Abstract
We aim to examine the relationship between diabetes and depression risk in longitudinal cohort studies and by how much the incidence of depression in a population would be reduced if diabetes was reduced. Medline/PubMed, EMBASE, PsycINFO, and Cochrane Library databases were searched for English-language published literature from January 1990 to December 2017. Longitudinal studies with criteria for depression and self-report doctors' diagnoses or diagnostic blood test measurement of diabetes were assessed. Systematic review with meta-analysis synthesized the results. Study quality, heterogeneity, and publication bias were examined. Pooled odds ratios were calculated using random effects models. Population attributable fractions (PAFs) were used to estimate potential preventive impact. Twenty high-quality articles met inclusion criteria and were analyzed. The pooled odds ratio (OR) between diabetes and depression was 1.33 (95% CI, 1.18–1.51). For the various study types the ORs were as follows: prospective studies (OR 1.34, 95% CI 1.14–1.57); retrospective studies (OR 1.30, 95% CI 1.05–1.62); self-reported diagnosis of diabetes (OR 1.37, 95% CI 1.17–1.60); and diagnostic diabetes blood test (OR 1.25, 95% CI 1.04–1.52). PAFs suggest that over 9.5 million of global depression cases are potentially attributable to diabetes. A 10–25% reduction in diabetes could potentially prevent 930,000 to 2.34 million depression cases worldwide. Our systematic review provides fairly robust evidence to support the hypothesis that diabetes is an independent risk factor for depression while also acknowledging the impact of risk factor reduction, study design and diagnostic measurement of exposure which may inform preventive interventions.
Keywords: Epidemiology, Diabetes, Depression, Systematic review, Meta-analysis, Population attributable fractions, Projected effects
Highlights
-
•
Depression risk is 1.33 times higher in people with diabetes.
-
•
Prospective studies likely to report depression incidence
-
•
Self-reported diabetes diagnoses likely to report depression
-
•
A 10–25% diabetes reduction could prevent 930,000–2.34 million depression.
1. Introduction
The global prevalence of diabetes is on a steady rise. A recent analysis of diabetes worldwide reported that the number of adults aged 18 years and over globally, living with diabetes substantially increased from 108 million in 1980 to 422 million as of the year 2014, almost a 400% increase (NCD Risk Factor Collaboration (NCD-RisC), 2016). Population growth and population aging have also contributed to the number of diabetes cases worldwide (NCD Risk Factor Collaboration (NCD-RisC), 2016). Diabetes is recognized as an important determinant of premature death, disability, morbidity, and increased health-system costs (Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration, 2014; Seuring et al., 2015). Depressive symptoms and major depressive disorder (MDD) are more common in people with diabetes compared to those without diabetes. Recent studies revealed that depression is twice as prevalent among individuals with Type 2 diabetes compared to controls (Anderson et al., 2001; Ali et al., 2006). Some researchers have argued that diabetes precedes depression and increases the risk of developing depression due to the psychological trauma following diagnoses of diabetes and its burdens such as hyperglycemia leading to altered glucose transport or treatment of the disease itself or both combined as they pose significant challenges for clinical practice (Anderson et al., 2001; Engum, 2007). This line of argument was challenged by recent longitudinal studies that found that depression may be a risk factor for diabetes (Anderson et al., 2001; Golden et al., 2008) but diabetes may not necessarily predict depression or diabetes may just be modestly associated with depression (Engum, 2007). A recent WHO study reported individuals with both conditions are more likely to rate their health as poor more in comparison to individuals with depression only or other chronic conditions only (Moussavi et al., 2007).
Depression, a common and often recurrent disorder has a number of risk factors which have been documented in the literature. Some of these include comorbidities with other conditions (van der Veen et al., 2015), other mental illnesses (WHO. Promoting Mental Health, 2004), family history of depression and mental illness (Myrna et al., 2016), adverse events of childhood (Li et al., 2016), prior history of depression (Ian et al., 2011), and treatment of depression and outcomes of treatment (Miquel et al., 2011), physical inactivity (Meng and D'Arcy, 2013), female gender, younger adults, smoking and having a chronic disease (Meng and D'Arcy, 2014), and unhealthy eating styles (Rawana et al., 2010). Depression is also a large burden on most economies (Egede et al., 2002) and leads to increased mortality (Bruce et al., 2005; Katon et al., 2005). Regular screening for depression is recommended by most clinical guidelines for diabetes (International Diabetes Federation, 2005; National Institute for Health and Clinical Excellence, 2009).
Most studies in this subject utilized cross-sectional study designs which limits causal inferences, making recommendations for practice problematic (Anderson et al., 2001; Ali et al., 2006). A number of systematic reviews and meta-analyses (Knol et al., 2006; Cosgrove et al., 2008; Mezuk et al., 2008; Yu et al., 2015; Vancampfort et al., 2015) found that depression was associated with an increased risk of incident diabetes while earlier systematic reviews and meta-analysis found the reverse that is individuals with diabetes had a modestly increased risk of developing depression (Mezuk et al., 2008; Nouwen et al., 2010; Rotella and Mannucci, 2013; Syed et al., 2015; Tong et al., 2016). The possibility of a bidirectional relationship has gained much attention in recent years become the focus of a number of longitudinal prospective studies, literature reviews, systematic reviews and meta-analysis (Pan et al., 2010; Zhuang et al., 2017; Alzoubi et al., 2018; Hasan et al., 2013; Roy and Lloyd, 2012).
A variety of biological pathways that have been mooted as being shared origins for depression and diabetes including innate immunity and inflammation, the hypothalamic –pituitary-adrenal-axis (HPA axis), insulin resistance and secretion, circadian rhythms, and anti-depressant medications. In-utero and early childhood experiences are also posited as a common pathway linking depression and diabetes, particularly Type 2 diabetes (Holt et al., 2014; Moulton et al., 2015).
In previous reviews, the authors did not distinguish between studies that used diagnostic blood tests to diagnose diabetes and those that used self-report. Studies using self-report usually underestimate diabetes prevalence in contrast to studies that use diagnostic blood tests (Bowlin et al., 1996). In addition, there is little information on the potential impact of reducing diabetes prevalence in decreasing the incidence of depression in a population or vice versa. Population attributable fractions (PAFs) are used to indicate the proportional reduction of a disease in a population (incidence or mortality) that would occur if exposure to a risk factor were reduced to an ideal exposure level (Rockhill et al., 1998). PAFs are recognized as an effective tool for measuring the potential effects of risk factors reduction on disease occurrence (Sareen et al., 2008; Bolton and Robinson, 2010; Barnes and Yaffe, 2011; Meng and D'Arcy, 2013; Meng and D'Arcy, 2014). Northridge (Northridge, 1995) writes that PAFs can assist policy-makers in judging priorities for public health action, intervention planning, and decision-making.
The current study aims to: (1) systematically examine the relationship between diabetes, measured using both self-report of doctor's diagnoses and blood tests, and depression risk in longitudinal cohort studies and (2) provide estimates of by how much the population incidence of depression would be reduced if diabetes was reduced. While a previous study (Nouwen et al., 2010) sub-analyzed their results according to the outcome (depression), our analyses were based on sub-analysis according to the method of diagnoses of the exposure of interest (diabetes). What this analysis adds new is the use of only longitudinal cohort studies, separate analysis of studies that used diagnostic blood tests versus self-report of doctor's diagnoses as measures of diabetes, and the calculation of the potential population's effects on depression incidence of reducing diabetes.
2. Methods – systematic review and meta-analysis
The current systematic review and meta-analysis follow the PRISMA guidelines, 2009 revision (Moher et al., 2009), and the Meta-analysis of Observational Studies in Epidemiology (MOOSE) recommendations (Stroup et al., 2000). The Newcastle–Ottawa Scale criteria were used to characterize study quality (Wells et al., 2012).
2.1. Search strategy
A computerized search for published articles was conducted in Medline/PubMed, EMBASE, PsycINFO, and Cochrane Library databases between January 1990 and December 2017. A manual search was done on other resources for additional relevant studies. We also scanned through the reference lists of the selected articles, as well as review articles on the topic, and also screened for grey literature.
To get a maximum number of relevant citations, we conducted three steps search process under the MeSH terms using relevant keywords or title search. In step I, depression was searched as follows; “depression OR major depressive disorder OR MDD OR depressive disorders OR depression symptoms OR depressive symptoms”. At step II, diabetes was also searched as “diabetes mellitus OR diabetes OR type 2 diabetes OR diabetes symptoms”. In step III, we combined step I AND step II AND (cohort studies OR prospective OR retrospective OR follow up OR follow-up OR longitudinal OR panel OR incident OR concurrent OR incidence) for study literature retrieval.
2.2. Inclusion and exclusion criteria
The following inclusion and exclusion criteria for article selection were used: 1) published between (January 1990 and December 2017); 2) written in English; 3) cohort study designs; 4) use clear diagnostic criteria for depression measured by the use of Centre for Epidemiologic Studies Depression Scale Questionnaire (CES-D), Hospital Anxiety and Depression Scale Questionnaire (HADS), Beck Depression Inventory (BDI), a structured diagnostic interview, or other measurements such as antidepressants use (American Psychiatric Association, 2013; WHO, 1992),; 5) explicit exclusion of patients with depression at baseline; 6) give clear information on the diagnosis of diabetes used either a self-report of a doctor's diagnosis or a diagnostic blood test to measure diabetes;7) provided a statistical indicator (relative risk, odds ratio, hazard ratio) or original data to estimate the relationship between diabetes and depression; 8) controlled for confounders by using statistical adjustment in the analysis or matching in the study design. We excluded studies that were: 1) case reports, cross-sectional, case-control, a chart review, or 2) did not provide enough information on key inclusion criteria.
2.3. Selection of articles
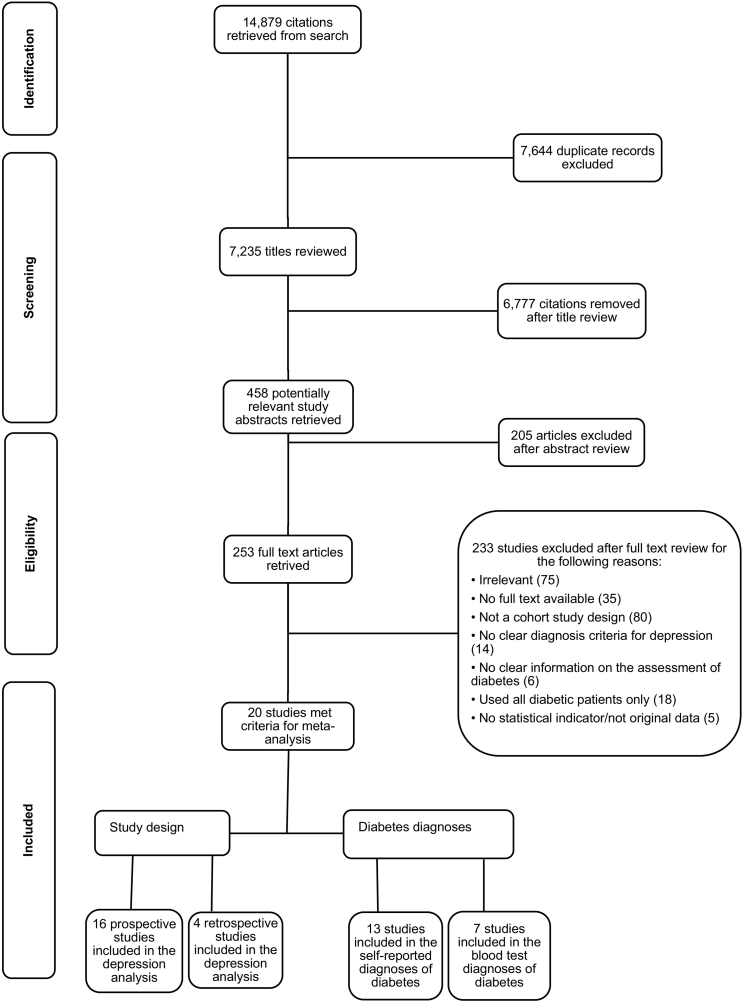
Authors (B.C. and M.L.) independently screened abstracts and full texts and extracted data from the eligible articles. In instances where disagreements emerged, reviewers consulted each other and they were resolved through discussion. The 14,879 titles retrieved in our initial search were later reduced to 7235 after duplicates were excluded. After title review 458 potentially relevant articles remained. After abstract screening, the full-text of 253 articles was retrieved for review. One author of a selected article was contacted for a full-text article after it could not be retrieved online. It was directly sent to us. After full-text review, 20 articles met the selection criteria and were included in the study. Fig. 1 provides details on the articles selection process. Data on author, publication year, journal, sample size, methods, indicators, outcomes, adjustments, study design, and results were extracted independently by two authors [B.C. and M.L.].
Fig. 1.
PRISMA flow diagram – Diabetes and incidence of depression in later life.
2.4. Data synthesis
The analyses generated pooled estimates of the effects of diabetes on depression risk in general and by study design and method of diabetes diagnosis. We evaluated heterogeneity with DerSimonian and Laird I2 statistics for each analysis category (Higgins et al., 2003). In order to provide a visual assessment of publication bias, funnel plots and Egger's tests were used (Egger et al., 1997). A Begg-adjusted rank correlation test was also used to check for publication bias. If these tests showed non-significant heterogeneity, we used fixed-effects model, otherwise, a more conservative random-effects model was used. Sensitivity analysis was performed to assess the influence of each individual study on overall estimates by recalculating odds ratios with studies being removed one at a time. The quality of each study was rated according to the Newcastle–Ottawa Scale. Finally, the influence of each study design and method of diabetes diagnosis on depression incidence and the impact of study quality on results was investigated using meta-regression analyses. Stata v. 14.2 statistical software (StataCorp., USA) was used for the analyses.
2.5. Calculation of projected effects – population attributable fractions (PAFs)
PAF represents the proportional reduction in disease risk that would be achieved by removing an exposure or reducing it to a specified level. It estimates the proportion of a disease in a population that is potentially attributable to a given risk factor (Benichou, 2001). PAFs estimate the strength of association between a risk factor and a disease outcome. We used the following formula derived from the literature (Rockhill et al., 1998; Sareen et al., 2008; Barnes and Yaffe, 2011).
where p represents the population prevalence of the exposure and OR is the pooled odds ratio of outcomes given different categories of diabetes diagnosis and the different study designs. We used the worldwide prevalence estimates of diabetes to generate PAFs for prospective and retrospective studies as well as self-reported doctor's diagnosis and diagnostic blood test for diabetes (NCD Risk Factor Collaboration (NCD-RisC), 2016).
Finally, we estimated the total number of depression cases attributable to diabetes by multiplying PAF estimates and the present number of cases worldwide. We also calculated the number of cases that could potentially have been prevented if the prevalence of diabetes were 10% or 25% lower. Confidence ranges for the PAF estimates were calculated.
3. Results
We retrieved 14,879 citations in our initial search which later reduced to 7235 titles after duplicates were excluded. Another 6777 articles were removed after title review which resulted in 458 potentially relevant articles remaining. A little over half of the articles (253) were maintained after the abstract screening. A final list of 20 articles that met the criteria for meta-analysis after full-text screening and were included in the study (Asamsama et al., 2015; Chen et al., 2013; de Jonge et al., 2006; Golden et al., 2008; Hamer et al., 2011; Hasan et al., 2015; Icks et al., 2013; Kim et al., 2006; Luijendijk et al., 2008; Polsky et al., 2005; Pan et al., 2010; Garcia et al., 2016; Maraldi et al., 2007; Engum, 2007; Palinkas et al., 2004; Brown et al., 2006; Aarts et al., 2009; Finkelstein et al., 2003; O'Connor et al., 2009). Table 1 shows the detailed summary of study attributes and data on the characteristics of the reviewed articles. Articles were assess based on; population representativeness, accuracy in selecting non-exposed groups, the absence of the outcome of interest before the start of the study, proper assessment of both exposure and outcome, adequate follow-up period for the outcome to occur, appropriate statistical analysis, control for confounding and other related information. This quality is evident in the fact that none of the study characteristics examined had any impact on observed odds ratios in any of our analyses and by the absence of any publication bias.
Table 1.
Summary of studies' attributes.
| First Author | Year | Setting | Study design | Sample/data source | Sample size | Age of exposure | Follow–up (years) |
Ascertainment of exposure | Assessment of health outcome | Depression criteriaa |
|---|---|---|---|---|---|---|---|---|---|---|
| Asamsama et al. (Asamsama et al., 2015) | 2015 | USA | Prospective | Biopsychosocial Religion and Health Study of Adventist Adults | 4152 | ≥61 | 3 | Self-report of doctor's diagnosis | Centre for Epidemiologic Study Depression Scale Questionnaire | CES-D scale score ≥ 16 |
| Bisschop et al. (Bisschop et al., 2004) | 2004 | Netherlands | Prospective | Longitudinal Aging Study Amsterdam | 1839 | 55–85 | 6 | Self-report of doctor's diagnosis | Centre for Epidemiologic Study Depression Scale Questionnaire | CES-D scale score ≥ 16 |
| Chen et al. (Chen et al., 2013) | 2013 | Taiwan | Prospective | National Health Insurance claims of the General population | 33,914 | ≥35 | 7 | Self-report of doctor's diagnosis | Medical reports | Physician-diagnosed depression |
| de Jonge et al. (de Jonge et al., 2006) | 2006 | Spain | Prospective | Community based study of the elderly | 4757 | ≥55 | 5 | Self-report of doctor's diagnosis | Structured Interview (GMS & AGECAT) | GMS-AGECAT ≥3 |
| Engum (Engum, 2007) | 2007 | Norway | Prospective | Nord-Trøndelag Health Study | 37,291 | ≥30 | 10 | Self-report of doctor's diagnosis | Hospital Anxiety and Depression Scale Questionnaire | HADS-D scale score ≥ 8 |
| Garcia et al. (Garcia et al., 2016) | 2016 | USA | Prospective | Sacramento Latino Study on Aging | 1583 | ≥60 | 10 | Fasting blood glucose | Centre for Epidemiologic Study Depression Scale Questionnaire | CES-D scale score ≥ 16 |
| Golden et al. (Golden et al., 2008) | 2008 | USA | Prospective | Multi-Ethnic Study of Atherosclerosis | 5201 | 45–84 | 3 | Fasting Plasma Glucose (FPG) | Centre for Epidemiologic Study Depression Scale Questionnaire | CES-D scale score ≥ 16 |
| Hamer et al. (Hamer et al., 2011) | 2011 | England | Prospective | English Longitudinal Study of Aging (ELSA) | 4338 | ≥62 | 2 | Fasting Plasma Glucose (FPG) | Centre for Epidemiologic Study Depression Scale Questionnaire | CES-D scale score ≥ 4 |
| Hasan et al. (Hasan et al., 2015) | 2015 | Australia | Prospective | Australian Pregnancy and Birth Cohort Study | 2791 | Agenotspecified | 6 | Self-report of doctor's diagnosis | Delusions-Symptoms-States-Inventory (DSSI) | DSSI score ≥ 4 |
| Icks et al. (Icks et al., 2013) | 2013 | Germany | Prospective | Population-based Heinz Nixdorf Recall Study | 3633 | 45–75 | 5 | Fasting blood glucose | Centre for Epidemiologic Study Depression Scale Questionnaire | CES-D scale score ≥ 17 |
| Kim et al. (Kim et al., 2006) | 2006 | South Korea | Prospective | Community Residents aged 65+ | 521 | ≥65 | 2 | Self-report of doctor's diagnosis | Structured Interview (GMS & AGECAT) | GMS-AGECAT ≥3 |
| Luijendijk et al. (Luijendijk et al., 2008) | 2008 | Netherlands | Prospective | Rotterdam Study of Community dwelling elderly | 2931 | ≥61 | 5 | Fasting Plasma Glucose | Centre for Epidemiologic Study Depression Scale Questionnaire | CES-D scale score ≥ 16 |
| Maraldi et al. (Maraldi et al., 2007) | 2007 | USA | Prospective | Health, Aging & body composition study | 2522 | 70–79 | 5.9 | Self-report of doctor's diagnosis | Centre for Epidemiologic Study Depression Scale Questionnaire | CES-D scale score ≥ 10 |
| Pan et al. (Pan et al., 2010) | 2010 | USA | Prospective | Nurses' Health Study Cohort | 56,857 | 50–75 | 10 | Self-report of doctor's diagnosis | Antidepressant medications (drugs) | Physician-diagnosed depression or antidepressant use |
| Palinkas et al. (Palinkas et al., 2004) | 2004 | USA | Prospective | Adult population of Rancho Bernardo | 971 | ≥50 | 8 | Oral Glucose Tolerance Test (OGTT) | Beck Depression Inventory (BDI) | BDI score ≥ 11 |
| Polsky et al. (Polsky et al., 2005) | 2005 | USA | Prospective | Health & Retirement Study of elderly | 8387 | 51–61 | 8 | Self-report of doctor's diagnosis | Centre for Epidemiologic Study Depression Scale Questionnaire | CES-D scale score ≥ 5 |
| Aarts et al. (Aarts et al., 2009) | 2009 | Netherlands | Retrospective | Registration Network Family Practice Study | 24,556 | ≥40 | 7.8 | Fasting Plasma Glucose (FPG) | Diagnostic interview by a specialist | Physician-diagnosed depression |
| Brown et al. (Brown et al., 2006) | 2006 | Canada | Retrospective | Population-based Saskatchewan Residents | 88,776 | ≥20 | 4.5 | Self-report of doctor's diagnosis | Antidepressant medications (drugs) | Physician-diagnosed depression or antidepressant use |
| Finkelstein et al. (Finkelstein et al., 2003) | 2003 | USA | Retrospective | Medicare Standard Analytic Files | 237,864 | ≥65 | 6 | Self-report of doctor's diagnose | Medical reports | Physician-diagnosed depression |
| O'Connor et al. (O'Connor et al., 2009) | 2009 | USA | Retrospective | Health Partners Medical Group (HPMG) | 28,288 | ≥40 | 2 | Self-report of doctor's diagnose | Antidepressant medications (drugs) | Physician-diagnosed depression or antidepressant use |
CES-D Scale: Centre for Epidemiologic Studies Depression Scale. GMS-AGECAT: Geriatric Mental State Schedule Automated Geriatric Examination for Computer Assisted Taxonomy. HADS-D: Hospital Anxiety and Depression Scale. DSSI: Delusions –Systems-State-Inventory. BDI: Beck Depression Inventory.
The reviewed articles were categorized into four groups for the analyses: (1) prospective studies and depression incidence; (2) retrospective studies and depression incidence; (3) self-reported doctor's diagnosis of diabetes and depression incidence; (4) blood test diagnosis of diabetes and depression incidence. Some studies are involved in multiple separate analyses as their available data permitted.
3.1. Relationship between diabetes and depression in prospective studies
Sixteen articles (Bisschop et al., 2004; Asamsama et al., 2015; Chen et al., 2013; de Jonge et al., 2006; Golden et al., 2008; Hamer et al., 2011; Hasan et al., 2015; Icks et al., 2013; Kim et al., 2006; Luijendijk et al., 2008; Polsky et al., 2005; Pan et al., 2010; Garcia et al., 2016; Maraldi et al., 2007; Engum, 2007; Palinkas et al., 2004) used prospective study designs in examining the relationship between diabetes and depression incidence. Most of these studies used the Epidemiologic Studies Depression Scale Questionnaire (CES-D) to measure depression. They had a median follow-up period of 5.95 years. Eight studies(Chen et al., 2013; de Jonge et al., 2006; Hamer et al., 2011; Hasan et al., 2015; Luijendijk et al., 2008; Pan et al., 2010; Garcia et al., 2016; Maraldi et al., 2007) with a median follow-up of 5.95 years reported a significant association between diabetes and depression incidence, the other eight studies (Bisschop et al., 2004; Asamsama et al., 2015; Golden et al., 2008; Icks et al., 2013; Kim et al., 2006; Polsky et al., 2005; Engum, 2007; Palinkas et al., 2004) with a median follow-up of 5.5 years reported no association.
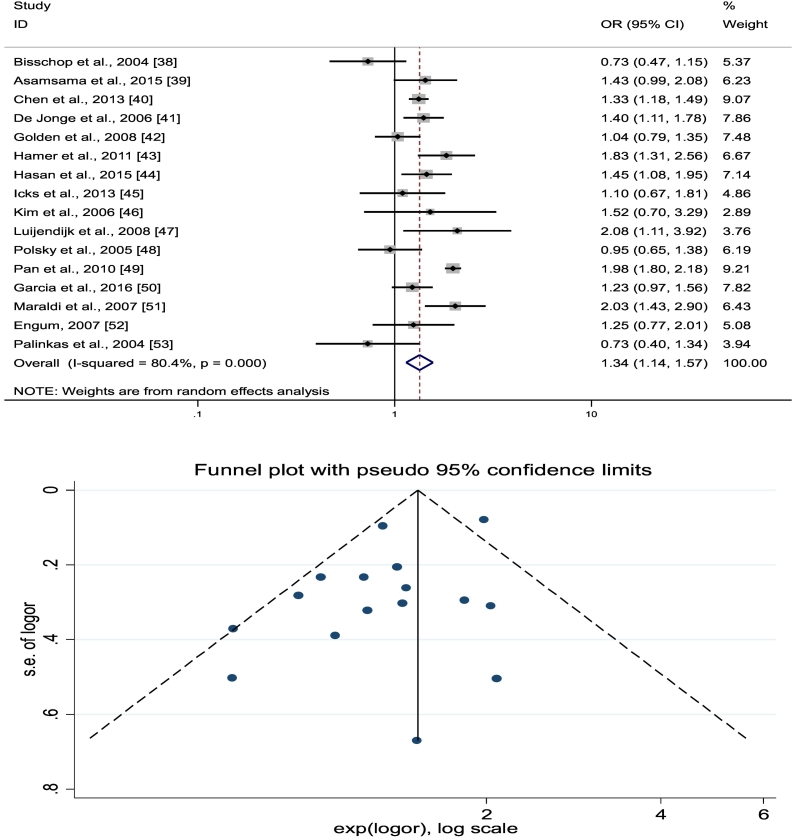
Fig. 2a presents the individual study, pooled estimates, and funnel plots for this group of studies. A random-effects model was used. The pooled OR for incident depression among respondents with diabetes in these prospective studies was 1.34 (95% CI 1.14–1.57, χ2 = 76.65, I2 = 80.4%, p < .001) clearly indicating that diabetes was a risk factor for depression. Fig. 2a shows all the studies were within the domain which represents 95% CI limits. No evidence of asymmetry or publication bias was found (Egger's test, p = .053). Sensitivity analysis yielded ORs ranging from 1.29 (95% CI 1.14–1.47) to 1.39 (95% CI 1.19–1.62) in these prospective studies.
Fig. 2.
a Prospective studies and risk of depression.
b: Retrospective studies and risk of depression.
c: Self-report doctors' diagnosis of diabetes and risk of depression.
d: Blood test diagnoses of diabetes and risk of depression.
3.2. Relationship between diabetes and depression in retrospective studies
Four articles (Brown et al., 2006; Aarts et al., 2009; Finkelstein et al., 2003; O'Connor et al., 2009) used retrospective study designs to examine diabetes and incident depression relationship. Depression was assessed through antidepressants use, medical reports or structured interviews by a specialist. The median follow-up time was 5.25 years. Two studies (Aarts et al., 2009; Finkelstein et al., 2003) with a median follow-up of 6.9 years reported an association while the two other studies (Brown et al., 2006; O'Connor et al., 2009) with an average follow-up of 3.25 years did not find an association. Fig. 2b shows the individual study and pooled estimates, and funnel plots. A random-effects model was used. The pooled OR for these studies was 1.30 (95% CI 1.05–1.62, χ2 = 46.71, I2 = 93.6%, p < .000). No asymmetry or publication bias was found (Egger's test, p = .85). Sensitivity analyses for the retrospective studies reported ORs ranging from 1.23 (95% CI 0.95–1.60) to 1.46 (95% CI 1.34–1.59).
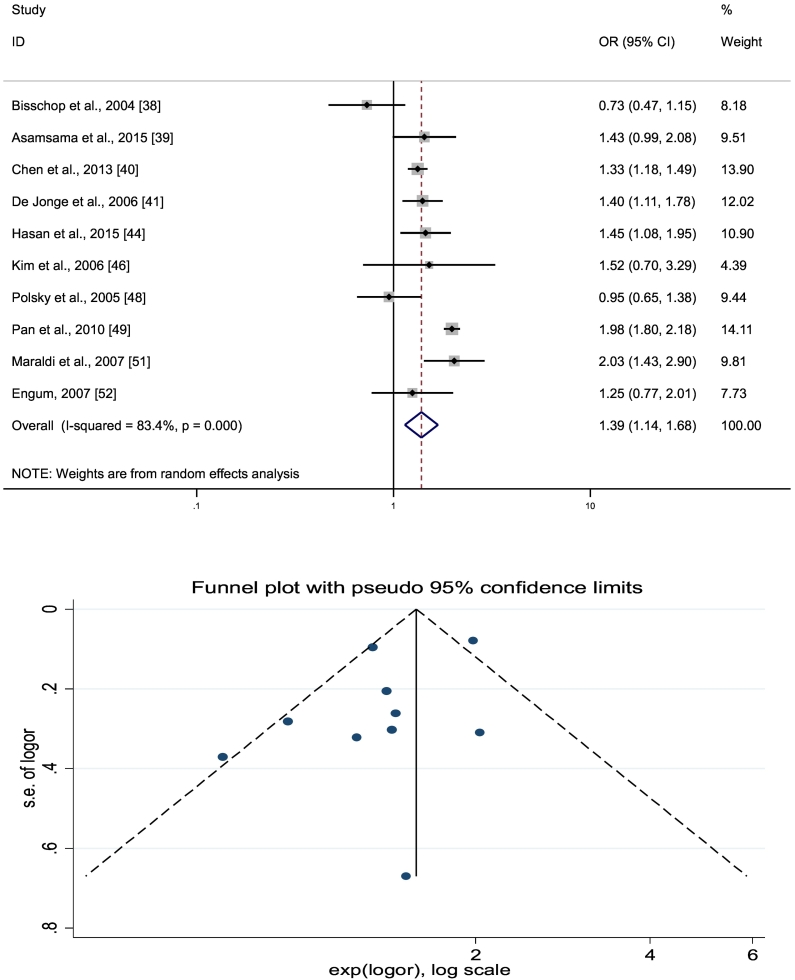
3.3. Relationship between self-report of doctors' diagnosis of diabetes and depression
Thirteen articles (Bisschop et al., 2004; Asamsama et al., 2015; Chen et al., 2013; de Jonge et al., 2006; Hasan et al., 2015; Kim et al., 2006; Polsky et al., 2005; Pan et al., 2010; Maraldi et al., 2007; Engum, 2007; Brown et al., 2006; Finkelstein et al., 2003; O'Connor et al., 2009) measured diabetes using self-reported doctor's diagnosis of diabetes. Fig. 2c presents the individual study ORs, pooled estimates, and funnel plots. A random-effects model was used. The pooled OR for incident depression for these studies was 1.37 (95% CI 1.17–1.160, χ2 = 127.51, I2 = 90.6%, p < .001). No asymmetry or publication bias was found (Egger's test, p = 0. 848). Sensitivity analysis produced ORs ranging from 1.32 (95% CI 1.15–1.51) to 1.43 (95% CI 1.26–1.63).
3.4. Relationship between diabetes and depression in studies using a diagnostic blood test to diagnose diabetes
Seven articles (Golden et al., 2008; Hamer et al., 2011; Icks et al., 2013; Luijendijk et al., 2008; Garcia et al., 2016; Palinkas et al., 2004; Aarts et al., 2009) were included in this sub-analysis. A random-effects model was used. Fig. 2d reports individual study estimates, pooled estimates, and funnel plots. The pooled OR for incident depression in these studies was 1.25 (95% CI 1.04–1.52, χ2 = 12.76, I2 = 53.0%, p = .047). No asymmetry or publication bias was present (Egger's test = 0. 896). Sensitivity analysis yielded ORs ranging from 1.17 (95% CI 1.0–1.38) to 1.31 (95% CI 1.06–1.62).
3.5. Prospective studies of diabetes and depression that used self-report of doctors' diagnosis of diabetes
Ten prospective studies (Bisschop et al., 2004; Asamsama et al., 2015; Chen et al., 2013; de Jonge et al., 2006; Hasan et al., 2015; Kim et al., 2006; Polsky et al., 2005; Maraldi et al., 2007; Engum, 2007) used self-report of a doctors' diagnosis of diabetes. Fig. 3a shows that in prospective studies that used self-report diagnosis of diabetes were 1.39 times (95% CI 1.14–1.68, χ2 = 54.28, I2 = 83.4%, p < .001) more likely to report incident depression compared to those without diabetes. There was some marginal evidence of asymmetry and publication bias (see Table 2).
Fig. 3.
a. Prospective studies and self-report measures of diabetes.
b: Prospective studies and blood test measures of diabetes.
c: Retrospective studies and self-report doctors' diagnosis measures of diabetes.
Table 2.
Summarizes the results of our meta-analysis.
| Study group | Odds ratios (OR) | 95% Confidence interval (CI) | p-Value |
|---|---|---|---|
| Prospective studies | 1.34 | 1.14–1.57 | <0.001 |
| Retrospective studies | 1.30 | 1.05–1.62 | <0.001 |
| Studies using self-report | 1.37 | 1.17–1.60 | <0.001 |
| Studies using blood tests | 1.25 | 1.04–1.52 | 0.047 |
| Prospective studies using self-report measure | 1.39 | 1.14–1.68 | <0.001 |
| Prospective studies using blood test measure | 1.26 | 0.98–1.61 | 0.026 |
| Retrospective studies using self-report measure | 1.32 | 1.02–1.72 | <0.001 |
3.6. Prospective studies of diabetes and depression in studies that use a blood test measure of diabetes
Six prospective studies measured diabetes-depression relationship using diagnostic blood tests (Golden et al., 2008; Hamer et al., 2011; Icks et al., 2013; Luijendijk et al., 2008; Garcia et al., 2016; Palinkas et al., 2004). In comparison to prospective self-report studies these studies did not show diabetes as a risk factor for incident depression (OR = 1.26, 95% CI 0.98–1.61, χ2 = 12.78, I2 = 60.9%, p = .026). The non-significant results are shown in Fig. 3b. However, three of the six studies reported a positive relationship. There was no evidence of asymmetry or publication bias.
3.7. Retrospective studies of diabetes and depression in studies using self-report of doctors' diagnoses of diabetes
Three of these four retrospective studies (Brown et al., 2006; Finkelstein et al., 2003; O'Connor et al., 2009) used self-report diagnosis of diabetes to examine the diabetes-depression relationship. The pooled odds for these studies showed that individuals with diabetes were 1.32 times (95% CI 1.02–1.72, χ2 = 46.66, I2 = 95.7%, p < .001) more likely to report incident depression (see Fig. 3c). Asymmetry and publication bias was evident. The one study (Aarts et al., 2009) that used a diagnostic blood test measure reported an OR of 1.25 (CI 1.01–1.54).
In summary, our analyses show that although there is some variability in findings by study method the pooled ORs emerging from this group of studies generally support findings that diabetes is a risk factor for depression (Table 2).
3.8. Projected effects (PAFs) of risk reduction
3.8.1. Prevalence of diabetes and PAFs
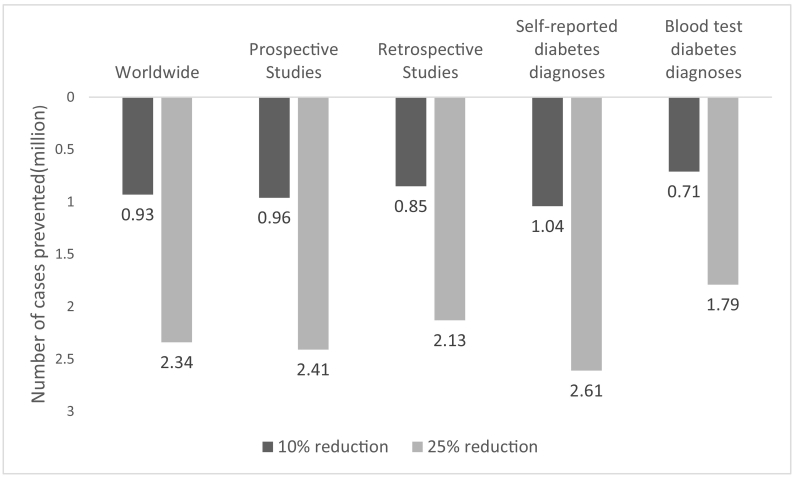
As of 2016, the worldwide estimated prevalence of diabetes was 8.5% (422 million) (NCD Risk Factor Collaboration (NCD-RisC), 2016) whilst that of depression was estimated to affect 350 million (WHO, 2012). The PAF estimates used here for the effect of diabetes on the incidence of depression is 2.73%, which indicates that over (9.55 million) of depression cases are potentially attributable to diabetes globally (Table 3). If the global prevalence of diabetes was reduced by 10%, we estimated that there would be (930,000) fewer depression cases worldwide, whereas a 25% reduction in diabetes could reduce depression prevalence by (2.34 million) cases (Fig. 4). It should be noted that the number of cases attributable to diabetes may be overestimated as a result of co-morbidity with other chronic diseases. Many diseases are caused by multiple risk factors, and individual risk factors may interact in their impact on overall risk of disease. Using prospective study values it is estimated that 2.81% (over 9.83 million) of depression cases in the world are potentially attributable to diabetes. If the incidence of diabetes was reduced by 10%, 960,000 cases of depression could potentially be reduced; whilst a 25% reduction in the incidence of diabetes would result in reducing the incidence of depression by 2.41 million cases worldwide. Using retrospective study values yields slightly lower estimates of reduction in the incidence of depression. Estimates from studies using self-report and blood test measure again yield sizeable reductions in depression incidence (see Fig. 4).
Table 3.
Estimated depression cases attributable to diabetes presence worldwide by type of study design.
| Pooled OR (95% CI) | Population prevalence of diabetes | PAF (confidence range) | Number of cases attributable-millions (confidence range) | |
|---|---|---|---|---|
| Worldwide | 1.33 (1.18–1.51) | 8.50% | 2.73% (1.51–4.15) | 9.55 (5.27–14.54) |
| Prospective and depression | 1.34 (1.14–1.57) | 8.50% | 2.81% (1.18–4.62) | 9.83 (4.12–16.17) |
| Retrospective and depression | 1.30 (1.05–1.62) | 8.50% | 2.49% (0.42–5.01) | 8.70 (1.48–17.52) |
| Self-reported diabetes measure and depression | 1.37 (1.17–1.60) | 8.50% | 3.05% (1.42–4.85) | 10.67 (4.99–16.98) |
| Blood test diabetes measure and depression | 1.25 (1.04–1.52) | 8.50% | 2.08% (0.34–4.23) | 7.28 (1.19–14.82) |
OR, Odds ratio; CI, confidence interval; PAF, population attributable fraction.
Fig. 4.
Potential depression cases that could be prevented through diabetes reduction worldwide estimates based on various study designs.
4. Discussion
This meta-analysis generally showed that people with diabetes had a greater risk of developing depression compared to those without. Out of the 20 studies involving 547,417 participants, half of them (10 studies) constituting 67.6% of the participant population suggested increased depression risk. The pooled OR between diabetes and depression for all the studies included in this analysis was 1.33 (95% CI 1.18–1.51). The ORs for various study types were: prospective studies OR 1.34 (95% CI 1.14–1.57); retrospective OR 1.30 (95% CI 1.05–1.62); self-reported doctor's diagnosis OR 1.37 (95% CI 1.17–1.60) and blood test diagnosis OR 1.25 (95% CI 1.04–1.52). Specific studies that did not find an increased risk of depression generally had smaller sample sizes, had a shorter follow-up period and had an earlier publication date. Conversely, studies that found a relationship between the two conditions had long years of follow-up, larger sample size and published more recently.
Our results are consistent with previous reviews that reported diabetes was a risk factor for depression. The pooled OR of 1.33 reported in this systematic review is higher than the ORs reported in previous meta-analyses of 1.15 (95% CI 1.02–1.30), 1.24 (95% CI 1.09–1.40) and 1.29 (95% CI 1.03–1.63) respectively (Mezuk et al., 2008; Nouwen et al., 2010; Tong et al., 2016) but fell short of a two-fold increased risk of depression in diabetes found in a previous meta-analysis (Anderson et al., 2001). Also, our current finding is in keeping with recent bidirectional reviews measuring the relationship between diabetes and depression where a moderate association was found between the two debilitating conditions (Zhuang et al., 2017; Hasan et al., 2013; Roy and Lloyd, 2012). Our review is however at odds with a small meta-analysis that involved 3 longitudinal studies which found those with diabetes to have had an insignificant higher risk of developing incident depression compared to controls, RR 1.50 (95% CI 0.92–2.44) (Chang-Quan et al., 2010).
Overall prospective studies using both diabetes diagnosis methods reviewed here found that respondents with diabetes were 34% more likely to develop depression compared to controls (OR 1.34, 95% CI 1.14–1.57) while retrospective study designs found those with diabetes were 1.30 times more likely to develop depression. These findings are consistent with an earlier meta-analysis of seven longitudinal studies where the pooled OR for risk of depression was 1.15 (95% CI 1.02–1.30) (Mezuk et al., 2008).
A previous meta-analysis of studies using clinical measures of diabetes reported smaller effects (RR1.11) compared to self-reported studies (RR 1.16) (Mezuk et al., 2008). We found that studies using self-report of doctor's diagnosis showed a slightly larger effect (OR 1.37, 95% CI 1.17–1.60) than studies that used clinical measures or diagnostic blood tests. Our study is consistent with what has been earlier reported (Mezuk et al., 2008). Among the seven studies analyzed here that examined the relationship between diabetes and depression using diagnostic blood tests, we found a pooled OR = 1.25 (95% CI 1.04–1.52). Four of the studies largely from the USA reported a negative relationship between diabetes and depression while three of the studies, from two European countries, reported a positive relationship between diabetes and depression. The literature suggests that while the overall prevalence of obesity among adults has increased in the US, there are significant ethnic or racial disparities with the highest prevalence among the African-American populations (Ogden et al., 2013). We suggest that the sample variations in these studies, oversampling of white or Latino populations, could possibly explain the non-significant results reported.
In our review heterogeneity was large compared to previous reviews (Mezuk et al., 2008; Nouwen et al., 2010). This could probably be due to the fact that, earlier studies did not report a more increased risk of depression in people with diabetes is currently being reported by later studies owing to differences in clinical and methodological aspects. We cannot authoritatively state why recent studies report an increased risk of depression in people with diabetes. However, a plausible explanation could be that health care professionals and patients with diabetes are increasingly becoming knowledgeable about depression or depressive symptoms in people with diabetes and this could possibly influence responses during follow-up periods. But the results of this study should be interpreted with caution since it is possible that the incident depression reported in this study can be due to recurrence of depressive disorder among those with a history of depression or as a result of diabetes-related complications.
To the authors' knowledge, this is the first study to provide quantitative estimates on the projected reduction of depression cases that could result from a reduction in the worldwide prevalence of diabetes. The PAFs estimates show a significant number of depression cases worldwide (9.55 million) are potentially attributable to diabetes prevalence. Measures used to reduce the prevalence of diabetes will eventually lead to a reduction in depression and that should be the focus of public health prevention efforts. This study projects that a 10–25% reduction in diabetes prevalence could potentially prevent 930,000–2.34 million depression cases worldwide.
4.1.1. Strength and limitations of the current study
The major strength of this study comes from the pooled findings of longitudinal cohort studies and the relatively large number of studies involved. The reviewed studies were of high quality. We also provided PAF estimates to show the potential impact of substantially reducing diabetes prevalence on the global incidence of depression. However, the current study has limitations that may affect generalizability. First and foremost, the study is limited by our restriction of the literature search to only studies conducted in the English language since there have been divergent views on the impact of language bias on the quality of systematic reviews. Secondly, our reviewed studies were not geographically representative of the world's population. Majority of the studies reviewed emanated from the US, Europe, and other developed countries. There were no studies from Africa, South America, and other developing countries. However, the International Diabetes Federation 2013 report suggested that about 80% of people living with diabetes are resident in low and middle-income countries (International Diabetes Federation, 2013).
In addition, some of our studies failed to adequately adjust for strong moderating factors such as gender, smoking, alcohol abuse, and the presence of other chronic diseases (Albers et al., 2011). Confounding is possible. Another limitation is the high values of heterogeneity that were recorded in 3 out of the 4 analyses performed in our meta-analysis. This shows substantial variation in the degree of association between diabetes and depression in the studies reviewed. We reported on studies using self-report of doctor's diagnosis of diabetes and diagnostic blood tests (fasting plasma glucose or oral glucose tolerance test). Both measures have their respective strengths and limitations. A major drawback of self-reported diagnosis is that it may be an underestimate of the real prevalence of diabetes. On the other hand, it is suggested that a part of the patients classified as having diabetes using diagnostic blood tests (fasting glucose or oral glucose tolerance test) may remain unaware of this diagnosis, thus avoiding the psychological effects of this diagnosis (Bowlin et al., 1996).
It is not clear cut that all self-reported diagnosis lead to over or underestimate diabetes prevalence. We assume that the source of the recorded heterogeneity is either clinical or methodological which suggests the need to adjust for known moderators in future studies of the diabetes-depression relationship.
Finally in estimating PAF values the worldwide prevalence of diabetes was not broken down by the severity of complications, we used crude overall prevalence rate to calculate PAFs. Our PAF estimates did not take into account diabetes severity and its effects on complications and their combined effect on depression incidence. Diabetes in itself does not usually cause death directly but rather it is the complications that arise from the disease that has a substantial impact on an individual's health.
5. Conclusion
Despite limitations, our systematic review provides fairly robust evidence to support the hypothesis that diabetes is a risk factor in the development of depression and that the risk of depression is higher in people with diabetes compared to the general population. This increased risk reported may be due to recurrence of depression among people with a history of depression or as a result of diabetes-related complications. We also note some of the impacts of risk factor reduction, study design, and diagnostic measurements of exposure of interest. More and better-designed cohort studies are still needed to corroborate our study and to also firmly establish the relationship between diabetes and depression and the possibility of a two-way interaction between these disorders. The calculated PAFs showed that a large reduction in the worldwide prevalence of diabetes could translate into a significant reduction in the incidence of depression. However, this impact is not limited to the incidence of depression but has a larger effect because of the clinical and economic repercussions that come with the long-term management and treatment of both conditions globally. Interventions and services for diabetes prevention such as healthy diet, physical activity, and weight loss also improve the mental health of general populations. This review reinforces the need for a holistic approach toward combating diabetes. Well-managed diabetes could help weaken the association between depression and diabetes.
Funding
Batholomew Chireh is a PhD candidate at the University of Saskatchewan and is funded by the University of Saskatchewan School of Public Health Scholarship program.
Conflict of interest statement
The authors have no potential or real conflicts of interest to declare.
Acknowledgments
We thank the University of Saskatchewan School of Public Health Scholarship program for their financial support to the first author.
Contributor Information
Batholomew Chireh, Email: bac563@mail.usask.ca.
Muzi Li, Email: mul280@mail.usask.ca.
Carl D'Arcy, Email: kcd156@mail.usask.ca.
References
- Aarts S., van den Akker M., van Boxtel M.P. Diabetes mellitus type II as a risk factor for depression: a lower than expected risk in a general practice setting. Eur. J. Epidemiol. 2009;24(10):641–648. doi: 10.1007/s10654-009-9385-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albers B., Kruse J., Giani G. Diabetes and incident depression: is the association mediated or modified by sociodemographic factors or co-morbidities? A systematic review. Exp. Clin. Endocrinol. Diabetes. 2011;119(10):591–598. doi: 10.1055/s-0031-1280800. [DOI] [PubMed] [Google Scholar]
- Ali S., Stone M.A., Peters J.L. The prevalence of co-morbid depression in adults with type 2 diabetes: a systematic review and meta-analysis. Diabet. Med. 2006;23:1165–1173. doi: 10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]
- Alzoubi A., Abunaser R., Khassawneh A. The bidirectional relationship between diabetes and depression: a literature review. J. Korean Acad. Fam. Med. 2018;39(3):137–146. doi: 10.4082/kjfm.2018.39.3.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . 5th ed. American Psychiatric Publishing; Arlington, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Anderson R.J., Freedland K.E., Clouse R.E., Lustman P.J. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- Asamsama O.H., Jerry W.L., Kelly R.M., Serena T. Bidirectional longitudinal study of type 2 diabetes and depression symptoms in black and white church going adults. J. Diabetes Metab. Disord. 2015;14(25):1–7. doi: 10.1186/s40200-015-0150-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes D.E., Yaffe K. The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol. 2011;10:819–828. doi: 10.1016/S1474-4422(11)70072-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benichou J. A review of adjusted estimators of attributable risk. Stat. Methods Med. Res. 2001;10:195–216. doi: 10.1177/096228020101000303. [DOI] [PubMed] [Google Scholar]
- Bisschop M.I., Kriegsman D.M.W., Deeg D.J.H., Beekman A.T.F., Tilburg W.V. The longitudinal relation between chronic diseases and depression in older persons in the community: the longitudinal aging study Amsterdam. J. Clin. Epidemiol. 2004;57:187–194. doi: 10.1016/j.jclinepi.2003.01.001. [DOI] [PubMed] [Google Scholar]
- Bolton J.M., Robinson J. Population-attributable fractions of Axis I and Axis II mental disorders for suicide attempts: findings from a representative sample of the adult, noninstitutionalized US population. Am. J. Public Health. 2010;100:2473–2480. doi: 10.2105/AJPH.2010.192252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlin S.J., Morrill B.D., Nafziger A.N. Reliability and changes in validity of self-reported cardiovascular disease risk factors using dual response: the behavioral risk factor survey. J. Clin. Epidemiol. 1996;49(5):511–517. doi: 10.1016/0895-4356(96)00010-8. May. [DOI] [PubMed] [Google Scholar]
- Brown L., Majumdar S., Newman S., Johnson J. Type 2 diabetes does not increase risk of depression. CMAJ. 2006;175:42–46. doi: 10.1503/cmaj.051429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce D.G., Davis W.A., Starkstein S.E. A prospective study of depression and mortality in patients with type 2 diabetes: the Fremantle Diabetes Study. Diabetologia. 2005;48:2532–2539. doi: 10.1007/s00125-005-0024-3. [DOI] [PubMed] [Google Scholar]
- Chang-Quan H., Bi-Rong D., Zhen-Chan L., Ji-Rong Y., Qing-Xiu L. Chronic diseases and risk for depression in old age: a meta-analysis of published literature. Ageing Res. Rev. 2010;9:131–141. doi: 10.1016/j.arr.2009.05.005. [DOI] [PubMed] [Google Scholar]
- Chen P.C., Chan Y.T., Chen H.F., Ko M.C., Li C.Y. Population-based cohort analyses of the bidirectional relationship between type 2 diabetes and depression. Diabetes Care. 2013;36(2):376–382. doi: 10.2337/dc12-0473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosgrove M.P., Sargeant L.A., Griffin S.J. Does depression increase the risk of developing type 2 diabetes? Occup. Med. (Lond.) 2008;58:7–14. doi: 10.1093/occmed/kqm105. [DOI] [PubMed] [Google Scholar]
- de Jonge P., Roy J.F., Saz P., Marcos G., Lobo A. Prevalent and incident depression in community-dwelling elderly persons with diabetes mellitus: results from the ZARADEMP project. Diabetologia. 2006;49:2627–2633. doi: 10.1007/s00125-006-0442-x. [DOI] [PubMed] [Google Scholar]
- Egede L.E., Zheng D., Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25:464–470. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- Egger M., Davey S.G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engum A. The role of depression and anxiety in onset of diabetes in a large population-based study. J. Psychiatr. Res. 2007;62:31–38. doi: 10.1016/j.jpsychores.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Finkelstein A., Bray W., Chen H. Prevalence and costs of major depression among elderly claimants with diabetes. Diabetes Care. 2003;26:415–420. doi: 10.2337/diacare.26.2.415. [DOI] [PubMed] [Google Scholar]
- Garcia M.E., Lee A., Neuhaus J. Diabetes mellitus as a risk factor for development of depressive symptoms in a population-based cohort of older Mexican Americans. J. Am. Geriatr. Soc. 2016;64:619–624. doi: 10.1111/jgs.14019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardio metabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2:634–647. doi: 10.1016/S2213-8587(14)70102-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden S.H., Lazo M., Carnethon M. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299:2751–2759. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer M., Batty G.D., Kivimaki M. Haemoglobin A1c, fasting glucose and future risk of elevated depressive symptoms over 2 years of follow-up in the English longitudinal study of ageing. Psychol. Med. 2011;41:1889–1896. doi: 10.1017/S0033291711000079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan S.S., Alexandra M.C., Kaeleen D., Abdullah A.M., Therese K. Diabetes mellitus and the risk of depressive and anxiety disorders in Australian women: a longitudinal study. J. Women's Health. 2015;24:889–898. doi: 10.1089/jwh.2015.5210. [DOI] [PubMed] [Google Scholar]
- Hasan S.S., Clavarino A.M., Mamun A.A., Doi S.A.R., Kairuz T. Population impact of depression either as a risk factor or consequence of type 2 diabetes in adults: a meta-analysis of longitudinal studies. Asian J. Psychiatr. 2013;6:460–472. doi: 10.1016/j.ajp.2013.09.008. [DOI] [PubMed] [Google Scholar]
- Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta analyses. Br. Med. J. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt I.G.R., de Groot M., Golden H.S. Diabetes and depression. Curr. Diab. Rep. 2014;14(6) doi: 10.1007/s11892-014-0491-3. (491:1–17) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ian C., Kiyuri N., Yiye Z. Predictors of long-term prognosis of depression. CMAJ. 2011;183(17) doi: 10.1503/cmaj.110676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Icks A., Albers B., Haastert B. Risk for high depressive symptoms in diagnosed and previously undetected diabetes: 5-year follow-up results of the Heinz Nixdorf recall study. PLoS One. 2013;8(2) doi: 10.1371/journal.pone.0056300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Diabetes Federation . International Diabetes Federation; 2005. Global Guideline for Type 2 Diabetes.www.idf.org/Global_guideline Available from. (accessed 25 July 2018) [Google Scholar]
- International Diabetes Federation Diabetes Atlas. 2013. http://www.idf.org/diabetesatlas (accessed 12 October 2017)
- Katon W.J., Rutter C., Simon G. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28:2668–2672. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- Kim J., Stewart R., Kim S. Vascular risk factors and incident late-life depression in a Korean population. Br. J. Psychiatry. 2006;189:26–30. doi: 10.1192/bjp.bp.105.015032. [DOI] [PubMed] [Google Scholar]
- Knol M.J., Twisk J.W., Beekman A.T. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49:837–845. doi: 10.1007/s00125-006-0159-x. [DOI] [PubMed] [Google Scholar]
- Li M., D'Arcy C., Meng X. 2016. Maltreatment in Childhood Substantially Increases the Risk of Adult Depression and Anxiety in Prospective Cohort Studies: Systematic Review, Meta-analysis, and Proportional Attributable Fractions. [DOI] [PubMed] [Google Scholar]
- Luijendijk H.J., Stricker B.H., Hofman A., Witteman J.C.M., Tiemeier H. Cerebrovascular risk factors and incident depression in community-dwelling elderly. Acta Psychiatr. Scand. 2008;118:139–148. doi: 10.1111/j.1600-0447.2008.01189.x. [DOI] [PubMed] [Google Scholar]
- Maraldi C., Volpato S., Penninx B. Diabetes mellitus, glycemic control, and incident depressive symptoms among 70- to 79-year-old persons: the health, aging and body composition study. Arch. Intern. Med. 2007;167:1137–1144. doi: 10.1001/archinte.167.11.1137. [DOI] [PubMed] [Google Scholar]
- Meng X., D'Arcy C. The projected effect of increasing physical activity on reducing the prevalence of common mental disorders among Canadian men and women: a national population-based community study. Prev. Med. 2013;56:59–63. doi: 10.1016/j.ypmed.2012.11.014. [DOI] [PubMed] [Google Scholar]
- Meng X., D'Arcy C. The projected effect of risk factor reduction on major depression incidence: a 16-year longitudinal Canadian Cohort of the National Population Health Survey. J. Affect. Disord. 2014;158:56–61. doi: 10.1016/j.jad.2014.02.007. [DOI] [PubMed] [Google Scholar]
- Mezuk B., Eaton W.W., Albrecht S. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31:2383–2390. doi: 10.2337/dc08-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miquel R., Mauro G.-T., Javier G.-C. Clinical differences between early and late remission in depressive patients. J. Affect. Disord. 2011;134:235–241. doi: 10.1016/j.jad.2011.05.051. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- Moulton D.C., Pickup C.J., Khalida I. The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol. 2015;3:461–471. doi: 10.1016/S2213-8587(15)00134-5. [DOI] [PubMed] [Google Scholar]
- Moussavi S., Chatterji S., Verdes E. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;379:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- Myrna M.W., Obianuju O.B., Virginia W. A 30-year study of 3 generations at high risk and low risk for depression. JAMA Psychiat. 2016;73(9):970–977. doi: 10.1001/jamapsychiatry.2016.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence . National Institute for Health and Clinical Excellence; 2009. Depression: Management of Depression in Primary Care and Secondary Care.http://guidance.nice.org.uk/CG23 Available from. (accessed 25 July 2018) [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4 ∗ 4 million participants. Lancet. 2016;387(10027):1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northridge M.E. Annotation: public health methods-attributable risk as a link between causality and public health action. Am. J. Public Health. 1995;85:1202–1203. doi: 10.2105/ajph.85.9.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nouwen K.A., Winkley J., Twisk C.E.J. Type 2 diabetes mellitus as a risk factor for the onset of depression: a systematic review and meta-analysis. Diabetologia. 2010;53:2480–2486. doi: 10.1007/s00125-010-1874-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor P.J., Crain A.L., Rush W.A. Does diabetes double the risk of depression? Ann of. Fam. Med. 2009;7:328–335. doi: 10.1370/afm.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden C.L.C.M., Kit B.K., Flegal K.M. 2013. Prevalence of Obesity among Adults: United States, 2011–2012. (National Center for Health Statistics NCHS data brief) [PubMed] [Google Scholar]
- Palinkas L.A., Lee P.P., Barrett-Connor E. A prospective study of type 2 diabetes and depressive symptoms in the elderly: the Rancho Bernardo Study. Diabet. Med. 2004;21:1185–1191. doi: 10.1111/j.1464-5491.2004.01315.x. [DOI] [PubMed] [Google Scholar]
- Pan A., Lucas M., Sun Q. Bidirectional association between depression and type 2 diabetes in women. Arch. Intern. Med. 2010;170(21):1884–1891. doi: 10.1001/archinternmed.2010.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polsky D., Doshi J., Marcus S. Long-term risk for depressive symptoms after a medical diagnosis. Arch. Intern. Med. 2005;165:1260–1266. doi: 10.1001/archinte.165.11.1260. [DOI] [PubMed] [Google Scholar]
- Rawana J.S., Morgan A.S., Nguyen H. The relation between eating- and weight-related disturbances and depression in adolescence: a review. Clin. Child. Fam. Psychol. Rev. 2010;13:213–230. doi: 10.1007/s10567-010-0072-1. [DOI] [PubMed] [Google Scholar]
- Rockhill B., Newman B., Weinberg C. Use and misuse of population attributable fractions. Am. J. Public Health. 1998;88:15–19. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotella F., Mannucci E. Diabetes mellitus as a risk factor for depression. A meta-analysis of longitudinal studies. Diabetes Res. Clin. Pract. 2013;99:98–104. doi: 10.1016/j.diabres.2012.11.022. [DOI] [PubMed] [Google Scholar]
- Roy T., Lloyd C.E. Epidemiology of depression and diabetes: a systematic review. J. Affect. Disord. 2012;142S1:S8–S21. doi: 10.1016/S0165-0327(12)70004-6. [DOI] [PubMed] [Google Scholar]
- Sareen J., Belik S.L., Afifi TO Canadian military personnel's population attributable fractions of mental disorders and mental health service use associated with combat and peacekeeping operations. Am. J. Public Health. 2008;98:2191–2198. doi: 10.2105/AJPH.2008.134205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seuring T., Archangelidi O., Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. PharmacoEconomics. 2015;33:811–831. doi: 10.1007/s40273-015-0268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup D., Berlin J., Morton S. The Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Syed S.H., Abdullah A.M., Alexandra M.C. Incidence and risk of depression associated with diabetes in adults: evidence from longitudinal studies. Community Ment. Health J. 2015;51:204–210. doi: 10.1007/s10597-014-9744-5. [DOI] [PubMed] [Google Scholar]
- Tong A., Wang X., Li F. Risk of depressive symptoms associated with impaired glucose metabolism, newly diagnosed diabetes, and previously diagnosed diabetes: a meta-analysis of prospective cohort studies. Acta Diabetol. 2016;53(4):589–598. doi: 10.1007/s00592-016-0845-1. [DOI] [PubMed] [Google Scholar]
- van der Veen D.C., van Zelst W.H., Schoevers R.A. Comorbid anxiety disorders in late-life depression: results of a cohort study. Int. Psychogeriatr. 2015;27:1157. doi: 10.1017/S1041610214002312. [DOI] [PubMed] [Google Scholar]
- Vancampfort D., Mitchell A.J., De Hert M. Type 2 diabetes in patients with major depressive disorder: a meta-analysis of prevalence estimates and predictors. Depress. Anxiety. 2015;32(10):763–773. doi: 10.1002/da.22387. [DOI] [PubMed] [Google Scholar]
- Wells G., Shea B., O'Connell D. Ottawa Hospital Research Institute; 2012. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-analyses.http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed 15 July 2018) [Google Scholar]
- WHO . World Health Organization; Geneva: 1992. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. [Google Scholar]
- WHO . World Health Organization; 2012. Depression: Fact sheet.www.who.int/mediacentre/factsheets/fs369/en/ (Accessed 10 September 2017) [Google Scholar]
- WHO. Promoting Mental Health . World Health Organization; Geneva: 2004. Concepts, Emerging Evidence, Practice (Summary Report) [Google Scholar]
- Yu M., Zhang X., Lu F., Fang L. Depression and risk for diabetes: a meta-analysis. Can. J. Diabetes. 2015;39(4):266–272. doi: 10.1016/j.jcjd.2014.11.006. [DOI] [PubMed] [Google Scholar]
- Zhuang Q.S., Shen L., Ji H.F. Quantitative assessment of the bidirectional relationships between diabetes and depression. Oncotarget. 2017;8(14):23389–23400. doi: 10.18632/oncotarget.15051. [DOI] [PMC free article] [PubMed] [Google Scholar]