Abstract
Introduction
Multiple ways to access the dural carotid cavernous fistula have been described. The aim of the present study was to assess the results of embolization of a dural carotid cavernous fistula via different routes using endovascular accesses as a first-line strategy.
Methods
A retrospective data analysis of a consecutive series of 63 patients presenting with dural carotid cavernous fistula was performed.
Results
The dural carotid cavernous fistula was accessed by an endovascular approach in 58 patients (92.1%) and by direct puncture in five patients (7.9%). The inferior petrosal sinus was the main route accessed (65%). A recanalization of an occluded inferior petrosal sinus was obtained in 20.6% of cases. The access via either facial ophthalmic veins or the superior petrosal sinus was obtained in 20.6% and 3.1% of cases, respectively. Complete angiographic occlusion of a dural carotid cavernous fistula immediately after treatment was achieved in 53 patients (84.1%), whereas 10 patients (15.9%) displayed a partial occlusion. Treatment-related complications were observed in two patients (3.2%).
Conclusions
In this study, the endovascular approach allowed dural carotid cavernous fistula embolization in most patients. The inferior petrosal sinus, even when thrombosed, was the main route used to access the dural carotid cavernous fistula, followed by the facial vein, direct cavernous sinus puncture, and the superior petrosal sinus.
Keywords: Dural carotid cavernous fistula; embolization; transvenous approach; direct puncture of cavernous sinus
Introduction
Endovascular embolization has become the standard treatment for dural carotid cavernous fistula (DCCF).1–3 Despite improvements in endovascular devices and embolic materials, transvenous embolization remains the most commonly indicated strategy for treating DCCF. To allow transvenous embolization of a DCCF, a microcatheter must be positioned inside the cavernous sinus. Multiple endovascular routes to the cavernous sinus have been described, including via the inferior petrosal sinus, superior petrosal sinus, facial and ophthalmic veins, pterigoid plexus, and the vein of Labbé.1–11 In addition to endovascular routes, a direct puncture of other accesses to the cavernous sinus have also been described, such as a puncture of ophthalmic veins, the foramen ovale, and the superficial middle cerebral vein, in addition to a transorbital puncture of the cavernous sinus.12–16 Although a cure for DCCF can be achieved with an occlusion of the fistula compartment using coils and/or liquids, reaching the DCCF compartment is one of the most technically challenging steps in DCCF treatment. As previous studies reported, multiple accesses to the cavernous sinus have been described, showing how complex the treatment of DCCF can be.
The aim of the present study was to assess the results of transvenous embolization of DCCF via different routes to the cavernous sinus.
Methods
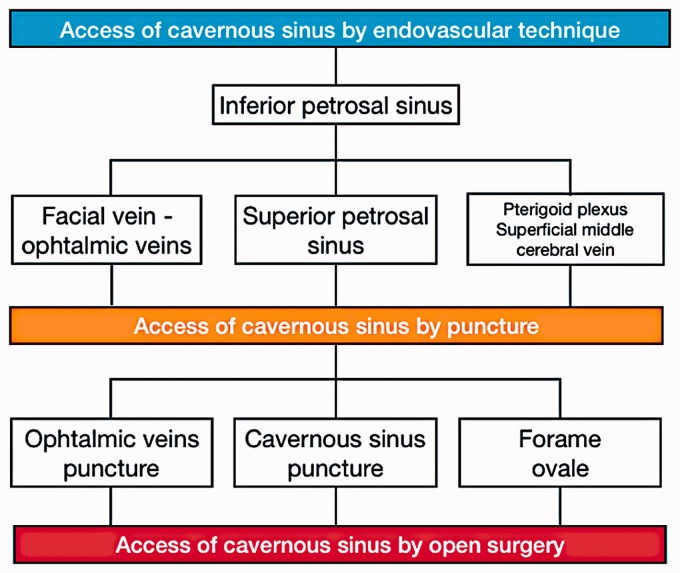
This is a retrospective study of a consecutive series of patients presenting with DCCF, all of whom were managed in two interventional neuroradiology centers. The data extraction and manuscript preparation were in accordance with recommendations from the Strengthening the Reporting of Observational Studies in Epidemiology guidelines. The study protocol was approved by the institutional review boards, which waived the need for written informed consent from the participants. We assessed clinical, radiological, and procedural data for all patients presenting with DCCF who were admitted to our institution between January 2006 and October 2017. Methods for data extraction and analysis were previously published.17 Compared to our previous publication, we included two additional patients in the series, and one patient that presented a spontaneous occlusion of the DCCF was excluded from this study. As previously reported, all procedures were performed under general anesthesia, and continuous anti-coagulation was maintained with non-fractioned heparin. Among the three endovascular embolization strategies (venous, arterial, or combined embolization), venous embolization was usually the first choice for treatment, whereas arterial or combined approaches were indicated if venous embolization could not be achieved. If endovascular access to the DCCF could not be obtained via the ipsilateral side, contra-lateral catheterization was attempted before resorting to the direct puncture of the cavernous sinus (CS). The direct puncture of the CS was indicated when access to the DCCF could not be achieved by the endovascular approach. If all strategies failed, open surgery was indicated. Figure 1 describes our DCCF treatment flowchart.
Figure 1.
Dural carotid cavernous fistula treatment flowchart.
A 5-F diagnostic catheter with continuous saline perfusion was positioned in the cervical carotid artery near the DCCF. A 6-F guiding catheter (Guider Softip, Boston Scientific, Natick, MA, USA) or a 5-F diagnostic catheter with continuous saline perfusion was positioned in the internal jugular vein or in the inferior petrous sinus. Through the guiding catheter, a DMSO-compatible microcatheter (Echelon; Medtronic, Irvine, CA, USA) was advanced using a 0.014-inch guidewire (Silverspeed – Medtronic or Transend – Stryker). The coils used were GDC, Target (Stryker), or Axium (Medtronic). Liquids perfused included Onyx 18 (Medtronic) or a solution of the acrylic glue N-butyl cyanoacrylate (Hystoacryl (B. Braun Melsungen AG, Melsungen, Germany) or Glubran 2 (GEM, Viareggio, Italy)) and lipiodol. Corticosteroids were administered for 5 days after the procedure. In the absence of complications, patients were extubated in the operating room and discharged 24 or 48 hours after the treatment.
Continuous variables were presented as means (range ± SD), and categorical variables were presented as numbers and percentages. One independent blinded statistician received all data collected for statistical analysis. IBM SPSS Statistics software version 20.0 (Chicago, IL, USA) was used for the statistical analysis. We considered p values < 0.05 significant.
Results
Among the 63 patients studied, venous embolization was performed in 60 (95.2%), venous and arterial embolization was performed in one (1.5%), and arterial embolization was performed in two patients (3.1%). For most of the cases the endovascular approach was performed (92%). Meanwhile, for a minority (8%) of cases, a direct puncture of the cavernous sinus was necessary to allow embolization of the DCCF. Among patients treated by the endovascular approach, the inferior petrosal sinus was the main route accessed (65% of cases), and inferior petrosal sinus recanalization was obtained in 20.6% of cases.
One patient had a recurrence of symptoms 2 weeks after a partial venous embolization of the DCCF using coils, and retreatment was performed using coils and Onyx. Complete angiographic occlusion of DCCF immediately after treatment was achieved in 53 patients (84.1%), while 10 patients (15.9%) displayed a partial occlusion. All patients who had complete immediate occlusion of the DCCF after treatment showed DCCF occlusion after 6 months. Treatment-related complications were observed in two patients (3.2%). One patient experienced an asystole for 5 seconds caused by a trigeminal reflex during Onyx injection, and the other experienced a perforation of the inferior petrous sinus during catheterization, which was promptly managed by coiling. Among the 53 patients (84.1%) who underwent digital subtracted angiography at 6 months, all (100%) had complete angiographic occlusion of the DCCF. The baseline data and results are summarized in Table 1. Figure 2 shows the three most frequent examples of DCCF access performed in this study. The results are shown in the table.
Table 1.
NBCA.
| Characteristics and results | Patients (n=63) |
|---|---|
| Age (mean, range, SD) | 62.7 (21-82, 12) |
| Barrow classification (n, %) | |
| B | 14 (22.2) |
| C | 6 (9.5) |
| D | 43 (68.2) |
| Venous cortical reflux (n, %) | 18 (28.5) |
| Side of the fistula (n, %) | |
| Right | 28 (44.4) |
| Left | 28 (44.4) |
| Bilateral | 7 (11.1) |
| Transvenous embolization (n, %) | 60 (95.2) |
| Arterial embolization (n, %) | 2 (3.1) |
| Combined arterial + venous embolization (n, %) | 1 (1.5) |
| Ipsilateral access | 52 (82.5) |
| Contralateral access | 5 (7.9) |
| Bilateral access | 4 (6.3) |
| Transvenous routes to the fistula (n, %) | 61 (96.8) |
| Inferior petrosal sinus | 41 (65) |
| Recanalization of occluded inferior petrosal sinus (n, %) | 13 (20.6) |
| Facial vein | 13 (20.6) |
| Superior petrosal sinus | 2 (3.1) |
| Direct puncture of cavernous sinus | 5 (7.9) |
| Embolic materials (n, %) | |
| Coils | 33 (52.3) |
| NBCA | 3 (4.7) |
| Onyx | 5 (7.9) |
| Coils + NBCA | 6 (9.5) |
| Coils + Onyx | 16 (25.4) |
| Treatment related complications (n, %) | 2 (3.1) |
| Complete immediate angiographic occlusion (n, %) | 53 (84.1) |
| Complete angiographic occlusion at the 6-month follow-up (n, %) | 53/53 (100) |
| Recurrence during 6-month follow-up (n, %) | 1 (1.5) |
NCBA: N-butyl cyanoacrylate.
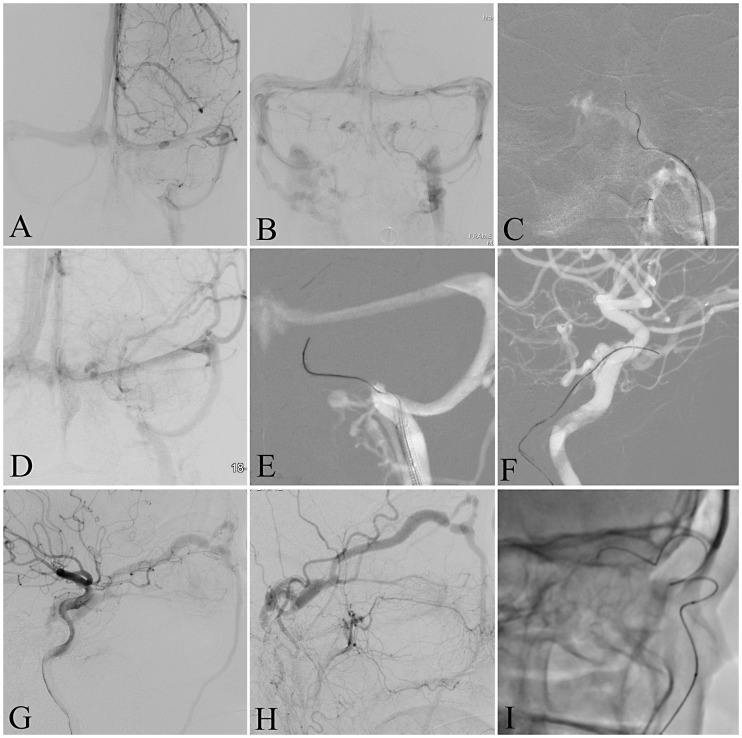
Figure 2.
(Case 1: A, B, C) (A) Digital subtracted angiography (DSA), frontal view, venous phase of left internal carotid injection showing bilateral facial veins but no visualization of cavernous sinus; (B) DSA, frontal view, venous phase, after a left vertebral artery injection showing both cavernous and inferior petrosal sinus; (C) road-map, frontal view, showing catheterization of left cavernous sinus through an opened inferior petrosal sinus. (Case 2: D, E, F) (D) DSA frontal view, venous phase of left internal carotid injection showing occlusion of inferior petrosal sinus; (E, F) road-map, frontal view (E), and lateral view (F), showing recanalization of left cavernous sinus through an occluded inferior petrosal sinus. (Case 3: G, H, I) DSA, lateral views, after right carotid artery injection initial (G), and late (H) phases, showing a dural carotid cavernous fistula (DCCF) draining through superior ophthalmic vein to facial vein and occlusion of inferior petrosal sinus; (I) X-ray lateral view showing catheterization of DCCF through the facial vein and superior ophthalmic vein.
Discussion
This study reports the results of a large consecutive series of patients presenting with DCCF, who were treated at two centers based on the same treatment rationale (Figure 1). The treatment algorithm used in this study derived from one of the main principles of neuro-endovascular procedures: to be as minimally invasive as possible. Therefore, we often attempted to access the DCCF via the endovascular approach even if it was isolated or all venous routes to it were occluded. In general, the DCCF was accessed through an endovascular route in 92% of cases, while a direct cavernous sinus puncture was necessary in 8% of cases. The endovascular treatment strategy may be challenging for some DCCF cases in which endovascular catheterization may be difficult, time consuming, and at risk of vessel perforations during catheterization. However, in this study, a high rate (92%) of DCCF catheterizations were successful using the endovascular technique. Only one patient (1.5%) experienced a complication related to an occluded inferior petrosal sinus (IPS) perforation. When the endovascular access of the CS is difficult, some techniques can be used before indicating a direct puncture of the CS. Firstly, the catheter must have a good stability that can be obtained by an internal jugular vein puncture and/or using a coaxial guiding catheter system with a distal access catheter. These strategies improve catheterization of the CS using microcatheters. Second, in cases of difficult catheterization of occluded IPS, use of extra-stiff wires facilitate catheterization of the CS when the regular micro-guidewires cannot penetrate the IPS. Third, if an ipsilateral IPS cannot be crossed by a microcatheter, an approach via inter-cavernous sinus from the contralateral side can be used.
As in the present study, two other large studies indicated that the endovascular approach could serve as an effective first-line treatment strategy for DCCF, while ophthalmic or CS sinus punctures only occurred in cases of endovascular technique failure.2,4 In a study of 161 patients presenting with DCCF, Kirsh et al. reported 159 embolization procedures performed by endovascular access, whereas only two procedures (1.2%) were performed by ophthalmic vein exposure. Out of the 159 endovascular procedures, the authors positioned a guide catheter in the jugular bulb for 155 treatments and only four were positioned in the facial vein.2 In another large DCCF series, Jung et al. reported the results of 76 DCCF, for which 36.8% underwent transarterial embolization, 10% underwent arterial and transvenous embolization, and 52.6% underwent transvenous embolization. The transvenous accesses to the CS were performed in 48 patients (63.1%), the ipsilateral IPS was performed in 32 patients (66.7%), the contralateral IPS was performed in six patients (12.5%), the facial vein was performed in seven patients (14.5%), and direct surgical superior ophthalmic vein puncture was performed in three patients (6.2%).
In contrast to the present study, Wenderoth reported a series of 32 DCCF in which a direct puncture of the CS was performed in 21 patients (65.6%), 19 patients (59.3%) were treated only by direct puncture of the CS, eight patients (25%) were treated by transvenous access, three patients (9.3%) were treated by transarterial embolization, and two patients (6.2%) were treated by combined CS puncture and transarterial embolization. The author indicated that catheterization was used only through visible or open IPS, and a transorbital CS puncture was reserved for cases of occluded IPS.12
A direct puncture of the confluence of the ophthalmic veins or the cavernous sinus itself has been considered effective and safe as a result of a reduction in the procedure time.12,18–20 However, potential complications of direct puncture include eyeball perforation, orbital cellulitis, optic nerve damage, injury to the cranial nerves, intra-orbital hematoma requiring an emergent decompressive surgery, carotid lesions, or even subarachnoid haemorrhage.18–20 Despite the results for the direct puncture and the fact that endovascular embolization seems to be relatively similar, safe, and effective by observational case series, no prospective study comparing endovascular versus direct puncture for treatment of DCCF has been performed.
This study has limitations because it involved a single arm with no comparative control group. Despite the consecutive and prospective registry of cases, all data analysis in this study was retrospective, and some data for each case were missing, such as the procedure times, the exact sequences and time spent on catheterization attempts for each case, and cases in which contra-lateral catheterization attempts were performed and failed. Large prospective studies could clarify the results with regard to treatment strategies for DCCF.
Conclusion
In this study, the endovascular approach allowed DCCF embolization in most patients. The inferior petrosal sinus, even when thrombosed, was the main route used to access the DCCF, followed by the facial vein, direct cavernous sinus puncture, and the superior petrosal sinus.
Acknowledgments
None.
Contributorship statement
Luís H de Castro-Afonso participated in the concept of the study, drafted and approved the manuscript; Felipe P Trivelato participated in the study concept and design, data analysis, revision, and final approval of the manuscript; Marco T Rezende, Alexandre Ulhôa, Guilherme S Nakiri, and Lucas M Monsignore participated in data acquisition, figure and table editing, revision, and final approval of the manuscript; Daniel G Abud conceived the study, acquired data, critically revised the manuscript, and approved the final work.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Luo CB, Chang FC, Teng MM, Lin CJ, Wang AG, Ting TW. Aggressive cavernous sinus dural arteriovenous fistula: Angioarchitecture analysis and embolization by various approaches. J Chin Med Assoc. 2016; 79: 152–8. [DOI] [PubMed] [Google Scholar]
- 2.Kirsch M, Henkes H, Liebig T, Weber W, Esser J, Golik S, Kühne D. Endovascular management of dural carotid-cavernous sinus fistulas in 141 patients. Neuroradiology. 2006; 48: 486–90. [DOI] [PubMed] [Google Scholar]
- 3.Klisch J, Huppertz HJ, Spetzger U, Hetzel A, Seeger W, Schumacher M. Transvenous treatment of carotid cavernous and dural arteriovenous fistulae: Results for 31 patients and review of the literature. Neurosurgery. 2003; 53: 836–56. [DOI] [PubMed] [Google Scholar]
- 4.Jung KH, Kwon BJ, Chu K, Noh Y, Lee ST, Cho YD, Han MH, Roh JK. Clinical and angiographic factors related to the prognosis of cavernous sinus dural arteriovenous fistula. Neuroradiology. 2011; 53: 983–92. [DOI] [PubMed] [Google Scholar]
- 5.Satow T, Murao K, Matsushige T, Fukuda K, Miyamoto S, Iihara K. Super selective shunt occlusion for the treatment of cavernous sinus dural arteriovenous fistulae. Neurosurgery. 2013; 73(1 Suppl Operative): ons100–5. [DOI] [PubMed] [Google Scholar]
- 6.Lekkhong E, Pongpech S, Ter Brugge K, Jiarakongmun P, Willinsky R, Geibprasert S, Krings T. Transvenous embolizations of intracranial dural arteriovenous shunts through occluded venous segments: Experience in 51 patients. AJNR Am J Neuroradiol. 2011; 32: 1738–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chalouhi N, Dumont AS, Tjoumakaris S, Gonzalez LF, Bilyk JR, Randazzo C, Hasan D, Dalyai RT, Rosenwasser R, Jabbour P. The superior ophthalmic vein approach for the treatment of carotid-cavernous fistulas: A novel technique using Onyx. Neurosurg Focus. 2012; 32: E13. [DOI] [PubMed] [Google Scholar]
- 8.Jiang C, Lv X, Li Y, Wu Z, Shi J. Surgical access on the superior ophthalmic vein to the cavernous sinus dural fistula for embolization. J Neurointerv Surg. 2013; 5: e13. [DOI] [PubMed] [Google Scholar]
- 9.Briganti F, Caranci F, Leone G, Napoli M, Cicala D, Briganti G, Tranfa F, Bonavolontà G. Endovascular occlusion of dural cavernous fistulas through a superior ophthalmic vein approach. Neuroradiol J. 2013; 26: 565–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kurata A, Suzuki S, Iwamoto K, Nakahara K, Inukai M, Niki J, Satou K, Yamada M, Fujii K, Kan S, Katsuta T. A new transvenous approach to the carotid-cavernous sinus via the inferior petro-occipital vein. J Neurosurg. 2012; 116: 581–7. [DOI] [PubMed] [Google Scholar]
- 11.Konstas AA, Song A, Song J, Thanos A and Ross IB. Embolization of a cavernos carotid fistula through the vein of Labbé: a new alternativa tranvenous access route. J Neurointerv Surg. 2018 Apr 7 doi: 10.1136/neurintsurg-2017-013229.rep. [Epub ahead of print]. [DOI] [PubMed]
- 12.Wenderoth J. Novel approaches to access and treatment of cavernous sinus dural arteriovenous fistula (CS-DAVF): Case series and review of the literature. J Neurointerv Surg. 2017; 9: 290–296. [DOI] [PubMed] [Google Scholar]
- 13.Elhammady MS, Peterson EC, Aziz-Sultan MA. Onyx embolization of a carotid cavernous fistula via direct transorbital puncture. J Neurosurg. 2011; 114: 129–32. [DOI] [PubMed] [Google Scholar]
- 14.Ong CK, Wang LL, Parkinson RJ, Wenderoth JD. Onyx embolisation of cavernous sinus dural arteriovenous fistula via direct percutaneous transorbital puncture. J Med Imaging Radiat Oncol. 2009; 53: 291–5. [DOI] [PubMed] [Google Scholar]
- 15.Liu A, Liu J, Qian Z, Peng T, Li Y, Yang J, Wu Z, Jiang C. Onyx embolization of cavernous sinus dural arteriovenous fistulas via direct transorbital puncture under the guidance of three-dimensional reconstructed skull image (reports of six cases). Acta Neurochir (Wien). 2014; 156: 897–900. [DOI] [PubMed] [Google Scholar]
- 16.Chaudhary N, Lownie SP, Bussière M, Pelz DM and Nicolle D. Transcortical venous approach for direct embolization of a cavernous sinus dural arteriovenous fistula: Technical case report. Neurosurgery. 2012 Jun;70(2 Suppl Operative):343–8. [DOI] [PubMed]
- 17.de Castro-Afonso LH, Trivelato FP, Rezende MT, Ulhôa AC, Nakiri GS, Monsignore LM, Colli BO, Velasco-E-Cruz AA, Abud DG. Transvenous embolization of dural carotid cavernous fistulas: the role of liquid embolic agents in association with coils on patient outcomes. J Neurointerv Surg. 2018; 10: 461–462. [DOI] [PubMed] [Google Scholar]
- 18.Gil A, Ibor LL, Flores GL, Cuellar H, Murais E, Boto GR. Treatment of a carotid cavernous fistula via direct transovale sinus puncture. J Neurosurg. 2013; 119: 247–51. [DOI] [PubMed] [Google Scholar]
- 19.Dashti SR, Fiorella D, Spetzler RF, Albuquerque FC, McDougall CG. Transorbital endovascular embolization of dural carotid cavernous fistula: Access to cavernous sinus through direct puncture: Case examples and technical report. Neurosurgery. 2011; 68(1 Suppl Operative): 75–83. discussion 83. [DOI] [PubMed] [Google Scholar]
- 20.Puffer RC, Lanzino G and Cloft HJ. Using Xperguide planning software to safely guide catheter access to the cavernous sinus via transorbital puncture: A case report. Neurosurgery. 2014 Jun;10 Suppl 2:E370–3; discussion E373. [DOI] [PubMed]