Abstract
Introduction
Within tobacco prevention programming, it is useful to identify youth that are at risk for experimenting with various tobacco products and e-cigarettes. The susceptibility to smoking construct is a simple method to identify never-smoking students that are less committed to remaining smoke-free. However, the predictive validity of this construct has not been tested within the Canadian context or for the use of other tobacco products and e-cigarettes.
Methods
This study used a large, longitudinal sample of secondary school students that reported never using tobacco cigarettes and noncurrent use of alternative tobacco products or e-cigarettes at baseline in Ontario, Canada. The sensitivity, specificity, and positive and negative predictive values of the susceptibility construct for predicting tobacco cigarette, e-cigarette, cigarillo or little cigar, cigar, hookah, and smokeless tobacco use 1 and 2 years after baseline measurement were calculated.
Results
At baseline, 29.4% of the sample was susceptible to future tobacco product or e-cigarette use. The sensitivity of the construct ranged from 43.2% (smokeless tobacco) to 59.5% (tobacco cigarettes), the specificity ranged from 70.9% (smokeless tobacco) to 75.9% (tobacco cigarettes), and the positive predictive value ranged from 2.6% (smokeless tobacco) to 32.2% (tobacco cigarettes). Similar values were calculated for each measure of the susceptibility construct.
Conclusions
A significant number of youth that did not currently use tobacco products or e-cigarettes at baseline reported using tobacco products and e-cigarettes over a 2-year follow-up period. The predictive validity of the susceptibility construct was high and the construct can be used to predict other tobacco product and e-cigarette use among youth.
Implications
This study presents the predictive validity of the susceptibility construct for the use of tobacco cigarettes among secondary school students in Ontario, Canada. It also presents a novel use of the susceptibility construct for predicting the use of e-cigarettes, cigarillos or little cigars, cigars, hookah, and smokeless tobacco among secondary school students in Ontario, Canada.
Introduction
The prevalence of tobacco cigarette smoking has decreased dramatically within Canada since the early 2000s.1 Not only are fewer Canadian youth current smokers,1 but they are also less likely to be exposed to smoking due to strong tobacco control policies (eg, smoke-free spaces) and fewer adult smokers. However, there remains a significant number of youth that continue to experiment with tobacco cigarettes, alternative tobacco products (such as cigarillos, little cigars, and hookah), and e-cigarettes. It is well-known that smoking tobacco products poses significant negative health effects.2–5 Furthermore, nicotine is a very addictive substance6 that can alter adolescent brain development.7,8 Therefore, it would be beneficial to identify youth that are at risk for experimenting with various tobacco products and e-cigarettes in order to provide targeted programming to prevent smoking experimentation and nicotine addiction.
Simple methods that do not require biochemical validation have been developed to identify students that have never smoked tobacco cigarettes who are less committed to remaining smoke-free.9,10 Given that intentions are a strong predictor of performing a behavior,11 it follows that individuals who respond positively to questions about their intentions to start smoking cigarettes in the future and to smoke cigarettes if offered by friends, may be more likely to experiment with tobacco products and e-cigarettes. These never-smoking individuals are identified as susceptible to future smoking using the susceptibility construct.9,10 As described elsewhere, Pierce et al.9,10 use responses to three smoking-related intention measures to determine if a never smoker is classified as “not susceptible to future smoking” or “susceptible to future smoking.” In the domain of tobacco control prevention research, the ability to identify nonsmoking youth who are most likely to become future smokers is a considerable asset for being able to target prevention resources to where they are needed the most.12 Based on their initial study, a strong univariate relationship was found between positive responses to susceptibility questions and experimentation with and established smoking.9 A validation study later identified the sensitivity (62.2%) and the specificity (49.6%) of the susceptibility construct.13
Since its development, the susceptibility construct has been widely used in cross-sectional (eg, refs.14,15) and longitudinal studies (eg, refs.16,17) to identify students susceptible to tobacco cigarette smoking. These studies have used the complete construct as well as variations that only include one or two questions from the construct to identify students susceptible to future tobacco cigarette smoking. However, given the significant changes that have occurred over the last 20 years to the tobacco control landscape via the implementation of prevention and cessation programs and policies and the expansion of the tobacco market to include other tobacco products and e-cigarettes, it is unknown whether the susceptibility construct is still valid for predicting the onset of tobacco cigarette smoking. Furthermore, the susceptibility construct has not been tested within the Canadian context where differences in policies for tobacco advertising, access, and taxation may affect the validity of using this construct. Given the variations in the number of questions used to assess susceptibility across studies, it would also be helpful to identify whether the full construct is needed or whether a single question performs adequately.
The susceptibility measures presented by Pierce et al.9,10 have been extensively used to identify future tobacco cigarette smokers. More recently, some studies have modified these measures to identify students susceptible to e-cigarettes18–20; cigars, cigarillos, or little cigars21; and smokeless tobacco.21,22 However, with the exception of one study,20 these studies have used a cross-sectional design, barring the examination of their predictive ability. It is well known that youth experiment with a variety of tobacco products and e-cigarettes, poly-use is common, and youth that experiment with tobacco products and/or e-cigarettes may share many characteristics in common. As a result, the tobacco cigarette susceptibility construct may predict the use of various tobacco products and/or e-cigarettes and not strictly tobacco cigarettes. Longitudinal approaches are necessary to assess the predictive ability of these measures and elucidate if they are reliable or whether alternative measures need to be developed for each product.
Given these gaps in the literature, this study examined the ability of the tobacco cigarette susceptibility construct as a whole and each measure of the susceptibility construct to predict ever and past 30 day use of tobacco cigarettes, as well as past 30 day use of 4 additional tobacco products (cigarillos or little cigars, cigars, hookah, and smokeless tobacco) and e-cigarettes, within a longitudinal sample of Canadian secondary school students through calculation of the sensitivity, specificity, positive predictive value, and negative predictive value.
Methods
COMPASS is a prospective cohort study designed to collect hierarchical longitudinal data from a sample of grade 9 to 12 secondary school students and the schools they attend in Ontario and Alberta, Canada.23 Data were collected annually from students in class time on the day of their school’s scheduled data collection using the COMPASS questionnaire (Cq) in purposefully sampled schools that provided permission to use active-information passive-consent parental permission protocols (as described elsewhere24). The current study reports longitudinal student-level linked data from year 2 (2013–2014), year 3 (2014–2015), and year 4 (2015–2016) of the COMPASS host study given that (1) these three waves of data have the largest sample size (as described by Reel et al.25), and (2) year 2 was the first time the Cq included a measure of e-cigarette use. For the purpose of our objectives, data from year 2 will be considered “baseline,” year 3 will be “follow-up year 1,” and year 4 will be “follow-up year 2.” A full description of the COMPASS study and its methods is available online (www.compass.uwaterloo.ca) and in print.23 The COMPASS study received ethics approval from the University of Waterloo Research Ethics Board, as well as participating school board review panels.
Sample Selection
At baseline, 52529 students in grades 9 to 12 were enrolled in the 79 participating schools in Ontario and 41734 of them (79.5%) completed the Cq; 11253 of these students were in grade 9. In follow-up year 1, 49773 students in grades 9 to 12 were enrolled in the 78 participating schools in Ontario and 39013 of them (78.7%) completed the Cq; 10381 of these students were in grade 10. Finally, in follow-up year 2, 46458 students in grades 9 to 12 were enrolled in the 72 participating schools in Ontario and 37106 of them (79.9%) completed the Cq; 9168 of these students were in grade 11. Missing data were primarily a result of student absenteeism the day of the data collection and students on spare (N = 29806; 20.0% of total); relatively few data were missing due to student or parent refusal (N = 1101; 0.7% of total). Using the unique code generated by each student to link their data over time,26 4651 students in grade 9 were linked across all 3 years of study (linked sample; 41.3%); 6602 students in grade 9 did not have data for each data collection year (unlinked sample). A comparison of demographic and behavioral characteristics of the linked sample to the unlinked sample can be found in Supplementary Table 1. Given that we were interested in identifying students that were susceptible to using tobacco products and e-cigarettes, grade 9 students that reported ever using tobacco cigarettes (even just a puff; N = 400) or another tobacco product or e-cigarette in the last 30 days (N = 134) were excluded from these analyses. An additional 250 students were excluded due to missing demographic (age or gender; N = 9) or outcome variables (tobacco product use or susceptibility; N = 241), leaving a final linked sample of 3867 students that had never smoked, not used an alternative tobacco product within the last 30 days, and not used e-cigarettes within the last 30 days at baseline (herein called current nontobacco/e-cigarette users).
Measures
The Cq uses items with demonstrated reliability and validity for current smoking27 and smoking susceptibility among never smokers.9 Susceptibility to future tobacco cigarette smoking among current nontobacco/e-cigarette users was derived by three previously validated measures9 that asked respondents:
Do you think in the future you might try smoking cigarettes? (S1-Try)
If one of your best friends was to offer you a cigarette, would you smoke it? (S2-Offer)
At any time during the next year do you think you will smoke a cigarette? (S3-Smoke)
Students indicated the degree to which they agreed with each statement on a Likert scale ranging from “definitely not” to “definitely yes.” Consistent with the algorithm proposed by Pierce et al.,9,10 current nontobacco/e-cigarette users who responded “definitely not” to all three questions were classified as “not susceptible to future tobacco/e-cigarette use,” while all other response groupings were classified as “susceptible to future tobacco/e-cigarette use.” Only measures that assessed susceptibility to future tobacco cigarette smoking were included in the Cq. Responses to this measure of susceptibility to future tobacco cigarette smoking were also used to identify students susceptible to future use of alternative tobacco products and e-cigarettes.
Experimentation with tobacco cigarettes was measured with a single question: “Have you ever tried cigarette smoking, even just a few puffs?” Similarly, experimentation with alternative tobacco products and e-cigarettes was measured with a single multi-item question. This question measured current use of each alternative tobacco product and e-cigarettes among respondents: “In the last 30 days, did you use any of the following? (Mark all that apply),” followed by a list of products other than tobacco cigarettes: cigarillos or little cigars (plain or flavored), cigars (not including cigarillos or little cigars, plain or flavored), e-cigarettes (electronic cigarettes that look like cigarettes/cigars, but produce vapor instead of smoke), smokeless tobacco (chewing tobacco, pinch, snuff, or snus), hookah (water-pipe) to smoke tobacco, hookah (water-pipe) to smoke herbal sheesha/shisha. Although this measure of use is different from that for tobacco cigarettes (ie, use in the last 30 days vs. ever use), it is a common measure of alternative tobacco product and e-cigarette use and it may measure more regular use rather than experimentation. A comparison of the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for different measures of tobacco cigarette smoking (ever use, past 30-day use, smoked 100 cigarettes in life) is presented in Supplementary Table 2. For our analyses, any respondents with all items missing from this question of alternative tobacco product and e-cigarette use had alternative tobacco product and e-cigarette use set to missing; additionally, respondents that indicated using hookah to smoke tobacco or to smoke herbal sheesha/shisha were combined and identified as “hookah users.”
Analysis
Given that students that smoke tend to drop out of longitudinal studies28 which could affect the analyses, chi-square tests compared the baseline demographic and behavioral characteristics of the linked and unlinked samples (Supplementary Table 1). A higher proportion of students that were linked across all 3 years were female, had less spending money, were not susceptible to future smoking, and did not have any friends that smoked cigarettes at baseline. Tobacco product use was assessed at follow-up year 1 and follow-up year 2 among students susceptible and not susceptible to future tobacco/e-cigarette use at baseline. Consistent with a previous validation study,13 the sensitivity, specificity, PPV, and NPV of the tobacco cigarette susceptibility construct (as a whole, and each of the three measures of the construct) were calculated for ever and past 30 day use of tobacco cigarettes, as well as past 30 day use of four additional tobacco products (cigarillos or little cigars, cigars, hookah, and smokeless tobacco) and e-cigarettes in follow-up year 1 and follow-up year 2. The sensitivity was defined as the percentage of students who reported currently using each tobacco product or e-cigarette at follow-up who were identified as susceptible to future tobacco/e-cigarette use. Similarly, the specificity was defined as the percentage of students who reported not currently using each tobacco product or e-cigarette at follow-up who were identified as not susceptible to future tobacco/e-cigarette use. Finally, the PPV was defined as the percentage of students identified as susceptible to future tobacco/e-cigarette use who reported currently using each tobacco product or e-cigarette at follow-up, while the NPV was defined as the percentage of students identified as not susceptible to future tobacco/e-cigarette use who did not report currently using each tobacco product or e-cigarette at follow-up.
Results
Self-Reported Tobacco or E-Cigarette Use at Follow-up
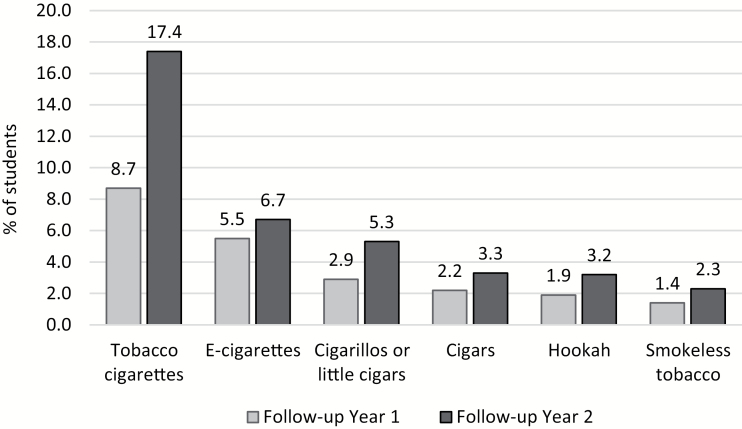
Among current nontobacco/e-cigarette users at baseline, 29.4% were susceptible to future tobacco/e-cigarette use. By follow-up year 1, 13.6% of current nontobacco/e-cigarette users at baseline reported using any tobacco product or e-cigarette. By follow-up year 2, the percentage of students that reported using any tobacco product or e-cigarette increased by 67% to 22.8%. Figure 1 presents the prevalence of tobacco product or e-cigarette use at follow-up year 1 and follow-up year 2. The most frequently used products in follow-up year 1 were tobacco cigarettes (8.7%), e-cigarettes (5.5%), and cigarillos or little cigars (CLC, 2.9%). Similarly, the most frequently used products at follow-up year 2 were tobacco cigarettes (17.4%), e-cigarettes (6.7%), and CLC (5.3%). The increase in prevalence of use of tobacco products and e-cigarettes was not uniform across products. Between follow-up year 1 and follow-up year 2 the prevalence of use of tobacco cigarettes doubled, the prevalence of use of CLC increased by 82.8%, and the prevalence of hookah use increased by 68.4%; the prevalence of use of e-cigarettes only increased by 21.8%.
Figure 1.
Self-reported tobacco product and e-cigarette use at follow-up year 1 and follow-up year 2 among current nontobacco/e-cigarette users at baseline, 2013–2016 COMPASS study.
Classification Accuracy of the Susceptibility Construct
Table 1 presents the sensitivity, specificity, PPV, and NPV for the tobacco cigarette susceptibility construct (presented by Pierce et al.) at follow-up year 1 and follow-up year 2 for each tobacco product and e-cigarettes. At both follow-up year 1 and follow-up year 2, the sensitivity, specificity, and NPV of the construct was high (over 50%, 70%, and 80%, respectively). At follow-up year 1, the sensitivity of the construct was highest for tobacco cigarettes (59.5%), hookah (57.5%), and smokeless tobacco (56.6%). At follow-up year 2, the sensitivity of the construct was highest for tobacco cigarettes (54.6%), e-cigarettes (51.5%), and hookah (51.2%). At follow-up year 1, the specificity of the construct was highest of tobacco cigarettes (73.5%), e-cigarettes (72.0%), and CLC (71.3%). Similarly, at follow-up year 2 the specificity of the construct was highest for tobacco cigarettes (75.9%), e-cigarettes (72.2%), and CLC (71.8%). Across all products, the NPV of the susceptibility construct decreased between follow-up year 1 and follow-up year 2. The PPV of the susceptibility construct varied between products and usually increased between follow-up year 1 and follow-up year 2. At follow-up year 1, the PPV of the construct was highest for tobacco cigarettes (17.7%), e-cigarettes (10.0%), and CLC (5.0%). Similarly, at follow-up year 2, the PPV of the construct was highest for tobacco cigarettes (32.2%), e-cigarettes (11.8%), and CLC (9.1%). Overall, the susceptibility construct was able to predict 25.6% of students that reported using any tobacco product or e-cigarette at follow-up year 1 and 39.5% of students that reported using any tobacco product or e-cigarette at follow-up year 2.
Table 1.
Sensitivity, Specificity, Positive Predictive Value, and Negative Predictive Value of the Susceptibility Construct at Follow-up Year 1 and Follow-up Year 2 for Each Tobacco Product or E-Cigarette, 2013–2016 COMPASS Study
| Tobacco product or e-cigarette | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | ||||
|---|---|---|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | |
| Tobacco cigarettes | 59.5 | 54.6 | 73.5 | 75.9 | 17.7 | 32.2 | 95.0 | 88.8 |
| E-cigarettes | 53.1 | 51.5 | 72.0 | 72.2 | 10.0 | 11.8 | 96.3 | 95.4 |
| Cigarillos or little cigars | 50.9 | 50.5 | 71.3 | 71.8 | 5.0 | 9.1 | 98.0 | 96.3 |
| Cigars | 56.0 | 49.6 | 71.2 | 71.3 | 4.1 | 5.6 | 98.6 | 97.7 |
| Hookah | 57.5 | 51.2 | 71.2 | 71.4 | 3.7 | 5.6 | 98.9 | 97.8 |
| Smokeless tobacco | 56.6 | 43.2 | 71.0 | 70.9 | 2.6 | 3.4 | 99.2 | 98.2 |
| Any tobacco product or e-cigarette | 55.2 | 51.1 | 74.7 | 77.0 | 25.6 | 39.5 | 91.4 | 84.3 |
Classification Accuracy of Each Susceptibility Measure
Table 2 presents the sensitivity, specificity, PPV, and NPV for each of the three tobacco cigarette susceptibility measures (S1-Try, S2-Offer, S3-Smoke) at follow-up year 1 and follow-up year 2 for each tobacco product and e-cigarettes. At both follow-up year 1 and follow-up year 2 the specificity of S1-Try, S2-Offer, and S3-Smoke was high (over 70%); however, the sensitivity of S1-Try, S2-Offer, and S3-Smoke was lower than that for the overall susceptibility construct. The PPV of S1-Try, S2-Offer, and S3-Smoke varied between products and increased between follow-up year 1 and follow-up year 2, while the NPV of S1-Try, S2-Offer, and S3-Smoke decreased between follow-up year 1 and follow-up year 2.
Table 2.
Sensitivity, Specificity, Positive Predictive Value, and Negative Predictive Value of Each Susceptibility Measure at Follow-up Year 1 and Follow-up Year 2 for Each Tobacco Product or E-Cigarette, 2013–2016 COMPASS Study
| Tobacco product or e-cigarette | S1-Try | S2-Offer | S3-Smoke | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | |||||||||||||
| Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | Year 1 | Year 2 | |
| Tobacco cigarettes | 52.7 | 47.7 | 78.6 | 80.8 | 19.0 | 34.3 | 94.6 | 88.1 | 47.2 | 40.6 | 83.7 | 85.6 | 21.7 | 37.2 | 94.3 | 87.3 | 41.8 | 34.7 | 86.6 | 88.0 | 23.0 | 37.8 | 94.0 | 86.5 |
| E-cigarettes | 43.4 | 44.2 | 77.0 | 77.3 | 9.9 | 12.4 | 95.9 | 95.1 | 39.2 | 35.0 | 82.2 | 82.2 | 11.3 | 12.4 | 95.9 | 94.6 | 31.6 | 29.7 | 85.0 | 85.1 | 10.9 | 12.5 | 95.5 | 94.4 |
| Cigarillos or little cigars | 42.3 | 41.9 | 76.4 | 76.9 | 5.1 | 9.1 | 97.8 | 96.0 | 39.3 | 36.3 | 81.6 | 82.0 | 6.0 | 10.1 | 97.8 | 95.8 | 30.4 | 27.5 | 84.5 | 84.8 | 5.5 | 9.1 | 97.6 | 95.4 |
| Cigars | 47.6 | 39.4 | 76.4 | 76.4 | 4.3 | 5.4 | 98.5 | 97.4 | 45.8 | 34.9 | 81.6 | 81.6 | 5.2 | 6.0 | 98.6 | 97.4 | 34.5 | 22.2 | 84.5 | 84.3 | 4.7 | 4.6 | 98.3 | 97.0 |
| Hookah | 48.6 | 42.4 | 76.4 | 76.5 | 3.8 | 5.7 | 98.7 | 97.5 | 46.6 | 33.6 | 81.6 | 81.5 | 4.6 | 5.7 | 98.8 | 97.3 | 34.3 | 30.7 | 84.5 | 84.6 | 4.1 | 6.2 | 98.5 | 97.4 |
| Smokeless tobacco | 45.3 | 34.1 | 76.2 | 76.1 | 2.6 | 3.2 | 99.0 | 98.0 | 39.6 | 31.8 | 81.3 | 81.3 | 2.9 | 3.8 | 99.0 | 98.1 | 22.6 | 18.2 | 84.2 | 84.2 | 2.0 | 2.6 | 98.7 | 97.8 |
| Any tobacco product or e-cigarette | 47.7 | 44.0 | 79.6 | 81.7 | 26.9 | 41.3 | 90.6 | 83.3 | 41.6 | 36.9 | 84.6 | 86.3 | 29.9 | 44.1 | 90.2 | 82.3 | 36.7 | 31.6 | 87.4 | 88.7 | 31.4 | 44.9 | 89.7 | 81.6 |
S1-Try: “Do you think in the future you might try smoking cigarettes?”
S2-Offer: “If one of your best friends was to offer you a cigarette, would you smoke it?”
S3-Smoke: “At any time during the next year do you think you will smoke a cigarette?
Discussion
This study identified that a significant number of youth that did not report current tobacco/e-cigarette use at baseline progressed to try smoking, use an alternative tobacco product, or use e-cigarettes over a 2-year follow-up period. In the current sample, more than 1 in 10 current nonsmoking students reported using a tobacco product or e-cigarette within 1 year of follow-up, and almost one in four students reported using a tobacco product or e-cigarette within 2 years of follow-up. It is apparent that many students use tobacco products or e-cigarettes during secondary school, even those that would not be identified as “at risk” (ie, not susceptible) to future tobacco product or e-cigarette use. The vast majority of tobacco product or e-cigarette users were students that were identified as “at risk” (ie, susceptible) to future tobacco product or e-cigarette use, indicating that methods of measuring susceptibility to future smoking are still useful and could identify those that would benefit the most from school-based tobacco prevention programming.
We found that the tobacco cigarette susceptibility construct predicted tobacco cigarette use among youth that did not report current tobacco/e-cigarette use in Ontario, Canada over a 2-year follow-up period, suggesting that this susceptibility construct is valid for identifying nonsmoking Ontario youth who are at the greatest risk of future tobacco cigarette use. Compared to the sensitivity (62.2%) and the specificity (49.6%) of the susceptibility construct calculated in a previous validation study that also used a longitudinal design,13 the sensitivity of the construct in the current study was lower and both the specificity and PPV were higher. Differences in assessing tobacco cigarette smoking between the current study (ever use) and the previous validation study (smoking 100 cigarettes in life) may explain some of these differences, especially the higher PPV calculated in the current study. Alternatively, age differences of the sample populations at baseline and follow-up between the current study and the previous validation study may account for some of these differences; the current study identified smoking status 1 and 2 years later, when the sample was still in secondary school. In contrast, the study by Strong et al.13 identified smoking status 3 and 6 years later, when the sample was in young adulthood. Finally, differences in tobacco control programs and policies across the two jurisdictions (California, USA vs. Ontario, Canada) and over time (1996 vs. 2014) may explain the reduced sensitivity and increased specificity and PPV. Differences in the tobacco control policy and program environment would also impact the baseline prevalence of use of these products among youth, which would impact later experimentation among susceptible and not susceptible youth. Given the potential influence of these differences, this construct should continue to be evaluated using different populations. Although the PPV of the construct was highest for tobacco cigarettes, it was still only able to predict about 17% of tobacco cigarette ever users 1 year later and 32% of tobacco cigarette ever users 2 years later. Additionally, the sensitivity values indicate that only about half of smokers were identified as “at risk” at baseline. It is evident that there is still knowledge to be gained about the smoking susceptibility construct and methods to identify those at risk of using tobacco cigarettes.
These data also illustrate that the tobacco cigarette susceptibility construct is transferrable to other products besides tobacco cigarettes. The results identify that the tobacco cigarette susceptibility construct best predicted e-cigarette use and CLC use; although the PPV for both products was lower than that for tobacco cigarettes (due to a lower prevalence of use), the sensitivity and specificity were both similar to that of tobacco cigarettes. Therefore, creating additional susceptibility measures specific to these products may not be necessary. Recent studies have begun to modify the susceptibility questions to identify students susceptible to the use of other tobacco products and e-cigarettes.18–22 Only one study used a longitudinal design to identify whether susceptibility measures specific to e-cigarettes predicted future e-cigarette use among youth.20 To our knowledge the sensitivity, specificity, PPV, and NPV of these measures have not been calculated. This study represents the first to explore the predictive validity of the original tobacco cigarette susceptibility construct for alternative tobacco products and e-cigarettes. Future studies should continue to compare the relative effectiveness of the original tobacco cigarette susceptibility construct to susceptibility measures that are specific to each tobacco product or e-cigarettes.
In addition to validating the tobacco cigarette susceptibility construct as a whole, these results illustrate that each susceptibility measure (S1-Try, S2-Offer, and S3-Smoke) was predictive of tobacco product and e-cigarette use. This suggests that although each measure asks about different situations where students could be tempted to try a tobacco product or e-cigarette, they all measure underlying intention to smoke in the future. Therefore, all three measures of the susceptibility construct or a single question from the construct could be used to measure susceptibility. This has important implications for survey development where the possibility of using a single question to measure susceptibility would reduce the burden on subjects while still providing useful data. However, it should be noted that given the differences in the sensitivity, specificity, PPV, and NPV of each measure, the choice of which measure to use should be considered carefully. For example, the sensitivity of S1-Try was always highest of all the measures, while the sensitivity of S3-Smoke was always the lowest of all the measures. Therefore, when the sensitivity of the measure is valued, S1-Try should be selected rather than S2-Offer or S3-Smoke. In contrast, the specificity was high and relatively stable across tobacco products, e-cigarettes, and measures. Therefore, specificity is less useful in determining which measure to include. The three measures of susceptibility may also perform differently depending on the measure of frequency of tobacco product or e-cigarette use; based on one study of susceptibility to e-cigarette use and initiation and current use 6 months later, being offered an e-cigarette by a friend was more predictive of e-cigarette initiation, while thinking about using an e-cigarette in the future was more predictive of current e-cigarette use.20 Additional evidence is needed for the reliability and validity of each measure of tobacco cigarette susceptibility and the tobacco cigarette susceptibility construct overall.
This study fills a much needed research gap with respect to the use of the tobacco cigarette susceptibility construct in Canada. Despite not having been validated for use in this context, numerous Canadian studies have used this construct to identify students at risk for using tobacco cigarettes and sociodemographic and behavioral characteristics associated with being susceptible to using tobacco cigarettes.29–31 The results from this large longitudinal study indicate that the tobacco cigarette susceptibility construct is valid for use among Canadian youth populations. The Cq collected data on a range of tobacco products and e-cigarettes, which allowed for the investigation of a novel use of the tobacco cigarette susceptibility construct for predicting the use of alternative tobacco products and e-cigarettes. Additionally, the use of passive consent procedures maximized the number of students that participated from each school, increasing the sample size available for analysis.
Although there are numerous strengths with this study, there are some limitations. The largest limitation rests with our measure of alternative tobacco product and e-cigarette use, which only assessed use within the last 30 days and not ever use. This measure also differed from our assessment of tobacco cigarette use (ever use). The more sensitive measure of tobacco cigarette use likely improved the positive predictive value that was calculated for tobacco cigarettes relative to the other products; however, the different measure of frequency of use did not have a noticeable impact on the calculated sensitivity or specificity as shown by the similar calculated values across tobacco products and e-cigarettes (also compare with Supplementary Table 2). The measure of alternative tobacco product and e-cigarette use also reduced our ability to limit the baseline sample to never tobacco/e-cigarette users. We excluded students that reported using an alternative tobacco product or e-cigarette in the past 30 days from the baseline sample, but some students may have tried alternative tobacco products or e-cigarettes in the past but not within the last 30 days; this would increase their susceptibility to future use. We expect that keeping these students in the sample would have had a limited effect on these analyses given that prevalence rates of alternative tobacco product and e-cigarette use among this young population remain low32 and the majority of alternative tobacco product and e-cigarette users also report using tobacco cigarettes.33,34 Given that our sample at baseline excluded students that reported ever using a tobacco cigarette, the vast majority of students would never have used a tobacco product or e-cigarette. Finally, a single question measured the use of each alternative tobacco product and e-cigarettes within the past 30 days, which may not reflect usual use or initiation of each product.
Other limitations are common to longitudinal studies of tobacco use. Consistent with previous evidence,28,35 the linked sample differed significantly on all demographic and behavioral characteristics from the unlinked sample (Supplementary Table 1). Given that tobacco users tend to drop-out of longitudinal studies,28 the current results may be an underestimate of the predictive validity of the tobacco cigarette susceptibility construct. This study relied on self-reported smoking behaviors; therefore, the validity of responses cannot be guaranteed. However, self-reported tobacco use measures have previously been demonstrated to be reliable and valid27,36 and students were ensured that their responses were confidential. Furthermore, limitations in the study design meant that data collections only occurred yearly, potentially missing critical developmental periods or life events that lead to smoking experimentation. Finally, the COMPASS study used a convenience sample of students; therefore, the results may not be generalizable to all youth in Ontario or Canada. However, given the longitudinal nature of the study and the large school and student sample size, the results have important implications for current research and practice.
Conclusion
A significant number of youth that did not report current tobacco product or e-cigarette use at baseline reported using tobacco products and e-cigarettes over a 2-year follow-up period. Methods to identify youth at risk for using various tobacco products and e-cigarettes continue to be warranted. The predictive validity of the tobacco cigarette susceptibility construct for tobacco cigarette, alternative tobacco product, and e-cigarette use among youth current nontobacco/e-cigarette users over a 2-year follow-up period was high. Furthermore, the predictive validity of each measure of the tobacco cigarette susceptibility construct for tobacco cigarettes, alternative tobacco product, and e-cigarette use was also high for youth current nontobacco/e-cigarette users. The tobacco cigarette susceptibility construct can be used to identify students at risk of using various tobacco products and e-cigarettes within Ontario, Canada. Future studies should continue to explore methods of identifying students at risk for using various tobacco products and e-cigarettes to inform and tailor tobacco prevention programs.
Funding
This work was supported by a Canadian Institutes of Health Research (CIHR) Doctoral Research Award—Frederick Banting and Charles Best Canada Graduate Scholarship (to AGC). The COMPASS study was supported by a bridge grant from the Canadian Institutes of Health Research (CIHR) Institute of Nutrition, Metabolism and Diabetes (INMD) through the “Obesity—Interventions to Prevent or Treat” priority funding awards (OOP-110788 to S.T.L.) and an operating grant from the Canadian Institutes of Health Research (CIHR) Institute of Population and Public Health (IPPH) (MOP-114875 to STL). STL is a Chair in Applied Public Health funded by the Public Health Agency of Canada (PHAC) in partnership with Canadian Institutes of Health Research (CIHR) Institute of Neurosciences, Mental Health and Addiction (INMHA) and Institute of Population and Public Health (IPPH).
Declaration of Interests
None declared.
Supplementary Material
References
- 1. Reid JL, Hammond D, Rynard VL, Burkhalter R.. Tobacco Use in Canada: Patterns and Trends. 2015 ed. Waterloo, Canada: Propel Centre for Population Health Impact, University of Waterloo; 2015:1–96. http://www.tobaccoreport.ca/. Accessed December 11, 2015. [Google Scholar]
- 2. Chapman SLC, Wu L-T. E-cigarette prevalence and correlates of use among adolescents versus adults: a review and comparison. J Psychiatr Res. 2014;54:43–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Choi K, Fabian L, Mottey N, Corbett A, Forster J. Young adults’ favorable perceptions of snus, dissolvable tobacco products, and electronic cigarettes: findings from a focus group study. Am J Public Health. 2012;102(11):2088–2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smith JR, Novotny TE, Edland SD, Hofstetter CR, Lindsay SP, Al-Delaimy WK. Determinants of hookah use among high school students. Nicotine Tob Res. 2011;13(7):565–572. [DOI] [PubMed] [Google Scholar]
- 5. Wray RJ, Jupka K, Berman S, Zellin S, Vijaykumar S. Young adults’ perceptions about established and emerging tobacco products: results from eight focus groups. Nicotine Tob Res. 2012;14(2):184–190. [DOI] [PubMed] [Google Scholar]
- 6. Benowitz NL. Nicotine addiction. N Engl J Med. 2010;362(24):2295–2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smith RF, McDonald CG, Bergstrom HC, Ehlinger DG, Brielmaier JM. Adolescent nicotine induces persisting changes in development of neural connectivity. Neurosci Biobehav Rev. 2015;55:432–443. [DOI] [PubMed] [Google Scholar]
- 8. Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain. J Physiol. 2015;593(16):3397–3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol. 1996;15(5):355–361. [DOI] [PubMed] [Google Scholar]
- 10. Pierce JP, Farkas AJ, Evans N, Gilpin E. An improved surveillance measure for adolescent smoking? Tob Control. 1995;4(suppl 1):S47–S56. [Google Scholar]
- 11. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- 12. Leatherdale ST. Evaluating school-based tobacco control programs and policies: an opportunity gained and many opportunities lost. Can J Program Eval. 2012;24(3):89–106. [Google Scholar]
- 13. Strong DR, Hartman SJ, Nodora J et al. . Predictive validity of the expanded susceptibility to smoke index. Nicotine Tob Res. 2015;17(7):862–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aslam SK, Zaheer S, Rao S, Shafique K. Prevalence and determinants of susceptibility to cigarette smoking among school students in Pakistan: secondary analysis of Global Youth Tobacco Survey. Subst Abuse Treat Prev Policy. 2014;9:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dube SR, Arrazola RA, Lee J, Engstrom M, Malarcher A. Pro-tobacco influences and susceptibility to smoking cigarettes among middle and high school students—United States, 2011. J Adolesc Health. 2013;52(5 suppl):S45–S51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Forrester K, Biglan A, Severson HH, Smolkowski K. Predictors of smoking onset over two years. Nicotine Tob Res. 2007;9(12):1259–1267. [DOI] [PubMed] [Google Scholar]
- 17. Nodora J, Hartman SJ, Strong DR et al. . Curiosity predicts smoking experimentation independent of susceptibility in a US national sample. Addict Behav. 2014;39(12):1695–1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Krishnan-Sarin S, Morean ME, Camenga DR, Cavallo DA, Kong G. E-cigarette use among high school and middle school adolescents in connecticut. Nicotine Tob Res. 2015;17(7):810–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Saddleson ML, Kozlowski LT, Giovino GA et al. . Risky behaviors, e-cigarette use and susceptibility of use among college students. Drug Alcohol Depend. 2015;149:25–30. [DOI] [PubMed] [Google Scholar]
- 20. Bold KW, Kong G, Cavallo DA, Camenga DR, Krishnan-Sarin S. E-cigarette susceptibility as a predictor of youth initiation of e-cigarettes. Nicotine Tob Res. 2016:1–5. doi: 10.1093/ntr/ntw393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Portnoy DB, Wu CC, Tworek C, Chen J, Borek N. Youth curiosity about cigarettes, smokeless tobacco, and cigars: prevalence and associations with advertising. Am J Prev Med. 2014;47(2 suppl 1):S76–S86. [DOI] [PubMed] [Google Scholar]
- 22. Mathur C, Stigler MH, Erickson DJ et al. . Socioeconomic differences in the risk profiles of susceptibility and ever use of tobacco among Indian urban youth: a latent class approach. Nicotine Tob Res. 2014;16(4):454–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Leatherdale ST, Brown KS, Carson V et al. . The COMPASS study: a longitudinal hierarchical research platform for evaluating natural experiments related to changes in school-level programs, policies and built environment resources. BMC Public Health. 2014;14:331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Thompson-Haile A, Leatherdale ST.. School Board and School Recruitment Procedures. Waterloo, Canada: University of Waterloo; 2013:1–4. www.compass.uwaterloo.ca. Accessed October 8, 2015. [Google Scholar]
- 25. Reel R, Bredin C, Battista K, Leatherdale ST.. COMPASS Year 3 and 4 School Recruitment and Retention. Waterloo, Canada: University of Waterloo; 2017:1–9. www.compass.uwaterloo.ca. Accessed April 24, 2017. [Google Scholar]
- 26. Bredin C, Leatherdale ST.. Methods for Linking COMPASS Student-Level Data Over Time. Waterloo, Canada: University of Waterloo; 2013:1–6. www.compass.uwaterloo.ca. Accessed October 13, 2015. [Google Scholar]
- 27. Wong SL, Shields M, Leatherdale S, Malaison E, Hammond D. Assessment of validity of self-reported smoking status. Health Rep. 2012;23(1):47–53. [PubMed] [Google Scholar]
- 28. Siddiqui O, Flay BR, Hu FB. Factors affecting attrition in a longitudinal smoking prevention study. Prev Med. 1996;25(5):554–560. [DOI] [PubMed] [Google Scholar]
- 29. Azagba S, Asbridge M. School connectedness and susceptibility to smoking among adolescents in Canada. Nicotine Tob Res. 2013;15(8):1458–1463. [DOI] [PubMed] [Google Scholar]
- 30. Kaai SC, Brown KS, Leatherdale ST, Manske SR, Murnaghan D. We do not smoke but some of us are more susceptible than others: a multilevel analysis of a sample of Canadian youth in grades 9 to 12. Addict Behav. 2014;39(9):1329–1336. [DOI] [PubMed] [Google Scholar]
- 31. Leatherdale ST, Wong SL, Manske SR, Colditz GA. Susceptibility to smoking and its association with physical activity, BMI, and weight concerns among youth. Nicotine Tob Res. 2008;10(3):499–505. [DOI] [PubMed] [Google Scholar]
- 32. Reid JL, Hammond D, Rynard VL, Madill CL, Burkhalter R.. Tobacco Use in Canada: Patterns and Trends. 2017 ed. Waterloo, Canada: Propel Centre for Population Health Impact, University of Waterloo; 2017:1–112. https://uwaterloo.ca/tobacco-use-canada/sites/ca.tobacco-use-canada/ files/uploads/files/2017_tobaccouseincanada_final_0.pdf. Accessed June 19, 2017. [Google Scholar]
- 33. Brooks A, Gaier Larkin EM, Kishore S, Frank S. Cigars, cigarettes, and adolescents. Am J Health Behav. 2008;32(6):640–649. [DOI] [PubMed] [Google Scholar]
- 34. Saunders C, Geletko K. Adolescent cigarette smokers’ and non-cigarette smokers’ use of alternative tobacco products. Nicotine Tob Res. 2012;14(8):977–985. [DOI] [PubMed] [Google Scholar]
- 35. Qian W, Battista K, Bredin C, Brown KS, Leatherdale ST.. Assessing Longitudinal Data Linkage Results in the COMPASS Study. Waterloo, Canada: University of Waterloo; 2015:1–28. www.compass.uwaterloo.ca. Accessed April 24, 2017. [Google Scholar]
- 36. Fendrich M, Mackesy-Amiti ME, Johnson TP, Hubbell A, Wislar JS. Tobacco-reporting validity in an epidemiological drug-use survey. Addict Behav. 2005;30(1):175–181. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.