Abstract
Background:
Osteochondritis dissecans (OCD) of the capitellum is an increasingly recognized disease affecting young athletes. Because lesion progression is common, early identification is potentially beneficial for an athlete’s treatment and recovery. However, there is currently no analysis available that evaluates the impact of symptom duration on preoperative and postoperative outcomes.
Purpose/Hypothesis:
The purpose of this study was to perform a systematic review of surgically treated OCD lesions to examine the effect of symptom duration before the initial presentation on preoperative and postoperative outcomes. We hypothesized that a longer symptom duration would correlate with more severe preoperative signs and symptoms and poorer postoperative outcomes.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
Ovid MEDLINE, Embase, Scopus, the Cochrane Central Register of Controlled Trials, and the Database of Abstracts of Reviews of Effects were queried for studies evaluating symptom duration before the clinical presentation of capitellar OCD and surgical outcomes. A systematic review was conducted according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
Results:
A total of 23 studies reporting outcomes in 258 patients (mean patient age, 14.4 ± 1.5 years) were analyzed. Locking as a chief complaint predominated in a greater proportion of patients who presented with a longer history of OCD symptoms (P = .007). A longer symptom duration also correlated with a longer time to return to sport (P = .008) and older age (P < .001). Range of motion limitations as both a chief complaint and a physical examination finding correlated with a longer symptom duration (P = .014 and .001, respectively). Symptom duration did not show a relationship with most postoperative outcomes, including the return-to-sport rate (P = .172), which ranged from 70.7% to 91.1% depending on the surgical procedure performed. No significant difference was observed between symptom duration and the surgical procedure performed (P = .376).
Conclusion:
Advanced OCD lesions were observed in patients with a longer symptom duration. However, treatment specifics rather than symptom duration correlated best with return to sport for patients with advanced OCD lesions requiring surgery. The earlier detection of capitellar OCD may be valuable in reducing the severity of lesions, the time to return to sport, and potential need for surgery in young athletes.
Keywords: osteochondritis dissecans, elbow, symptom duration
Osteochondritis dissecans (OCD) is a cause of pain and functional impairment in the joints of adolescents. Elbow OCD lesions are relatively uncommon in the general population, with an incidence of 2.2 per 100,000 in 1 study.16 Within the elbow, the humeral capitellum is the most commonly reported location for OCD lesions.16,29 The cause of these, as with OCD lesions in other joints, is often unknown. They have been defined as a focal, idiopathic alteration of subchondral bone with the potential for instability and disruption of adjacent articular cartilage that may result in premature (early secondary) osteoarthritis.8,11,29 Microtrauma as a result of compressive and shear forces on the joint during upper extremity–dominant sports has been hypothesized as a component in the pathogenesis of OCD and is a significant factor in the development of symptoms in these athletes. However, the cause and, as a result, the best method for preventing or treating them are often not known.
Young athletes participating in upper extremity–dominant sports such as baseball, gymnastics, and wrestling are most prone to this disease.9,29,38 For young baseball players, it has been reported that greater than 3% have capitellar OCD.17 Among these young athletes, at the time of presentation, only 15% were found to have early-stage OCD lesions. Treatment options for these patients are well established in the literature, and nonoperative approaches involving activity restriction and physical therapy have yielded favorable results in these early-stage lesions.26,35 However, more advanced lesions historically have not done as well when treated conservatively, resulting in the development of multiple operative techniques. These techniques range from debridement and microfracture to osteochondral transfer, and in the correct settings, they have demonstrated good results for more advanced OCD.3,32,40
Investigations into possible causes for the progression of capitellar OCD severity are sparse, although a long duration of symptoms before seeking medical treatment has been suggested as a potentially significant factor.14,21,34 Compounding this issue are the often varied and nonspecific symptoms of capitellar OCD early on in the disease process,29 making the timely identification of affected patients difficult. A better understanding is therefore of value to raise awareness among athletes, coaches, parents, and medical providers to allow for an earlier diagnosis and injury intervention.
Previous studies have suggested that a relationship between symptom duration and OCD lesion severity exists.14,21,34 This systematic review of surgically treated OCD lesions sought to more thoroughly examine correlations between symptom duration before the clinical presentation and preoperative disease severity with postoperative outcomes. We hypothesized that a longer symptom duration would be correlated with a higher likelihood of advanced damage to the subchondral bone and articular cartilage and poorer postoperative outcomes.
Methods
Search Strategy
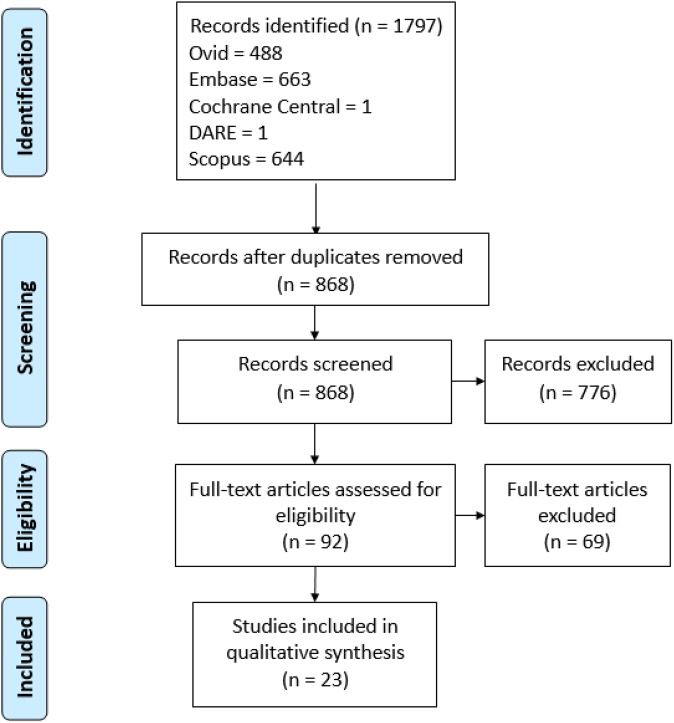
We conducted a search of the published literature for the concepts of OCD and elbow. Search strategies with a combination of standardized terms and keywords including “osteochondritis dissecans,” “osteochondrosis,” “elbow,” and “capitellum” were implemented in Ovid MEDLINE, Embase, Scopus, the Cochrane Central Register of Controlled Trials, and the Database of Abstracts of Reviews of Effects. The search was completed in June 2016 and resulted in 1797 total studies. Further screening was conducted according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Figure 1). After the removal of duplicates, a total of 868 unique citations were available for further screening. Exclusion criteria at this stage included Non–English-language studies, animal studies, review studies, abstracts or comments, and studies involving OCD of regions other than the capitellum. After applying these criteria, we identified 92 full-text studies for an in-depth review and confirmation. Of these, 69 were excluded for having a mean patient age of >20 years, describing nonoperative treatment, and/or failing to quantitatively report symptom duration before the clinical presentation. A final total of 23 articles was selected for meta-analysis; all were evidence level 4 studies.¶
Figure 1.
Literature search and screening using PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) guidelines.
Statistical Analysis
Relationships between clinical outcomes and mean symptom duration were assessed using meta-regression analyses with freeware OpenMetaAnalyst (Brown University) in consultation with a statistician.39 In these regression models, the outcomes were postoperative outcomes (Table 1), and the predictor was mean symptom duration before initial clinical presentation. The program fits random-effects models, which are used in the meta-regression to account for heterogeneity between study methods and patient groups. Statistical analyses were assessed at a .05 alpha level of significance. Numerators and denominators for proportions (eg, proportion returning to sport) were obtained from the included studies. For proportions, the Freeman-Tukey transformation was used to stabilize variances. For odds ratio analysis, the program takes proportions and converts them to a log odds ratio scale for binary comparisons. Means and standard deviations were obtained from studies directly. Statistical analysis was performed to explore the relationship between symptom duration and a set of preoperative and postoperative measures, as described in Table 1. Symptom duration was recorded in months (with associated standard deviations).
TABLE 1.
Preoperative and Postoperative Variables Tested Against Capitellar OCD Symptom Durationa
| Variable Tested | Metric |
|---|---|
| Preoperative | |
| Locking (chief complaint) | Percentage (with locking) |
| Decreased ROM (chief complaint) | Percentage (with decreased ROM) |
| Pain (chief complaint) | Percentage (with pain) |
| Swelling (chief complaint) | Percentage (with swelling) |
| Extension | Degrees |
| Flexion | Degrees |
| Stage 2 vs stage 1 lesion | Odds ratio |
| Stage 3 vs stage 1 lesion | Odds ratio |
| Stage 3 vs stage 2 lesion | Odds ratio |
| Age | Years |
| Skeletal maturity (on radiography) | Percentage (with open epiphysis) |
| Postoperative | |
| Extension | Degrees |
| Flexion | Degrees |
| Return to sport | Percentage |
| Time to return to sport | Months |
| Lesion healing (on radiography) | Percentage (with healing) |
| Lesion healing (on MRI) | Percentage (with healing) |
aMRI, magnetic resonance imaging; OCD, osteochondritis dissecans; ROM, range of motion.
Results
Outcomes across the 23 studies were reported in 258 patients with a mean age of 14.4 ± 1.5 years (range, 10-19 years); 87% (224/258) were male. All patients participated in sports, with the majority being baseball players (73%) and gymnasts (12%) and the remaining 15% participating in other sports including football, basketball, hockey, and track and field. Symptom duration before the initial clinical presentation ranged from 4.6 to 72 months, with a mean of 22.2 ± 16.6 months. All patients underwent surgical treatment for their OCD lesion. The most common surgical procedures performed were osteochondral autograft transfer (24%), microfracture (19%), and fixation (18%), with other or unspecified procedures comprising the remaining 39%. Patients had a mean follow-up of 34.7 ± 22.6 months.
Results of the analysis between symptom duration and the selected pre- and postoperative measures are summarized in Table 2.
TABLE 2.
Correlation Between Symptom Duration and Tested Variables After Meta-regression Analysisa
| Variable Tested | P Value |
|---|---|
| Preoperative | |
| Locking (chief complaint) | .007b |
| Decreased ROM (chief complaint) | .014b |
| Pain (chief complaint) | .064 |
| Swelling (chief complaint) | .319 |
| Extension | .001b |
| Flexion | .127 |
| Stage 2 vs stage 1 lesion | .058 |
| Stage 3 vs stage 1 lesion | .068 |
| Stage 3 vs stage 2 lesion | .410 |
| Age | <.001b |
| Skeletal maturity (on radiography) | .110 |
| Postoperative | |
| Extension | .531 |
| Flexion | .781 |
| Return to sport | .172 |
| Time to return to sport | .008b |
| Lesion healing (on radiography) | .944 |
| Lesion healing (on MRI) | .477 |
aMRI, magnetic resonance imaging; ROM, range of motion.
bStatistically significant relationship between variable tested and symptom duration (P < .05).
Chief Complaint
Twenty-two studies# totaling 242 patients, with a mean age of 14.4 ± 1.6 years and mean symptom duration of 21.8 ± 16.9 months, reported pain as a chief complaint in patient histories. No statistically significant correlation was found between symptom duration and the proportion of patients reporting pain in the elbow joint at the initial evaluation (P = .064). Seven studies1,3,7,21,25,37,41 totaling 89 patients reported swelling in the elbow joint as one of the patient’s chief complaints. The mean age of this group was 13.8 ± 1.6 years, with a mean symptom duration of 14.0 ± 10.3 months. Meta-regression analysis did not find a statistically significant relationship (P = .319) between symptom duration and the proportion of patients reporting swelling as a chief complaint.
Twelve studies** totaling 147 patients reported decreased range of motion (ROM) of the elbow as one of the patient’s chief complaints. The mean age in this group was 14.0 ± 1.1 years, with a mean symptom duration of 15.0 ± 9.3 months. Meta-regression analysis revealed that the proportion of patients reporting decreased ROM as a chief complaint correlated with an increased mean symptom duration before initial clinical presentation (P = .014). Nine studies3,7,15,19,21–23,25,28 totaling 126 patients reported elbow locking as one of the patient’s chief complaints. The mean age was 13.8 ± 1.3 years, and the mean symptom duration was 20.2 ± 13.6 months. A significant direct correlation (P = .007) was found between symptom duration and the proportion of patients with a chief complaint of locking.
Preoperative and Postoperative ROM
Twelve studies†† with 178 patients, with a mean age of 13.7 ± 0.9 years and mean symptom duration of 12.8 ± 6.2 months, provided preoperative extension and flexion data. Symptom duration before the initial clinical presentation had a statistically significant direct correlation with preoperative loss of elbow extension (P = .001). The relationship between symptom duration and preoperative flexion was statistically nonsignificant (P = .127). Eight studies10,18,22,23,25,32,36,41 including 104 patients with a mean age of 13.8 ± 0.7 years and mean symptom duration of 14.7 ± 8.5 months, provided postoperative extension and flexion data. No statistically significant correlation was found between symptom duration and postoperative extension (P = .531). Also, no statistical significance was found when examining symptom duration and postoperative flexion (P = .781).
Return to Sport
Return to the initial level of sport was assessed both in terms of the proportion of patients who returned and the mean time to return. Nineteen studies‡‡ involving 202 patients provided data on the proportion of patients who returned to their initial level of sport. The mean age was 14.1 ± 1.4 years, and the mean symptom duration was 20.9 ± 16.5 months. There was no significant relationship between symptom duration and the proportion of patients who returned to their previous level of activity (P = .172). However, from 8 studies,5,10,19,22,23,36,37,41 a significant correlation was found between symptom duration and the time that it took to return to sport (P = .008); these studies consisted of 71 patients with a mean age of 13.6 ± 1.1 years and mean symptom duration of 14.8 ± 6.3 months.
Age and Skeletal Maturity
All studies included in the analysis evaluated the relationship between symptom duration and patient age. A significant correlation was found between symptom duration and age (P < .001). However, across 6 studies6,12,22,23,36,41 totaling 112 patients reporting skeletal maturity at the time of presentation, no significant correlation was found between symptom duration and skeletal maturity (P = .110); the mean age of patients in these studies was 13.8 ± 0.8 years, and the mean symptom duration was 11.4 ± 6.6 months.
Surgical Procedures
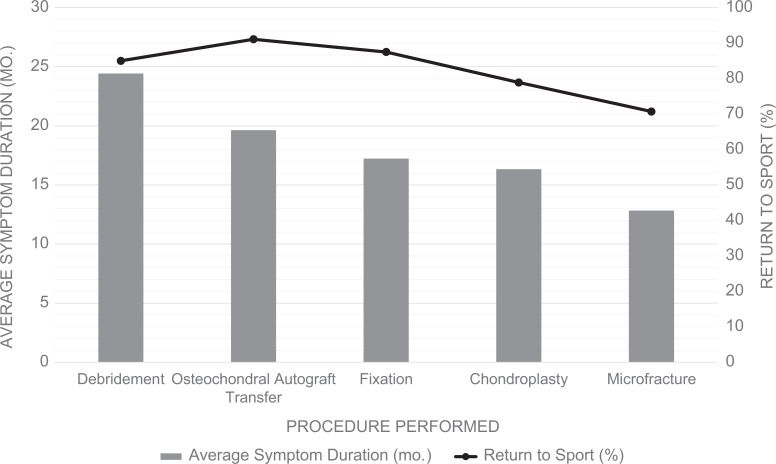
All studies provided data regarding the surgical procedure performed. Of the 23 studies, 21§§ provided data regarding symptom duration, and 18∥∥ provided data regarding the proportion of patients returning to sport after those procedures (Figure 2). In total, 19 patients underwent chondroplasty, with a mean symptom duration of 16.3 months and 78.9% (15/19) returning to sport. Twenty-two patients underwent debridement with a mean symptom duration of 24.4 months, and 85.0% (17/20) returned to sport. Thirty-two patients underwent fixation and had symptoms for a mean 17.2 months, with an 87.5% (28/32) return-to-sport rate. Forty-one patients underwent microfracture and were symptomatic for a mean 12.8 months, with a 70.7% (29/41) return-to-sport rate. Finally, 58 patients underwent osteochondral autograft transfer. These patents had a mean symptom duration of 19.6 months and a 91.1% (51/56) return-to-sport rate. There was no statistically significant difference in symptom duration between patients who underwent the different procedures (P = .376, analysis of variance). No significant difference was observed in the return-to-sport rate between the different procedures (P = .099, chi-square analysis).
Figure 2.
Surgical procedures with mean symptom duration and return-to-sport rate (black line).
Discussion
Symptom duration before seeking medical treatment has been suggested to play a role in capitellar OCD severity and outcomes by several groups in the literature. Jackson et al14 suggested “length of time before seeking medical advice” as an explanation for poor postoperative outcomes in 10 cases of gymnasts with capitellar OCD. Takahara et al34 also reported “timing of the initial presentation of the patient” as a possible contributor to differences in return to sport in 106 young athletes treated for capitellar OCD. Most recently, Lewine et al21 highlighted a correlation between longer symptom duration and the presentation of mechanical symptoms in their 21-patient retrospective review. Given the adolescent patient population, increased involvement in sports, the increasing trend of early sports specialization, and involvement at increasingly younger ages,20,24,29 a timely diagnosis of OCD is potentially beneficial for attaining better treatment outcomes. This systematic review sought to better understand the relationship between symptom duration before the initial presentation on OCD lesion progression and treatment outcomes. This analysis revealed that a longer symptom duration often correlated with more severe OCD lesions. Lesion severity, however, did not correlate ultimately with patients’ ability to return to sport, although they did take longer to return.
OCD lesions often present with a diffuse set of symptoms. Pain, swelling, decreased ROM, and locking are among the most common.29 Although symptoms are nonspecific, given that OCD lesions progress on a continuum from articular cartilage fissuring to loose body formation, patients’ chief complaints can be indicators of lesion severity. The current meta-regression analysis revealed that the chief complaint at initial presentation varies based on the duration of symptoms before seeking medical treatment. It was found that locking predominates in a greater proportion of patients who present with a longer history of OCD symptoms. This supports the idea that locking is a symptom associated with advanced OCD lesions, which occur later in the progression of OCD.29,38 This group of patients was also found to have a longer time to return to sport. This can be attributed to treatments for more advanced OCD lesions requiring more invasive surgical techniques with more extensive rehabilitative measures.33,38,40 Taken together, this finding suggests that an increased mean OCD symptom duration before seeking medical advice can be predictive of more advanced OCD lesions and consequently longer recovery periods. These findings extend and complement links between the severity of OCD lesions at the time of treatment and outcomes established in the existing literature. Takahara et al35 and Mihara et al26 reported that in patients managed nonoperatively for capitellar OCD, lesion severity correlated with outcomes. Baumgarten et al3 and Ruch et al32 described similar trends in cases of the surgical treatment of capitellar OCD.
While an increase in mean OCD symptom duration correlated with a longer time to return to sport, our analysis found that it did not influence whether patients ultimately returned to sport. This suggests that good outcomes are generally achieved across a variety of surgical treatments for capitellar OCD. Westermann et al40 conducted a meta-analysis of 24 studies with 492 patients who underwent microfracture and debridement, fixation, or osteochondral autograft transfer for capitellar OCD. At 6 months postoperatively, 86% of patients were able to return to sport (87%, 63%, and 95% by procedure, respectively). Although differences in outcomes were found to exist between procedures, positive results were generally obtained. Our meta-analysis revealed that symptom duration showed little relationship with postoperative outcomes and that the type of surgical procedure that was ultimately performed did not correlate with symptom duration. It seems, therefore, that for patients with advanced OCD lesions requiring surgical intervention, the specific surgical procedure necessary rather than symptom duration correlates best with when and whether they return to sport.
This meta-regression analysis also revealed that limitations in ROM as both a chief complaint and a physical examination finding correlated significantly with a longer symptom duration before the initial presentation. A possible conclusion is that athletes often play through pain or attribute it to being a “normal” part of the sport, seeking medical advice only when symptoms prohibit their ability to participate in their chosen sport. For these patients, decreased ROM may well be the first symptom prompting them to seek medical attention, making decreased ROM an “early presenting” symptom. Patient age, along with the associated higher levels of competition, may contribute to this detrimental behavior, as this study revealed a significant correlation between age and an increase in mean symptom duration before the initial presentation. Because the conservative treatment of early OCD lesions yields good outcomes with short return-to-sport durations, increased awareness and the early detection of capitellar OCD may allow more patients to be treated conservatively.26,35 Continuing to play through the pain may cause the lesion to propagate, necessitating surgical intervention and increasing the risks associated with surgery, particularly in the adolescent population. Further studies will need to look into specific treatment protocols, including conservative management, to determine which algorithm is the most effective for any given stage of capitellar OCD.
This study has some important limitations. This meta-analysis was conducted using level 4 studies; thus, the conclusions drawn from the regression analysis are based on low-level evidence. This analysis also focused only on surgical OCD studies. The specific surgical procedure used between and within each study varied. Differences in their outcomes and timelines were not able to be controlled. The same is true regarding variations in postoperative rehabilitation protocols between studies that may have influenced our return-to-sport proportion and duration statistics. The assessment of skeletal maturity as opposed to chronological age can also vary tremendously with the onset of puberty in our target patient group. Regarding the chief complaint analysis, patients who were not specifically described to have an absence of any chief complaint in this study were excluded rather than assumed to have a lack of that particular chief complaint. This may result in an overly conservative estimate. The different reporting methods inherent in a meta-analysis are also a potential confounder. Of note, preoperative lesion severity could not be reliably evaluated because of the variation in radiographic classifications used between studies. Only 6 studies in this meta-analysis used a previously established radiographic classification system (by Takahara et al,34 Minami et al,27 or Iwase and Igata13). A unified classification system would help future analyses better evaluate preoperative lesion severity.
Conclusion
Symptom duration before the initial clinical visit showed significant correlation with several parameters associated with advanced OCD lesions, including more severe chief complaints at the time of initial visit and a longer time to return to sport. These findings suggest a predictive role of symptom duration on the severity of OCD lesions at the initial presentation. Although most postoperative measures did not correlate with symptom duration, suggesting that for capitellar OCD requiring surgery, the type of procedure has a significant role in outcomes, catching these lesions at early stages may be valuable in reducing the need for surgery in young athletes. Ultimately, the earlier detection of capitellar OCD will lead to decreases in the severity of the lesions and the time to return to sport.
Acknowledgment
The authors sincerely thank Susan A. Fowler, MLIS (Washington University School of Medicine) for her help in formulating and curating the list of appropriate published literature from multiple electronic databases used in this study. They also thank James J. Grady, DrPH (University of Connecticut School of Medicine), and Matthew Solomito, PhD (Connecticut Children’s Medical Center), for their guidance and expertise in conducting statistical analyses, including the meta-analysis.
One or more of the authors has declared the following potential conflict of interest or source of funding: C.C. and H.S.R. have received an unrestricted grant from the Research in Osteochondritis Dissecans of the Knee (ROCK) Group. M.D.M. and C.W.N. have received unrestricted research grants from AlloSource and Vericel as members of the ROCK Group and receive royalties from Elsevier. J.J.N. is a consultant for Smith & Nephew, Responsive, and Ceterix Orthopaedics and has received research funding from Smith & Nephew and Zimmer. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Allaqui M, Koubaa M, Zied B, et al. Osteochondritis dissecans of the capitellum: autologous osteochondral mosaicplasty. A case report. Chir Main. 2012;31:206–209. [DOI] [PubMed] [Google Scholar]
- 2. Aydin H, Karahasanoglu I, Kerimoglu S, Turhan A. Treatment of capitellar osteochondritis dissecans with a tendon graft: a case report. Eklem Hastalik Cerrahisi. 2012;23:55–57. [PubMed] [Google Scholar]
- 3. Baumgarten TE, Andrews JR, Satterwhite YE. The arthroscopic classification and treatment of osteochondritis dissecans of the capitellum. Am J Sports Med. 1998;26:520–523. [DOI] [PubMed] [Google Scholar]
- 4. Bilsel K, Demirhan M, Atalar A, Akkaya S. A new surgical technique to facilitate osteochondral autograft transfer in osteochondral defects of the capitellum: a case report. Acta Orthop Traumatol Turc. 2010;44:82–87. [DOI] [PubMed] [Google Scholar]
- 5. Bojanic I, Ivkovic A, Boric I. Arthroscopy and microfracture technique in the treatment of osteochondritis dissecans of the humeral capitellum: report of three adolescent gymnasts. Knee Surg Sports Traumatol Arthrosc. 2006;14:491–496. [DOI] [PubMed] [Google Scholar]
- 6. Bojanic I, Smoljanovic T, Dokuzovic S. Osteochondritis dissecans of the elbow: excellent results in teenage athletes treated by arthroscopic debridement and microfracture. Croat Med J. 2012;53:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Byrd JWT, Jones KS. Arthroscopic surgery for isolated capitellar osteochondritis dissecans in adolescent baseball players: minimum three-year follow-up. Am J Sports Med. 2002;30:474–478. [DOI] [PubMed] [Google Scholar]
- 8. Edmonds E, Polousky J. A review of knowledge in osteochondritis dissecans: 123 years of minimal evolution from Konig to the ROCK Study Group. Clin Orthop Relat Res. 2013;471:1118–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Guerra JJ, Timmerman LA. Clinical anatomy, histology, and pathomechanics of the elbow in sports. Oper Tech Sports Med. 1996;4:69–76. [Google Scholar]
- 10. Harada M, Ogino T, Takahara M, Ishigaki D, Kashiwa H, Kanauchi Y. Fragment fixation with a bone graft and dynamic staples for osteochondritis dissecans of the humeral capitellum. J Shoulder Elbow Surg. 2002;11:368–372. [DOI] [PubMed] [Google Scholar]
- 11. Hixon AL, Gibbs LM. Osteochondritis dissecans: a diagnosis not to miss. Am Fam Physician. 2000;61:151–156. [PubMed] [Google Scholar]
- 12. Itsubo T, Murakami N, Uemura K, et al. Magnetic resonance imaging staging to evaluate the stability of capitellar osteochondritis dissecans lesions. Am J Sports Med. 2014;42:1972–1977. [DOI] [PubMed] [Google Scholar]
- 13. Iwase T, Igata T. Osteochondrosis of the humeral capitellum. Seikeigeka MOOK. 1988;54:26–44. [Google Scholar]
- 14. Jackson DW, Silvino N, Reiman P. Osteochondritis in the female gymnast’s elbow. Arthroscopy. 1989;5:129–136. [DOI] [PubMed] [Google Scholar]
- 15. Kenniston JA, Beredjiklian PK, Bozentka DJ. Osteochondritis dissecans of the capitellum in fraternal twins: a case report. J Hand Surg Am. 2008;33:1380–1383. [DOI] [PubMed] [Google Scholar]
- 16. Kessler JI, Nikizad H, Shea KG, Jacobs JC, Bebchuk JD, Weiss JM. The demographics and epidemiology of osteochondritis dissecans of the ankle, elbow, foot, and shoulder in children. Orthop J Sports Med. 2013;1(suppl 4):2325967113S00024. [Google Scholar]
- 17. Kida Y, Morihara T, Kotoura Y, et al. Prevalence and clinical characteristics of osteochondritis dissecans of the humeral capitellum among adolescent baseball players. Am J Sports Med. 2014;42:1963–1971. [DOI] [PubMed] [Google Scholar]
- 18. Koehler S, Walsh A, Pruzansky JS, Hausman MR. Arthroscopic all-inside suture fixation and bone grafting of osteochondritis dissecans lesions of the capitellum. J Shoulder Elbow Surg. 2015;24:1607–1612. [DOI] [PubMed] [Google Scholar]
- 19. Krijnen MR, Lim L, Willems WJ. Arthroscopic treatment of osteochondritis dissecans of the capitellum: report of 5 female athletes. Arthroscopy. 2003;19:210–214. [DOI] [PubMed] [Google Scholar]
- 20. LaPrade RF, Agel J, Nissen C, et al. AOSSM early sports specialization consensus statement. Orthop J Sports Med. 2016;4:2325967116644241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lewine EB, Miller PE, Micheli LJ, Waters PM, Bae DS. Early results of drilling and/or microfracture for grade IV osteochondritis dissecans of the capitellum. J Pediatr Orthop. 2016;36:803–809. [DOI] [PubMed] [Google Scholar]
- 22. Maruyama M, Satake H, Takahara M, et al. Treatment for ulnar neuritis around the elbow in adolescent baseball players: factors associated with poor outcome. Am J Sports Med. 2017;45:803–809. [DOI] [PubMed] [Google Scholar]
- 23. Maruyama M, Takahara M, Harada M, Satake H, Takagi M. Outcomes of an open autologous osteochondral plug graft for capitellar osteochondritis dissecans: time to return to sports. Am J Sports Med. 2014;42:2122–2127. [DOI] [PubMed] [Google Scholar]
- 24. Maruyama M, Takahara M, Satake H. Diagnosis and treatment of osteochondritis dissecans of the humeral capitellum. J Orthop Sci. 2018;23:213–219. [DOI] [PubMed] [Google Scholar]
- 25. Mihara K, Suzuki K, Makiuchi D, Nishinaka N, Yamaguchi K, Tsutsui H. Surgical treatment for osteochondritis dissecans of the humeral capitellum. J Shoulder Elbow Surg. 2010;19:31–37. [DOI] [PubMed] [Google Scholar]
- 26. Mihara K, Tsutsui H, Nishinaka N, Yamaguchi K. Nonoperative treatment for osteochondritis dissecans of the capitellum. Am J Sports Med. 2009;37:298–304. [DOI] [PubMed] [Google Scholar]
- 27. Minami M, Nakashita K, Ishii S, Usui M, Muramatsu I. Twenty-five cases of osteochondritis dissecans of the elbow. Rinsho Seikei Geka. 1979;14:805–810. [Google Scholar]
- 28. Nakagawa Y, Matsusue Y, Ikeda N, Asada Y, Nakamura T. Osteochondral grafting and arthroplasty for end-stage osteochondritis dissecans of the capitellum: a case report and review of the literature. Am J Sports Med. 2001;29:650–655. [DOI] [PubMed] [Google Scholar]
- 29. Nissen CW. Osteochondritis dissecans of the elbow. Clin Sports Med. 2014;33:251–265. [DOI] [PubMed] [Google Scholar]
- 30. Nobuta S, Ogawa K, Sato K, Nakagawa T, Hatori M, Itoi E. Clinical outcome of fragment fixation for osteochondritis dissecans of the elbow. Ups J Med Sci. 2008;113:201–208. [DOI] [PubMed] [Google Scholar]
- 31. Oka Y, Ikeda M. Treatment of severe osteochondritis dissecans of the elbow using osteochondral grafts from a rib. J Bone Joint Surg Br. 2001;83:738–739. [DOI] [PubMed] [Google Scholar]
- 32. Ruch DS, Cory JW, Poehling GG. The arthroscopic management of osteochondritis dissecans of the adolescent elbow. Arthroscopy. 1998;14:797–803. [DOI] [PubMed] [Google Scholar]
- 33. Ruchelsman DE, Hall MP, Youm T. Osteochondritis dissecans of the capitellum: current concepts. J Am Acad Orthop Surg. 2010;18:557–567. [DOI] [PubMed] [Google Scholar]
- 34. Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89:1205–1214. [DOI] [PubMed] [Google Scholar]
- 35. Takahara M, Ogino T, Fukushima S, Tsuchida H, Kaneda K. Nonoperative treatment of osteochondritis dissecans of the humeral capitellum. Am J Sports Med. 1999;27:728–732. [DOI] [PubMed] [Google Scholar]
- 36. Takeba J, Takahashi T, Hino K, Watanabe S, Imai H, Yamamoto H. Arthroscopic technique for fragment fixation using absorbable pins for osteochondritis dissecans of the humeral capitellum: a report of 4 cases. Knee Surg Sports Traumatol Arthrosc. 2010;18:831. [DOI] [PubMed] [Google Scholar]
- 37. Tsuda E, Ishibashi Y, Sato F, Yamamoto Y, Toh S. Osteochondral autograft transplantation for osteochondritis dissecans of the capitellum in nonthrowing athletes. Arthroscopy. 2005;21:1270. [DOI] [PubMed] [Google Scholar]
- 38. van Bergen C, van den Ende K, ten Brinke B, Eygendaal D. Osteochondritis dissecans of the capitellum in adolescents. World J Orthop. 2016;7:102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. Journal of Statistical Software. 2012;49:1–15. [Google Scholar]
- 40. Westermann RW, Hancock KJ, Buckwalter JA, Kopp B, Glass N, Wolf BR. Return to sport after operative management of osteochondritis dissecans of the capitellum. Orthop J Sports Med. 2016;4:2325967116654651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wulf CA, Stone RM, Giveans MR, Lervick GN. Magnetic resonance imaging after arthroscopic microfracture of capitellar osteochondritis dissecans. Am J Sports Med. 2012;40:2549–2556. [DOI] [PubMed] [Google Scholar]