Abstract
Objective:
To understand the transition of changed body image after the diagnosis and surgery in women with breast cancer.
Methods:
Semi-structured interview and focus group with narrative approach. Thematic analysis was performed using methodological and investigator triangulation methods.
Results:
Participants’ body image transformation was categorized into three phases: (1) the moment of diagnosis and changed self, (2) transition and recovery, and (3) normalization.
Conclusion:
The truth-telling process of breast cancer diagnosis and the freedom to choose their treatment options have a profound impact on body image transformation of women with breast cancer. Family support, social construction, and social support could help women with breast cancer pass through these transitional process faster, while inappropriate truth-telling by their surgeons and not having any choice in their treatment options will delay the transitional process.
Keywords: Breast cancer, body image, qualitative research
Background
Breast cancer is the most prevalent cancer in Thailand with a good prognostic outcome.1 The treatment options usually comprise surgery (mastectomy and breast-conserving surgery (BCT)), radiotherapy, and systemic therapy. The overall survival rate is around 70%.2,3 However, with the longer life expectancy in breast cancer survivors, women with breast cancer also have to face various side effects from their treatments such as loss of their breast, hair loss, and loss of fertility.4,5 Apart from the physical changes, they also face psychological disturbances as well: anxieties, depression, and fear of cancer recurrence.5–8 Furthermore, several studies also reported the breast cancer effects on survivors’ family, their social status, body image (BI), and quality of life (QoL).9,10
BI is defined as women’s perception and feelings of and about their body11 and their self-observation, social interaction, and belief.11 Body image disturbance (BID) can affect the psychosocial domain of women with breast cancer. It is also a predictive factor of their QoL. A woman who has persistent BID 1 year after the surgery can develop future psychosocial issues up to the next 6 years of their life.10,12–14
A previous longitudinal 2-year follow-up study showed that there was no change of BID at 2 years after surgery.12 However, in our previous study, we found that BI was the only modifiable factor affecting the QoL of women with breast cancer.13 Still, there has been no study that aims to understand the process of changed BI in women with breast cancer yet. Thus, this study aims to understand the transition of changed BI in Southern Thai women who have breast cancer.
Material and methods
Study design
Since we wanted to encapsulate transitional stage of women with breast cancer and their experiences, we chose to use qualitative research with a narrative approach. Semi-structured individual interviews and focus groups were both used to increase the data rigour. Participants were women with breast cancer who received treatment at the Radiation Oncology Division, Department of Radiology, Songklanagarind Hospital from October 2016 until April 2017. Inclusion criteria were women aged between 18 and 50 years, treated with mastectomy or BCT in the previous year, and could communicate in Thai. Exclusion criteria were any diagnosis of recurrence or metastatic cancer, secondary malignancy, and any psychiatric disorders, including schizophrenia or major depressive disorder. Participants were selected using the purposive sampling method with face-to-face approach by one of the research team members. One potential participant refused the semi-structured interview due to time constraint. All conversations were voice-recorded and transcribed verbatim after the written permission from the participants.
The interviewing process
After signing the informed consent form, the participants joined either a focus group session, semi-structured individual interview, or both. Focus groups were conducted with three to four researchers (one or two doctors (T. Peerawong or T. Phenwan)), one palliative care nurse (K.T.), and one psychologist (U.P.). T. Peerawong is a male radiation oncologist with 10 years’ experience in breast cancer care and also took cause in Human and Social development module. T. Phenwan is a male family doctor who specialized in palliative care and qualitative research. K.D. is a female nurse who had more than 30 years’ experience in palliative care. U.P. is a female counselling psychologist.
For the focus group session, 3–6 participants joined the focus groups, and the sessions took 60–90 min. The first 15 min was ice-breaking activities led by K.T. After that, they were instructed to draw a picture that ‘represents their body image’ and took turn talking about their drawings and BI.
As for the semi-structured interview session, the interviews took 45–90 min. Participants were individually interviewed in a private room in radiation oncology division with T.N.P. who treated all participants, thus already establishing a rapport with them. Participants were also asked to draw a picture with the same instruction. Both sessions were focused on three questions: (1) How did your BI change after the diagnosis? (2) How was it during the treatment? (3) What is your future plan regarding your changed BI? Audit trails were also made immediately after each session.
Data were analysed using content analysis with methodological and investigator triangulation methods. Two researchers (T.N.P. and T.R.P.) individually created codes from the interviews in ATLAS.ti software. Any discrepancies were discussed thoroughly until consensus for the final analysis was reached.
Trustworthiness of data
We used Lincoln and Guba as an evaluative framework and also Consolidated criteria for reporting qualitative research (COREQ) to describe the data collection and analysis process15 (Supplementary Appendix).
We used data and investigator triangulation methods to enhance the credibility. Thick description was also used for the transferability. Audit trail of the process was performed for the confirmability of our work along with data and investigator triangulation method.
This study was approved by the Human Research and Ethics Committee of the Prince of Songkla University (EC No. REC 59-179-07-1).
Results
In total, 25 participants joined the study. We conducted 11 semi-structured interviews and 4 focus groups in total. One interview could not be recorded and transcribed due to technical errors. No repeated interview was carried out. For the demographic data of all participants, the median age with interquartile ranges was 45 (40.5, 47.3) years and most of them were Buddhist and married. 71% of the participants received BCT and 67% received chemotherapy. The details are shown in Table 1.
Table 1.
Participants’ characteristics.
| Sessions | Semi-structured interview (n = 10) | Focus group (n = 14) |
|---|---|---|
| Age (years), median (IQR) | 45.5 (41.0, 47.0) | 45.0 (40.0, 47.8) |
| Religion | ||
| Buddhist | 9 | 12 |
| Muslim | 1 | 2 |
| Marital status | ||
| Married | 9 | 9 |
| Single | 1 | 2 |
| Unknown | 0 | 3 |
| BMI (kg/m2), median (IQR) | 24.4 (21.2, 28.3) | 22.5 (19.9, 24.6) |
| Working | 9 | 4 |
| Disease status | ||
| Stage | ||
| DCIS | 2 | 1 |
| IA | 4 | 2 |
| IIA | 2 | 7 |
| IIB | 1 | |
| IIIA | 1 | 1 |
| IIIB | 1 | 1 |
| IIIC | 1 | |
| Treatment | ||
| Type of surgery | ||
| Breast conservative surgery | 7 | 10 |
| Modified radical mastectomy | 3 | 4 |
| Radiotherapy | 10 | 14 |
| Chemotherapy and/or targeted therapy | 6 | 10 |
| Hormonal therapy | 9 | 12 |
IQR: interquartile range; BMI: body mass index; DCIS: ductal carcinoma in situ.
For the qualitative analysis, participants’ BID was categorized into three phases: (1) the moment of diagnosis and changed self, (2) transition and recovery, and (3) normalization (Figure 1).
Figure 1.
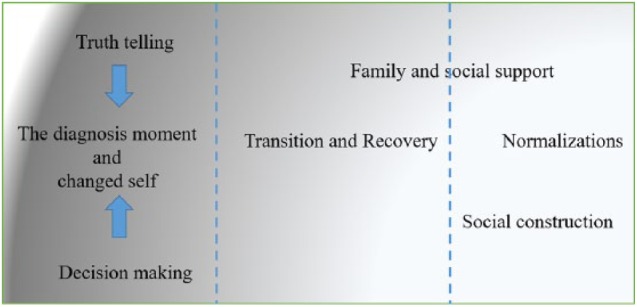
Participants’ body image disturbance transition.
The moment of diagnosis and changed self
All the participants remembered the moment of their breast cancer diagnosis vividly. They stated that their life changed completely right after the news:
When I heard the word [cancer], my life changed completely. Am I dying? Is my one foot already in the grave?
From our study, the severity and duration of this phase depended on two factors: the freedom to make treatment decisions and the truth-telling of their primary doctors. Participants who could decide their treatment plan had less BID than those who could not:
[Breast cancer] Cut it out or die … That’s what he [doctor] said. I had no choice at all.
However, the most influential factor was the truth-telling process. Participants who went through improper or rushed truth-telling by their primary doctor had more severe BID:
I was entering the doctor’s office with my husband when he [doctor] told us, ‘You have breast cancer and it needs to be removed or else you will die. My husband just broke down and cried right at the door’.
Afterwards, participants’ BI changed. They admitted feeling completely changed from the inside out. Participants with significant body changes, such as hair loss, also had more BID:
I feel I am different … I shaved my head because I could not bear the sight of my hair falling out and withering. We were crying, my husband and my daughter, because life was not the same for us anymore.
Transition and recovery
The stigmatized word ‘cancer’ will spread from participants to their spouses, children, and close relatives; the ripple effect will spread into their communities, changing a woman-mother-wife into an embodiment that represents loss, death, and suffering:
When my son told his teacher that I had cancer and begged her not to punish him for not doing his homework, she wept horribly. They [the teachers] kept supporting us, buying stuff, visiting our house. But they were always crying and pitying me.
I was the first person to get cancer in my village. Lots of people came to my place because they wanted to have a look at ‘cancer’. When I showed them my breast that had pus and a smelly wound, they either cried or turned their head away or showed clear disgust on their face. I was a freak show for the whole village.
Apart from breast cancer, treatments changed the BI of these women as well. At first, they avoided attending social gatherings, due to hair loss and fear of social alienation. They stated that they lost confidence and felt uncertain about their current self:
I went to the market without my bandana on and people kept staring. A child saw my bald head and screamed like mad.
During this phase, the transition speed varied, depending on the participants’ background, how they received the bad news, or whether they had a treatment option or not. Participants who had a strong family or social support also got through this phase quicker.
Normalization
The third phase was the process of bringing normality into participants’ lives. Like other phases, each person reached this state at a different pace. However, we found that the major contributing factors that helped them cope were family support and social support.
Family support
Participants that had excellent family support reached this phase quicker than those who did not. This may be due to an aspect of Thai culture in which BI in women is more of a familial image than an individual one. When significant changes, in this case cancer, occurred, they lived through it with the support of their families:
My daughter told me ‘Don’t worry, mum. I’m sure that you will get better. Don’t worry about me, just focus on getting better’. She’s the positive thing in my life and I’m so lucky to have her.
This also applied to the cases in which the women needed to be their own pillars of support:
My husband was weak-hearted. I waited for three days after the diagnosis to tell him the news. He couldn’t stop sobbing and I had to be the one to console him. ‘Why do you cry so much? I’m the one that has it [cancer], not you’. I can’t be weak. I need to be strong for my husband, and my son who is studying far away.
Social support
The society or community that they lived in also had a supportive effect on their BI. If the society perceived them as ‘normal’, participants would feel at ease, fitting in the society, and, as result, have drastically reduced BID:
I went back to teaching. Everything was more or less the same. No students were making fun of me. My boss and my colleagues were also very supportive.
I went to the market and the merchants were laughing and joking with me that I looked normal and did not have the [cancer] look. (laugh)
Discussion
Breast cancer is the most prevalent cancer in Thai women. The disease not only impacts the patients physically but also has a lasting impact on their BI as well. Apart from that, the very treatment of cancer also causes them BID as well. Our work demonstrates how women with breast cancer transcended each phase of their cancer journey. From this study, participants had a changed BI in three phases: (1) the moment of diagnosis and changed self, (2) transition and recovery, and (3) normalization. During the first phase, participants’ ability to have a choice in their treatment and the process in which bad news is related to them are the two factors that will either hasten or delay their transition. Participants that received improper truth-telling process would take longer time to pass the first stage of their transition. This finding coincides with previous research that determined that the manner in which bad news is disclosed is directly correlated with patient QoL and BI.10,16–21
Once they enter the second phase, participants need family and social support to get them through the cancer stigmatization. We found that those who had good support got through this phase faster than those who did not. This finding also supports past studies’ findings that breast cancer survivors need both family support and social support.6,22 We also found that in married participants the most influential factor which allowed them to pass through this phase quickest was family, with their spouse being recognized as the most important support they needed.
As for the final phase, participants who felt that they could blend into society had drastically reduced BID. Like other works, participants’ perception of being back to ‘normal’ varied but it consisted of being physically independent (could do chores and work), family perceiving them as being normal, and was socially constructed as normal.6,23 However, from our study, the social construction of the ‘cancer’ was still perceived and related with negativity and death until they could be perceived as normal again.24 Thus, these findings showed that participants’ BI was affected by a multitude of factors apart from their illnesses. From our findings, one of the most prominent modifiable factors was the truth-telling process by their doctors. Most participants received an incomplete or improper breaking bad news process and thus delayed their transition in the first phase. This may be due to the fact that, in the older medical curriculum, most doctors in Thailand did not learn the truth-telling process during their undergraduate study or in their postgraduate training period. An emphasis of delivering bad news efficiently is noteworthy since it has a direct link to a patient’s perceived health and QoL.18,21,25–28
The other modifiable factor was their peer support: family support, social support, and the perceived social construction of cancer patients. While each participant may have had a different family background and level of support, social support still played a major role in helping these women. Social support groups to raise breast cancer awareness, supporting women with breast cancer while demystifying cancer, clarifying that cancer does not mean certain death, are recommended.5–7 Fortunately, in the recent years, there has been an increasing number of healthcare professional support groups and also volunteer groups to support women with breast cancer across Thailand. However, the quality of care and support they delivered still varied immensely. Thus, education programmes with quality assessment may be helpful.
To our knowledge, this is the first work that delves into the transition of Southern Thai women’s breast cancer journey. It demonstrates that these women require not only medical support from healthcare providers, but they also need family and social support in order to feel normal again. In addition, we also used drawings to act as a distraction which allowed them to express any concerns they had. We discovered that the concept of their BI differed from previous studies.11 Their BI was collective and familial rather than individualistic, which coincides with the collective nature of Thai culture.29 Thus, in order to help them cope with breast cancer, extra social support is recommended.
Our work has a few limitations. First, while the majority of Thais are Buddhist by nature, in Southern Thailand, especially in the borderland where we conducted our study, the demographic data are different. The locals are living in a culturally pluralistic background with an amalgamation of Buddhist, Muslim, Christian, and other ethnic minorities. Thus, generalization to other parts of the country or other countries may not be applicable. Second, several focus group interviews had participants who came from different educational backgrounds; thus, some of these participants intellectually dominated the group process. We then selected certain cases for further in-depth interviews in order to collect more data.
Conclusion
In Southern Thai women with breast cancer, the manner of disclosing the breast cancer diagnosis and choice of treatment options both have an important impact on body image transformation. Social support also plays a significant role in helping these women. Social support groups to raise breast cancer awareness and support women with breast cancer, in order to demystify cancer while clarifying that recovery is a real possibility, are recommended.
Supplemental Material
Supplemental material, Appendix_1 for Body image transformation after breast cancer diagnosis and treatment in southern Thai women by Thanarpan Peerawong, Tharin Phenwan, Somrit Mahattanobon, Kandawsri Tulathamkij and Uraiwan Pattanasattayavong in SAGE Open Medicine
Acknowledgments
We thank our staff in Radiation Oncology Division, Department of Radiology, Faculty of Medicine for kindly support during the focus group sessions. We would also like to thank International Affair Unit, Faculty of Medicine, Prince of Songkla University for his help with English language style and editing.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: This study was approved by the Human Research and Ethics Committee of the Prince of Songkla University (EC No. REC 59-179-07-1).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by the Faculty of Medicine, Prince of Songkla University with No. REC 59-179-07-1.
Informed consent: After signing the informed consent form, participants joined either a focus group session or a semi-structured individual interview.
ORCID iDs: Thanarpan Peerawong  https://orcid.org/0000-0003-1725-6355
https://orcid.org/0000-0003-1725-6355
Tharin Phenwan  https://orcid.org/0000-0003-0120-952X
https://orcid.org/0000-0003-0120-952X
Supplemental material: Supplemental material for this article is available online.
References
- 1. Khuhaprema T. Cancer in Thailand, vol. 7 Bangkok: National Cancer Institute, 2013. [Google Scholar]
- 2. Gradishar WJ, Comprehensive RHL, Forero A, et al. NCCN guidelines index table of contents discussion. Breast Cancer 2018; 209: MS16–MS48. [Google Scholar]
- 3. Che Y, You J, Zhou S, et al. Comparison of survival rates between Chinese and Thai patients with breast cancer. Asian Pac J Cancer Prev 2014; 15(15): 6029–6033. [DOI] [PubMed] [Google Scholar]
- 4. Odle TG. Adverse effects of breast cancer treatment. Radiol Technol 2014; 85: 297M–319M, quiz 320M–323M. [PubMed] [Google Scholar]
- 5. Tripathi L, Datta SS, Agrawal SK, et al. Stigma perceived by women following surgery for breast cancer. Indian J Med Paediatr Oncol 2017; 38(2): 146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Trusson D, Pilnick A. Between stigma and pink positivity: women’s perceptions of social interactions during and after breast cancer treatment. Sociol Health Illn 2017; 39(3): 458–473. [DOI] [PubMed] [Google Scholar]
- 7. Meacham E, Orem J, Nakigudde G, et al. Exploring stigma as a barrier to cancer service engagement with breast cancer survivors in Kampala, Uganda. Psycho-Oncology 2016; 25(10): 1206–1211. [DOI] [PubMed] [Google Scholar]
- 8. Curtis R, Groarke A, McSharry J, et al. Experience of breast cancer: burden, benefit, or both. Cancer Nurs 2014; 37(3): E21–E30. [DOI] [PubMed] [Google Scholar]
- 9. Morrison TL, Thomas RL. Cancer survivors’ concealment or disclosure of diagnosis: implications for return to work. Work 2015; 52(3): 643–655. [DOI] [PubMed] [Google Scholar]
- 10. Fingeret MC, Teo I, Epner DE. Managing body image difficulties of adult cancer patients: lessons from available research. Cancer 2014; 120(5): 633–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lehmann V, Hagedoorn M, Tuinman MA. Body image in cancer survivors: a systematic review of case-control studies. J Cancer Surviv 2015; 9(2): 339–348. [DOI] [PubMed] [Google Scholar]
- 12. Collins KK, Liu Y, Schootman M, et al. Effects of breast cancer surgery and surgical side effects on body image over time. Breast Cancer Res Treat 2011; 126(1): 167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Peerawong T, Phenwan T, Supanitwatthana S, et al. Breast conserving therapy and quality of life in Thai females: a mixed methods study. Asian Pac J Cancer Prev 2016; 17(6): 2917–2921. [PubMed] [Google Scholar]
- 14. Moreira H, Canavarro MC. A longitudinal study about the body image and psychosocial adjustment of breast cancer patients during the course of the disease. Eur J Oncol Nurs 2010; 14(4): 263–270. [DOI] [PubMed] [Google Scholar]
- 15. Booth A, Hannes K, Harden A, et al. COREQ (Consolidated Criteria for Reporting Qualitative Studies). In: Moher D, Altman D, Schulz K, et al. (eds) Guidelines for reporting health research: a user’s manual. Hoboken, NJ: John Wiley & Sons, pp. 214–226. [Google Scholar]
- 16. Rhoten BA, Murphy B, Ridner SH. Body image in patients with head and neck cancer: a review of the literature. Oral Oncol 2013; 49(8): 753–760. [DOI] [PubMed] [Google Scholar]
- 17. Jie B, Qiu Y, Feng ZZ, et al. Impact of disclosure of diagnosis and patient autonomy on quality of life and illness perceptions in Chinese patients with liver cancer. Psycho-Oncology 2016; 25(8): 927–932. [DOI] [PubMed] [Google Scholar]
- 18. Nakajima N, Hata Y, Onishi H, et al. The evaluation of the relationship between the level of disclosure of cancer in terminally ill patients with cancer and the quality of terminal care in these patients and their families using the Support Team Assessment Schedule. Am J Hosp Palliat Care 2013; 30(4): 370–376. [DOI] [PubMed] [Google Scholar]
- 19. Smith TJ, Dow LA, Virago E, et al. Giving honest information to patients with advanced cancer maintains hope. Oncology 2010; 24(6): 521–525. [PubMed] [Google Scholar]
- 20. Da Costa Vargens OM, Bertero CM. Living with breast cancer: its effect on the life situation and the close relationship of women in Brazil. Cancer Nurs 2007; 30(6): 471–478. [DOI] [PubMed] [Google Scholar]
- 21. Lheureux M, Raherison C, Vernejoux JM, et al. Quality of life in lung cancer: does disclosure of the diagnosis have an impact. Lung Cancer 2004; 43(2): 175–182. [DOI] [PubMed] [Google Scholar]
- 22. Badr H. New frontiers in couple-based interventions in cancer care: refining the prescription for spousal communication. Acta Oncol 2017; 56(2): 139–145. [DOI] [PubMed] [Google Scholar]
- 23. Aguilar Cordero MJ, Neri Sanchez M, Mur Villar N, et al. Influence of the social context on the body image perception of women undergoing breast cancer surgery. Nutr Hosp 2013; 28(5): 1453–1457. [DOI] [PubMed] [Google Scholar]
- 24. Suwankhong D, Liamputtong P. Breast cancer treatment: experiences of changes and social stigma among Thai women in southern Thailand. Cancer Nurs 2016; 39(3): 213–220. [DOI] [PubMed] [Google Scholar]
- 25. Montazeri A, Hole DJ, Milroy R, et al. Does knowledge of cancer diagnosis affect quality of life? A methodological challenge. BMC Cancer 2004; 4: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dias L, Chabner BA, Lynch TJ, Jr, et al. Breaking bad news: a patient’s perspective. Oncologist 2003; 8(6): 587–596. [DOI] [PubMed] [Google Scholar]
- 27. Wang QX, Bai Y, Lu GF, et al. Perceived health-related stigma among patients with breast cancer. Chin Nurs Res 2017; 4: 158–161. [Google Scholar]
- 28. Seyedrasooly A, Rahmani A, Zamanzadeh V, et al. Association between perception of prognosis and spiritual well-being among cancer patients. J Caring Sci 2014; 3(1): 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hofstede GH, Hofstede GJ, Minkov M. Cultures and organizations: software of the mind: intercultural cooperation and its importance for survival. 3rd ed. New York: McGraw-Hill, 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendix_1 for Body image transformation after breast cancer diagnosis and treatment in southern Thai women by Thanarpan Peerawong, Tharin Phenwan, Somrit Mahattanobon, Kandawsri Tulathamkij and Uraiwan Pattanasattayavong in SAGE Open Medicine


