876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Erickson BJ, Chalmers PN, Bush-Joseph CA, Verma NN, Romeo AA. Ulnar collateral ligament reconstruction of the elbow: a systematic review of the literature. Orthop J Sports Med. 2015;3(12):2325967115618914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Erickson BJ, Gupta AK, Harris JD, et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med. 2014;42(3):536–543. [DOI] [PubMed] [Google Scholar]
- 21. Erickson BJ, Romeo AA. The ulnar collateral ligament injury: evaluation and treatment. J Bone Joint Surg Am. 2017;99(1):76–86. [DOI] [PubMed] [Google Scholar]
- 22. Farrow LD, Mahoney AJ, Stefancin JJ, Taljanovic MS, Sheppard JE, Schickendantz MS. Quantitative analysis of the medial ulnar collateral ligament ulnar footprint and its relationship to the ulnar sublime tubercle. Am J Sports Med. 2011;39(9):1936–1941. [DOI] [PubMed] [Google Scholar]
- 23. Jackson TJ, Jarrell SE, Adamson GJ, Chung KC, Lee TQ. Biomechanical differences of the anterior and posterior bands of the ulnar collateral ligament of the elbow. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2319–2323. [DOI] [PubMed] [Google Scholar]
- 24. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68(8):1158–1163. [PubMed] [Google Scholar]
- 25. Lin F, Kohli N, Perlmutter S, Lim D, Nuber GW, Makhsous M. Muscle contribution to elbow joint valgus stability. J Shoulder Elbow Surg. 2007;16(6):795–802. [DOI] [PubMed] [Google Scholar]
- 26. Liu JN, Garcia GH, Conte S, ElAttrache N, Altchek DW, Dines JS. Outcomes in revision Tommy John surgery in Major League Baseball pitchers. J Shoulder Elbow Surg. 2016;25(1):90–97. [DOI] [PubMed] [Google Scholar]
- 27. Marshall NE, Keller RA, Lynch JR, Bey MJ, Moutzouros V. Pitching performance and longevity after revision ulnar collateral ligament reconstruction in Major League Baseball pitchers Am J Sports Med. 2015;43(5):1051–1056. [DOI] [PubMed] [Google Scholar]
- 28. Marshall TJ, Frangiamore S, Schickendantz M. Medial ulnar collateral ligament reconstruction: restoring the ulnar footprint. Tech Shoulder Elbow Surg. 2017;18(2):62–64. [Google Scholar]
- 29. Morrey BF. Applied anatomy and biomechanics of the elbow joint. Instr Course Lect. 1986;35:59–68. [PubMed] [Google Scholar]
- 30. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11(5):315–319. [DOI] [PubMed] [Google Scholar]
- 31. Morrey BF, An KN. Functional anatomy of the ligaments of the elbow. Clin Orthop Relat Res. 1985;201:84–90. [PubMed] [Google Scholar]
- 32. Morrey BF, Tanaka S, An KN. Valgus stability of the elbow: a definition of primary and secondary constraints. Clin Orthop Relat Res. 1991;265:187–195. [PubMed] [Google Scholar]
- 33. Mullen DJ, Goradia VK, Parks BG, Matthews LS. A biomechanical study of stability of the elbow to valgus stress before and after reconstruction of the medial collateral ligament. J Shoulder Elbow Surg. 2002;11(3):259–264. [DOI] [PubMed] [Google Scholar]
- 34. Rohrbough JT, Altchek DW, Hyman J, Williams RJ III, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30(4):541–548. [DOI] [PubMed] [Google Scholar]
- 35. Schwab GH, Bennett JB, Woods GW, Tullos HS. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin Orthop Relat Res. 1980;146:42–52. [PubMed] [Google Scholar]
- 36. Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36(6):1193–1205. [DOI] [PubMed] [Google Scholar]