Abstract
Background:
Degenerative medial meniscal tears and subsequent partial meniscal resection compromise meniscal function and lead to an overload of the medial compartment. In addition, lower limb alignment plays a key role in load distribution between the medial and lateral knee compartments, and varus alignment is a potential risk factor for medial osteoarthritis.
Purpose/Hypothesis:
The purpose of this biomechanical study was to investigate the effect of valgus and varus alignment on peak pressure and contact area in knees with concomitant horizontal medial meniscal tears and subsequent leaflet resection. It was hypothesized that varus alignment in combination with meniscal loss leads to the highest peak pressure within the medial compartment.
Study Design:
Controlled laboratory study.
Methods:
Six fresh-frozen human cadaveric knees were axially loaded using a 1000-N compressive load in full extension with the mechanical axis rotated to intersect the tibial plateau at 40%, 45%, 50%, 55%, and 60% of its width (TPW) to simulate varus and valgus alignment. Tibiofemoral peak contact pressure and contact area of the medial and lateral compartments were determined using pressure-sensitive foils in each of 4 different meniscal conditions: intact, 15-mm horizontal tear of the posterior horn, inferior leaflet resection, and resection of both leaflets.
Results:
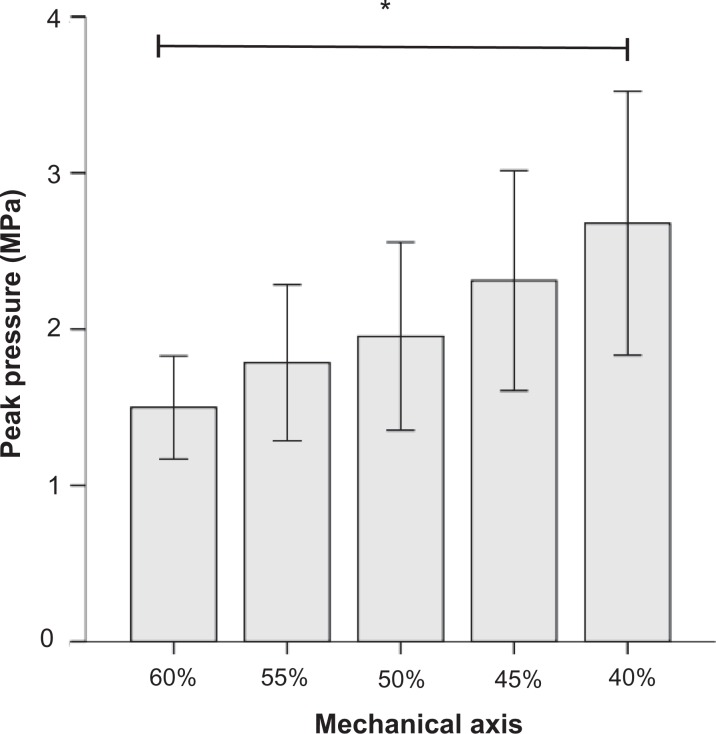
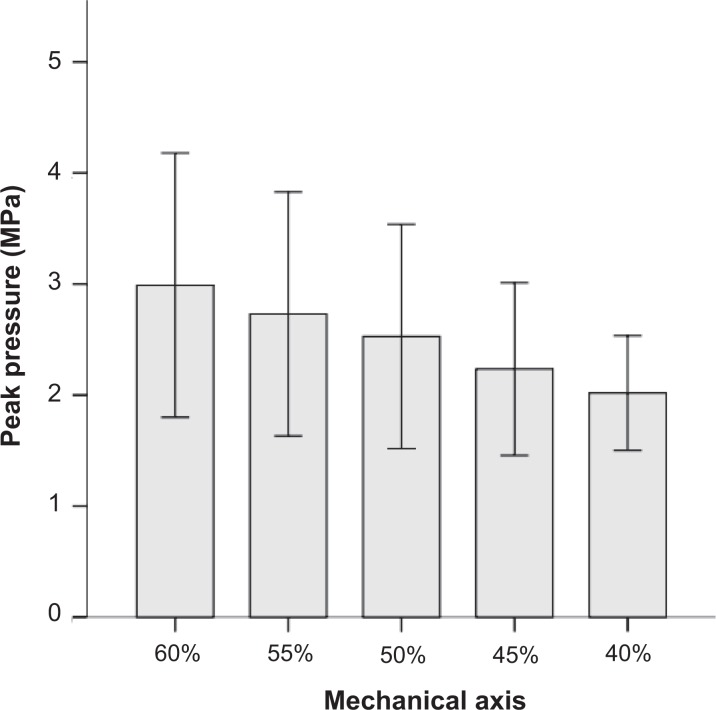
The effect of alignment on peak pressure (normalized to the neutral axis) within the medial compartment in cases of an intact meniscus was measured as follows: varus shift resulted in a mean increase in peak pressure of 18.5% at 45% of the TPW and 37.4% at 40% of the TPW, whereas valgus shift led to a mean decrease in peak pressure of 8.7% at 55% of the TPW and 23.1% at 60% of the TPW. Peak pressure changes between the intact meniscus and resection within the medial compartment was less in valgus-aligned knees (0.21 MPa at 60% TPW, 0.59 MPa at 50% TPW, and 0.76 MPa at 40% TPW). Contact area was significantly reduced after partial meniscal resection in the neutral axis (intact, 553.5 ± 87.6 mm2; resection of both leaflets, 323.3 ± 84.2 mm2; P < .001). This finding was consistent in any alignment.
Conclusion:
Both partial medial meniscal resection and varus alignment led to an increase in medial compartment peak pressure. Valgus alignment prevented medial overloading by decreasing contact pressure even after partial meniscal resection. A horizontal meniscal tear did not influence peak pressure and contact area even in varus alignment.
Clinical Relevance:
As a clinical consequence, partial meniscal resection should be avoided to maintain the original biomechanical behavior, and the mechanical axis should be taken into account if partial meniscectomy is necessary.
Keywords: tibiofemoral joint, peak pressure, contact area, varus, valgus, horizontal medial meniscal tear, biomechanical study
A meniscal tear is the most common knee injury, and its incidence increases up to 50% with age.11,12 In the elderly, degenerative changes in the meniscal matrix lead to mostly horizontal cleavage tears of the posterior horn of the medial meniscus.11 It is believed that these degenerative tears of the meniscus might be the first sign of osteoarthritis within the joint.14 Even though conservative treatment shows good clinical outcomes, partial meniscectomy is necessary for over 30% of these patients because of persistent pain and locking.19,21,30 As a consequence, it is evident that meniscal loss is associated with the development and rapid progression of osteoarthritis.13,14,27 Postoperative femoral osteonecrosis has also been described after meniscectomy.10,26,29
The joint deterioration process could be explained by significant biomechanical changes in the meniscus-deficient compartment and has been attributed to the adverse biomechanical consequence of partial meniscectomy.2–5,8,17,22,25 After partial meniscectomy, contact pressure increases, whereas contact area is reduced.2,5,8,17,25 On the other hand, it has been shown that lower limb alignment significantly influences knee contact pressure in case of cartilage defects.1,24 The mechanical axis plays a key role in load distribution between the medial and lateral knee compartments, and varus alignment is a potential risk factor for medial overloading.14,24 In these patients, high tibial osteotomy is an option to change load distribution within the joint and prevent the necessity of early arthroplasty.7,9,16,28 The surgical indication for valgus osteotomy in case of severe malalignment is well described, whereas the benefit in only mild varus remains uncertain.
The purpose of this biomechanical study was to investigate the effect of small changes in valgus and varus alignment on peak pressure and contact area in knees with concomitant horizontal medial meniscal tears and subsequent leaflet resection. It was hypothesized that varus alignment in combination with meniscal loss would lead to the highest peak pressure within the medial compartment.
Methods
Six unpaired fresh-frozen human cadaveric knees (4 male, 2 female) (MedCure) with a mean age of 68.0 ± 9.4 years were used for biomechanical testing. The knees were free of osteoarthritis, and ligaments and menisci were intact. This was ensured by a radiological examination before testing and a gross inspection during the dissection process. Before delivery, all specimens had been transected 20 cm proximal and distal to the joint line of the knee. Before dissection and testing, all specimens were thawed for 24 hours at room temperature.
Skin, muscles, tendons, and patellae were dissected, leaving the cruciate and collateral ligaments and the remaining capsule intact. Knees were kept moist with NaCl (0.9% solution) during the entire test.
The specimens were embedded in custom-made 3-dimensionally printed prismatic casts (polyethylene, 70 × 90 mm2, 90 mm in height) by using quick hardening polyurethane resin (RenCast FC 52/53 Isocyanate/FC 52 Polyol; Huntsman). The embedding casts were aligned by a standardized protocol in full extension matching the center of the tibial plateau in the frontal and sagittal planes as well as the joint line using a laser line with 2 perpendicular projection lines. First, the tibial plateau width (TPW) was determined by using a sliding caliper, and the center of the tibial plateau was marked. Based on anatomic studies, the center of the virtual femoral head was defined as a point 50 cm proximal and directly above the center of the tibial plateau.15,20 The femoral pot was parallel and centrally oriented in relation to the tibial plateau, thereby adapting the femoral anatomic axis with a lateral offset of approximately 6° (Figure 1). The tibial pot was aligned alike in reference to the determined center of the tibial plateau, resulting in an approximate 3° tibial offset.
Figure 1.
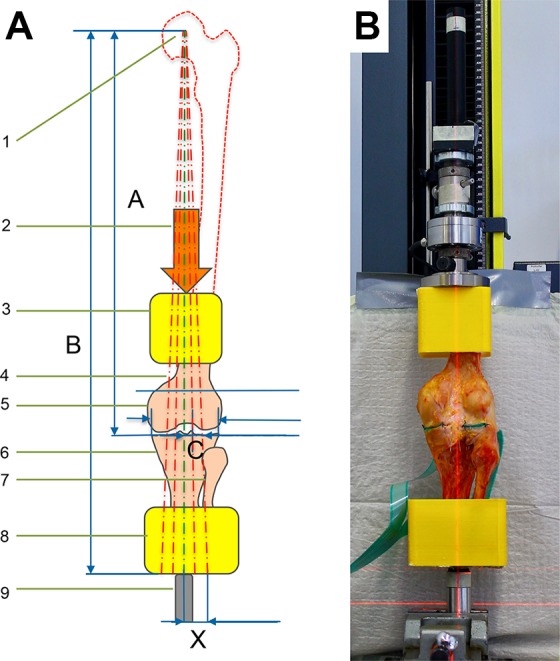
(A) Overview of the biomechanical alignment and compression setup (not to scale), consisting of (1) the center point of the femoral head, (2) the direction of the applied force, (3, 8) specimen potting, (4) laser projections for varus/neutral/valgus, (5) the distal femur, (6, 7) the proximal tibia and fibula, and (9) the ball bearing that can be shifted to meet the corresponding laser line. The amount of medial and lateral translation of the tibial fixation cap was calculated as: X = (B/A) × C. (B) Photograph depicting the virtual femoral head 50 cm above the joint line and the approximate 6° offset of the femoral anatomic axis to the potting casts. The neutral mechanical axis was defined as a strictly vertical connection between the center of the femoral head, the center of the tibial plateau, and the tibial ball bearing. Perpendicular laser lines imitating the Mikulicz line and the joint line monitored the medial and lateral shifts of the tibial fixation cap.
The potted specimens were rigidly attached to a universal testing device (zwickiLine Z2.5; Zwick/Roell), equipped with a load cell rated up to 2.5 kN (KAF-Z2.5, Class 0.05%; A.S.T.) and keeping the neutral mechanical axis collinear to the load application. The neutral mechanical axis was defined as a strictly vertical connection between the center of the femoral head, the center of the tibial plateau, and the center of the tibial ball bearing (Figure 1). Exact potting allowed central fixation of the femoral cast to the load cell of the testing device and further ensured 2 keys of the setup: (1) the joint line was perpendicular to the compression axis, and (2) the neutral mechanical axis was concordant with the loading axis.
For mechanical bearing of the potted tibia, an anatomic alignment method was developed to mechanically simulate the valgus and varus conditions without the need for tibial osteotomy. A spherical cap was used and shifted out of the neutral axis to create lateral and medial off-center loading cases. The amount of medial and lateral translation of the tibial fixation cap was calculated by the use of the following intercept theorem: X = (B/A) × C (Figure 1A). The Mikulicz line was rotated around the reconstructed center of the femoral head to intersect the joint line at its target of 40%, 45%, 50%, 55%, and 60% of the coronal TPW, and a laser line was used to monitor the individual lateral shift of the tibial bearing. Finally, all compression tests were performed in full extension with a preload of 10 N and a compression ramp of 10 mm/min until a load of 1000 N was reached.
A K-Scan 4000 knee sensor foil (Tekscan) was used for testing. The sensor elements were protected on both sides by a thin film of self-adhesive tape. Calibration and equilibration were performed according to the manufacturer’s guidelines before insertion with a flat-ended cylindrical calibration body of a known diameter and mass. The sensor was placed between the menisci and the tibial plateau, followed by suturing the nonsensitive boundary area of the foil to the anterior and posterior capsules to avoid displacement shifts during testing. The meniscotibial ligaments were anteriorly and posteriorly incised (20 mm) to allow sensor foil insertion, while the medial and lateral coronary ligaments and the meniscus roots were carefully preserved. The 2 separate sensors measured the femorotibial contact pressure and contact area of the medial and lateral compartments, respectively.
For each specimen, 4 different meniscal conditions were consecutively tested: (1) intact, (2) a standardized 15-mm horizontal tear of the posterior horn, (3) inferior leaflet resection, and (4) resection of both leaflets. The horizontal tear was created according to previous reports using a scalpel blade between 2 inserted needles from posterior to anterior and directed inferior to the central edge.8,18 The leaflets were successively resected in the same manner through the posterior approach with a remaining 3-mm meniscal rim (Figure 2). As the maximum load of 1000 N was reached, the pressure distribution was recorded via the inserted sensor foil and evaluated by the included software tool, provided by the manufacturer.
Figure 2.
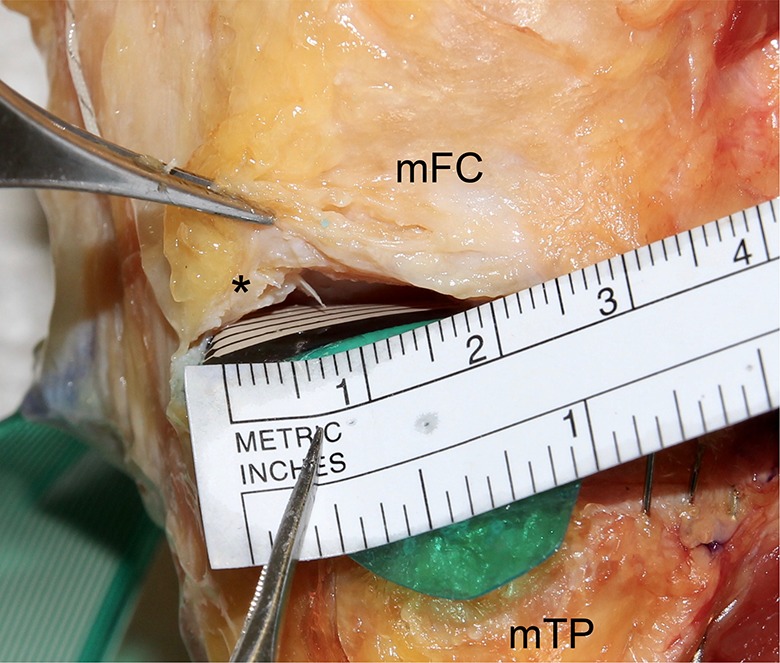
A 15-mm horizontal meniscus tear was created and subsequently stepwise resected through a small posterior approach. A 3-mm rim remained to maintain the peripheral meniscal rim (*). mFC, medial femoral condyle; mTP, medial tibial plateau.
Statistical Analysis
Data were analyzed using SPSS statistics software version 23.0 (IBM). The statistical analysis was based on 2-factor analysis of variance with repeated measures. The dependent variables (peak pressure and contact area) were compared across the independent variable meniscal condition and limb alignment in the lateral and medial compartments. Statistical significance was set at P < .05. Based on previous results and assuming a P value of .05, a preliminary sample size calculation resulted in a number of 6 specimens to detect a change in peak pressure in the medial compartment between the intact and resection states of 30% with a standard deviation of 15% and a statistical power of 80%.8,22
Results
The effect of alignment on peak pressure compared with the neutral mechanical axis within the medial compartment resulted in mean increase of 18.5% at 45% of the TPW and 37.4% at 40% of the TPW (varus offset), whereas 55% of the TPW and 60% of the TPW (valgus offset) resulted in a mean decrease in peak pressure of 8.7% and 23.1%, respectively (P < .05) (Figure 3). The presence of a horizontal meniscal tear did not significantly affect peak pressure in any alignment.
Figure 3.
Small changes in the mechanical axis (rotated to intersect the joint line at different percentages of the tibial plateau width) showed a significant change in peak pressure within the medial compartment (*P < .05).
The impact of the resection of both meniscus leaflets compared with the intact state was higher in varus-aligned knees. The increase in peak pressure with respect to the mechanical axis was measured as follows: 0.21 MPa at 60% of the TPW, 0.32 MPa at 55% of the TPW, 0.59 MPa at 50% of the TPW, 0.87 MPa at 45% of the TPW, and 0.76 MPa at 40% of the TPW. These findings corresponded to an alignment-dependent increment of peak pressure between the intact meniscus and double-leaflet resection of 14% at 60% of the TPW, 18% at 55% of the TPW, 30% in the neutral axis, 38% at 45% of the TPW, and 27% at 40% of the TPW (Figure 4A). Results are displayed in detail in Table 1, Figure 4A, and Figure 5.
Figure 4.
Summary of (A) peak pressure and (B) contact area as functions of the meniscal state and limb alignment in the medial compartment. (A) Peak pressure was significantly different between 40% of the tibial plateau width (TPW) and 60% of the TPW in the designated meniscal conditions (*P < .05). (B) Contact area was significantly reduced after single- and double-leaflet resection from the intact meniscus (*) and from the tear state (°) (P < .05).
TABLE 1.
Peak Pressure in the Medial Compartment According to Lower Limb Alignment and the Meniscal Statea
| Intersection Point of the Mechanical Axis Along the Coronal Tibial Plateau Width | Meniscal State | |||
|---|---|---|---|---|
| Intact | Horizontal Tear | Single-Leaflet Resection | Double-Leaflet Resection | |
| 60% (valgus) | 1.50 ± 0.31 (77%) | 1.43 ± 0.37 (73%) | 1.76 ± 0.37 (90%) | 1.71 ± 0.41 (88%) |
| 55% (valgus) | 1.78 ± 0.48 (91%) | 1.71 ± 0.56 (88%) | 2.18 ± 0.73 (112%) | 2.10 ± 0.76 (108%) |
| Neutral | 1.95 ± 0.57 (100%) | 2.00 ± 0.55 (103%) | 2.45 ± 0.87 (126%) | 2.54 ± 0.76 (130%) |
| 45% (varus) | 2.31 ± 0.67 (118%) | 2.40 ± 0.65 (123%) | 2.85 ± 1.15 (146%) | 3.18 ± 0.95 (163%) |
| 40% (varus) | 2.67 ± 0.80 (137%) | 2.68 ± 0.82 (137%) | 3.24 ± 1.24 (166%) | 3.43 ± 1.34 (176%) |
aData are shown as mean ± SD (in MPa). Percentages are related to peak pressure in the medial compartment in neutral alignment and the intact meniscus.
Figure 5.
Visual representation of the peak pressure changes in the medial compartment depending on lower limb alignment with the intact meniscus and the Mikulicz line intersecting the tibial plateau at (A) 60%, (B) 55%, (C) 50%, (D) 45%, and (E) 40% of its width. Illustration of peak pressure changes in the medial compartment in the neutral axis with (F) an intact meniscus, (G) a horizontal tear, (H) single-leaflet resection, and (I) double-leaflet resection.
Contact area was significantly reduced after double-leaflet resection compared with the intact and tear states (P < .05). These changes were found in all examined mechanical axes (Figure 4B). The mechanical axis did not influence contact area of the medial compartment. Regarding the lateral compartment, peak pressure showed a linear change when shifting the axis from varus to valgus alignment within a maximum displacement of ±10% of the Mikulicz line along the tibial plateau (R 2 = 0.99) (Figure 6).
Figure 6.
Changes in peak pressure within the lateral compartment for the intact meniscus. A continuous decrease can be assumed when shifting the mechanical axis toward varus alignment (nonsignificant).
Discussion
The most relevant finding of this study was that double-leaflet resection of a horizontal medial meniscal tear in combination with varus alignment showed the highest peak pressure within the medial compartment. Peak pressure increased after single- and double-leaflet resection but not in the case of a tear and was higher in varus-aligned knees than in valgus alignment. Peak pressure after double-leaflet resection in valgus (intersection at 60%) did not exceed the contact pressure in the neutral axis with an intact meniscus. Contact area decreased after single- and double-leaflet resection but not in the meniscal tear state in all tested alignments.
The fundamental role of the meniscus on knee load distribution and stability has been extensively described.12,23 The integrity of the circumferential collagen fibers is essential for load distribution and shock absorption through the conversion of an axial load to hoop stresses to preserve the joint from mechanical overloading. In the case of degenerative horizontal cleavage tears, the primary treatment aim is to preserve as much tissue as possible, even when meniscal repair is not possible.19,21 Single-leaflet resection is one option to maintain meniscus tissue and an overlying meniscal surface.
Tibiofemoral biomechanical changes in the medial compartment in case of horizontal cleavage tears have gained much scientific interest. Primarily, Haemer et al18 performed a biomechanical study using sheep knee cadaveric specimens and showed that single- and double-leaflet resection led to higher peak pressure and decreased contact area within the medial joint compartment. More recently, several authors have biomechanically evaluated the effect of horizontal tears and resection patterns in human cadaveric specimens.3,4,8,22 In those studies, the presence of a horizontal tear of the meniscus showed similar results when a static axial compression force was applied.4,8,22 In accordance with our findings, previous studies reported no increment in peak pressure as a result of a horizontal tear of the posterior meniscal horn.8,22 However, a more extended tear involving the whole meniscal rim appears to increase peak pressure within the medial compartment.4
Interestingly, biomechanical results after single-leaflet resection are controversial, and the benefit of single-leaflet resection is still unclear. Brown et al8 reported that a remaining single leaflet could maintain meniscal function and avoid significant changes in peak pressure in comparison with intact and tear conditions. In contrast, other authors have shown a significant increase in peak pressure after single-leaflet resection.4,18,22 Despite the controversial results regarding peak pressure, a substantial decrease in contact area in the medial compartment after single-leaflet resection was reported by those authors.4,18,22 On the other hand, these same authors agreed that the resection of both leaflets led to a significant increase in peak pressure and decrease in contact area.4,8,22 Koh et al22 reported an additional increase in contact pressure after the resection of both leaflets: up to 79% compared with the intact state. The results of the present setup support the findings that even single-leaflet resection remarkably influences contact pressure in the medial compartment. These results also reinforce the findings that even single-leaflet resection has a high effect on contact area, even though statistical significance has not been reached in all investigated alignments. This might be explained by the loss of meniscal height and the following decrement of joint congruency.
Furthermore, this study investigated the influence of the mechanical axis on peak pressure changes within the knee joint. Previous biomechanical studies have shown that valgus osteotomy to unload cartilage defects results in a decrease of peak pressure in the medial compartment. In accordance with our results, Mina et al24 reported a linear increase in medial contact pressure from 10° valgus to 8° varus alignment. Agneskirchner et al1 also showed a significantly higher peak pressure in varus-aligned knees compared with neutral alignment with intact menisci in the medial compartment. The results of the present study showed a linear increase in peak pressure from valgus to varus alignment in the case of an intact meniscus and could therefore support previous findings.1,24 The results also showed that the effect of partial meniscectomy on the peak pressure increase was higher in varus than valgus alignment. As a clinical consequence of our findings, surgeons have to consider the mechanical axis in patients with degenerative meniscal changes if partial meniscectomy is necessary. One viable option to unload the medial compartment might be valgus osteotomy to prevent the rapid progression of osteoarthritis and the need for arthroplasty.6,7,16,28 Nevertheless, the impact of osteotomy with possible detrimental effects has to be carefully considered in clinical decision making.
As with all controlled laboratory studies, this study includes some limitations. Results using cadaveric specimens for biomechanical testing may not be completely comparable with in vivo conditions. Limitations include testing only in restrained full extension and in a static loading ramp. This might underestimate the impact of horizontal meniscal tears when compared with dynamic testing and gait analysis, but it was necessary to reduce shear stresses on the pressure-sensitive foils.3,5 The resection of muscles, the anterior capsule (including the patella), and anterior and posterior coronary ligaments to insert the sensors might lead to an alteration in anatomic loading patterns and increased meniscal mobility. Leaflet resection was conducted via a mini-open posterior approach and not arthroscopically. The thickness and rigidity of the Tekscan sensor foil might have affected joint contact measurements. Sensors were sutured to the capsule but might have shifted during testing. Nevertheless, the created meniscal tear imitates a degenerative horizontal meniscal tear often seen in clinical practice. The methodology and loading were similar to well-established test protocols of previous studies.8,25 Furthermore, a validated method of varus and valgus alignment testing was described.
Conclusion
Varus alignment combined with partial resection of a horizontal medial meniscal tear led to an increase in medial compartment peak pressure and decrease in contact area compared with the intact meniscal condition. The effect of partial meniscal resection on peak pressure in the medial compartment was higher in varus than valgus alignment. Valgus alignment prevented medial overloading by decreasing medial compartment contact pressure even after partial meniscal resection. A present horizontal meniscal tear did not, by itself, influence peak pressure and contact area even in varus alignment within a stand configuration. As a clinical consequence, partial meniscal resection should be avoided to maintain biomechanical properties. If the patient suffers from ongoing pain and surgical treatment is necessary, lower limb alignment should be taken into account in clinical practice.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: The Technical University of Munich has received direct funding from the German Arthritis Foundation. This work was supported by the German Research Foundation and the Technical University of Munich within the framework of the Open Access Publishing Program. Funding had no influence on the study design, data collection, or interpretation of the results or the final article. A.B.I. is a consultant for medi GmbH & Co KG and Arthrosurface. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the Technical University of Munich.
References
- 1. Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23(8):852–861. [DOI] [PubMed] [Google Scholar]
- 2. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–1931. [DOI] [PubMed] [Google Scholar]
- 3. Arno S, Bell CP, Uquillas C, Borukhov I, Walker PS. Tibiofemoral contact mechanics following a horizontal cleavage lesion in the posterior horn of the medial meniscus. J Orthop Res. 2015;33(4):584–590. [DOI] [PubMed] [Google Scholar]
- 4. Beamer BS, Walley KC, Okajima S, et al. Changes in contact area in meniscus horizontal cleavage tears subjected to repair and resection. Arthroscopy. 2017;33(3):617–624. [DOI] [PubMed] [Google Scholar]
- 5. Bedi A, Kelly NH, Baad M, et al. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010;92(6):1398–1408. [DOI] [PubMed] [Google Scholar]
- 6. Birmingham TB, Giffin JR, Chesworth BM, et al. Medial opening wedge high tibial osteotomy: a prospective cohort study of gait, radiographic, and patient-reported outcomes. Arthritis Rheum. 2009;61(5):648–657. [DOI] [PubMed] [Google Scholar]
- 7. Bonasia DE, Dettoni F, Sito G, et al. Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: prognostic factors. Am J Sports Med. 2014;42(3):690–698. [DOI] [PubMed] [Google Scholar]
- 8. Brown MJ, Farrell JP, Kluczynski MA, Marzo JM. Biomechanical effects of a horizontal medial meniscal tear and subsequent leaflet resection. Am J Sports Med. 2016;44(4):850–854. [DOI] [PubMed] [Google Scholar]
- 9. Cotic M, Vogt S, Hinterwimmer S, et al. A matched-pair comparison of two different locking plates for valgus-producing medial open-wedge high tibial osteotomy: peek-carbon composite plate versus titanium plate. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):2032–2040. [DOI] [PubMed] [Google Scholar]
- 10. Di Caprio F, Meringolo R, Navarra MA, Mosca M, Ponziani L. Postarthroscopy osteonecrosis of the knee: current concepts. Joints. 2017;5(4):229–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Englund M, Guermazi A, Gale D, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359(11):1108–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Englund M, Roemer FW, Hayashi D, Crema MD, Guermazi A. Meniscus pathology, osteoarthritis and the treatment controversy. Nat Rev Rheumatol. 2012;8(7):412–419. [DOI] [PubMed] [Google Scholar]
- 13. Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum. 2003;48(8):2178–2187. [DOI] [PubMed] [Google Scholar]
- 14. Englund M, Roos EM, Roos HP, Lohmander LS. Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology (Oxford). 2001;40(6):631–639. [DOI] [PubMed] [Google Scholar]
- 15. Feldesman MR, Kleckner JG, Lundy JK. Femur/stature ratio and estimates of stature in mid- and late-Pleistocene fossil hominids. Am J Phys Anthropol. 1990;83(3):359–372. [DOI] [PubMed] [Google Scholar]
- 16. Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):170–180. [DOI] [PubMed] [Google Scholar]
- 17. Goyal KS, Pan TJ, Tran D, Dumpe SC, Zhang X, Harner CD. Vertical tears of the lateral meniscus: effects on in vitro tibiofemoral joint mechanics. Orthop J Sports Med. 2014;2(8):23259 67114541237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Haemer JM, Wang MJ, Carter DR, Giori NJ. Benefit of single-leaf resection for horizontal meniscus tear. Clin Orthop Relat Res. 2007;457:194–202. [DOI] [PubMed] [Google Scholar]
- 19. Herrlin S, Hallander M, Wange P, Weidenhielm L, Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):393–401. [DOI] [PubMed] [Google Scholar]
- 20. Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed] [Google Scholar]
- 21. Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ. 2016;354:i3740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Koh JL, Yi SJ, Ren Y, Zimmerman TA, Zhang LQ. Tibiofemoral contact mechanics with horizontal cleavage tear and resection of the medial meniscus in the human knee. J Bone Joint Surg Am. 2016;98(21):1829–1836. [DOI] [PubMed] [Google Scholar]
- 23. Lau BC, Conway D, Mulvihill J, Zhang AZ, Feeley BT. Biomechanical consequences of meniscal tear, partial meniscectomy, and meniscal repair in the knee. JBJS Rev. 2018;6(4):e3. [DOI] [PubMed] [Google Scholar]
- 24. Mina C, Garrett WE, Jr, Pietrobon R, Glisson R, Higgins L. High tibial osteotomy for unloading osteochondral defects in the medial compartment of the knee. Am J Sports Med. 2008;36(5):949–955. [DOI] [PubMed] [Google Scholar]
- 25. Muriuki MG, Tuason DA, Tucker BG, Harner CD. Changes in tibiofemoral contact mechanics following radial split and vertical tears of the medial meniscus an in vitro investigation of the efficacy of arthroscopic repair. J Bone Joint Surg Am. 2011;93(12):1089–1095. [DOI] [PubMed] [Google Scholar]
- 26. Muscolo DL, Costa-Paz M, Makino A, Ayerza MA. Osteonecrosis of the knee following arthroscopic meniscectomy in patients over 50-years old. Arthroscopy. 1996;12(3):273–279. [DOI] [PubMed] [Google Scholar]
- 27. Roos H, Lauren M, Adalberth T, Roos EM, Jonsson K, Lohmander LS. Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum. 1998;41(4):687–693. [DOI] [PubMed] [Google Scholar]
- 28. Schuster P, Gesslein M, Schlumberger M, et al. Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and varus malalignment. Am J Sports Med. 2018;46(6):1362–1370. [DOI] [PubMed] [Google Scholar]
- 29. Turker M, Cetik O, Cirpar M, Durusoy S, Comert B. Postarthroscopy osteonecrosis of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):246–250. [DOI] [PubMed] [Google Scholar]
- 30. Yim JH, Seon JK, Song EK, et al. A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med. 2013;41(7):1565–1570. [DOI] [PubMed] [Google Scholar]