Abstract
Purpose
We examined quitting behaviors among a cohort of dual users (cigarettes and electronic cigarettes [e-cigarettes]) and exclusive cigarette smokers for: (1) cigarette smoking reduction, (2) quit attempts, (3) abstinence from cigarettes, and (4) abstinence from all tobacco products.
Methods
Participants enrolled in the Tobacco User Adult Cohort and categorized as “daily” user of cigarettes and “daily” or “some days per week” use of e-cigarettes (ie, dual users; n = 88) or “daily” user of cigarettes only (ie, cigarette smokers; n = 617) served as the analytic sample. Participants were interviewed face to face every 6 months, through 18 months. Data on self-reported current product(s) used, cessation interest, quit attempts and abstinence from cigarettes, and all tobacco products were collected.
Results
No difference in reduction of cigarette consumption over time was noted between groups. Rates of reporting an attempt to quit all tobacco products (≥ 24 hours of not using any tobacco in an attempt to quit) also did not differ by group. Compared to cigarette smokers, dual users were more likely to report abstinence from cigarettes at 6 months (OR = 2.54, p = .045) but not at 12 or 18 months. There was no significant difference in abstinence from all tobacco products by group at 6, 12, or 18 months.
Conclusions
Although dual use of e-cigarettes has been cited as a potential cessation tool for cigarette smokers, our findings indicated that this association was only observed in the short term. We also found no evidence of any association between dual use and eventual abstinence from all tobacco products.
Implications
Our study observed that, in the natural environment, dual users of cigarettes and e-cigarettes were more likely than cigarette smokers to quit cigarettes in the short term but no more likely to quit using cigarettes and all tobacco products over time.
Introduction
The use of electronic cigarettes (e-cigarettes) has increased dramatically since their introduction in the US market a decade ago1,2 and the implications of this trend for public health remains a source of controversy. E-cigarettes have lower levels of tobacco-derived components known to be harmful to health compared to combustible cigarettes,3–5 which has led some public health policy makers, most notably in the United Kingdom, to advocate for their use as a harm reduction strategy.6–8 Conversely, many view e-cigarettes as a threat to public health due to their adverse health effects,9 and potential contribution to nicotine addiction among youth.5,9,10
Dual use of e-cigarettes and combustible cigarettes is common; 37.8% of all smokers in the United States use more than one tobacco product, with e-cigarettes and cigarettes the most common combination of products used together.11 E-cigarettes may help smokers reduce their use of combustible cigarettes or facilitate achieving abstinence from tobacco products. Alternatively, they might actually inhibit smokers from quitting altogether by providing a more socially acceptable alternative to maintaining their nicotine addiction in selected settings, as well as a means to circumvent smoke-free or tobacco-free regulations.
Several studies have evaluated the role of e-cigarettes in smoking cessation with varying conclusions. A recent meta-analysis of cohort, cross-sectional, and randomized controlled trial data found that dual users of cigarettes and e-cigarettes were 28% less likely to quit smoking cigarettes compared to smokers who did not also use e-cigarettes.12 However, another large systematic review independently reached a different conclusion, finding “low-grade” evidence, primarily from randomized controlled trials, that e-cigarettes may help with smoking cessation.13 A prospective examination of population-level data from the Current Population Survey–Tobacco Use Supplement also found an association between e-cigarette use and increased rates of quitting.14 This analysis concluded that dual users were more likely to achieve smoking cessation compared to exclusive cigarette smokers and suggested the increase in the rate of smoking cessation among US smokers between 2010 and 2015 (4.5%–5.6%) was due to the increasing use of e-cigarettes in the population.14
In this article, we extend this research and report findings that compared dual users of cigarettes and e-cigarettes with cigarette smokers in the natural environment and that were enrolled in a longitudinal cohort study of urban and rural tobacco users. Using data collected at baseline, 6, 12, and 18 months, we assessed cigarette reduction, quit attempts, and abstinence rates over time. We examined four related research questions: (1) Are dual users more likely than cigarette smokers to reduce their consumption of combustible cigarettes over time? (2) Do dual users make more tobacco product(s) quit attempts compared to cigarette smokers over time? (3) Are dual users more likely to achieve complete abstinence from cigarettes compared to cigarette smokers over time? (4) Are dual users more likely to achieve complete abstinence from all tobacco products (including e-cigarettes) compared to cigarette smokers over time?
Methods
Design
The Tobacco User Adult Cohort (TUAC), initiated in 2014, is an observational, longitudinal study of a prospective cohort of Ohio rural and urban adults (≥18 years) who reported tobacco use at enrollment and has been described elsewhere.15 For this analysis, we included those who reported, at baseline (1) daily exclusive cigarette smoking (hereafter referred to as cigarette smokers), or (2) dual use of daily cigarettes and every day or some days per week use of e-cigarettes (hereafter referred to as dual users). This analytic sample consisted of 617 cigarette smokers and 88 dual users. Urban participants were from Franklin County, Ohio, a large metropolitan county (population 1 836 500)16 that includes Columbus, Ohio. Smoking prevalence in Franklin County was estimated to be 19.8% in 2015.17 Rural participants were from six counties in Appalachian Ohio (Brown, Guernsey, Lawrence, Muskingum, Scioto, and Washington). These counties were chosen because of their high prevalence of smoking (27%–35%), largely rural population (42%–79%), and preexisting research infrastructure. The Appalachian region of Ohio includes 2 million residents (17.6% of the state population) and is characterized by higher rates of poverty and unemployment compared to the state as a whole.18 Approximately 92% of residents in Appalachian Ohio are white.18 Prevalence of smoking in this region is higher than that in non-Appalachian counties (27.4%, compared to 21.6% in non-Appalachian counties).17
All cohort participants were identified using an address-based sampling method.19 A total of 180 075 home addresses (90 312 households in Appalachian counties and 89 763 households in Franklin County) were mailed an introductory packet that explained the study as a university-sponsored health project. The packet included a brief screening questionnaire that asked households to enumerate those living at the address and respond to questions about behaviors including diet, exercise, and tobacco use. Intentionally, the packet did not disclose that tobacco use behaviors were the focus of the study. Households were instructed to complete the questionnaire and return in a preaddressed stamped envelope. A $2 bill was included in the packet. Households that did not respond to the initial mailing after 3 weeks were mailed a second packet, without the $2 incentive. The overall response rate to the mailed screening questionnaire was 21.6% (urban = 20.8%, rural = 22.4%).15 Fifty-seven percent of households contacted to participate in the study were reached (urban = 65%, rural = 51%).15 Among those eligible participants contacted and invited to enroll in the cohort, the cooperation (ie, enrollment) rate was 95% for urban and 89% for rural participants.15
Procedure for Data Collection
Cohort enrollment occurred between October 2014 and December 2015, with all participants completing 18-month data collection by June 2017. In-person interviews were conducted by a trained field interviewer either in the participant’s home or in a public setting such as a restaurant or library, according to participant preference. The baseline interview lasted about 60–90 minutes, with follow-up interviews taking approximately 30–45 minutes. Ninety-three percent of participants who were interviewed at baseline completed all four interviews, with no difference in retention by urban or rural region. After each interview, participants received a $50 gift card. Participant survey responses were recorded electronically in the field using an encrypted laptop and synchronized to a centralized database that was accessible to investigators for analysis. This study was approved by the Ohio State University Institutional Review Board.
Eligibility Criteria
Respondents were eligible to participate in the parent TUAC study if they met the following criteria: (1) age at least 18 years; (2) resident of one of the six participating rural counties or Franklin County; (3) responded as “daily” or “some days/week” use of combustible tobacco, smokeless tobacco, e-cigarettes, or dual use of two or more products; and (4) consented to participate in the research study. Only one adult per household was included in the study. If a household had more than one eligible adult, one participant was randomly selected. In this article, we analyzed the subset of the parent cohort who responded as (1) daily cigarette smoking (cigarette smokers), or (2) daily cigarette smoking and either daily or some days per week use of e-cigarettes (dual users) at the time of their baseline interview.
Measures
Demographic data collected included age, gender, race, household income, employment status, marital status, and highest level of education. Data collected on smoking behavior for current cigarette smokers included frequency of use (average number of cigarettes smoked per day). Data collected on e-cigarette use behavior for current e-cigarette users included nicotine concentration, brand and flavor of e-liquid used, and device type (disposable, cartridge, tank, multiple). All participants were asked about previous tobacco use quit attempts; at baseline this was assessed over the past year; at each follow-up, participants were asked to report whether they had made one or more attempts to quit tobacco (yes/no) since the last interview (ie, past 6 months).
Current cigarette use was defined as lifetime use of at least 100 cigarettes and currently smoking daily at baseline. Current e-cigarette use was defined as currently using e-cigarettes daily or some days per week at baseline. A quit attempt was defined as 24 or more hours of not using any tobacco in an attempt to quit all tobacco products.20 Abstinence from cigarettes was defined either as (1) self-reported not smoking cigarettes since last interview or (2) if smoked since last interview, the response of “not at all” to the question “do you now smoke cigarettes every day, some days/week, occasionally, rarely or not at all?”21 Point prevalence abstinence from all tobacco products was defined as no use of any tobacco products, including e-cigarettes, in the past 7 days.21
Nicotine dependence was assessed using the Fagerström Test of Nicotine Dependence22 and the Heaviness of Smoking Index.22 Readiness to quit smoking was evaluated using the stages of change construct from the transtheoretical model.23 We also assessed cessation interest, characterized on a scale from 1 to 10 (1 = low).24 Finally, we evaluated perceptions about the health risks associated with smoking by measuring absolute risk perception (ie, belief about the risk of smoking), comparative risk perception (ie, belief about one’s own risk of smoking compared to a nonsmoker), and feeling at risk (ie, subjective perception of dying early from smoking).25,26
Data Analysis
Differences between cigarette smokers and dual users were evaluated with chi-square tests, t tests, or Wilcoxon rank sum tests, as appropriate. Linear and logistic regression models were fit for the change in number of cigarettes smoked per day from baseline (Δ = number of cigarettes smoked at follow-up − the number of cigarettes smoked at baseline) and abstinence from cigarettes and abstinence from all tobacco. These models were fit at each follow-up time point (6, 12, and 18 months). Baseline tobacco user group and cessation interest were included as covariates in all models in addition to significant sociodemographic characteristics. All analyses were conducted with SAS 9.4 (SAS Institute Inc, Cary, NC).
Results
Sample Characteristics
Participants’ baseline characteristics, stratified on their tobacco user group (ie, cigarette smoker or dual user), are given in Table 1. There were few differences in demographic characteristics between the groups, with the exception of self-reported race, where a greater proportion of dual users were white. There were no significant differences in the relative proportions of dual users and cigarette smokers across the three stages of change. Conversely, dual users reported significantly higher cessation interest compared to cigarette smokers. Dual users did not differ from cigarette smokers with regard to their level of nicotine dependence. There were no group differences in perceptions about the risks of smoking cigarettes (data not shown).
Table 1.
Characteristics of Cigarette Smokers (n = 617) and Dual Users (n = 88) at Baseline
| Cigarette smokers | Dual users | p valuea | |||
|---|---|---|---|---|---|
| Age (mean, SD) | 50.5 | 14.0 | 49.3 | 14.6 | .446b |
| N | % | N | % | ||
| Sex | .231 | ||||
| Male | 266 | 43.1 | 32 | 36.4 | |
| Female | 351 | 56.9 | 56 | 63.6 | |
| Race | .027 | ||||
| White | 501 | 81.3 | 80 | 90.9 | |
| Other | 115 | 18.7 | 8 | 9.1 | |
| Education | .242 | ||||
| Less than high school | 91 | 14.8 | 9 | 10.2 | |
| GED/high school | 204 | 33.1 | 25 | 28.4 | |
| At least Some college | 322 | 52.2 | 54 | 61.4 | |
| Household income | .229 | ||||
| Less than $25 000 | 251 | 43.0 | 38 | 45.2 | |
| $25 000–$50 000 | 196 | 33.6 | 21 | 25.0 | |
| More than $50 000 | 137 | 23.5 | 25 | 29.8 | |
| Marital status | .235 | ||||
| Single/never married | 195 | 31.6 | 23 | 26.1 | |
| Married/cohabitating | 230 | 37.3 | 37 | 42.1 | |
| Separated/divorced | 146 | 23.7 | 17 | 19.3 | |
| Widowed | 46 | 7.5 | 11 | 12.5 | |
| Employment status | .237 | ||||
| Full-time | 241 | 39.2 | 27 | 30.7 | |
| Part-time | 82 | 13.3 | 11 | 12.5 | |
| Unemployed | 292 | 47.5 | 50 | 56.8 | |
| Region | |||||
| Rural | 313 | 50.7 | 37 | 42.1 | |
| Urban | 304 | 49.3 | 51 | 58.0 | |
| Stage of change | .324 | ||||
| Precontemplation | 307 | 57.9 | 37 | 50.0 | |
| Contemplation | 191 | 36.0 | 30 | 40.5 | |
| Preparation | 32 | 6.0 | 7 | 9.5 | |
| FTND score | .639 | ||||
| Low/moderate | 264 | 48.2 | 42 | 53.8 | |
| Moderate/high | 284 | 51.8 | 36 | 46.2 | |
| mean | SD | mean | SD | ||
| Cessation interest | 6.3 | 3.0 | 7.4 | 2.5 | .002c |
GED = General Education Development, FTND = Fagerström Test for Nicotine Dependence, SD = standard deviation.
aChi-square test unless otherwise noted.
b t test.
cWilcoxon rank sum test.
Among dual users reporting a regular brand of e-cigarettes, the majority (59%) reported that they used flavored e-cigarettes as opposed to an unflavored or tobacco-flavored product and most used either cartridge (42%) or tank (41%) devices. Approximately 25% of dual users reported that they did not know if their e-cigarettes contained nicotine. For those who knew the nicotine content (n = 64), 95% reported their e-liquid contained nicotine.
Smoking Reduction
Regression models for the change in number of cigarettes smoked per day were fit from data collected at each follow-up interview. Approximately 6% of the sample reported nondaily smoking at each follow-up; as cigarettes smoked per day could not be calculated, these participants were coded as zero cigarettes smoked per day. The percentage of nondaily smokers did not differ between cigarette smokers and dual users. Gender was significant in the models predicting change from baseline at 12 and 18 months. At 12 months, men reduced their cigarette consumption from baseline by an average of 4 cigarettes/day whereas women reduced their cigarette consumption by an average of 3 cigarettes/day. Similarly at 18 months, men reduced by 5 cigarettes/day whereas women reduced by 3 cigarettes/day. Age and education were significant in the model for change at 18 months whereas region, race, income, marital status, employment status, and type of e-cigarette device were not significant in any of the models. Participants who received a General Education Development (GED) or high school education reduced their cigarette consumption by an average 5 cigarettes/day from baseline whereas participants who had less than a high school education or at least some college reduced by an average of 3 cigarettes/day. Further, older participants were more likely to decrease their cigarette consumption; for each year increase in age, the number of cigarettes smoked per day decreased by 0.06. No statistically significant differences in change in number of cigarettes smoked at any of the three time points were noted, implying that dual users and cigarette smokers did not reduce their cigarette consumption at different rates (Table 2).
Table 2.
Linear Regression Models for Change in the Number of Cigarettes Smoked per Day at 6, 12, and 18 Months With Baseline Group and Cessation Interest Included in All Models; Adjusted for Significant Sociodemographic Covariates
| 6 mo | 12 mo | 18 mo | ||||
|---|---|---|---|---|---|---|
| Change (95% CI) | p value | Change (95% CI) | p value | Change (95% CI) | p value | |
| Baseline group | .148a | .313a | .283a | |||
| Cigarette smoker | −2.07 (−2.71% to −1.43%) | −2.78 (−3.43% to −2.12%) | −3.07 (−3.90% to −2.24%) | |||
| Dual user | −3.41 (−5.11% to −1.71%) | −3.75 (−5.53% to −1.97%) | −4.21 (−6.22% to −2.20%) | |||
| Cessation interest (slope) | −0.06 (−0.26% to 0.14%) | .554 | −0.21 (−0.41% to 0.00%) | .0497 | −0.12 (−0.35% to 0.11%) | .310 |
| Gender | .025a | .018a | ||||
| Male | — | −3.97 (−5.17 to −2.77%) | −4.48 (−5.86% to −3.09%) | |||
| Female | — | −2.56 (−3.63 to −1.49%) | −2.81 (−4.07% to −1.55%) | |||
| Age (slope) | — | — | −0.06 (−0.11% to −0.01%) | .019a | ||
| Education | .019a | |||||
| Less than high school | — | — | −2.85 (−4.88% to −0.81%) | |||
| GED/high school | — | — | −5.05 (−6.48% to −3.63%) | |||
| At least some college | — | — | −3.03 (−4.24% to −1.82%) | |||
CI = confidence interval, GED = General Education Development.
a p value for comparison between groups.
Quit Attempts
To compare quit attempts among dual users and cigarette smokers over time, logistic regression models were fit including tobacco user group at baseline and cessation interest. Race was significant in all models whereas age, household income, and region were only significant in the model for quit attempts at 18 months. Gender, education, marital status, employment status, and type of e-cigarette device were not significant in any of the models. In these models, dual users were no more likely than cigarette smokers to make one or more attempt to quit using all tobacco products at any time interval (data not shown).
Abstinence From Cigarettes and All Tobacco Products
Logistic regression models assessed how dual users’ odds of quitting cigarettes and achieving abstinence from all tobacco products (including e-cigarettes) compared to cigarette smokers after adjustment for cessation interest (Table 3). Age, gender, race, education, household income, marital status, employment status, region, and type of e-cigarette device were not significant in the models. In the models assessing the odds of quitting cigarettes, dual users had greater odds of quitting cigarettes compared to cigarette smokers after 6 months (OR = 2.54, 95% CI = 1.02% to 6.31%); dual users did not have greater odds of quitting cigarettes at 12 or 18 months. In models assessing the odds of abstaining from all tobacco products, dual users did not have greater odds of achieving abstinence from all tobacco products compared to cigarette smokers at any time point.
Table 3.
Adjusted Odds Ratios for Abstinence From Cigarettes and All Tobacco Products From Logistic Regression Models at 6, 12, and 18 Months With Baseline Group and Cessation Interest Included in All Models
| Abstinence from cigarettes | ||||||
|---|---|---|---|---|---|---|
| 6 mo | 12 mo | 18 mo | ||||
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| Baseline group | .045a | .188a | .091a | |||
| Cigarette smoker | Reference | Reference | Reference | |||
| Dual user | 2.54 (1.02% to 6.31%) | 1.73 (0.77% to 3.92%) | 1.81 (0.91% to 3.61%) | |||
| Cessation interest (for unit change) |
1.07 (0.93% to 1.24%) | .355 | 1.10 (0.98% to 1.23%) | .121 | 1.10 (0.999% to 1.22%) | .052 |
| Abstinence from all tobacco | ||||||
| 6 mo | 12 mo | 18 mo | ||||
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| Baseline group | .402a | .841a | .909a | |||
| Cigarette smoker | Reference | Reference | Reference | |||
| Dual user | 0.42 (0.05% to 3.23%) | 1.12 (0.37% to 3.35%) | 0.94 (0.36% to 2.51%) | |||
| Cessation interest (for unit change) |
1.20 (0.97% to 1.47%) | .088 | 1.22 (1.04% to 1.43%) | .016 | 1.14 (1.003% to 1.28%) | .044 |
CI = confidence interval, OR = odds ratio.
a p value for comparison between groups.
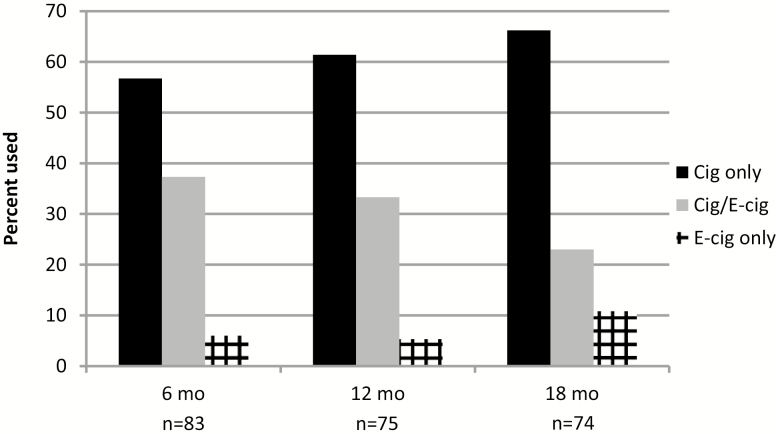
For baseline dual users who continued to use tobacco products every day or some days per week at follow-up interviews, the majority (57%–66%) transitioned to exclusive cigarette product use. Fewer remained dual users (21%–36%) and 6%–10% were categorized as exclusive e-cigarette users (see Figure 1).
Figure 1.
Product(s) used every day/some days per week at 6, 12, and 18 months among those reporting dual use (Cig/E-cig) at baseline. Cig = cigarette, E-cig = electronic cigarette.
Discussion
This study tracks a cohort of adult tobacco users longitudinally, providing valuable insight into how individuals change their tobacco use behavior over time in the natural environment. Gaining a better understanding of factors that may facilitate or inhibit quitting cigarettes is of vital importance to public health. The Centers for Disease Control and Prevention estimate that one in five deaths in the United States are caused by smoking and the life expectancy of smokers is as least 10 years shorter than that of nonsmokers.27 Consequently, even small increases in smoking cessation rates across the population would result in significant reductions in mortality from tobacco-related illness.
This 2014–2017 study provided an opportunity to examine dual users of e-cigarettes and cigarettes and evaluate how dual use is associated with cessation. Our analysis suggests that dual users, compared to cigarette smokers, were more likely to quit using cigarettes in the short term but were no different from cigarette smokers at 12 or 18 months. In addition, dual users were no more likely than cigarette smokers to quit using tobacco products altogether at any of the follow-up time points. Although dual users reported a significantly higher interest in cessation at baseline and had greater odds of quitting at 6 months, long-term abstinence resembled exclusive cigarette smokers over time. Our cigarette cessation rate among dual users was roughly similar to rates of quitting smoking documented in randomized controlled trials. We observed an unadjusted cessation rate of 8.1% among dual users over 6 months, whereas a randomized controlled trial of smokers using an e-cigarette for cessation reported a cessation rate of 7.3% over 6 months.28 Similarly, our unadjusted quit rate among dual users after 12 months (10.1%) was roughly comparable to the 12-month cessation rate observed in a second randomized controlled trial of smokers not interested in quitting who were given e-cigarettes (8.7%).29
There are several possible hypotheses that may explain the observed association between e-cigarette use and combustible cigarette cessation at 6 months. First, it is possible that e-cigarettes directly facilitate cigarette cessation in the short term. Nicotine delivery via an e-cigarette may moderate symptoms of nicotine withdrawal (eg, craving) making it easier for smokers to avoid relapse. Several smoking cessation modalities that have been shown to be effective, including the nicotine replacement patch, inhaler, gum, and lozenges, involve the replacement of nicotine and work in this manner.30 Second, e-cigarettes may have an additional advantage as they mimic smoking behavior. Studies demonstrate that psychological factors are important components of tobacco use dependency.31,32 Smokers become conditioned to using cigarettes at certain times and in response to various social and emotional triggers.32 E-cigarettes may offer an effective alternative to cigarette smoking when an event triggers an urge to smoke. However, the use of an e-cigarette may only influence cigarette abstinence in the short term. Over time, the typical phenomenon of short-term abstinence followed by relapse to cigarette smoking may occur.33
Importantly, therapeutic cessation aids have been shown to help smokers transition to complete abstinence.33 In our analysis, e-cigarettes were not associated with total abstinence from tobacco products over time. E-cigarettes may carry more addictive potential than therapeutic nicotine replacement aids. This could explain why many dual users in our study continued to use tobacco products even after they had quit cigarettes in the short term. Alternatively, over time dual users may become accustomed to using e-cigarettes in selected settings where social norms influence product preferences. Future research that examines motivations for continued use of e-cigarettes will be required to better understand dual use behaviors.
Dual users did not reduce the number of cigarettes smoked over the course of the study. This finding is consistent with a randomized controlled trial in which the initiation of an e-cigarette lead to an initial decline in combustible cigarette consumption, but combustible cigarette use remained relatively constant or gradually increased after that.29 Because the dual users in our cohort were already using e-cigarettes at the beginning of the study, we cannot say definitively whether they reduced their use of combustible cigarettes after e-cigarette initiation or if this group smoked fewer cigarettes in general.
This study did not evaluate short- or long-term health outcomes and any conclusions regarding the net effect of e-cigarettes on health are only speculative. Serious concerns have been raised about the potential long-term health outcomes of e-cigarette use, with some studies indicating harms of certain e-liquid components and flavorings34,35 and health risks associated with exposure to ultrafine particles in e-liquid vapor.9 Nevertheless, most available evidence suggests that smoking cigarettes is more harmful to health than using e-cigarettes.5,36 However, there is no available evidence whether or not long-term e-cigarette use among dual users influences morbidity and mortality compared to those who exclusively smoke cigarettes.5 Whether or not e-cigarettes have a net positive impact on health for smokers may depend on the reason for using e-cigarettes. If smokers are using e-cigarettes as an alternative to empirically validated cessation modalities in an effort to achieve total cessation, e-cigarettes could have a net negative impact on health by causing the user to maintain their nicotine addiction rather than quitting completely. Conversely, for smokers not interested in quitting tobacco altogether, completely switching to an e-cigarette could have the potential to reduce short-term adverse health outcomes in several organ systems.5 Unfortunately, in our cohort, this transition to exclusive e-cigarette use only occurred for about 6%–10% of dual users whereas the majority transitioned back to exclusive cigarette smoking.
This study highlights the need for more research on the use of e-cigarettes as a smoking cessation aid and tool for harm reduction. Having a better understanding of the modalities that help smokers quit is a matter of urgent public health concern. There is a need for additional large, population-based cohort studies, such as the ongoing Population and Assessment of Tobacco and Health study (PATH),11 examining the relationship between e-cigarettes and smoking behavior as well as randomized controlled trials evaluating the efficacy of e-cigarettes as a cessation aid and directly comparing e-cigarettes to approved cessation treatments. Such research would be of great value to smokers who want to quit and health care professionals who advise smoking patients about the risks and potential benefits of e-cigarette use. Should e-cigarettes demonstrate cessation efficacy, the option of using an e-cigarette could be acceptable to some smokers who are not interested in other methods of cessation, and could be useful as an alternative for smokers who have attempted to quit using other methods and have not been successful.
Unlike studies that have used convenience samples, a strength of this study is its randomly selected sample more likely to be representative of the population of tobacco users in Ohio. Although low-income, unemployed, and women were overrepresented, cohort members resembled tobacco users’ income and employment status throughout these Ohio regions.17,18 As such, the generalizability of this study may be restricted to this region of the United States. It should also be noted that the initial overall response rate to the household screening questionnaire did not differ by region. However, urban residents were more likely to be reached with an invitation to participate, and subsequently enrolled in the cohort.
Study participants were followed over an 18 month time period. Few other studies of e-cigarette use have followed research participants in the natural environment for this length of time. Furthermore, the study had a high rate of retention, with 93% of participants completing all four interviews. Retention rates were similar by region.
This study is limited by its reliance on self-reported data, a short point prevalence estimate of abstinence (ie, 7 days), and lack of biochemical measures to validate tobacco use status. It is likely that the self-reported cessation rates overestimate the true rates of cessation. However, because the study was observing smoking behavior over time and not evaluating e-cigarettes as a cessation aid, reporting bias is likely to have been nondifferential. Finally, because we did not observe smokers from the time of initiation of e-cigarettes, we cannot draw definitive conclusions about the relationship between e-cigarettes and cigarette consumption or report the amount of time from e-cigarette initiation to cessation.
In conclusion, our study suggests that dual users of cigarettes and e-cigarettes are more likely than cigarette smokers to quit cigarettes in the short term but no more likely to quit using cigarettes and all tobacco products over time. More research is needed to better understand the safety and efficacy of e-cigarettes as a cessation aid and possible harm reduction tool and to compare e-cigarette use with empirically validated cessation modalities.
Funding
This work was supported by the National Institutes of Health (NIH) and the US Food and Drug Administration (Center for Tobacco Products) (P50 CA180908 and UL1 TR001070). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Declaration of Interests
None declared.
Acknowledgments
The authors acknowledge the field interviewers from Franklin and Ohio Appalachian counties.
References
- 1. King BA, Patel R, Nguyen KH, Dube SR. Trends in awareness and use of electronic cigarettes among US adults, 2010–2013. Nicotine Tob Res. 2015;17(2):219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McMillen RC, Gottlieb MA, Shaefer RM, Winickoff JP, Klein JD. Original investigation trends in electronic cigarette use among U.S. adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;17(10):1195–1202. [DOI] [PubMed] [Google Scholar]
- 3. Bhatnagar A, Whitsel LP, Ribisl KM, et al. ; American Heart Association Advocacy Coordinating Committee, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research. Electronic cigarettes: a policy statement from the American Heart Association. Circulation. 2014;130(16):1418–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hajek P, Etter JF, Benowitz N, Eissenberg T, McRobbie H. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014;109(11):1801–1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stratton K, Kwan LY, Eaton DL, eds. Public Health Consequences of E-Cigarettes. Washington, DC: National Academies Press; 2018. doi: 10.17226/24952 http://nationalacademies.org/hmd/Reports/2018/public-health-consequences-of-e-cigarettes.aspx. Accessed April 1, 2018. [DOI] [PubMed] [Google Scholar]
- 6. Abrams DB. Promise and peril of e-cigarettes: can disruptive technology make cigarettes obsolete?JAMA. 2014;311(2):135–136. [DOI] [PubMed] [Google Scholar]
- 7. Cahn Z, Siegel M. Electronic cigarettes as a harm reduction strategy for tobacco control: a step forward or a repeat of past mistakes?J Public Health Policy. 2011;32(1):16–31. [DOI] [PubMed] [Google Scholar]
- 8. Royal College of Physicians. Nicotine Without Smoke: Tobacco Harm Reduction. 2016. https://www.rcplondon.ac.uk/projects/outputs/nicot. Accessed May 7, 2017. [Google Scholar]
- 9. Glantz SA, Bareham DW. E-cigarettes: use, effects on smoking, risks, and policy implications. Annu Rev Public Health. 2018;39:215–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. US Department of Health and Human Services. E-Cigarette Use Among Youth and Young Adults : A Report of the Surgeon General. 2016. https://e-cigarettes.surgeongeneral.gov/documents/2016_sgr_full_report_non-508.pdf. Accessed May 7, 2017. [Google Scholar]
- 11. Kasza KA, Ambrose BK, Conway KP, et al. . Tobacco-product use by adults and youths in the United States in 2013 and 2014. N Engl J Med. 2017;376(4):342–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4(2):116–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016;9:CD010216 www.cochranelibrary.com. Accessed March 28, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhu SH, Zhuang YL, Wong S, Cummins SE, Tedeschi GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. BMJ. 2017;358:j3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brasky TM, Hinton A, Doogan NJ, et al. . Characteristics of the tobacco user adult cohort in urban and rural Ohio. Tob Regul Sci. 2018;4(1):614–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. US Census Fact finder. American FactFinder – Community Facts. http://factfinder.census.gov. Accessed July 2, 2017.
- 17. Adult Dashboard. Ohio Medicaid Assessment Survey 2015. http://grcapps.osu.edu/dashboards/OMAS/adult/. Accessed July 30, 2017.
- 18. County Trends. Ohio Development Services Agency https://development.ohio.gov/reports/reports_countytrends_map.htm. Accessed July 2, 2017.
- 19. Brick JM, Williams D, Montaquila JM. Address based sampling for subpopulation surveys. Public Opin Q. 2011;75(3):409–428. [Google Scholar]
- 20. Centers for Disease Control and Prevention. Quitting smoking among adults—United States 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(44):1513–1519. https://www.cdc.gov/mmwr/ preview/mmwrhtml/mm6044a2.htm. Accessed January 18, 2018. [PubMed] [Google Scholar]
- 21. Velicer WF, Prochaska JO, Rossi JS, Snow MG. Assessing outcome in smoking cessation studies. Psychol Bull. 1992;111(1):23–41. [DOI] [PubMed] [Google Scholar]
- 22. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. [DOI] [PubMed] [Google Scholar]
- 23. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. [DOI] [PubMed] [Google Scholar]
- 24. Niaura R, Shadel W. Assessment to inform smoking cessation treatment. In: Abrams D, Niaura R, Brown R, Emmons K, Goldstein M, Monti P, eds. The Tobacco Dependence Treatment Handbook. New York: Guildford Press; 2003:27–72. [Google Scholar]
- 25. Dillard AJ, McCaul KD, Klein WM. Unrealistic optimism in smokers: implications for smoking myth endorsement and self-protective motivation. J Health Commun. 2006;11 (suppl 1):93–102. [DOI] [PubMed] [Google Scholar]
- 26. Dillard AJ, Ferrer RA, Ubel PA, Fagerlin A. Risk perception measures’ associations with behavior intentions, affect, and cognition following colon cancer screening messages. Health Psychol. 2012;31(1):106–113. [DOI] [PubMed] [Google Scholar]
- 27. The Centers for Disease Control and Prevention. Tobacco-Related Mortality https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/tobacco_related_mortality/index.htm. Accessed January 1, 2017.
- 28. Bullen C, Howe C, Laugesen M, et al. . Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382(9905):1629–1637. [DOI] [PubMed] [Google Scholar]
- 29. Caponnetto P, Campagna D, Cibella F, et al. . EffiCiency and Safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One. 2013;8(6):e66317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. West R, Shiffman S. Effect of oral nicotine dosing forms on cigarette withdrawal symptoms and craving: a systematic review. Psychopharmacology (Berl). 2001;155(2):115–122. [DOI] [PubMed] [Google Scholar]
- 31. Fagerström KO. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict Behav. 1978;3(3–4):235–241. [DOI] [PubMed] [Google Scholar]
- 32. West R, Schneider N. Craving for cigarettes. Br J Addict. 1987;82(4):407–415. [DOI] [PubMed] [Google Scholar]
- 33. Agency for Healthcare Research and Quality. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: Agency for Healthcare Research and Quality; 2008. https://www.ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/tobacco/index.html. AccessedApril 11, 2018. [Google Scholar]
- 34. Allen JG, Flanigan SS, LeBlanc M, et al. . Flavoring chemicals in e-cigarettes: diacetyl, 2,3-pentanedione, and acetoin in a sample of 51 products, including fruit-, candy-, and cocktail-flavored e-cigarettes. Environ Health Perspect. 2016;124(6):733–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Barrington-Trimis JL, Samet JM, McConnell R. Flavorings in electronic cigarettes: an unrecognized respiratory health hazard?JAMA. 2014;312(23):2493–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zeller M, Hatsukami D; Strategic Dialogue on Tobacco Harm Reduction Group The strategic dialogue on tobacco harm reduction: a vision and blueprint for action in the US. Tob Control. 2009;18(4):324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]