Abstract
Daily habits and actions powerfully affect the risk of cardiovascular disease (CVD), in general, and coronary heart disease, in particular. Regular physical activity, sound nutrition, weight management, and not smoking cigarettes have all been demonstrated to significantly reduce the risk of CVD. In 2 large cohort studies a reduction of risk of CVD of >80% and diabetes >90% were demonstrated in individuals who followed a cluster of these lifestyle practices. The study of the impact of lifestyle factors on CVD risk has coalesced under the framework of “lifestyle medicine.” Despite the overwhelming evidence that lifestyle factors affect CVD, a distinct minority of individuals are following these practices. The American Heart Association estimates that only 5% of individuals follow all of these lifestyle factors as components of a strategy to achieve “ideal” cardiovascular health. The challenge to the medical and health care communities is to more aggressively incorporate this information into the daily practices of medicine.
Keywords: Lifestyle medicine and cardiovascular disease, risk factor reduction, cardiovascular health
‘. . ., progress in helping individuals incorporate these practices into their daily lives has been difficult to achieve.’
What each of us does in our daily lives profoundly affects the likelihood of developing chronic diseases, in general, and cardiovascular disease (CVD), in particular.1-10 Thousands of studies support the concept that regular physical activity, maintenance of a proper weight, sound nutritional practices, and avoiding tobacco products all significantly reduce the risk of CVD. The strength of the scientific literature supporting the health-promoting impact of positive daily habits and actions has been underscored by their inclusion in virtually every evidence-based clinical guideline addressing the prevention and treatment of metabolically related diseases.11-16 These principles are also incorporated in numerous documents and guidelines from both the American Heart Association (AHA)3,8,10,16 and the American College of Cardiology (ACC).9
Despite the overwhelming evidence in support of positive lifestyle measures, progress in helping individuals incorporate these practices into their daily lives has been difficult to achieve. While improvements in lifestyle measures have been cited as the major reason for the reduction in CVD in the past 20 years, major challenges remain. For example, between 1980 and 2000 the mortality rates from coronary heart disease (CHD) in the United States fell by more than 40%.17 Nonetheless, CVD remains the leading cause of worldwide mortality. In the United States, CVD results in more than 37% of annual mortality. While almost half of the reduction in CVD between 1980 and 2000 has been attributed to improvement in lifestyle-related risk factors such as smoking cessation, increased physical activity, and better control of cholesterol and blood pressure, it is important to note that increases in obesity and diabetes moved in the opposite direction and could potentially wipeout the gains achieved in other lifestyle-related risk factors unless progress can be made on these negative trends.17
Despite overwhelming evidence that lifestyle factors significantly affect short- and long-term health and quality of life, it has been frustratingly difficult to help patients adopt these habits and practices. For example, when the AHA released its Strategic Plan for 2020, it concluded that only 5% of individuals achieved “ideal cardiovascular health,” which involved a series of lifestyle factors such as regular physical activity, sound nutrition, weight management, and avoidance of tobacco as well as some cardiovascular health–related factors such as control of cholesterol, blood pressure, and glucose.3 Clearly, there are significant challenges ahead of us.
Within the past decade, the AHA and the ACC have been leaders in promoting the power of lifestyle habits and practices as key factors in promoting cardiovascular health. For example, in the AHA Strategic Plan the concept of “primordial” prevention (preventing risk factors from occurring in the first place) was introduced into the cardiovascular lexicon in addition to the construct of “ideal” cardiovascular health.3
While numerous studies have been published relating lifestyle factors to health and numerous constructs have been proposed, it appears that this discipline will coalesce under the concept of “lifestyle medicine.” For example, the AHA and ACC, in 2013, issued “Guidelines for Lifestyle Management to Reduce Cardiovascular Risk.”5 The Council within the AHA, which had previously been called “Council on Nutrition, Physical Activity and Metabolism,” in 2013, changed its name to the “Council on Lifestyle and Cardiometabolic Health.”8 A series of articles was published in 2011 in Circulation titled “Recent Advances in Preventive Cardiology and Lifestyle Medicine.”
These initiatives focus on reducing or treating CVD, largely through lifestyle endeavors, and also incorporate many of the principles from the Dietary Guidelines for Americans 2015-20204 and the Physical Activity Guidelines for Americans 2018.18 A nascent academic organization titled The American College of Lifestyle Medicine has been established and has doubled its membership every year for the past 5 years.19
I had the privilege of naming the field “lifestyle medicine” in the academic literature with the publication of my first, multiauthored textbook in this area in 1999 (Lifestyle Medicine, Blackwell Science, 1999).20 The third edition of this book will be published in 2019.21 In addition, I have the privilege of editing the only peer-reviewed academic journal in this area (The American Journal of Lifestyle Medicine).22 The construct of “lifestyle medicine” seems particularly appropriate since these habits and practices are clearly part of a positive lifestyle, and their health promoting benefits constitute a powerful approach to medicine and healing.
The current review attempts to summarize recent scientific literature related to how lifestyle habits and practices may be employed to lower the risk of CVD and frames this literature as “lifestyle medicine.”
Defining Cardiovascular Health
The Strategic Plan from the AHA for 2020, articulated the goal “by 2020 to improve the cardiovascular health of all Americans by 20%, while reducing deaths from CVD and stroke by 20%.”3 To achieve these goals the AHA outlined a series of steps, many of which depend on lifestyle modalities. The overall strategy was based on 3 pillars: (a) primordial prevention, (b) evidence that risk factors for CVD develop early in life, and (c) balancing individualized risk approaches with population level approaches.
The strategic plan also introduced the concept of primordial prevention, which incorporates strategies to avoid developing adverse levels of cardiovascular risk factors in the first place. It also outlined the concept of “ideal” cardiovascular health which was defined as a series of seven health behaviors and health factors, including not smoking, maintaining a healthy body mass index, achieving appropriate levels of physical activity, achieving a healthy diet, maintaining a total cholesterol of <200 mg/dL, maintaining a blood pressure of <120/80 mm Hg, and a maintaining a fasting glucose of <100 mg/dL. (The cholesterol, blood pressure and glucose parameters were all defined as “untreated” values.) The central role of lifestyle factors in virtually all of these seven factors provides the overall framework for the current review.
Lifestyle Strategies for Cardiovascular Health
Physical Activity
Physical inactivity represents a significant risk factor for CHD.18 Yet substantially fewer than half of adults meet even the minimum recommendation for regular aerobic exercise. Young people are even less likely to meet recommended standards, with fewer than 20% of adolescents performing the recommended 60 minutes or more of daily physical activity.23
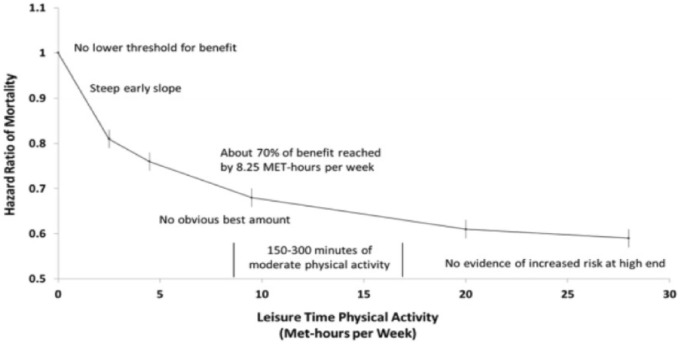
Compared with those who are very physically active, the risk of CHD in sedentary individuals is 150% to 240% higher.24 Only about 25% of all Americans engage in the minimum standards from the Centers for Disease Control and Prevention and the Physical Activity Guidelines for Americans 2018 guidance of at least 150 minutes per week of moderate intensity aerobic exercise or at least 75 minutes of vigorous exercise and muscle strengthening activities at least 2 days per week.25 As demonstrated in Figure 1 the greatest benefit in terms of reduction of risk of CHD appears to come to those engaging in even modest amount of physical activity compared to the most physically inactive.26
Figure 1.
Relationships of moderate-to-vigorous physical activity to all-cause mortality, with highlighted characteristics common to studies of this type.
Source: From the 2018 Physical Activity Guidelines Advisory Committee Scientific Report.18
These data suggest that even relatively small increases in physical activity could potentially result in a significant decrease in CHD for a large portion of the American population. Additional benefits from physical activity occur up to 150 to 300 minutes of moderate intensity physical activity and even further decreases in CHD occur for even substantially higher amounts of physical activity, although, as illustrated in the figure, the curve flattens above 150 minutes of moderate physical activity per week.
The 2018 Physical Activity Guidelines Advisory Committee report also emphasizes that physical activity significantly lowers the risk of adult weight gain and helps to control high blood pressure, while reducing the risk of developing hypertension in the first place.18 It should be noted that increasing amounts of physical activity also lower the risk of stroke and heart failure with a dose dependent relationship.
Despite the well-known benefits of physical activity, many physicians are not encouraging their patients to exercise. Furthermore, many physicians do not appear adequately prepared to provide recommendations for exercise and physical activity. In a survey of 175 primary care physicians only 12% were aware of the recommendations from the American College of Sports Medicine.27 Another survey of 51 internal medicine residents reported that 88% were confident in their knowledge of the benefits of exercise, but only 25% demonstrated adequate knowledge useful for patient counseling.28
In general, the relationship of physical activity to lipids is modest, although the 2013 AHA/ACC Guidelines for Lifestyle Management rated the evidence in this area as “moderate.”9 Regular exercise moderately increases high-density lipoprotein (HDL) cholesterol but has minimal effects on low-density lipoprotein (LDL) cholesterol.
The overall conclusions from the Physical Activity for Americans 2018 Advisory Committee emphasized that with regard to physical activity some was better than none and that those meeting the current guidelines of 150 minutes of moderate intensity physical activity or 75 minutes of vigorous physical activity per week achieved 75% of the maximum benefits.18 Additional physical activity results in greater benefit for CVD reduction, although the incremental benefit is less. These recommendations are consistent with the 2013 AHA/ACC Guidelines for Lifestyle Management to Reduce Cardiovascular Risk.9
Diet
Multiple studies have demonstrated that a diet containing more fruits and vegetables, fish (particularly, oily fish), whole grains and fiber, and maintaining a caloric balance lowers the risk of CVD.5,7,10,29 The nutritional guidelines offered by the AHA10 and other evidence-based documents such as the 2013 AHA/ACC Guidelines on Lifestyle Management to Reduce Cardiovascular Risk3 as well as the 2020 Strategic Plan for Improving Cardiovascular Health and Lowering Cardiovascular Risk as well as the report of the Dietary Guidelines Advisory Committee 2015-20204 are all very similar. In addition, all these guidelines place an emphasis not only on nutrition but also on a broader approach toward lifestyle factors to improve cardiovascular health and reduce the risk of CVD.
These consensus statements and guidelines consistently recommend a dietary pattern higher in fruits and vegetables, whole grains (particularly, high fiber), nonfat dairy, seafood, legumes, and nuts. The guidelines further recommend that those who consume alcohol (among adults) do so in moderation and are consistent in recommending diets lower in red and processed meats, refined grains, sugar-sweetened beverages, and saturated and trans fats. All these guidelines have also emphasized the importance of balancing calories and physical activity as a strategy for maintaining healthy weight and, thereby, reducing the risk of CVD.
Dietary guidance, over the past 20 years, has moved from specific foods and nutrients to a primary emphasis on dietary patterns. The following dietary patterns have all been recommended to lower the risk of CVD:
US healthy eating pattern
Low-fat diets
Mediterranean diet
DASH (Dietary Approaches to Stop Hypertension) diet
Vegetarian diet
Plant-based diets
There has been a recent surge in evidence and publications concerning “plant-based diets.” These diets are defined by an emphasis on plants, including fruits and vegetables. Low-fat diets, the Mediterranean diet, DASH diet, and vegetarian diets are all, in essence, plant-based diets since they emphasize fruits and vegetables and legumes and nuts, and limit the amount of red meat, processed meat, sweets, and oils.5,6,9,10
There has been some question about what actually constitutes a “plant-based” diet.30-34 A recent publication created a healthy plant-based diet index (hPBDI), where healthy plant foods (whole grains, fruits/vegetables, nuts/legumes, oils, tea, coffee) received positive scores and less healthy plant foods (juices/ sweetened beverages, refined grains, potatoes/fries, sweets, and animal foods) received adverse scores and were used to create an unhealthy plant-based diet index (uPBDI).35 This analysis of 93 329 women in the Nurses’ Health Study and Health Professionals Follow-up Study showed that diets that scored high in the hPBDI category substantially lowered CHD risk, whereas, foods in the uPBDI, which emphasized less healthy plant foods were associated with higher CHD risk. The interest in healthy plant-based diets offers an opportunity for further reduction in CVD.
Weight
Both overweight and obesity represent significant risk factors for CVD.1 The AHA lists obesity as a major risk factor for CVD not only because of its association with other risk factors (eg, diabetes, dyslipidemias, elevated blood pressure, metabolic syndrome) but also because it serves as an independent risk factor.36 Distribution of body fat also carries an additional risk since abdominal obesity is an independent risk factor for CHD.37 The accumulation of intra-abdominal fat promotes insulin resistance, which can lead to glucose intolerance, elevated triglycerides, and low HDL as well as hypertension.37
Recent estimates indicate that the prevalence of overweight (body mass index [BMI] 25-30 kg/m2) in the United States for adult women is 30% and for adult men approximately 40%.38 Estimates of obesity (BMI ⩾30 kg/m2) are currently 40% for women and approximately 35% for men. Within the obesity category severe obesity (BMI ⩾35 kg/m2) is approximately 16%.39 These prevalence figures constitute a significant public health concern because of their relationship of excess body fat to multiple chronic diseases, in general, and in CVD, in particular.
New guidelines were published in 2013 by the AHA and ACC and The Obesity Society to help clinicians manage obesity more effectively.40 These guidelines made 5 major recommendations, including the following:
Use BMI as a first step in establishing criteria to judge potential health risk.
Counsel patients that lifestyle changes can produce modest and sustained weight loss and achieve meaningful health benefits, while greater weight loss produces greater benefits.
Multiple dietary therapy approaches to weight loss are acceptable for weight loss. However, the diets should be prescribed to achieve reduced caloric intake.
Overweight or obese patients should be enrolled in comprehensive lifestyle interventions for weight loss delivered in programs of six months or longer.
Advice should be provided to patients who might be contemplating bariatric surgery (BMI ⩾40 kg/m2 or BMI ⩾30 kg/m2 with obesity-related comorbid conditions).
It is important to recognize that the key therapeutic modalities to treat weight gain and obesity are lifestyle based; namely, increased physical activity and sound nutrition. The large, National Institutes of Health–funded Look AHEAD (Action for Health and Diabetes) Trial showed that individuals who lost 7% of body weight significantly lowered all cardiovascular risk factors, except for LDL cholesterol levels.41 However, the rate of cardiovascular events was not reduced during the trial.
Smoking
Overwhelming evidence exists from multiple sources that cigarette smoking significantly increases the risk of both heart disease and stroke.42 This evidence has been extensively summarized elsewhere42 and is incorporated as a recommendation in the AHA 2020 Strategic Plan.3 Cigarette smoking in men is somewhat slightly more prevalent than in women, nearly 18 out of every 100 adult men (17.5%) still smoke, while nearly 14 out of 100 adult women (13.5%) still smoke cigarettes. The overall prevalence of cigarette smoking for adults 18 years of age or older is 15.5%.43 The health risks for cigarette smoking in women are equivalent to men. Conversely, substantial benefits of reduction in risk of CVD accrue in individuals who stop smoking cigarettes.44 These benefits occur over a very brief period of time. It should be noted that secondhand smoke also substantially increases the risk of CVD.42,44
Psychological Factors and Stress
Both the AHA 2020 Strategic Plan and the 2013 AHA/ACC Guidelines for Lifestyle Management were silent on psychological factors and stress. There is, however, a reasonably compelling body of literature that a variety of psychological factors may trigger both acute cardiac events and chronic increase in risk of CVD.45,46 Anxiety is the most prevalent chronic psychological condition with a lifetime incidence of more than 31%.47 Major depression has a lifetime incidence of approximately 10%.48 It has been reported that a third of individuals may experience enough stress in their daily lives to impact on their work or home performance. In addition, these factors may impact on adherence to medication and other lifestyle issues.49 Lifestyle modalities such as regular physical activity, mindfulness and relaxation response may prove effective in terms of treating these conditions.
Blood Pressure
Elevated blood pressure represents a significant risk factor for both CVD and stroke. Issues related to the optimum levels of blood pressure control have been somewhat controversial. The Joint National Commission VII (JNC VII) defined a normal blood pressure as <120/<80 mm Hg and defined 80 to 89 mm Hg diastolic and 120 to 139 mm Hg systolic as prehypertension. Levels >140 mm Hg systolic and >90 mm Hg diastolic were classified as “hypertension.”50 These recommendations were also incorporated into the AHA 2020 Strategic Plan.
The Commission established to formulate JNC VIII Guidelines came to somewhat different recommendations.51 JNC VIII recommended that individuals older than 60 years should be treated with blood pressure goals <150/90 mm Hg, and hypertensive individuals 30 to 69 years of age to a diastolic goal of <90 mm Hg. However, JNC VIII stated that there was insufficient evidence for hypertensive persons younger than 60 years to have an established systolic goal and those younger than 30 years for a diastolic goal. The panel recommended a blood pressure of <140/90 mm Hg for those groups based on expert opinion and relied on clinical judgement to make these decisions.
In 2017, the ACC/AHA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults established more stringent recommendations.11 These guidelines define a normal blood pressure as a systolic <120 mm Hg and diastolic <80 mm Hg. Elevated blood pressure was considered to be present with a systolic blood pressure 120 to 129 mm Hg and <80 mm Hg. Stage 1 hypertension was defined as blood pressure 130 to 139 mm Hg or 80 to 89 mm Hg while stage 2 hypertension was defined as systolic blood pressure >140 mg Hg or diastolic >90 mm Hg.
The more stringent blood pressure control guidelines were based largely on the results of the Systolic Blood Pressure Intervention Trial (SPRINT), which evaluated cardiovascular events in 9000 adults with the mean age of 67.9 years with baseline systolic blood pressure between 130 and 180 mm Hg.52 This study compared blood pressure targets of a systolic blood pressure of <120 mm Hg compared with a systolic target of <140 mm Hg and showed a significant lower all-cause mortality with the lower blood pressure target (hazard ratio 0.73, 95% CI 6-9, P = .003) and a significantly lower incidence (1.65% per year vs 2.919% per year) for the composite outcome (myocardial infarction, acute coronary syndrome, stroke, heart failure or death) compared with the standard treatment.
All 3 of these blood pressure recommendations highlighted the importance of lifestyle modalities that were also recommended in the 2013 AHA/ACC Lifestyle Management Guidelines,9 including
Consuming a diet high in vegetables, fruits, and whole grains, including low-fat dairy, poultry, fish, legumes, and nontropical vegetable oils and nuts, while limiting sweets, sugar, sugar-sweetened beverages, and red meat.
Consuming no more than 2400 mg of sodium per day.
Engaging in aerobic physical activity 3 to 4 sessions per week lasting an average of 40 minutes per session of moderate to vigorous intensity physical activity.
The 2013 AHA/ACC Strategic Guidelines for Lifestyle Management additionally recommended that individuals should attempt to achieve a further reduction of sodium intake to 1500 mg per day since a further reduction in blood pressure can occur at this level of sodium consumption.
Lipids
Dietary management of blood lipids has been a mainstay, along with pharmaceutical therapy, for many years.2,10 The 2013 AHA/ACC Lifestyle Medicine Guidelines for Nutrition, as a component of managing blood lipids, advocates a diet consisting of vegetables, fruits, and whole grains, including low-fat dairy products, poultry, fish, legumes, nontropical vegetable oils, and nuts, while limiting sweets, sugar-sweetened beverages, and red meat.9 This is the same dietary pattern that is recommended to lower blood pressure. These guidelines also emphasize adapting this dietary pattern to the appropriate caloric requirements as well as personal and cultural food preferences while also advocating medical nutritional therapy (MNT) for other medical conditions (including diabetes mellitus). The food patterns recommended to achieve this pattern include the DASH dietary pattern, the US Department of Agriculture’s Healthy Food Pattern4 and the AHA diet.2,10 The evidence for these interventions to help control lipids was considered to be “strong.”
Blood Glucose/Diabetes
Diabetes is a recognized and significant risk factor for CVD.53 CVD is the leading cause of morbidity and mortality among individuals with diabetes. Lifestyle therapies, including proper nutrition and regular physical activity, are key therapeutic modalities to reduce the risk of CVD in individuals with diabetes.
The American Diabetes Association recommends that individuals with diabetes and hypertension should be treated to a systolic blood pressure goal of <140 mm Hg and a diastolic blood pressure of <90 mm Hg.54 The 2017 Guidelines for Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults issued by the ACC and AHA recommend the blood pressure goal of <130/80 mm Hg in individuals with diabetes.11
Lifestyle modalities are a cornerstone treatment for diabetes care, including MNT, physical activity, smoking cessation, counseling, psychosocial care, and diabetes self-management education support.
MNT promotes healthy eating patterns emphasizing a variety of nutrient dense foods at appropriate levels with the goal of achieving and maintaining healthy body weight, maintaining individual glycemic control and lipid goals to delay or prevent complications from diabetes. There is not one ideal percentage of calories from carbohydrates, protein, or fat recommended for all people with diabetes. Eating patterns that are recommended include Mediterranean, DASH, and other plant-based diets.55
Weight management and, if necessary, reduction of weight, is important for overweight or obese people with diabetes. In the Look AHEAD Trial individuals who lost an average of 7% of body weight reduced all of their cardiovascular risk factors, except for LDL cholesterol level.
Regular physical activity is also vitally important for managing diabetes. Aerobic activity should be ideally at least 10 minutes per session with the goal of 30 minutes per day or more on most days of the week. Individuals with diabetes should also be encouraged to reduce sedentary activities such as working at a computer, watching TV, and so on, or break up the sedentary activities by briefly standing, walking, or performing light physical activity.
Metabolic Syndrome
The metabolic syndrome is a cluster of metabolic abnormalities that significantly increases the risk of CVD.55-57 It is estimated that between 36% and 38% of the adult population in the United States has metabolic syndrome.56,57 While various definitions exist for the metabolic syndrome, they have in common insulin resistance leading to hyperglycemia, elevated blood pressure, elevated triglycerides, and depressed HDL cholesterol. Increased abdominal obesity is an underlying factor in many of these metabolic abnormalities. Since most of CHD occurs in individuals with multiple risk factors it is important to treat the metabolic syndrome. Indeed, the ATP III Guidelines recommend that individuals with metabolic syndrome be treated as though they already have CHD.58 Lifestyle therapies constitute the core intervention for individuals with the metabolic syndrome. These include proper nutrition (following DASH or Mediterranean or comparable diet), regular physical activity (30 minutes or more on most if not all days of moderate intensity) and weight loss, if necessary. The recommendations for treatment of lipids and blood pressure for individuals with the metabolic syndrome are comparable to those individuals with diabetes.
Brain Health
Brain health and cognitive function are important components of healthy aging and predict quality of life and functional independence. Cardiovascular risk factors are closely associated with cognitive impairment and dementia. For this reason, the AHA and American Stroke Association (ASA) have released a Presidential Advisory titled “Defining Optimal Brain Health in Adults.”59 The purpose of this initiative was to provide the definition of optimal brain health and guidance of how to maintain it. Seven metrics were identified as components of optimal brain health and largely reflect the metrics for cardiovascular health in the AHA 2020 Strategic Plan.3 These include 4 ideal health behaviors (nonsmoking, physical activity at goal levels, a healthy diet consisting of current AHA guidelines, and body mass index <25 kg/m2). Three ideal health factors (untreated blood pressure <120/<80 mm Hg, untreated total cholesterol <200/mg/dL, and fasting blood glucose <100 mg/dL) were also recommended. Since these factors were all identified in the AHA 2020 Strategic Plan previous discussion of how lifestyle measures can positively affect all of these parameters has already been outlined in this review.
Behavioral Strategies and Adherence
The lifestyle strategies presented in this review for reduction of risk for CVD in many instances involve changes in behavior. Thus, it is important for physicians and other health care professionals to understand and use effective behavioral strategies as a key underlying component for overall lifestyle management. Multiple frameworks for behavioral change have been outlined and reviewed elsewhere in detail.60 A comprehensive review of these behavioral frameworks is beyond the scope of the current review.
Adherence to positive lifestyle factors also remains a challenging area. As already indicated, the AHA 2020 Strategic Plan concludes less than 5% of adults currently exhibit all the behaviors and health factors that the AHA has defined as “ideal cardiovascular health.” Furthermore, recent Scientific Statements from the AHA have emphasized the importance of implementing behavioral guidelines and emphasized that individual, familial, community, national, and other influences all affect the likelihood of individuals making positive behavior changes.61 Finding ways to enhance adherence to known risk factor reduction strategies represents an important challenge for the future of cardiovascular risk reduction.
Reduction of Cardiovascular Disease in Children and Adolescents
Many of the aspects of CVD that are manifested in adulthood have their roots in childhood.62 Recently, risk factors for heart disease in children and adolescents have significantly risen. In particular, there has been significant increase in both dyslipidemias63 and hypertension15 as well as dramatic increases in the prevalence of overweight and obesity.64
While a detailed review of these increasingly prevalent risk factors for CVD in children and adolescents is beyond the scope of this review, the same types of lifestyle measures that are applicable for the prevention and treatment of CVD in adults are highly relevant to children. Good information on physical activity in children can be found in the recently revised Physical Activity Guidelines for American 2018. Nutritional guidance from the 2015-2020 Dietary Guidelines for Americans is also highly appropriate for children and consistent with AHA recommendations. Since many of the lifestyle medicine modalities employed in adults are highly relevant to families, issues related to nutrition, physical activity, and weight management are all appropriate to be addressed in the family setting.
Summary/Conclusions
Daily habits and actions profoundly affect the likelihood of developing CVD. Increased physical activity, proper nutrition, weight management, avoidance of tobacco, and stress reduction are all key modalities that both lower the risk of CVD and enhance quality of life.
It is incumbent on physicians and other health care professionals to be leaders in identifying positive lifestyle measures as important strategies for lowering the risk of CVD or treating it if already present. Yet, despite multiple efforts on the part of the medical community, helping our patients adopt positive lifestyle factors remains a challenge. If we are to accomplish the goals of the 2020 AHA Strategic Plan of reducing CVD by 20%, lifestyle modalities will play a key role.
The purpose of this review has been to summarize the evidence of multiple lifestyle factors which impact on CVD. This discipline has coalesced under the framework of “lifestyle medicine.” This is an area where the medical community must continue to play a leading role if we are ever to meet the challenges of continuing to lower the risk of all forms of heart disease.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Rippe is Editor-in-Chief of the American Journal of Lifestyle Medicine (SAGE) and Editor-in-Chief of the comprehensive academic textbook Lifestyle Medicine (CRC Press, third edition to be published in spring, 2019). Dr Rippe’s research organization, Rippe Lifestyle Institute, has conducted numerous research studies in various aspects of lifestyle medicine, including physical activity, proper nutrition, and weight management and their impact on short- and long-term health and quality of life.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
References
- 1. Rippe JM. Lifestyle medicine: the health promoting power of daily habits and practices [published online July 20, 2018]. Am J Lifestyle Med. doi: 10.1177/1559827618785554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S1-S45. [DOI] [PubMed] [Google Scholar]
- 3. Lloyd-Jones DM, Hong Y, Labarthe D, et al. ; American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010:121:586-613. [DOI] [PubMed] [Google Scholar]
- 4. US Department of Health and Human Services; US Department of Agriculture. Dietary guidelines for Americans, 2015-2020. 8th ed. http://health.Gov/dietaryguidelines/2015/guidelines/. Published December 2015. Accessed October 26, 2018.
- 5. Mozaffarian D, Appel LJ, Van Horn L. Components of a cardioprotective diet: new insights. Circulation. 2011;123:2870-2891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Estruch R, Ros E, Salas-Salvadó J, et al. ; PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279-1290.23432189 [Google Scholar]
- 7. Chiuve SE, McCullough ML, Sacks FM, Rimm EB. Healthy lifestyle factors in the primary prevention of coronary heart disease among men: benefits among users and nonusers of lipid-lowering and antihypertensive medications. Circulation. 2006;114:160-167. [DOI] [PubMed] [Google Scholar]
- 8. American Heart Association. Council on Lifestyle and Cardiometabolic Health. https://professional.heart.org/professional/MembershipCouncils/ScientificCouncils/UCM_322856_Council-on-Lifestyle-and-Cardiometabolic-Health.jsp. Accessed September 19, 2018.
- 9. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S76-S99. [DOI] [PubMed] [Google Scholar]
- 10. American Heart Association Nutrition Committee; Lichtenstein AH, Appel LJ, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006:114:82-96. [DOI] [PubMed] [Google Scholar]
- 11. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/ABC/ACPM/AGS/ APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269-1324. [DOI] [PubMed] [Google Scholar]
- 12. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143-3421. [PubMed] [Google Scholar]
- 13. Glickman D, Parker L, Sim L, Del Valle Cook H, Miller E. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 14. American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes—2018. Diabetes Care. 2018;41(suppl 1):S13-S27. [DOI] [PubMed] [Google Scholar]
- 15. Flynn JT, Kaelber DC, Baker-Smith CM, et al. ; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904. [DOI] [PubMed] [Google Scholar]
- 16. Eyre H, Kahn R, Robertson RM, et al. Preventing cancer, cardiovascular disease, and diabetes: a common agenda for the American Cancer Society, the American Diabetes Association, and the American Heart Association. Circulation. 2004;109:3244-3255. [DOI] [PubMed] [Google Scholar]
- 17. Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in US deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356:2388-2398. [DOI] [PubMed] [Google Scholar]
- 18. Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington DC: US Department of Health and Human Services; 2018. [Google Scholar]
- 19. American College of Lifestyle Medicine. Home page. https://www.lifestylemedicine.org/. Accessed September 19, 2018.
- 20. Rippe JM, O’Brien D. The rationale for intervention to reduce the risk of coronary artery disease. In Rippe JM, ed. Lifestyle Medicine. Boston, MA: Blackwell Science; 1999. [Google Scholar]
- 21. Rippe JM. Lifestyle Medicine. 3rd ed. Boca Raton, FL: CRC Press; 2019. [Google Scholar]
- 22. Rippe JM, ed. American Journal of Lifestyle Medicine. Thousand Oaks, CA: Sage; http://journals.sagepub.com/home/ajl. Accessed September 19, 2018. [Google Scholar]
- 23. Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance System (YRBSS). https://www.cdc.gov/healthyyouth/data/yrbs/index.htm. Accessed September 19, 2018.
- 24. Writing Group Members; Mozaffarian D, Benjamin EJ, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133:e38-e360. [DOI] [PubMed] [Google Scholar]
- 25. Centers for Disease Control and Prevention. Adult participation in aerobic and muscle-strengthening physical activities—United States, 2011. MMWR Morb Mortal Wkly Rep. 2013;62:326-330. [PMC free article] [PubMed] [Google Scholar]
- 26. Moore SC, Patel AV, Matthews CE, et al. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med. 2012;9:e1001335. doi: 10.1371/journal.pmed.1001335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Walsh JM, Swangard DM, Davis T, McPhee SJ. Exercise counseling by primary care physicians in the era of managed care. Am J Prev Med. 1999;16:307-313. [DOI] [PubMed] [Google Scholar]
- 28. Rogers LQ, Gutin B, Humphries MC, et al. Evaluation of internal medicine residents as exercise role models and associations with self-reported counseling behavior, confidence, and perceived success. Teach Learn Med. 2006;18:215-221. [DOI] [PubMed] [Google Scholar]
- 29. Bassuk SS, Manson JE. Lifestyle and risk of cardiovascular disease and type 2 diabetes in women: a review of the epidemiologic evidence. Am J Lifestyle Med. 2008;2:191-213. [Google Scholar]
- 30. Williams KA, Sr, Patel H. Healthy plant-based diet. What does it really mean? J Am Coll Cardiol. 2017;70:423-425. [DOI] [PubMed] [Google Scholar]
- 31. Fraser GE. Vegetarian diets: what do we know of their effects on common chronic diseases? Am J Clin Nutr. 2009;89:1607S-1612S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hu FB, Willett WC. Optimal diets for prevention of coronary heart disease. JAMA. 2002;288:2569-2578. [DOI] [PubMed] [Google Scholar]
- 33. Freeman AN, Morris PB, Barnard N, et al. Trending cardiovascular nutrition controversies. J Am Coll Cardiol. 2017;69:1172-1187. [DOI] [PubMed] [Google Scholar]
- 34. McEvoy CT, Temple N, Woodside JV. Vegetarian diets, low-meat diets and health: a review. Public Health Nutr. 2012;15:2287-2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Satija A, Bhupathiraju SN, Spiegelman D, et al. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in US adults. J Am Coll Cardiol. 2017;70:411-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Eckel RH, Krauss RM. American Heart Association call to action: obesity as a major risk factor for coronary heart disease. AHA Nutrition Committee. Circulation. 1998;97:2099-2100. [DOI] [PubMed] [Google Scholar]
- 37. Després JP. Abdominal obesity as important component of insulin-resistance syndrome. Nutrition. 1993;9:452-459. [PubMed] [Google Scholar]
- 38. Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315:2284-2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-Term Trends in Health. Hyattsville, MD: National Center for Health Statistics; 2017. [PubMed] [Google Scholar]
- 40. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Obesity Society. J Am Coll Cardiol. 2014;63(25 pt B):2985-3023. [DOI] [PubMed] [Google Scholar]
- 41. Look AHEAD Research Group;Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369:145-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. US Office of the Surgeon General; US Office on Smoking and Health. The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 2004. [Google Scholar]
- 43. Centers for Disease Control and Prevention. Current cigarette smoking among adults in the United States. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm. Accessed September 19, 2018.
- 44. Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368:341-350. [DOI] [PubMed] [Google Scholar]
- 45. Mittleman MA, Mostofsky E. Physical, psychological and chemical triggers of acute cardiovascular events: preventive strategies. Circulation. 2011;124:346-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Stuart-Shor EM, Berra KA, Kamau MW, Kumanyika SK. Behavioral strategies for cardiovascular risk reduction in diverse and underserved racial/ethnic groups. Circulation. 2012;125:171-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21:169-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. National Institute of Mental Health. Major depression. https://www.nimh.nih.gov/health/statistics/major-depression.shtml. Accessed September 17, 2018.
- 49. Ockene JK, Schneider KL, Lemon SC, Ockene IS. Can we improve adherence to preventive therapies for cardiovascular health? Circulation. 2011;124:1276-1282. [DOI] [PubMed] [Google Scholar]
- 50. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood pressure: the JNC 7 report. JAMA. 2003;289:2560-2572. [DOI] [PubMed] [Google Scholar]
- 51. Armstrong C; Joint National Committee. JNC 8 guidelines for the management of hypertension in adults. Am Fam Physician. 2014;90:503-504. [PubMed] [Google Scholar]
- 52. SPRINT Research Group; Wright JT, Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. American Diabetes Association. 9. Cardiovascular disease and risk management. Diabetes Care. 2017;40(suppl 1):S75-S87. doi: 10.2337/dc17-S012 [DOI] [PubMed] [Google Scholar]
- 54. American Diabetes Association. 4. Lifestyle management: Standards of Medical Care in Diabetes—2018. Diabetes Care. 2018;41(suppl 1):S38-S50. doi: 10.2337/dc18-S004 [DOI] [PubMed] [Google Scholar]
- 55. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Curr Opin Cardiol. 2006;21:1-6. [DOI] [PubMed] [Google Scholar]
- 56. Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the Third National Health and Nutrition Examination Survey. JAMA. 2002;287:356-359. [DOI] [PubMed] [Google Scholar]
- 57. American Heart Association; American Stroke Association. AHA/ASA presidential advisory. http://www.heart.org/HEARTORG/Professional/FocusonQuality/e-Communications/AHAASA-Presidential-Advisory_UCM_460822_Article.jsp?appName=MobileApp. Accessed September 19, 2018.
- 58. US Department of Health and Human Services; Public Health Service; National Institutes of Health; National Heart, Lung, and Blood Institute. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Executive summary. https://www.nhlbi.nih.gov/files/docs/guidelines/atp3xsum.pdf; 2001 NIH Publication No. 01-3670. Published May 2001. Accessed October 27, 2018.
- 59. Gorelick PB, Furie KL, Iadecola C, et al. ; American Heart Association/American Stroke Association. Defining optimal brain health in adults: a presidential advisory from the American Heart Association/American Stroke Association. Stroke. 2017;48:e284-e303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Linke SE, Robinson CJ, Pekmezi D. Applying psychological theories to promote healthy lifestyles. Am J Lifestyle Med. 2014;8:4-14. [Google Scholar]
- 61. Gidding SS, Lichtenstein AH, Faith MS, et al. Implementing American Heart Association pediatric and adult nutrition guidelines: a scientific statement from the American Heart Association Nutrition Committee of the Council on Nutrition, Physical Activity and Metabolism, Council on Cardiovascular Disease in the Young, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiovascular Nursing, Council on Epidemiology and Prevention, and Council for High Blood Pressure Research. Circulation. 2009;119:1161-1175. [DOI] [PubMed] [Google Scholar]
- 62. Kavey RE, Daniels SR, Lauer RM, et al. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. J Pediatr. 2003;142:368-372. [DOI] [PubMed] [Google Scholar]
- 63. Kavey RE, Allada V, Daniels SR, et al. Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association Expert Panel on Population and Prevention Science; the Councils on Cardiovascular Disease in the Young, Epidemiology and Prevention, Nutrition, Physical Activity and Metabolism, High Blood Pressure Research, Cardiovascular Nursing, and the Kidney in Heart Disease; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. J Cardiovasc Nurs. 2007;22:218-253. [DOI] [PubMed] [Google Scholar]
- 64. Krebs NF, Jacobson MS; American Academy of Pediatrics Committee on Nutrition. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424-430. [DOI] [PubMed] [Google Scholar]