Abstract
Background
The Barrel vascular reconstruction device is an electrolytically detachable laser-cut closed-cell stent used for neck reconstruction in wide-necked bifurcation aneurysms to support coiling without necessitating dual stent implantation. The purpose is to lower the metal-to-artery ratio and its inherent risk of thromboembolic complications of multiple stents.
Case description
A 53-year-old woman presenting with subarachnoid hemorrhage due to acutely ruptured basilar tip aneurysm underwent emergency endovascular embolization with the Barrel vascular reconstruction device. Since the stent did not cover the entire neck of the aneurysm, an Atlas stent was released in a Y configuration through the Barrel. The Neuroform Atlas correctly opened through the Barrel and allowed the complete exclusion of the aneurysm.
Conclusion
If necessary, releasing a Neuroform Atlas through a Barrel vascular reconstruction device is a feasible technique.
Keywords: Barrel VRD stent, Neuroform Atlas stent, innovative biotechnologies, bifurcation stent, subarachnoid hemorrhage, intracranial ruptured aneurysm, wide-necked aneurysm
Introduction
Acutely ruptured wide-necked intracranial aneurysms are still technically challenging.1 Many endovascular techniques have been described to treat these lesions, including balloon-assisted coiling2 and double microcatheter techniques;3 however, these techniques lack permanent coil support inside the aneurysm sac, which may lead to coil prolapse or migration after the procedure.
For these reasons, when complex anatomy does not allow standard coiling, a device is implanted.
The Barrel stent (Barrel vascular reconstruction device (VRD), Medtronic, Minneapolis, MN, USA) is a self-expandable, laser-cut, fully retrievable nitinol stent featuring a bulged centre section that herniates over the ostium of the aneurysm sac to facilitate coiling. The device has 12 radio-opaque platinum markers that allow an easier positioning of the device: one at the proximal tip, one proximal and one distal centre marker, six markers at the ‘barrel’ section (to enhance device visualization during its deployment across the aneurysm neck) and three distal tip markers.4 It is designed to treat wide-necked bifurcation aneurysms without the need of a second stent and, as a result, to lower the metal-to-artery ratio and its inherent risk of thromboembolic complications of multiple stents.5,6
The Neuroform Atlas (Stryker Neurovascular, Fremont, USA) is a self-expanding nitinol stent with a mixed open-/closed-cell design that can be delivered through standard coiling catheters down to an inner diameter of 0.0165 inches.
To our knowledge, the feasibility of opening a Neuroform Atlas through the Barrel’s mesh for the treatment of a wide-necked bifurcation aneurysm is not reported in the literature.
Case description
A 53-year-old Caucasian woman was admitted to our emergency department at 1 hour from the onset of severe headache, right hemiplegia and mild left anisocoria. Her social history was notable for arterial hypertension and occasional alcohol use. There was no family history of aneurysms or vascular diseases.
The patient underwent brain computed tomography (CT) that showed a Fisher grade 4 subarachnoid hemorrhage (SAH) and a small left thalamic hemorrhagic infarction. The CT angiography showed a 10 mm large wide-necked basilar tip aneurysm (BTA), a 10 mm partially calcified left middle cerebral artery (MCA) aneurysm and a small right superior cerebellar artery (SCA) aneurysm. Due to a rapid deterioration of the clinical condition, the patient was rapidly intubated and transferred to the angiographic suite.
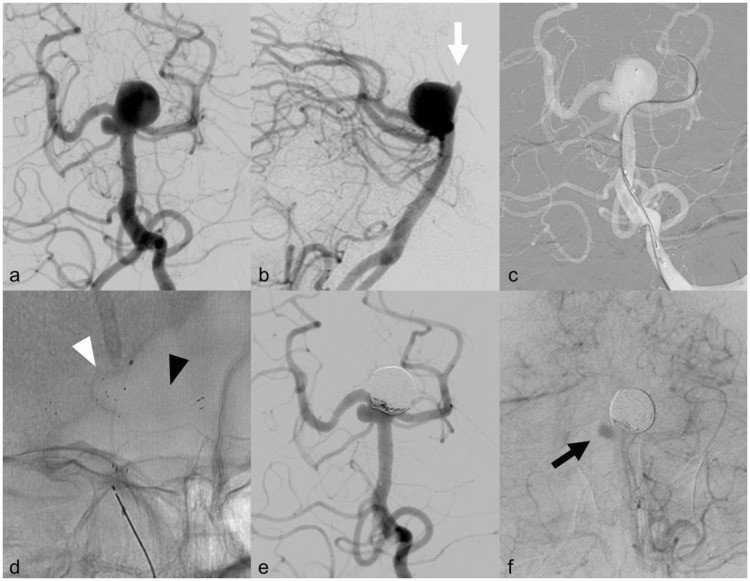
Under general anesthesia, after bilateral femoral access (right 6-Fr; left 5-Fr), a preliminary cerebral digital subtraction angiography (DSA) was performed and showed a wide-necked BTA (diameter: 11 mm; neck: 8.5 mm, Figure 1(a)) with an antero-cranial lobe (Figure 1(b)), a 4 mm sacciform right SCA aneurysm and a 9 mm partially calcified left MCA aneurysm.
Figure 1.
Endovascular procedure. (a) Frontal view of the basilar tip aneurysm during left vertebral artery injection. Please note the small right superior cerebellar artery (SCA) aneurysm; (b) lateral view of the basilar aneurysm during left vertebral artery injection showing the antero-cranial bleb (white arrow); (c) frontal view (roadmap) during left vertebral artery injection showing the microcatheter in the left posterior cerebral artery (PCA). Please note the Barrel stent already implanted from the left P1 segment to the basilar trunk and the microcatheter inside the sac. (d) Unsubtracted frontal view of the two stents deployed (white arrowhead: Barrel vascular reconstruction device (VRD); black arrowhead: Atlas stent) and the microcatheter inside the sac; (e) frontal view of the basilar aneurysm after left vertebral artery injection at the end of the embolization showing the complete exclusion of the sac. (f) Frontal view of the right SCA aneurysm after left vertebral artery injection. Please note the contrast media stagnation inside the sac as a mild flow-diversion effect.
Considering the distribution of the SAH, we decided to treat the BTA. Because the neck was considered too large for either an unassisted or a balloon-assisted coiling, the double microcatheter technique would have been a valid option. However, we thought it would not have been able to prevent coils from protrusion. Therefore, we proceeded to treat the aneurism with a stent-assisted technique.
A 6-Fr guiding catheter was placed in the vertebral artery (VA) and a 5-Fr guiding catheter in the contralateral VA. A BV-4070 Barrel stent (proximal end diameter: 4.0 mm; distal end diameter: 3.5 mm; Barrel diameter: 7.5 mm; Barrel length: 7.0 mm; usable length: 21 mm) was released with a Headway 21 microcatheter (Microvention, Tustin, CA) from the right P1 to the basilar trunk. The bulged centre section of the stent correctly opened in the planned location; however, the mesh did not sufficiently cover the aneurysm’s neck to allow a safe coiling of the sac.
An Echelon 10 microcatheter (Medtronic, Irvine, CA, USA) on a Synchro 0.14 guidewire (Stryker Neurovascular, Fremont, USA) was used to pass through the Barrel mesh and catheterize the arterial branch (Figure 1(c)). A 4x21 mm Neuroform Atlas stent was released through the Barrel from the left P1 segment to the basilar trunk in an Y configuration (Figure 1(d)). The same microcatheter was then used to release coils within the aneurysm. The two stents implanted allowed the complete embolization of the aneurysms (Raymond-Roy class I7) with a total of 10 coils (Figure 1(e)). Final DSA showed no angiographic complications and an unexpected mild flow-diversion effect in the right SCA aneurysms due to the presence of the two overlaid stents (Figure 1(f)).
The patient received heparin 5000 IU iv bolus after femoral puncture and acetylsalicylic acid (ASA) 500 mg after the release of the Barrel VRD. Double antiplatelet therapy was administered from the next day on.
Head CT performed 24 hours later showed a mild enlargement of the thalamic hemorrhagic infarction. No clinical change was noticed. Then 13 days after the procedure the patient developed a right frontal intraparenchymal hematoma; clopidogrel administration was therefore reduced to 75 mg every two days. Finally, 19 days after the procedure the patient died due to a huge intraparenchymal haemorrhage that developed inside the left thalamus, at the same point in which we first described it.
Discussion
Wide-necked bifurcation aneurysms are still a matter of debates. Unassisted coiling, balloon-assisted and single-stent techniques are frequently insufficient to protect the daughter vessels and to prevent coil protrusion leading to arterial occlusion.8
Some preliminary studies described the use of new alternative devices to treat wide-necked bifurcation aneurysms, such as the WEB-DL braided wire intrasaccular flow diverter (Sequent Medical, Aliso Viejo, CA, USA),9 the PulseRider stent (Pulsar Vascular, San Jose, CA, USA),10 and the pCONus self-expanding nitinol intrasaccular stent (Phenox, Bochum, Germany).11 These stents have had some success; however, procedural limitations and recanalization rates are significant.12,13
Y-stent-assisted coiling has been described as a feasible technique for treating a subset of challenging bifurcation aneurysms. Y-stenting is performed by placing two stents in the parent artery with each stent in one of the bifurcation branches, creating a new bifurcation point across the neck of the aneurysm.14 This technique offers many advantages in aneurysm remodeling such as support to prevent coil protrusion, a blood flow-diversion effect, a scaffold for neo-endothelization, modification of the parent vessel-aneurysm geometry and remodeling of the affected branches.15,16 It allows the complete exclusion of the aneurysms in 92.3% of cases,14 with a complication rate between 11 and 31.6%,17,18 most of which related to thromboembolic events. However, a comparison study between unassisted coiling, single-stent assisted-coiling and Y-stent coiling of BTA showed similar percentages of thromboembolic complications (respectively 6.8%, 6.9% and 6.2%) with higher complication rate (respectively 9.5%, 9.7% and 6.2%) and recanalization rate (respectively 38.9%, 19.2% and 8.3%) in single-stent assisted coiling.19
However, stent placement is generally avoided in acutely ruptured aneurysms because of the higher risk of thromboembolic events. Ko et al.20 described a 25% rate of acute in-stent thrombosis (IST) in a series in which most patients were treated with Y-stenting after the failure of other neck remodeling techniques. Furthermore, most operators are reluctant to use antiplatelet therapy in patients with SAH because of the potential need for a ventriculostomy and the potential for infarction secondary to vasospasm.21 Nonetheless, several studies have reported safe, successful treatment of ruptured aneurysms with stent-assisted techniques.22 Moreover, some anatomic conditions require the use of devices, even in an emergency setting.
In our case, the aneurysm’s broad neck did not seem to be suitable for unassisted coiling and its location made neurosurgical clipping difficult. Balloon-assisted coiling and the double-microcatheter technique, although feasible, were not judged adequate to contain the coils inside the sac.
To reduce the amount of metal implanted in an emergency setting, we intended to use only one stent. The Barrel VRD was judged appropriate for this purpose. However, after the deployment of the stent, we realized that the Barrel’s dilated central portion was not able to protect the whole neck and the risk of coil migration was high. The use of another stent was deemed necessary. The Atlas is an opened-cell stent that can be delivered with a 0.0165-inch microcatheter; this feature allows an easier and smoother passage through the Barrel’s mesh and the consequent catheterization of a hardly accessible left posterior cerebral artery. Furthermore, the same microcatheter was used to pass through both stents to release coils inside the sac.
In our institution, we usually do not administer a loading dose of clopidogrel 300 mg if the CT head scan shows any intraparenchymal hematoma, to prevent its extension through the brain. However, we believe as other authors do23 that intravenous application of ASA is feasible and safe during interventional aneurysm treatment both in unruptured aneurysms and after SAH.
To our knowledge, Y-configured stent-assisted coiling with Barrel VRD and Atlas has never been reported. Conversely, experiences of deploying a stent through another previously implanted device have already been described.24
Conclusions
The deployment of an Atlas stent through a Barrel VRD is a feasible technique for treating very selected acutely ruptured wide-necked aneurysms not suitable for unassisted coiling, remodelling or the double-microcatheter technique.
The Atlas stent can be delivered with a 0.0165-inch microcatheter. This is the key feature that allows an easier catheterization of anatomically difficult daughter vessels and a smoother passage through a previously implanted stent mesh.
We do not have enough data to verify the durability of this procedure. However, we assess that this technique allowed a complete coiling of the sac without displacing the previously implanted Barrel VRD and avoiding coils from prolapse in the parent vessels.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Yang P, Zhao K, Zhou Y, et al. Stent-assisted coil placement for the treatment of 211 acutely ruptured wide-necked intracranial aneurysms: A single-center 11-year experience. Radiol 2015; 276: 545–552. [DOI] [PubMed] [Google Scholar]
- 2.Moret J, Cognard C, Weill A, et al. The ‘remodelling technique’ in the treatment of wide neck intracranial aneurysms. Angiographic results and clinical follow-up in 56 cases. Interv Neuroradiol 1997; 3: 21–35. [DOI] [PubMed] [Google Scholar]
- 3.Wen HF, Zhao CX, Li JL, et al. Double microcatheter technique for detachable coil treatment of wide-necked and irregular intracranial aneurysms. J Interv Radiol 2012; 21: 890–892. [Google Scholar]
- 4.Kabbasch C, Mpotsaris A, Maus V, et al. The Barrel vascular reconstruction device: A retrospective, observational multicentric study. Clin Neuroradiol 2018; 17–23. [DOI] [PubMed]
- 5.Piotin M, Berge J, Turjman F, Blanc R. The Barrel VRD vascular reconstruction device for the treatment of wide-neck bifurcation aneurysms. J NeuroIntervent Surg 2015; 7 (Suppl 1: A1–114). [Google Scholar]
- 6.Mühl-Benninghaus R, Simgen A, Reith W, et al. The Barrel stent: New treatment option for stent-assisted coiling of wide-necked bifurcation aneurysms: Results of a single-center study. J Neurointerv Surg 2017; 9: 1219–1222. [DOI] [PubMed] [Google Scholar]
- 7.Mascitelli JR, Moyle H, Oermann EK, et al. An update to the Raymond–Roy Occlusion Classification of intracranial aneurysms treated with coil embolization. J Neurointerv Surg 2015; 7: 496–502. [DOI] [PubMed] [Google Scholar]
- 8.Mukherjee S, Chandran A, Gopinathan A, et al. PulseRider-assisted treatment of wide-necked intracranial bifurcation aneurysms: Safety and feasibility study. J Neurosurg 2016; 127 : [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 9.Pierot L, Klisch J, Liebig T. WEB-DL Endovascular treatment of wide-neck bifurcation aneurysms: Long-term results in a European series. AJNR Am J Neuroradiol 2015; 36: 2314–2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gory B, Spiotta AM, Mangiafico S, et al. PulseRider stent-assisted coiling of wide-neck bifurcation aneurysms: Periprocedural results in an international series. Am J Neuroradiol 2016; 37: 130–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gory B, Aguilar-Pérez M, Pomero E, et al. PCONus device for the endovascular treatment of wide-neck middle cerebral artery aneurysms. Am J Neuroradiol 2015; 36: 1735–1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cognard C, Januel AC. Remnants and recurrences after the use of the WEB intrasaccular device in large-neck bifurcation aneurysms. Neurosurgery 2015; 76: 522–530. [DOI] [PubMed] [Google Scholar]
- 13.Lubicz B, Morais R, Alghamdi F, et al. The pCONus device for the endovascular treatment of wide neck bifurcation aneurysms. J Neurointerv Surg 2016; 8: 940–944. [DOI] [PubMed] [Google Scholar]
- 14.Limbucci N, Renieri L, Nappini S, et al. Y-stent assisted coiling of bifurcation aneurysms with Enterprise stent: Long-term follow up. J Neurointerv Surg 2016; 8: 158–162. [DOI] [PubMed] [Google Scholar]
- 15.Melber K, Meila D, Draheim P, et al. Vascular angular remodeling by kissing-Y stenting in wide necked intracranial bifurcation aneurysms. J Neurointerv Surg 2017; 9: 1233–1237. [DOI] [PubMed] [Google Scholar]
- 16.Wanke I, Forsting M. Stents for intracranial wide-necked aneurysms: More than mechanical protection. Neuroradiol 2008; 50: 991–998. [DOI] [PubMed] [Google Scholar]
- 17.Fargen KM, Mocco J, Neal D, et al. A multicenter study of stent-assisted coiling of cerebral aneurysms with a Y configuration. Neurosurg 2013; 73: 466–472. [DOI] [PubMed] [Google Scholar]
- 18.Spiotta AM, Gupta R, Fiorella D, et al. Mid-term results of endovascular coiling of wide-necked aneurysms using double stents in a Y configuration. Neurosurg 2011; 69: 421–429. [DOI] [PubMed] [Google Scholar]
- 19.Chalouhi N, Jabbour P, Gonzalez LF, et al. Safety and efficacy of endovascular treatment of basilar tip aneurysms by coiling with and without stent assistance: A review of 235 cases. Neurosurg 2012; 71: 785–794. [DOI] [PubMed] [Google Scholar]
- 20.Ko JK, Han IH, Cho WH, et al. Crossing Y-stent technique with dual open-cell stents for coiling of wide-necked bifurcation aneurysms. Clin Neurol Neurosurg 2015; 132: 54–60. [DOI] [PubMed] [Google Scholar]
- 21.Bechan RS, Sprengers ME, Majoie CB, et al. Stent-assisted coil embolization of intracranial aneurysms: Complications in acutely ruptured versus unruptured aneurysms. Am J Neuroradiol 2016; 37: 502–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cho YD, Sohn CH, Kang HS, et al. Coil embolization of intracranial saccular aneurysms using the Low-profile Visualized Intraluminal Support (LVIS™) device. Neuroradiol 2014; 56: 543–551. [DOI] [PubMed] [Google Scholar]
- 23.Ries T, Buhk J-H, Kucinski T, et al. Intravenous administration of acetylsalicylic acid during endovascular treatment of cerebral aneurysms reduces the rate of thromboembolic events. Stroke 2006; 37: 1816–1821. [DOI] [PubMed] [Google Scholar]
- 24.Valente I, Limbucci N, Nappini S, et al. Enterprise deployment through Pulserider to treat anterior communicating artery aneurysm recurrence. World Neurosurg Epub ahead of print 2018. DOI: 10.1016/j.wneu.2017.11.024. [DOI] [PubMed]