Abstract
Background:
Lesion size is a major determinant of treatment strategy for osteochondral lesions of the talus (OLTs). Although magnetic resonance imaging (MRI) is commonly used in the preoperative evaluation of OLTs, the reliability of the MRI measurement compared with the arthroscopic measurement is unknown.
Purpose:
To compare preoperative lesion size measured on MRI versus intraoperative lesion size measured during arthroscopy.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
We retrospectively reviewed a consecutive series of patients treated with bone marrow stimulation for OLTs. The diameter of the lesion was measured at its widest point in 2 planes, and MRI measurements were compared with those made during arthroscopy using a custom-made graduated probe.
Results:
A total of 39 patients with 45 OLTs were analyzed. Mean ± SD area measurements on MRI were significantly greater than the equivalent arthroscopic measurements (42.2 ± 30.5 vs 28.6 ± 23.1 mm2, respectively; P = .03). Compared with the arthroscopic measurement, MRI overestimated OLT size in 53.3% (24/45) of ankles and underestimated OLT size in 24.4% (11/45). The mean MRI diameter measurement was significantly greater than the arthroscopic measurement in the coronal plane (MRI diameter vs arthroscopic measurement coronal plane, 6.1 ± 2.6 vs 4.9 ± 2.3 mm, P = .03; sagittal plane, 8.0 ± 3.6 vs 6.3 ± 3.6 mm, P = .05). Further, MRI overestimated coronal diameter in 48.9% (22/45) of ankles and underestimated in 26.7% (12/45) compared with the arthroscopic measurement. Similarly, sagittal plane MRI diameter measurements overestimated lesion size in 46.7% (21/45) of ankles and underestimated lesion size in 28.9% (13/45) compared with the arthroscopic findings.
Conclusion:
In a majority of lesions, MRI overestimated OLT area and diameter compared with arthroscopy. Surgeons should be aware of the discrepancies that can exist between MRI and arthroscopic measurements, as these data are important in making treatment decisions and educating patients.
Keywords: magnetic resonance imaging, arthroscopy, articular cartilage, osteochondral lesions of the talus, ankle, defect size
Osteochondral lesions of the talus (OLTs) are being increasingly recognized as a concern following trauma to the ankle.2,5,14,28,30,41,42 Up to 70% of ankle trauma may entail some form of chondral or osteochondral injury,1 and thus OLTs are a topic of increasing interest.
In an effort to establish a treatment algorithm, several authors have looked to lesion size, fully or partially based on magnetic resonance imaging (MRI) measurement, as a major indicator of which surgical intervention is appropriate for OLT.10,13,36 Lesions smaller than 150 mm2 may be treated with reparative procedures, such as bone marrow stimulation (BMS), whereas larger lesions may best be treated with replacement procedures, such as autologous osteochondral transplant.46 The decision as to whether a reparative or replacement procedure is performed has implications for surgical morbidity, outcomes, and cost.46 It is therefore important that the metric used to direct a particular treatment strategy be reliable and predictable.
MRI is commonly used in the preoperative evaluation and assessment of OLTs.# MRI aids in surgical decision making and planning by allowing the surgeon to better understand the lesion characteristics. However, to our knowledge, no previous study has compared OLT size measured preoperatively via MRI versus intraoperatively via arthroscopy.
The purpose of this study was to evaluate the preoperative size of OLTs measured on MRI compared with measurements of the OLTs made at the time of arthroscopy. We hypothesized that the size of the lesion on MRI preoperatively would be smaller than the size of the lesion measured arthroscopically.
Methods
This retrospective study was approved by our hospital institutional review board. Between September 2012 and March 2014, a consecutive series of 44 patients were treated with BMS for OLT. A senior surgeon (J.G.K.) performed all operative treatments and directed pre- and postoperative care. Surgery was indicated for patients who had evidence of an OLT on MRI, independent of lesion size, and for whom 3 months of nonoperative management had failed.
The inclusion criteria were patients who had an OLT treated with arthroscopic BMS and who underwent preoperative MRI within 6 months prior to surgery. Patients were excluded if they had any prior surgical intervention on the affected ankle, had diabetes, had autoimmune disease, had an active infection, or were current smokers. Patients who sustained cartilage damage on both talus and tibial surface were included; however, only the talar lesion was included for analysis.
MRI Assessment
Preoperative MRI was acquired by use of a 1.5-T MRI unit (Signa Horizon; GE Medical Systems). Coronal and sagittal plane T1-weighted and fat-suppressed T2-weighted images were obtained for all ankles. The repetition time/echo time for T1-weighted images were 500-600/11-15 milliseconds; for T2-weighted images, 2000/11-15 milliseconds; and for T2-weighted fat suppression images, 3400-3600/11-15 milliseconds. The other acquisition parameters were field of view, 150 × 150 mm; matrix size, 224 × 224; and slice thickness, 3.0 mm.
Two independent reviewers (Y.Y. and G.L.D.) who were not involved in patient care and were blinded to the outcome of the arthroscopic evaluation assessed the MRI and measured the lesions using an advanced image processing software (Picture Archiving and Communication System; McKesson Radiology). The diameter of the lesion was measured at the largest point in the coronal and sagittal planes (Figure 1). This measurement was taken from the rim of the surrounding cartilage layer to the base of the lesion. The lesion area was calculated by use of the elliptical area formula as described by Choi et al.10 When a discrepancy of 0.2 mm or more occurred between measurements taken by the 2 initial reviewers, a third reviewer (C.P.H.), who was also blinded to the arthroscopic measurement, assessed the images, and the mean of the closest 2 recorded measurements was taken. Any concomitant abnormalities of the foot and ankle were recorded.
Figure 1.
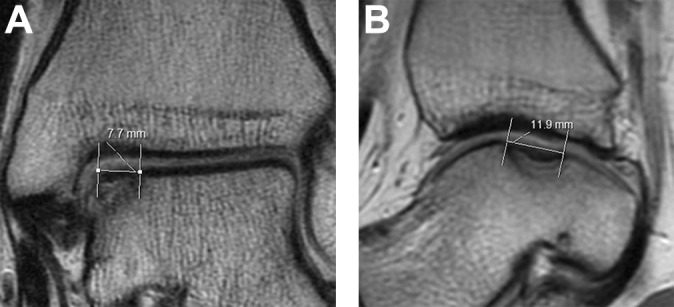
Preoperative T1-weighted magnetic resonance images of osteochondral lesion of the talus showing lesion diameter measurement on (A) coronal and (B) sagittal views.
Arthroscopic Assessment
Ankle arthroscopy was performed in all patients. A standard, noninvasive ankle distractor was used to increase joint access and visualization. A 2.7-mm, 30° scope was used via standard anteromedial, anterolateral, and posterolateral portals.19 A custom-made graduated probe (Smith & Nephew), with graduations every 1.0 mm, was used to measure the lesion at its widest point in 2 planes under direct arthroscopic visualization (Figure 2). The probe was custom-made so that it could measure the diameter from the perpendicular axis to the handle. Where a flap of cartilage existed, the measurement was taken from the peripheral rim of the remaining cartilage. Measurements were taken independently by the senior surgeon (J.G.K.) and a surgical fellow (E.J.F.), and if discrepancy of more than 0.5 mm was noted, measurements were rechecked until a consensus was reached. Following measurement of the lesion, the dead cartilage and the calcified subchondral bone were debrided. Microfracture was then performed as previously described.40
Figure 2.
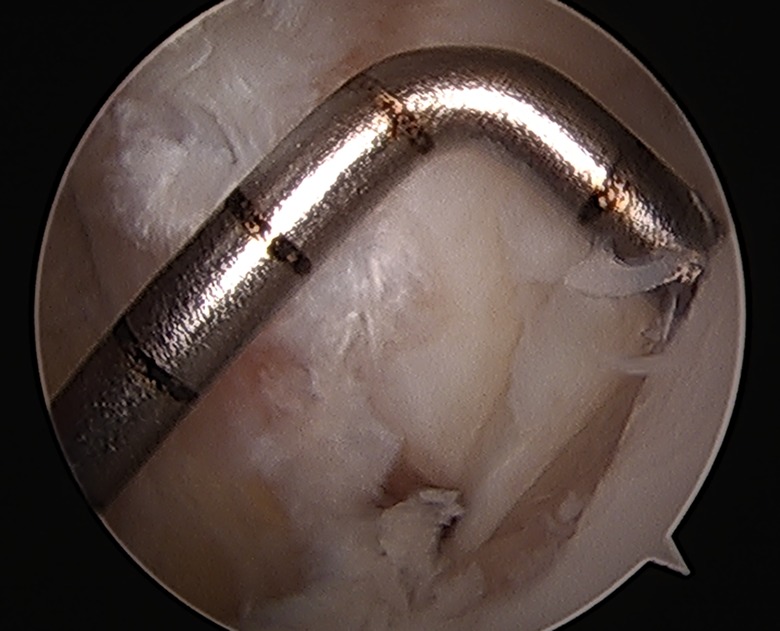
Measurement of lesion under arthroscopic view.
Concomitant intra-articular abnormality was identified at the time of surgery and recorded.
Statistical Analysis
All analyses were performed by use of SAS software version 9.1 (SAS Institute Inc). Lesion sizes were normally distributed and were compared by use of Student t tests. The Pearson correlation coefficient was calculated to assess the correlation between lesion size (MRI and arthroscopy area and diameter) and patient age, sex, laterality, history of trauma, associated abnormalities, medial/lateral lesion, and contained/uncontained lesion. P < .05 was considered significant. When a significant difference was found between the groups, a post hoc power analysis was conducted to confirm statistical power.
Results
Patient Demographics
The current study included 45 OLTs in 39 patients. Two patients were excluded because their preoperative MRI was taken more than 6 months prior to surgery. An additional 3 patients were excluded because they had prior surgery on the affected ankle.
The mean age of patients at the time of surgery was 38.3 ± 16.3 years (range, 18-69 years), and the mean time between MRI and surgery was 37.3 ± 10.1 days. Patient demographics, OLT characteristics, associated abnormalities, and concomitant procedures performed are summarized in Table 1.
TABLE 1.
Patient Demographics and Lesion Characteristicsa
| Total patients (total ankles), n | 39 (45) |
| Age, y, mean ± SD | 38.3 ± 16.3 |
| Male/female, n | 18/21 |
| History of trauma, n (%) of ankles | 31 (79.5) |
| Lesion location, medial/central/lateral, n of ankles | 31/0/14 |
| Days from MRI to surgery, mean ± SD | 37.3 ± 10.1 |
| Right-/left-sided lesion, n | 21/18 |
| Contained lesion/uncontained lesion in talus, n | 22/17 |
| Associated abnormalities, n | |
| Lateral ligament injury | 11 |
| Tendon involvement | 5 |
| Anterior bony impingement | 8 |
| Tibial plafond OCL | 6 |
| Subtalar OCL | 2 |
| Posterior ankle impingement | 1 |
| Osteoarthritis of the ankle joint | 1 |
| Hallux varus | 1 |
| Concomitant procedures, n | |
| Lateral ligament repair (Broström) | 8 |
| Anterior exostectomy | 8 |
| Tibialis posterior tendoscopy | 3 |
| Lateral ligament reconstruction | 2 |
| Subtalar microfracture | 2 |
| Loose body removal | 1 |
| Peroneal tendoscopy | 1 |
| Peroneus brevis repair | 1 |
| Hallux varus realignment | 1 |
aMRI, magnetic resonance imaging; OCL, osteochondral lesion.
Lesion Size
The mean lesion area measured on MRI was significantly greater than the mean lesion area measured arthroscopically (42.2 ± 30.5 vs 28.6 ± 23.1 mm2, respectively; P = .03; 95% CI, –24.9 to –2.26; statistical power, 0.78). When lesion size measured by MRI was compared with the arthroscopic measurement, 53.3% of ankles (24/45) had larger lesion size (overestimated) and 24.4% (11/45) had smaller lesion size (underestimated) on MRI measurement (Table 2).
TABLE 2.
Osteochondral Lesion Measurements on MRI vs During Arthroscopya
| Measurement | Result | P Value |
|---|---|---|
| Lesion area | ||
| Lesion area, mm2, mean ± SD | .03 | |
| MRI | 42.2 ± 30.5 | |
| Arthroscopy | 28.6 ± 23.1 | |
| MRI OLT size vs arthroscopic size, % | ||
| Overestimated | 53.3 | |
| Underestimated | 24.4 | |
| Coronal plane | ||
| Lesion diameter, mm, mean ± SD | .03 | |
| MRI | 6.1 ± 2.6 | |
| Arthroscopy | 4.9 ± 2.3 | |
| MRI OLT size vs arthroscopic size, % | ||
| Overestimated | 48.9 | |
| Underestimated | 26.7 | |
| Sagittal plane | ||
| Lesion diameter, mm, mean ± SD | .05 | |
| MRI | 8.0 ± 3.6 | |
| Arthroscopy | 6.3 ± 3.6 | |
| MRI OLT size vs arthroscopic size, % | ||
| Overestimated | 46.7 | |
| Underestimated | 28.9 |
aMRI, magnetic resonance imaging; OLT, osteochondral lesion of the talus. Underestimated: MRI lesion size was smaller than arthroscopic lesion size. Overestimated: MRI lesion size was larger than arthroscopic lesion size.
When lesion diameter measurements were compared, the mean MRI measurement was significantly greater than the arthroscopic evaluation in the coronal plane (MRI diameter vs arthroscopic measurement coronal plane, 6.1 ± 2.6 vs 4.9 ± 2.3 mm; P = .03; 95% CI, 0.14 to 2.35; statistical power, 0.99; sagittal plane, 8.0 ± 3.6 vs 6.3 ± 3.6 mm; P = .05; 95% CI, –0.02 to 3.25). Further, MRI overestimated coronal diameter in 48.9% of ankles (22/45) and underestimated it in 26.7% (12/45) compared with arthroscopic coronal diameter. Sagittal plane MRI diameter measurements overestimated lesion size in 46.7% (21/45) of ankles and underestimated lesion size in 28.9% (13/45) compared with arthroscopic findings.
Patient age, sex, history of trauma, associated abnormalities, medial/lateral, and contained/uncontained did not show significant correlation with lesion size or area evaluation (P > .05 for all associations).
Discussion
The results from this study demonstrate discrepancies between MRI and arthroscopic assessment of both surface area and diameter measurements for OLT.
Although Choi and colleagues12 reported a significant correlation between lesion size measured using preoperative MRI compared with measurements made under direct arthroscopic visualization, to our knowledge no published studies have investigated the differences in OLT size when assessed using MRI compared with arthroscopy as a primary outcome. Therefore, the current findings are valuable in terms of surgical planning for OLTs based on lesion size.
MRI has been a valuable tool in the diagnosis of OLT. Prior studies have reported that MRI is up to 100% specific and sensitive for diagnosing OLTs compared with arthroscopy.15,20,21,29,34,35,38 MRI is also advantageous in that it allows detailed assessment of the surrounding osseous and soft tissue structures (both intra- and extra-articular) that are commonly associated with OLTs.38,45 As a result, many clinicians obtain MRIs preoperatively both to diagnose OLTs and to aid in preoperative planning.**
Several staging systems based on the comparison of MRI and arthroscopic findings have been developed for grading OLTs.6,15–17,34 Although these staging systems can help physicians determine optimal treatment strategies, conflicting evidence has been reported with regard to MRI and arthroscopic OLT grading.17,18,29,34 Mintz et al34 performed a retrospective study on 54 patients who underwent MRI evaluation with subsequent arthroscopy and found that the MRI grade and arthroscopic grade were the same in 83% of patients. However, MRI underestimated the lesion grade in 17% of patients.34 In a retrospective study of 44 OLTs, Bae et al4 found that MRI overestimated lesion grade in 21% of patients and underestimated it in 14%. Although these studies compared the grading of OLTs on MRI and arthroscopically, to our knowledge no study has compared lesion size measurements. Whereas OLT grading helps describe OLTs, their clinical relevance and prognostic value remain to be elucidated. Ferkel et al19 showed no correlation between MRI grading and clinical outcomes. In a prospective study of 120 ankles, Choi et al12 found that plain radiograph, computed tomography, and MRI grade did not correlate with clinical outcomes. Furthermore, agreement between MRI and arthroscopic grading has been shown to vary in clinical studies, with concordance rates for lesion grading from 65.9% to 92% when these 2 modalities are compared.4,7,17,22,29,34,43
The current study demonstrates that MRI does not accurately measure lesion size when compared with arthroscopic measurements. MRI overestimated lesion size in up to 50% of cases, twice as often as it underestimated lesion size, leading to the conclusion that MRI measurement results in fairly inaccurate results favoring overestimation of talar lesion size. Additionally, mean lesion area and lesion diameter in the coronal plane measured via MRI were significantly greater than the values found by arthroscopic evaluation in the current study, with post hoc power analysis revealing sufficient power to support this finding.
To date, lesion size of 15 mm or 150 mm2 has been the standard cutoff criterion for using BMS for OLTs.36 However, a recent systematic review, including 25 therapeutic clinical studies evaluating both lesion size of OLTs and outcomes in patients who underwent BMS, revealed that the methods used to calculate the lesion area varied among these studies.36 Considering the results of the current study, caution is advised when one is interpreting the outcomes described in those studies, as there may be discrepancies in talar lesion size when measured on MRI and arthroscopically.
The reason why MRI overestimates lesion size remains unknown but may be due to multiple factors. The geometry of the articular surface of the ankle may alter lesion size measurements on MRI based on the location of the lesion. The convexity of the articular surface of the talus limits the ability of axial cuts to perfectly visualize the lesion. Ankle arthroscopy may also be limited because of the ankle mobility restriction or need for multiple portals, which may alter lesion size measurements. Further research is needed to better understand the relationship between MRI and arthroscopy in measuring lesion size. Yet, in light of the findings from the present study, larger interventions that require osteotomy and entail a greater likelihood of surgical morbidity may not always be necessary, particularly for patients with a lesion size of approximately 15 mm or 150 mm2, as this is the standard cutoff criterion for using BMS for OLTs. However, the treatment algorithm for smaller lesions, such as 10 mm or 100 mm2, does not necessarily depend on the method used to measure lesion size. Clinicians should recognize this limitation of MRI when making treatment decisions and educating patients on treatment options and clinical outcomes.
An accurate description of lesion size and homogeneity in lesion size assessment are important for future prognostic studies. Although MRI has been used as the standard for preoperative assessment and diagnosis of OLTs,24,31,33 it has several limitations compared with arthroscopy. Previous studies on OLTs have demonstrated that inconsistencies exist in the way lesion sizes are measured and characterized both on MRI and arthroscopically.†† In addition, many studies do not even report lesion size when describing outcomes after surgical treatment of OLTs, and many of the studies that do report lesion size do not describe how lesions are measured.23 In the current study, we describe a technique for measuring lesions intraoperatively and on MRI that is reproducible and may allow for more consistent reporting of lesion sizes.
This study has several limitations. The study is inherently limited by its retrospective design and the small number of patients. The current study included only smaller lesions (<150 mm2) treated with BMS that were compared only on MRI and arthroscopy. Lesions can be measured with other imaging modalities, such as plain radiographs and computed tomography, as well as during open procedures such as autologous osteochondral transplant. Future studies are warranted to compare sizes measured during open procedures and on other imaging modalities. The study is also limited because measurements made arthroscopically were conducted prior to debridement of unstable cartilage rims. Although lesion sizes were measured from the rim of native undamaged cartilage, debridement of any unstable cartilage may make the lesions larger. Future studies should compare arthroscopically conducted predebridement and postdebridement measurements versus measurements made on MRI.
Although a standardized approach was used to measure lesions on MRI and arthroscopically, some interobserver differences in measurement may have occurred, as previously described.37 The differences in resolution of 0.1 mm on MRI and 1 mm during arthroscopy are also limiting and may influence the results. Further, Choi et al10 found that the elliptical equation they described and that was used in this study overestimated lesion area by 15% compared with arthroscopy. Yet, our study found that MRI overestimated the lesion area by up to 47.5% compared with arthroscopy. This suggests that even when we account for the 15% overestimation inherent in the equation, MRI still overestimates the size of the lesion. In addition, and contrary to our study, Choi et al12 found that MRI underestimated lesion diameter. The difference between the results of our study and those of Choi et al12 highlight the limitation of measurements made on MRI compared with those made during arthroscopy. Future study into computer-assisted lesion measurement and area calculations would mitigate this limitation of MRI.
MRI may remain a valuable tool for diagnosis and characterization of OLTs. The results of the present study indicate that MRI inaccurately measures lesion size area and diameter compared with arthroscopic measurement. Physicians need to be aware of this discrepancy when counseling patients preoperatively, particularly in those with a lesion size of approximately 15 mm or 150 mm2; when planning their surgical technique; and when interpreting or conducting research on the correlation of lesion size and clinical outcomes.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.G.K. is a consultant for Arteriocyte and has received research support from the Ohnell Family Foundation, Mr. and Mrs. Michael J Levitt, and Arteriocyte. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hospital for Special Surgery (Protocol No. 29124).
References
- 1. Ackermann J, Fraser EJ, Murawski CD, Desai P, Vig K, Kennedy JG. Trends of concurrent ankle arthroscopy at the time of operative treatment of ankle fracture: a national database review. Foot Ankle Spec. 2016;9(2):107–112. [DOI] [PubMed] [Google Scholar]
- 2. Aktas S, Kocaoglu B, Gereli A, Nalbantodlu U, Guven O. Incidence of chondral lesions of talar dome in ankle fracture types. Foot Ankle Int. 2008;29(3):287–292. [DOI] [PubMed] [Google Scholar]
- 3. Angthong C, Yoshimura I, Kanazawa K, et al. Critical three-dimensional factors affecting outcome in osteochondral lesion of the talus. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1418–1426. [DOI] [PubMed] [Google Scholar]
- 4. Bae S, Lee HK, Lee K, et al. Comparison of arthroscopic and magnetic resonance imaging findings in osteochondral lesions of the talus. Foot Ankle Int. 2012;33(12):1058–1062. [DOI] [PubMed] [Google Scholar]
- 5. Berndt AL, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959;41:988–1020. [PubMed] [Google Scholar]
- 6. Bohndorf K. Osteochondritis (osteochondrosis) dissecans: a review and new MRI classification. Eur Radiol. 1998;8(1):103–112. [DOI] [PubMed] [Google Scholar]
- 7. Campbell AB, Knopp MV, Kolovich GP, et al. Preoperative MRI underestimates articular cartilage defect size compared with findings at arthroscopic knee surgery. Am J Sports Med. 2013;41(3):590–595. [DOI] [PubMed] [Google Scholar]
- 8. Choi GW, Choi WJ, Youn HK, Park YJ, Lee JW. Osteochondral lesions of the talus: are there any differences between osteochondral and chondral types? Am J Sports Med. 2013;41(3):504–510. [DOI] [PubMed] [Google Scholar]
- 9. Choi JI, Lee KB. Comparison of clinical outcomes between arthroscopic subchondral drilling and microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2140–2147. [DOI] [PubMed] [Google Scholar]
- 10. Choi WJ, Choi GW, Kim JS, Lee JW. Prognostic significance of the containment and location of osteochondral lesions of the talus: independent adverse outcomes associated with uncontained lesions of the talar shoulder. Am J Sports Med. 2013;41(1):126–133. [DOI] [PubMed] [Google Scholar]
- 11. Choi WJ, Kim BS, Lee JW. Osteochondral lesion of the talus: could age be an indication for arthroscopic treatment? Am J Sports Med. 2012;40(2):419–424. [DOI] [PubMed] [Google Scholar]
- 12. Choi WJ, Park KK, Kim BS, Lee JW. Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med. 2009;37(10):1974–1980. [DOI] [PubMed] [Google Scholar]
- 13. Chuckpaiwong B, Berkson EM, Theodore GH. Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy. 2008;24(1):106–112. [DOI] [PubMed] [Google Scholar]
- 14. Day GA, Swanson CE, Hulcombe BG. Operative treatment of ankle fractures: a minimum ten-year follow-up. Foot Ankle Int. 2001;22(2):102–106. [DOI] [PubMed] [Google Scholar]
- 15. De Smet AA, Fisher DR, Burnstein MI, Graf BK, Lange RH. Value of MR imaging in staging osteochondral lesions of the talus (osteochondritis dissecans): results in 14 patients. AJR Am J Roentgenol. 1990;154(3):555–558. [DOI] [PubMed] [Google Scholar]
- 16. De Smet AA, Ilahi OA, Graf BK. Reassessment of the MR criteria for stability of osteochondritis dissecans in the knee and ankle. Skeletal Radiol. 1996;25(2):159–163. [DOI] [PubMed] [Google Scholar]
- 17. Dipaola JD, Nelson DW, Colville MR. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy. 1991;7(1):101–104. [DOI] [PubMed] [Google Scholar]
- 18. Elias I, Jung JW, Raikin SM, Schweitzer MW, Carrino JA, Morrison WB. Osteochondral lesions of the talus: change in MRI findings over time in talar lesions without operative intervention and implications for staging systems. Foot Ankle Int. 2006;27(3):157–166. [DOI] [PubMed] [Google Scholar]
- 19. Ferkel RD, Zanotti RM, Komenda GA, et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med. 2008;36(9):1750–1762. [DOI] [PubMed] [Google Scholar]
- 20. Figueroa D, Calvo R, Vaisman A, Carrasco MA, Moraga C, Delgado I. Knee chondral lesions: incidence and correlation between arthroscopic and magnetic resonance findings. Arthroscopy. 2007;23(3):312–315. [DOI] [PubMed] [Google Scholar]
- 21. Friemert B, Oberlander Y, Schwarz W, et al. Diagnosis of chondral lesions of the knee joint: can MRI replace arthroscopy? A prospective study. Knee Surg Sports Traumatol Arthrosc. 2004;12(1):58–64. [DOI] [PubMed] [Google Scholar]
- 22. Gomoll AH, Yoshioka H, Watanabe A, Dunn JC, Minas T. Preoperative measurement of cartilage defects by MRI underestimates lesion size. Cartilage. 2011;2(4):389–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hannon CP, Smyth NA, Murawski CD, et al. Osteochondral lesions of the talus: aspects of current management. Bone Joint J. 2014;96(2):164–171. [DOI] [PubMed] [Google Scholar]
- 24. Hembree WC, Wittstein JR, Vinson EN, et al. Magnetic resonance imaging features of osteochondral lesions of the talus. Foot Ankle Int. 2012;33(7):591–597. [DOI] [PubMed] [Google Scholar]
- 25. Jung HG, Carag JA, Park JY, Kim TH, Moon SG. Role of arthroscopic microfracture for cystic type osteochondral lesions of the talus with radiographic enhanced MRI support. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):858–862. [DOI] [PubMed] [Google Scholar]
- 26. Kim YS, Lee HJ, Choi YJ, Kim YI, Koh YG. Does an injection of a stromal vascular fraction containing adipose-derived mesenchymal stem cells influence the outcomes of marrow stimulation in osteochondral lesions of the talus? A clinical and magnetic resonance imaging study. Am J Sports Med. 2014;42(10):2424–2434. [DOI] [PubMed] [Google Scholar]
- 27. Kuni B, Schmitt H, Chloridis D, Ludwig K. Clinical and MRI results after microfracture of osteochondral lesions of the talus. Arch Orthop Trauma Surg. 2012;132(12):1765–1771. [DOI] [PubMed] [Google Scholar]
- 28. Lee KB, Bai LB, Chung JY, Seon JK. Arthroscopic microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):247–253. [DOI] [PubMed] [Google Scholar]
- 29. Lee KB, Bai LB, Park JG, Yoon TR. A comparison of arthroscopic and MRI findings in staging of osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2008;16(11):1047–1051. [DOI] [PubMed] [Google Scholar]
- 30. Leontaritis N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J Bone Joint Surg Am. 2009;91(2):333–339. [DOI] [PubMed] [Google Scholar]
- 31. Leumann A, Valderrabano V, Plaass C, et al. A novel imaging method for osteochondral lesions of the talus—comparison of SPECT-CT with MRI. Am J Sports Med. 2011;39(5):1095–1101. [DOI] [PubMed] [Google Scholar]
- 32. Li S, Li H, Liu Y, Qu F, Wang J, Liu C. Clinical outcomes of early weight-bearing after arthroscopic microfracture during the treatment of osteochondral lesions of the talus. Chin Med J (Engl). 2014;127(13):2470–2474. [PubMed] [Google Scholar]
- 33. Linklater JM. Imaging of talar dome chondral and osteochondral lesions. Top Magn Reson Imaging. 2010;21(1):3–13. [DOI] [PubMed] [Google Scholar]
- 34. Mintz DN, Tashjian GS, Connell DA, Deland JT, O’Malley M, Potter HG. Osteochondral lesions of the talus: a new magnetic resonance grading system with arthroscopic correlation. Arthroscopy. 2003;19(4):353–359. [DOI] [PubMed] [Google Scholar]
- 35. O’Neill PJ, Van Aman SE, Guyton GP. Is MRI adequate to detect lesions in patients with ankle instability? Clin Orthop Relat Res. 2010;468(4):1115–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ramponi L, Yasui Y, Murawski CD, et al. Lesion size is a predictor of clinical outcomes after bone marrow stimulation for osteochondral lesions of the talus: a systematic review. Am J Sports Med. 2017;45(7):1698–1705. [DOI] [PubMed] [Google Scholar]
- 37. Schafer D, Boss A, Hintermann B. Accuracy of arthroscopic assessment of anterior ankle cartilage lesions. Foot Ankle Int. 2003;24(4):317–320. [DOI] [PubMed] [Google Scholar]
- 38. Schmid MR, Pfirrmann CW, Hodler J, Vienne P, Zanetti M. Cartilage lesions in the ankle joint: comparison of MR arthrography and CT arthrography. Skeletal Radiol. 2003;32(5):259–265. [DOI] [PubMed] [Google Scholar]
- 39. Shang XL, Tao HY, Chen SY, Li YX, Hua YH. Clinical and MRI outcomes of HA injection following arthroscopic microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1243–1249. [DOI] [PubMed] [Google Scholar]
- 40. Steadman JR, Rodkey WG, Rodrigo JJ. Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res. 2001;391(suppl):S362–S369. [DOI] [PubMed] [Google Scholar]
- 41. Stufkens SA, Knupp M, Horisberger M, Lampert C, Hintermann B. Cartilage lesions and the development of osteoarthritis after internal fixation of ankle fractures: a prospective study. J Bone Joint Surg Am. 2010;92(2):279–286. [DOI] [PubMed] [Google Scholar]
- 42. Takao M, Uchio Y, Naito K, Fukazawa I, Kakimaru T, Ochi M. Diagnosis and treatment of combined intra-articular disorders in acute distal fibular fractures. J Trauma. 2004;57(6):1303–1307. [DOI] [PubMed] [Google Scholar]
- 43. Vallotton JA, Meuli RA, Leyvraz PF, Landry M. Comparison between magnetic resonance imaging and arthroscopy in the diagnosis of patellar cartilage lesions: a prospective study. Knee Surg Sports Traumatol Arthrosc. 1995;3(3):157–162. [DOI] [PubMed] [Google Scholar]
- 44. van Bergen CJ, Kox LS, Maas M, Sierevelt IN, Kerkhoffs GM, van Dijk CN. Arthroscopic treatment of osteochondral defects of the talus: outcomes at eight to twenty years of follow-up. J Bone Joint Surg Am. 2013;95(6):519–525. [DOI] [PubMed] [Google Scholar]
- 45. Verhagen RA, Maas M, Dijkgraaf MG, Tol JL, Krips R, van Dijk CN. Prospective study on diagnostic strategies in osteochondral lesions of the talus: is MRI superior to helical CT? J Bone Joint Surg Br. 2005;87(1):41–46. [PubMed] [Google Scholar]
- 46. Yasui Y, Wollstein A, Murawski CD, Kennedy JG. Operative treatment for osteochondral lesions of the talus: biologics and scaffold-based therapy. Cartilage. 2017;8(1):42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Yoshimura I, Kanazawa K, Hagio T, Minokawa S, Asano K, Naito M. The relationship between the lesion-to-ankle articular length ratio and clinical outcomes after bone marrow stimulation for small osteochondral lesions of the talus. J Orthop Sci. 2015;20(3):507–512. [DOI] [PubMed] [Google Scholar]
- 48. Yoshimura I, Kanazawa K, Takeyama A, et al. Arthroscopic bone marrow stimulation techniques for osteochondral lesions of the talus: prognostic factors for small lesions. Am J Sports Med. 2013;41(3):528–534. [DOI] [PubMed] [Google Scholar]


