Abstract
Purpose:
To determine the association of depressive and PTSD symptoms with cardiac arrest survivors’ long-term recovery perceptions, after accounting for cognitive status, functional independence, and medical comorbidities.
Methods:
Perceived recovery of 78 cardiac arrest survivors at 6-months post-hospital discharge was assessed through the question, “Do you feel that you have made a complete recovery from your arrest?” Psychological symptoms were measured using the Center for Epidemiological Studies-Depression scale (CES-D) and the PTSD Checklist-Specific (PCL-S). Logistic regression was utilized to assess the association between psychological symptoms with positive and negative recovery perceptions, adjusting for demographics, cognitive impairment, functional dependence, and medical comorbidities.
Results:
At 6 months, 53% of patients (n=41) had negative recovery perceptions. 32.1% (n=25) of patients screened for depression and 28.2% (n=22) for PTSD. Patients with higher CES-D scores were significantly more likely to have negative recovery perceptions in both unadjusted and adjusted analyses (OR: 1.10, 95% CI [1.03, 1.16], p<0.01). PCL-S scores were significantly associated with negative recovery perceptions in an unadjusted model (OR: 1.05, 95% CI [1.01, 1.10], p < 0.01), but not after adjustment of covariates.
Conclusions:
In contrast with cognitive and functional measures, depressive symptoms were strongly associated with cardiac arrest survivors’ negative recovery perceptions at 6-months post-discharge.
Keywords: Cardiac Arrest, Perception, Value Based Health Care, Patient Report Outcome Measures, Depression, Posttraumatic Stress Disorder, Neuropsychological Tests, Cognitive Dysfunction
Introduction
Innovations in technology and treatment protocols have led to improvements in survival rates after cardiac arrest [1]. With the advent of greater survivability, there has been increased recognition of post-cardiac arrest survivorship as a chronic condition implicated in cognitive, functional, and psychological sequelae secondary to anoxic brain injury [2–4]. Given the overall increase in patients with multiple chronic conditions, value based health care systems [5] have prioritized outcomes deemed important by the patient (i.e. patient reported outcome measures (PROMs)), which can help facilitate shared decision making. Utilization of PROMs has led to improvements in patients’ daily lives, such as satisfaction with care [6] and depressive symptoms [7]. Accordingly, identifying underlying factors contributing to an encompassing PROM, such as perceived recovery, could improve the daily and multifaceted challenges faced by cardiac arrest survivors.
Despite the various chronic symptoms that cardiac arrest survivors face, it remains unclear which deficits are most strongly associated with long-term perceived recovery. For example, Steinbusch et al [8] found that post-arrest patients’ perceived cognitive impairments were not indicative of their actual cognitive impairments at 3- and 12-month follow-ups. On the contrary, Juan et al [9] found post-arrest patients’ cognitive impairments, but not depressive symptoms, to be strongly correlated with negative perceptions of recovery at 6-months; however, the incidence of depression in that cohort was low (6%), and the relatively small sample size (n=50) precluded definitive conclusions. In samples of stroke survivors and older adults, subjects’ cognitive complaints were correlated with emotional well-being and depressive symptoms, rather than objective measures of cognitive impairment [10,11].
There is strong support linking psychological sequelae with subjective well-being, and potentially perceived recovery, in patients with cardiac disease. For example, the prevalence of posttraumatic stress disorder (PTSD) secondary to a cardiac event has ranged from 0–38% (averaging 12%) [12]. This condition has been linked to negative illness perceptions, emotional distress, reduced quality of life, and preoccupation with somatic symptoms [12]. Depressive symptoms also pose a challenge for cardiac patients; 20–40% meet criteria for major depressive disorder or experience an increase in chronic and persistent depressive symptoms post-diagnosis [13]. Further, in cardiac patients, depression has been found to be a stronger predictor of quality of life than measures of disease severity including cardiac function, ejection fraction, and ischemia [14].
We recently demonstrated that posttraumatic stress and depressive symptoms, not cognitive or functional impairment, were associated with cardiac arrest survivors’ negative recovery perceptions at hospital discharge [15]. The present study aims to extend this work by examining the correlates of perceived recovery in these cardiac arrest survivors at 6 months after their hospital discharge. This is especially important to delineate in order to identify possible modifiable factors for improving perceived recovery, as is vital in value based health care systems. Based on the strong link between cardiac disease-induced psychological symptoms and outcomes of subjective well-being, we tested the hypothesis that depressive and PTSD symptoms are correlated with cardiac arrest survivors’ long-term recovery perceptions even after accounting for cognitive status, functional independence, and medical comorbidities. In addition, we examined the stability of recovery perceptions from discharge to 6 months.
Methods
Screening Procedure and Patient Enrollment
Details on the patient screening and enrollment procedure at hospital discharge can be found at Presciutti et al [15]. Briefly, subjects were included if they were ≥ 18 years of age, resuscitated following either in-hospital or out-of-hospital cardiac arrest, admitted to Columbia University Medical Center, and survived to hospital discharge between September 2015 and September 2017.
As part of research protocol, daily intensive care unit screening identified potential participants per diagnostic codes, who were then approached for consent; participants gave written informed consent. Participation was contingent on having sufficient mental status at hospital discharge, defined as having a Cerebral Performance Category score (CPC) of 3 or less, being alert and oriented to person, place, and date, and having no presence of delirium, agitation, or sedation according to the Confusion Assessment Method for the ICU (CAM-ICU) [16] and the Richmond Agitation-Sedation Scale (RASS) [17]. Patients with significant aphasia or dysarthria were not included.
Data Collection
Demographics and cardiac arrest variables were collected by a trained research coordinator at hospital discharge via chart review. Measures were collected by a trained research coordinator at approximately 6 months (median: 6.6 months, IQR 6.1–9.3) after each patient’s hospital discharge date. The main outcome of this study, perceived recovery, was assessed at hospital discharge and at 6 months. Interviews took place either in person or over the telephone for those who were limited by distance or travel issues. The order of collected measures during in-person interviews was as follows: The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) [18], the perceived recovery question, the Center for Epidemiological Studies - Depression (CES-D) scale [19], the PTSD Checklist - Specific (PCL-S) scale [20], and the Lawton Instrumental Activities of Daily Living Scale (M-IADL) [21]. For follow-ups conducted over the telephone, the Telephone Interview for Cognitive Status (TICS) [22] was administered in place of the RBANS.
Measures
Perceived Recovery from Cardiac Arrest
Perceived recovery was measured using a single item, “Do you feel that you have made a complete recovery from your arrest?” Response options were yes/no. This is an adapted version of a validated question used after stroke [23–27] and cardiac arrest [15,28]. Patients were categorized as having a “negative recovery perception” if they responded “no” to the recovery question. Patients who responded “yes” to the recovery question were categorized as having a “positive recovery perception.”
Cognitive Status
Cognitive status was measured through the RBANS, a 30-minute battery which assesses immediate memory, semantic fluency, attention, visuospatial awareness, and delayed memory. Scores range from 40–160, with average scores falling within 80–119 [29]. Results were scored according to the publisher’s normative data. Patients that could not attend in-patient follow-ups completed the TICS. TICS scores range from 0 (worst) to 51 (best). Scores ≤30 were considered impaired, a cut-off that has discriminated between demented and non-demented patients [30] and corresponded with global cognitive impairment after subarachnoid hemorrhage [31]. In this study, patients were considered cognitively impaired if they had an RBANS score of <80, or, for those unavailable for in-person follow-ups, a TICS score of ≤30.
Psychological Symptoms
Psychological symptoms were assessed at 6 months via the CES-D and the PCL-S, which are commonly used screeners for depression and PTSD symptoms, respectively. The CES-D queries for depressive symptomatology in the previous week. The CES-D ranges from 0–60; a score ≥ 16 indicates significant depression symptoms [19].
The PCL-S queries for PTSD symptomatology in relation to an identified stressful experience in the past month. In this study, PTSD symptoms were queried with reference to the acute cardiac arrest event and subsequent hospitalization. The PCL-S is a 17-item screener (scores ranging from 17–85) that relies on the DSM-IV conceptualization of PTSD; we used a suggested diagnostic cut-off of 36 for specialized medical settings [32].
Independence in Instrumental Activities of Daily Living
Independence in instrumental activities of daily living (IADLs) at 6 months was assessed through the M-IADL. The M-IADL ranges from 0–30, with a score of 0 signifying complete independence IADLs. In this study, patients were considered dependent in IADLs if they had an M-IADL score >0.
Medical Comorbidities
The Charlson Comorbidity Index (CCI) [33] was used to capture pre-arrest medical comorbidities based on chart review. The CCI has been used extensively to predict outcomes and has been validated across clinical cohorts [34].
Statistical Analyses
Fisher’s Exact and Wilcoxon-Rank Sum tests were used to compare differences between respondents in demographics and outcome measures. This same approach was used to compare baseline differences between patients that were included in the study with those lost to follow-up.
Univariate logistic regression models were used to calculate odds ratios (OR) for assessing the strength of associations between single factors and perceived recovery at 6 months (negative vs. positive recovery perception). Selection of variables included in the final multivariable models was based on clinical importance and expected confounders. Three increasingly adjusted logistic regression models (adjusted for demographics and comorbidities only; further adjusted for cognitive impairment; further adjusted for IADL dependence) were used to calculate adjusted ORs for assessing the strength of associations between PTSD and depressive symptoms, separately, with perceptions of recovery from cardiac arrest. Total scores were used for the CES-D and PCL-S and treated as continuous variables. Cognitive impairment and dependence of IADLs were treated as categorical variables as per criteria discussed above.
In addition to the main cross-sectional analysis, we also examined the extent of stability of patient perceptions from discharge to 6 months. Patients were categorized as either having a “stable negative perception” (negative perception at discharge and negative perception at 6 months), “new negative perception” (positive perception at discharge changed to a negative perception at 6 months), “stable positive perception” (positive perception at discharge and positive perception at 6 months), or “new positive perception” (negative perception at discharge changed to a positive perception at 6 months).
Results
Participant Characteristics
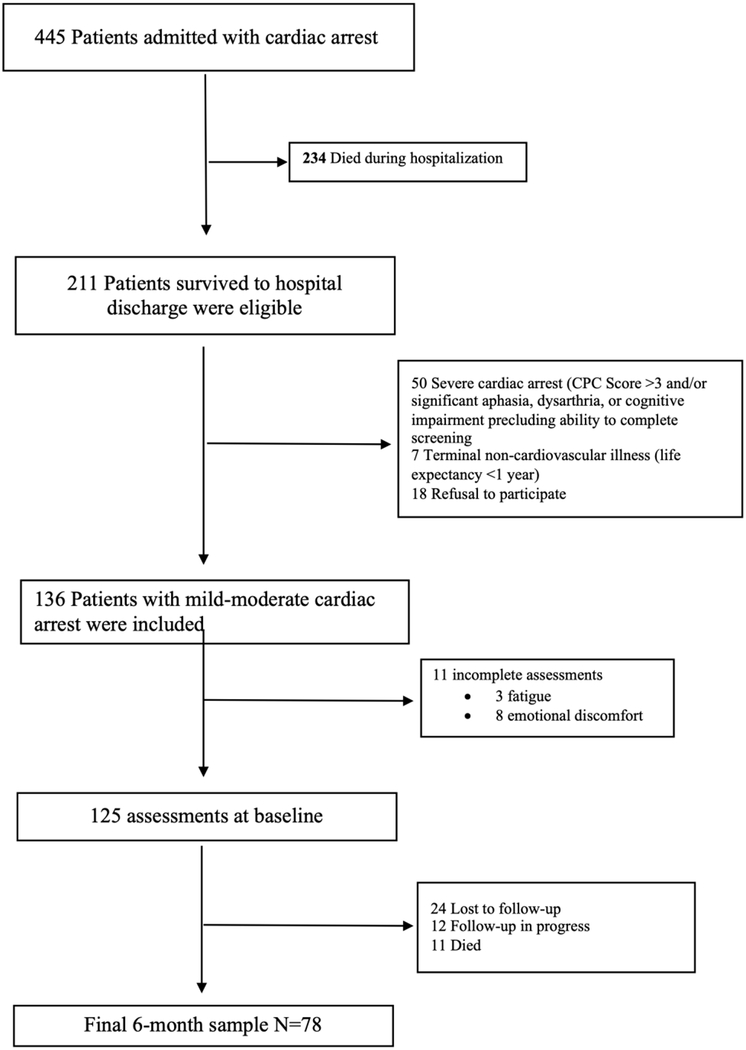
Information on the overall sample enrollment can be seen in Figure 1. No significant differences were found between those with a negative recovery perception from those with a positive recovery perception in terms of demographic characteristics (Table 1). Patients that were lost to follow-up had significantly shorter length of stays in both the intensive care unit (p < .05) and the hospital (p < .01) and were less likely to receive bystander CPR by nonmedical personnel (p < .05) compared to those included (Table 1 Supplemental).
Figure 1.
Flow chart of patient enrollment.
Table 1.
Association between demographics, comorbidity, and cardiac arrest factors and recovery perception
| Patient Characteristic | Negative Recovery Perception (53%; n = 41) | Positive Recovery Perception (47%; n = 37) | P-value |
|---|---|---|---|
| Demographics | |||
| Age, mean ± SD1 | 55.9 ± 16.6 | 52.3 ± 14.9 | .30 |
| Male, % (n) | 60.9 (25) | 70.3 (26) | .47 |
| Race, % (n) | .27 | ||
| White | 48.8 (20) | 59.4 (22) | |
| Black | 17.1 (7) | 8.1 (3) | |
| Hispanic | 29.3 (12) | 18.9 (7) | |
| Asian | 4.9 (2) | 13.5 (5) | |
| Insurance, % (n) | .96 | ||
| Medicare | 22 (9) | 27.8 (10) | |
| Medicaid | 19.5 (8) | 19.4 (7) | |
| Combined | 9.8 (4) | 8.3 (3) | |
| Private | 36.6 (15) | 36.1 (13) | |
| Uninsured | 12.2 (5) | 8.3 (3) | |
| Annual income, % (n) | .16 | ||
| <$45,000 | 30 (12) | 14.3 (5) | |
| >$45,000 | 70 (28) | 85.7 (30) | |
| Smoking, % (n) | .73 | ||
| Never Smoker | 48.7 (19) | 57.6 (19) | |
| Former Smoker | 36 (14) | 27.3 (9) | |
| Current Smoker | 15.4 (6) | 15.2 (5) | |
| Recent alcohol consumption, % (n) | 18 (7) | 27 (10) | .41 |
| Comorbidities at time of cardiac arrest | |||
| Obese, % (n) [BMI ≥ 30 kg/m2] | 40 (16) | 33.3 (12) | .64 |
| Charlson Comorbidity Index, median (IQR2) | 2 (1–4) | 3 (1–4) | .25 |
| Premorbid Psychological Diagnosis, % (n) | 22 (9) | 11.1 (4) | .23 |
| Premorbid CPC3, % (n) | .17 | ||
| CPC 1 | 83 (34) | 97.2 (35) | |
| CPC 2 | 9.8 (5) | 0 (0) | |
| CPC 3 | 7.3 (3) | 2.8 (1) | |
| Arrest Related Factors | |||
| In-hospital Arrests, % (n) | 63.4 (26) | 55.6 (20) | .49 |
| CPR4, % (n) | .41 | ||
| No CPR | 5 (2) | 14.7 (5) | |
| Bystander CPR | 20 (8) | 17.7 (6) | |
| CPR provided by EMS or medical personnel | 75 (30) | 67.7 (23) | |
| Defibrillation, % (n) | .9 | ||
| No Defibrillation | 23.1 (9) | 27.3 (9) | |
| Bystander Defibrillation | 2.6 (1) | 3 (1) | |
| Defibrillation provided by EMS or medical personnel | 74.4 (29) | 69.7 (23) | .9 |
| Initial Cardiac Rhythm, % (n) | .89 | ||
| Ventricular Tachycardia/Fibrillation | 48.8 (20) | 52.8 (19) | |
| Pulseless Electrical Activity | 24.4 (10) | 30.6 (11) | |
| Asystole | 26.8 (11) | 16.7 (6) | .6 |
| Return of Spontaneous Circulation minutes), median (IQR) | 9 (3–18) | 6 (3–15) | .42 |
| Targeted Temperature Management, % (n) | 39 (16) | 38.9 (14) | .58 |
| Length of ICU5 Stay (days), median (IQR) | 11 (6–20) | 10 (4–18) | .5 |
| Length of Hospital Stay (days), median (IQR) | 25 (15–36.5) | 23 (10–38) | .31 |
| Discharge Disposition, % (n) | .31 | ||
| Home | 36.6 (15) | 52.8 (19) | |
| Inpatient Rehabilitation | 53.7 (22) | 36.1 (13) | |
| Skilled Nursing | 9.8 (4) | 11.1 (4) |
SD Standard Deviation
IQR Interquartile Range
CPC Cerebral Performance Category scale
CPR Cardiopulmonary Resuscitation
ICU Intensive Care Unit
Correlates of Perceived Recovery at 6-Months after Cardiac Arrest
37.5% (n = 15) of patients that received the RBANS had below average cognitive functioning, according to the publisher’s normative data. After including patients who received the TICS, 26.9% (n = 21) of the total sample were cognitively impaired. There were no significant differences between those with a negative vs positive recovery perception in terms of cognitive status (Table 2).
Table 2.
Association between psychological, cognitive, and functional characteristics and cardiac arrest recovery perception
| Measures | Total Current Sample | Patients per Variable | Negative Recovery Perception | Positive Recovery Perception | p-value |
|---|---|---|---|---|---|
| Recovery Perception % (n) | - | 78 | 53 (41) | 47 (37) | - |
| RBANS1 below average (<80)*, % (n) | 37.5 (15) | 40 | 17.1 (7) | 21.6 (8) | .99 |
| Cognitive impairment@, % (n) | 26.9 (21) | 78 | 26.8 (11) | 27 (10) | .99 |
| Instrumental activities of daily living dependence (>0), % (n) | 64.1 (50) | 78 | 73.2 (30) | 54.1 (20) | .06 |
| Depressive symptoms (CES-D)3, median (IQR)4 | 10.5 (3–21) | 78 | 15 (6–25) | 4 (2–12) | <.001 |
| Probable Depression (CES-D ≥16)^, % (n) | 32.1 (25) | 78 | 48.8 (20) | 13.5 (5) | <.01 |
| PTSD symptoms (PCL-S)5, median (IQR) | 26 (20–39) | 78 | 30 (22–43) | 22 (19–28) | .01 |
| Probable PTSD (PCL-S ≥36)#, % (n) | 28.2 (22) | 78 | 39 (16) | 16.2 (6) | .04 |
RBANS = Repeatable Battery for Neuropsychological Status
TICS = Telephone Interview for Cognitive Status
CES-D = Center for Epidemiological Studies-Depression
IQR = Interquartile Range
PCL-S = Post-Traumatic Stress Disorder Checklist – Specific
Cut-off for average RBANS score (Randolph, 2012)
Impairment on RBANS or TICS if patient not available for in-person follow-up
Suggested CES-D cut-off (Lewinsohn et al., 1997)
Suggested PCL-S medical setting cut-off (National Center for PTSD, 2012)
64.1% (n = 50) of patients were dependent in at least one aspect of IADLs based on the M-IADL; patients with a negative recovery perception had a trend towards worse dependence in IADLs compared to those with a positive perception (p = .06) (Table 2).
Regarding psychological symptoms, 32.1% (n = 25) of patients had probable depression based on the suggested diagnostic cut-off on the CES-D and 28.2% (n = 22) had probable PTSD based on the suggested diagnostic cut-off on the PCL-S. Compared to patients with a positive recovery perception, patients with a negative recovery perceptions had worse CES-D (p < 0.01) and PCL-S scores (p < 0.05). Further, 80% (n = 20/25) of patients with probable depression and 73% (n = 16/22) of patients with probable PTSD had a negative recovery perception, respectively (Table 2).
Greater depressive symptoms (OR: 1.10, 95% CI [1.4, 1.16], p < 0.001) and PTSD symptoms (OR: 1.05, 95% CI [1.01, 1.10], p < 0.01) each demonstrated a significant association with negative recovery perceptions in univariate models. Regression diagnostics showed that depressive and PTSD were highly correlated (Pearson’s r2 = 0.82, p <0.001), with no evidence of an interaction between the two variables (p = 0.3). Due to artifact of the collinearity between these symptoms’ scores and the small sample size, two separate sets of three multivariable logistic regression models were created. Greater depressive symptoms remained significantly associated with negative recovery perceptions after adjusting for age, gender, race, CCI, impaired cognition, and dependence in IADLs (OR: 1.10, 95% CI [1.03, 1.16], p < 0.01) (Table 3). In the fully adjusted model, the association of PTSD symptoms with negative recovery perceptions approached, but did not reach, the level of statistical significance (Table 3).
Table 3.
Multivariable adjusted association between psychological symptoms and recovery perception
| Depression Models | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Covariates | 95% CI | 95% CI | 95% CI | ||||||
| CES-D1 Total Score | 1.04–1.16 | 1.04–1.17 | 1.03–1.16 | ||||||
| Age | .94–1.03 | .93–1.02 | .93–1.02 | ||||||
| Gender | .33–2.80 | .23–2.20 | .25–2.61 | ||||||
| Race | .74–1.68 | .78–1.89 | .75–1.85 | ||||||
| CCI2 | .68–1.30 | .67–.31 | .65–1.29 | ||||||
| Impaired Cognition | .11–1.50 | .11–1.48 | |||||||
| Dependent IADLs3 | .48–5.35 | ||||||||
| PTSD Models | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Covariates | 95% CI | 95% CI | 95% CI | ||||||
| PCL-S1 Total Score | 1.01–1.10 | 1.00–1.09 | 1.00–1.09 | ||||||
| Age | .94–1.03 | .94–1.03 | .94–1.03 | ||||||
| Gender | .29–2.23 | .22–1.80 | .25–2.18 | ||||||
| Race | .76–1.64 | .76–1.77 | .73–1.72 | ||||||
| CCI2 | .68–1.26 | .66–1.27 | .63–1.23 | ||||||
| Impaired Cognition | .18–1.94 | .16–1.87 | |||||||
| Dependent IADLs3 | .60–.5.75 | ||||||||
CES-D = Center for Epidemiological Studies Depression
CCI = Charlson Comorbidity Index
IADLs = Instrumental activities of daily living
PCL-S = PTSD Checklist - Specific
CCI = Charlson Comorbidity Index
IADLs = Instrumental activities of daily living
Stability of Perceived Recovery
79.5% of patient perceptions remained stable between discharge and 6 months. The breakdown between groups was as follows: 43.5% (n = 34) of patients had a stable negative perception, 3.8% (n = 3) new negative perception, 35.9% (n = 28) stable positive perception, and 16.6% (n = 13) new positive perception.
Discussion
This cross-sectional analysis found that depressive symptoms, not cognitive impairment, functional dependence, or medical comorbidities, were associated with cardiac arrest survivors’ recovery perceptions at long-term follow-up. Patients with greater depressive symptoms were more likely to have a negative recovery perception 6-months after hospital discharge from their cardiac arrest. Overall, 80% of patients that screened positive for probable depression and 73% of patients that screened positive for probable PTSD had a negative recovery perception at follow-up. Moreover, there were no significant differences in perceptions of recovery based on cardiac-arrest related medical variables between the two groups. In addition, the vast majority of patients (79.5%) experienced no change in recovery perceptions between discharge and six months.
The incidence of patients screening positive for probable depression in this cohort (32.1%) is comparable to other studies of patients with cardiac arrest and other acute cardiovascular events [4,13,35,37]. The association between depressive symptoms and negative recovery perceptions was expected, as depression in cardiac disease has consistently been shown to be a greater predictor of quality of life than various important medical predictors [14,37]. From a behavioral standpoint, depressive symptoms such as anhedonia and withdrawal have been shown to influence patients to take a passive role in their post-discharge treatment (i.e. medication nonadherence, lifestyle, and rehabilitation noncompliance) [35,38,39], which can ultimately lead to a worse perceived and actual recovery. Due to low rates of depression in Juan et al [9], their study could not assess the effect of depressive symptoms on recovery perceptions. Overall, our findings support the notion that, when present, depressive symptomatology holds greater importance in cardiac patients’ perceived recovery compared to other recovery domains. Value based health care paradigms, which strongly emphasize PROMs, must take this into account when treating such patients.
Despite 80% of patients screening for PTSD also having a negative recovery perception, PTSD symptoms approached, but did not reach, the level of a statistical association with perceived recovery. Further study examining the overlapping components of PTSD and depression, such as anhedonia and withdrawal, on recovery perceptions may uncover significant results.
This study provides further support for previous findings that cognitive impairment is not indicative of perceived recovery [8,10,11,15] and contrasts those of Juan et al [9]. A potential explanation for the lack of association between cognition and perceived recovery may be that patients were not fully aware of the true extent of their impairments [8]. Consequent studies of similar methodology should include an insight tool to test this hypothesis.
There were no significant differences in arrest related variables between the negative and the positive perception group. These findings complement those by Agarwal et al [40] such that arrest related variables are neither predictive of objective nor subjective long-term recovery. This finding is also consistent with the broader literature on PTSD secondary to a cardiac event in that objective measures of cardiac event severity are not associated with psychological outcomes in these patients [41].
Importantly, the vast majority of patients maintained the same recovery perception between discharge and six months. Furthermore, a sizeable percentage of patients experienced stable negative perceptions between the two time points (43.5%). The stability of these perceptions, particularly the negative perceptions, further indicate a need to attend to factors which characterize perceived recovery (i.e. depressive symptoms) as early as possible.
Finally, the use of perceived recovery as a PROM in this study and before [15, 23–28], has been validated in cardiac arrest and stroke. Continued use and analysis of this PROM in other chronic populations could reveal important underlying factors that impact a patient’s experience of the recovery process.
This study is not without limitations. First, because the Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition (DSM-5) was published after the conception of the parent study, the measures we used for posttraumatic stress and depressive symptoms were based on the Diagnostic and Statistical Manual for Mental Disorders-Fourth Edition (Text Revision) (DSM-IV-TR) PTSD criteria. Despite this, DSM-IV-TR PTSD symptoms have been found to reliably yield DSM-5 estimates of the disorder [42]. Further, there were minimal alterations between the DSM-IV-TR and DSM-5 for major depressive disorder, without any changes in the core criteria symptoms.
Second, our parent study lacked a comprehensive psychopathology assessment beyond the diagnostic screeners for PTSD and depression. Additionally, despite the high prevalence of anxiety symptoms in cardiac arrest survivors, an anxiety symptom screener was not included in the parent study during the enrollment of these patients and therefore was not included in these analyses. Employing a formal psychiatric evaluation is necessary to accurately capture the prevalence of patients meeting diagnostic criteria for PTSD, depression, and anxiety disorders.
Third, the TICS was used in approximately half of the sample and may be less sensitive than the RBANS. Nevertheless, the TICS remains a robust outcome measure and the cut-off that was used has reliably differentiated between demented and non-demented patients [30] and revealed impairments in other global brain injury models such as subarachnoid hemorrhage [31].
Fourth, given the cross-sectional nature of this study, there remains the possibility that negative recovery perceptions might be an indicator of depression rather than a separate construct. Additionally, we were unable to run a longitudinal analysis between time points due to the low occurrence of patients in the change categories (i.e. new negative perception, new positive perception) which would have resulted in inadequately powered models. However, based on the finding that 79.5% of patients did not experience a change in perception from baseline, intervention may be needed to address factors associated with negative recovery perceptions (e.g. depressive symptoms).
Finally, the cohort in this study was a small convenience sample which experienced a 24% dropout rate between discharge and 6 months. As a result, these findings may not be generalizable to all cardiac arrest survivors discharged with good neurological functioning.
Conclusions
In contrast with cognitive and functional measures, depressive symptoms were strongly associated with cardiac arrest survivors’ negative recovery perceptions. This study adds to the support that psychological symptoms are intimately tied to subjective recovery in patients with chronic cardiac conditions, and thus cannot be overlooked in the evaluation and management of such patients.
Supplementary Material
Acknowledgements:
We thank Dr. Angela Velazquez for her support with data collection. We also thank the nurses, physician assistants, nurse practitioners, and physicians who take care of these patients.
Financial Disclosures: Dr. Sumner acknowledges support of a K01 award (K01HL130650). Dr. Park acknowledges support of a K01 award (K01ES026833). Dr. Kronish acknowledges support of an R01 award (R01HL132347).
Footnotes
Conflicts of Interest:
The authors have no relevant conflicts of interest to report.
References
- 1.Girotra S, Nallamothu B, Spertus J, Li Y, Krumholtz H, Chan P. Trends in survival after in-hospital cardiac arrest. New England Journal of Medicine 2012;367:1912–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moulaert V, Verbunt J, van Heugten C, Wade D. Cognitive impairments in survivors of out-of-hospital cardiac arrest: A systematic review. Resuscitation 2009;80:297–305. [DOI] [PubMed] [Google Scholar]
- 3.Wachelder EM, Moulaert VR, van Heugten C, Verbunt JA, Bekkers SC, Wade DT. Life after survival: long-term daily functioning and quality of life after an out-of-hospital arrest. Resuscitation 2009;80:517–22. [DOI] [PubMed] [Google Scholar]
- 4.Wilder Schaaf KP, Artman LK, Peberdy MA, Walker WC, Ornato JP, Gossip MR, Kreutzer JS. Anxiety, depression, and PTSD following cardiac arrest: A systematic review of the literature. Resuscitation 2013;84:873–7. [DOI] [PubMed] [Google Scholar]
- 5.Porter ME, Pabo EA, Lee TH. Redesigning primary care: A strategic vision to improve value by organizing around patients’ needs. Health Affairs 2013;32:516–23. [DOI] [PubMed] [Google Scholar]
- 6.Wasson JH, Stukel TA, Weiss JE, Hays RD, Jette AM, Nelson EC. A randomized trial of the use of patient self-assessment data to improve community practices. Effective Clinical Practice: ECP 1999;2:1–10. [PubMed] [Google Scholar]
- 7.Ahles TA, Wasson JW, Seville JL, et al. A controlled trial of methods for managing pain in primary care patients with or without co-occuring psychosocial problems. Annals of Family Medicine 2006;4:341–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steinbusch CVM, van Heugten CM, Rasguin SMC, Verbunt JA, Moulaert VRM. Cognitive impairments and subjective cognitive complaints after survival of cardiac arrest: A prospective longitudinal cohort study. Resuscitation 2017;120:132–7. [DOI] [PubMed] [Google Scholar]
- 9.Juan E, De Lucia M, Breaud V, et al. How do you feel? Subjective perception of recovery as a reliable surrogate of cognitive and functional outcome in cardiac arrest survivors. Critical Care Medicine 2018;46:e286–93. [DOI] [PubMed] [Google Scholar]
- 10.Duits A, Munnecom T, van Heugten C, van Oostenbrugge RJ. Cognitive complains in the early phase after stroke are not indicative of cognitive impairment. Journal of Neurology, Neurosurgery, and Psychiatry 2008;79:143–6. [DOI] [PubMed] [Google Scholar]
- 11.Zlatar ZZ, Moore RC, Palmer BW, Wesley KT, Jeste DV. Cognitive complaints correlate with depression rather than concurrent objective cognitive impairment in the successful aging evaluation baseline sample. Journal of Geriatric Psychiatry and Neurology 2014;27:181–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vilchinsky N, Ginzburg K, Fait K, Foa EB. Cardiac-disease-induced PTSD (CDI-PTSD): A systematic review. Clinical Psychology Review 2017;55:92–106. [DOI] [PubMed] [Google Scholar]
- 13.Celano CM, Huffman JC. Depression and cardiac disease: A review. Cardiology in Review 2011;19:130–42. [DOI] [PubMed] [Google Scholar]
- 14.Davidson KW. Depression and coronary heart disease. ISRN 2012;vol.2012:Article ID 743813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Presciutti A, Verma J, Pavol M, Anbarasan A, Falo C, Brodie D, Rabbani LE, Roh DJ, Park S, Claassen J, Agarwal S. Posttraumatic stress and depressive symptoms characterize cardiac arrest survivors’ perceived recovery at hospital discharge [published online ahead of print May 10, 2018]. General Hospital Psychiatry. doi: 10.1016/j.genhosppsych.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 16.Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Critical Care Medicine 2001;29:1370–9. [DOI] [PubMed] [Google Scholar]
- 17.Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. American Journal of Respiratory and Critical Care Medicine 2002;166:1338–44. [DOI] [PubMed] [Google Scholar]
- 18.Randolph C, Tierney M, Mohr E, et al. The repeatable battery for the assessment of neuropsychological status (RBANS): Preliminary clinical validity. Journal of Clinical and Experimental Neuropsychology 1998;20:310–9. [DOI] [PubMed] [Google Scholar]
- 19.Lewinsohn PM, Seeley JR, Roberts RE, et al. Center for Epidemiological Studies-Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging 1997;12:277–87. [DOI] [PubMed] [Google Scholar]
- 20.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checlist (PCL_: Reliability, validity, and diagnostic utility 1993. Paper presented at the 9th Annual Conference of the ISTSS, San Antonio. [Google Scholar]
- 21.Lawton MP, Brody EM. Assessment of older people: Self maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–86. [PubMed] [Google Scholar]
- 22.Brandt J, Spencer M, Folstein M. The Telephone Interview for Cognitive Status. Cognitive and Behavioral Neurology 1998;1:111–8. [Google Scholar]
- 23.Berge E, Fjærtoft H, Indredavik B, et al. Validity and reliability of simple questions in assessing short- and long-term outcome in Norwegian stroke patients. Cerebrovascular Diseases 2001;11:305–10. [DOI] [PubMed] [Google Scholar]
- 24.Celani MG, Cantisani TA, Righetti E, et al. Different measures for assessing stroke outcome: An analysis from the International Stroke Trial in Italy. Stroke 2002;33:218–23. [DOI] [PubMed] [Google Scholar]
- 25.Lindley RI, Waddell F, Livingstone M, et al. Can simple questions assess outcome after stroke? Cerebrovascular Diseases 1994;4:314–24. [Google Scholar]
- 26.Mckevitt C, Dundas R, Wolfe C. Two simple questions to assess outcome after stroke: A European study. Stroke 2001;32:681–6. [DOI] [PubMed] [Google Scholar]
- 27.The International Stroke Trial. A randomised trial of aspirin, subcutaneous heparin, both, or neither among 19,435 patients with acute ischaemic stroke. The Lancet 1997;349:1569–81. [PubMed] [Google Scholar]
- 28.Longstreth WT, Nichol G, Van Ottingham L, et al. Two simple questions to assess neurologic outcomes at three months after out-of-hospital cardiac arrest: Experience from the public access defibrillation trial. Resuscitation 2010;81:530–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Randolph C RBANS update. Bloomington, IL: PsychCorp; 2012. [Google Scholar]
- 30.Brandt J, Folstein M. Telephone Interview for Cognitive Status, Professional Manual. Lutz: Psychological Assessment Resources, Inc. [Google Scholar]
- 31.Mayer SA, Kreiter KT, Copeland D, et al. Global and domain-specific cognitive impairment and outcome after subarachnoid hemorrhage. Neurology 2002;59:1750–8. [DOI] [PubMed] [Google Scholar]
- 32.National Center for PTSD. Using the PTSD Checklist. National Center for PTSD website. http://www.ptsd.va.gov/professional/pages/assessments/ptsd-checklist.asp.Accessed August 15, 2012.
- 33.Charlson ME, Pompei P, Ales KL, MacKenzie RC. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases 1987;40:373–83. [DOI] [PubMed] [Google Scholar]
- 34.Roffman CE, Buchanan J, Allison GT. Charlson Comorbidities Index. Journal of Physiotherapy 2016;62:171. [DOI] [PubMed] [Google Scholar]
- 35.Bradley SM, Rumsfeld JS. Depression and cardiovascular disease. Trends in Cardiovascular Medicine 2015;25:614–22. [DOI] [PubMed] [Google Scholar]
- 36.Bush DE, Ziegelstein RC, Patel UV, et al. Post-myocardial infarction depression. Evidence Report/Technology Assessment 2005;123:1–8. [PMC free article] [PubMed] [Google Scholar]
- 37.Lilja G, Nilsson G, Nielsen N, et al. Anxiety and depression among out-of-hospital cardiac arrest survivors. Resuscitation 2015;97:68–75. [DOI] [PubMed] [Google Scholar]
- 38.Davidson KW, Burg MM, Kronish IM, et al. Association of anhedonia with recurrent major adverse cardiac events and mortality 1 year after acute coronary syndrome. Archives of General Psychiatry 2010;67:480–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kronish IM, Rieckmann N, Halm EA, et al. Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. J Gen Intern Med 2006;21:1178–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Agarwal S, Presciutti A, Roth W, Matthews E, Rodriguez A, Roh DJ, Park S, Claassen J, Lazar RM. Determinants of long-term neurological recovery patterns relative to hospital discharge among cardiac arrest survivors. Critical Care Medicine 2018;46:e141–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Edmondson D, Cohen BE. Posttraumatic stress disorder and cardiovascular disease. Prog Cardiovasc Dis 2013;55:548–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosellini AJ, Stein MB, Colpe LJ, et al. Approximating a DSM-5 diagnosis of PTSD using DSM-IV criteria. Depression and Anxiety 2016;32:493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.