Abstract
Objective
To determine frequencies and trends in sialoendoscopy and sialoadenectomy for the treatment of obstructive, non-neoplastic submandibular gland disease in the United States.
Methods
Epidemiologic study of insurance claims from 2006–2013 in a large, private insurance claims database. Rates were calculated for patients undergoing one or both index procedures.
Results
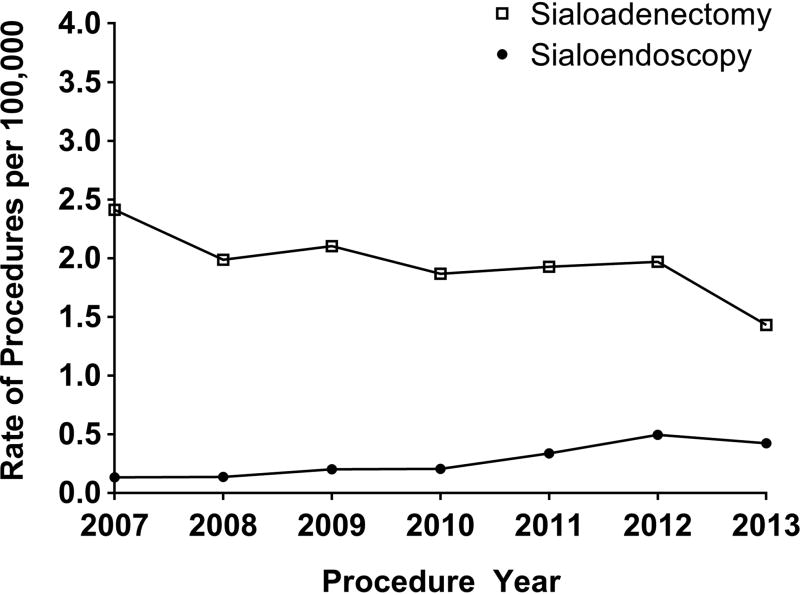
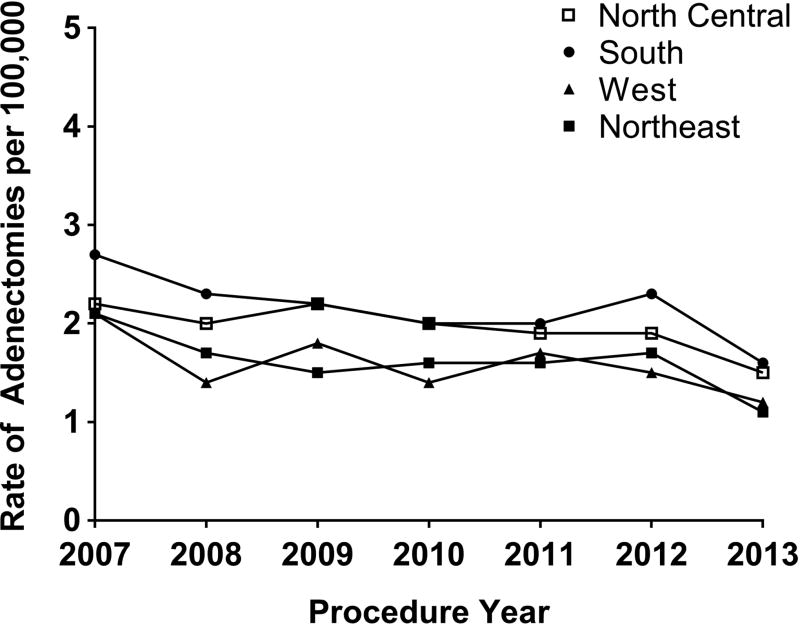
5,111 adults with sialadenitis who underwent sialoendoscopy or submandibular gland excision were included. Mean age was 47.6 years, and patients undergoing sialoendoscopy were less likely to be male (RR=0.84, 95% CI 0.78–0.89), more likely to have sialoadenitis without stones (RR=1.60, 95% CI 1.53–1.66) and had a similar number of comorbidities (RR=1.00, 95% CI 0.91–1.06) compared to patients undergoing sialoadenectomy. The most common complication after sialoadenectomy was surgical site infection (1.4%, 95% CI 1.1–1.8%), and complications after sialoendoscopy were rare. From 2007 to 2013, use of sialoendoscopy increased from 0.13 (95% CI 0.08–0.18) to 0.42 (95% CI 0.40–0.45) per 100,000 people, and sialoadenectomy decreased from 2.41 (95% CI 2.39–2.42) to 1.43 (95% CI 1.40–1.44) per 100,000. The highest mean rate of sialadenectomy was seen in the south (2.15 per 100,000, 95% CI 2.13–2.16), the lowest was in the west (1.6 per 100,000, 95% CI 1.57–1.62), and decreased in all regions over time.
Conclusion
Utilization of sialoendoscopy has increased over time, and the overall rate of sialoadenectomy is decreasing. Both procedures are safe for treatment of patients with sialadenitis and sialolithiasis. Future research should examine whether availability of sialoendoscopy leads to a decreased rate of sialoadenectomy in patients with salivary gland disease.
Keywords: Sialoendoscopy, sialendoscopy, sialadenitis, salivary gland diseases, epidemiology, health services research
INTRODUCTION
Introduced in 19901 and inspired by the treatment of kidney and gall bladder stones, sialoendoscopy has since been shown to be a safe and effective procedure for treatment of obstructive salivary gland disease.2,3 This minimally invasive method improves functional recovery of the salivary gland and may decrease the need for sialoadenectomy.4 The reported cure rates for sialolithiasis with sialoendoscopy range from 60 to 80 percent for stones of all sizes, and the success rate is higher with smaller stones, with one study showing 100% retrieval rate in stones less than 3 mm.5,6
Sialoendoscopy may be an improvement in the standard of care for patients with obstructive sialadenitis, by potentially allowing patients to avoid sialoadenectomy and improve salivary gland function. Barriers to adopting this technology include equipment cost, as well as the learning curve of a new technique.7–9 However, the rate of adoption of this technology is not well-documented.
Our hypothesis is that as sialoendoscopy rates increase, sialoadenectomy rates will decrease in patients with non-neoplastic obstructive sialadenitis. This hypothesis is supported by a large registry-based study from Denmark, which found a consistent decrease in the rate of submandibular gland removal with a corresponding increase in sialoendoscopy for benign, non-neoplastic salivary gland disease.10 In addition, sialoendoscopy volume, or simply availability of sialoendoscopy at a health care facility may potentially be used as a quality measure for the care of patients with salivary duct disease if this hypothesis proves true across a larger, more heterogeneous population. The goal of this study was to examine the rates of sialoendoscopy and sialoadenectomy in a large population, describe trends, and identify regional differences in the United States.
MATERIALS AND METHODS
We performed a retrospective observational study of privately insured persons who underwent sialoadenectomy or sialoendoscopy in the Truven Health MarketScan® Commercial Database (Truven Health Analytics, an IBM Company) from 2006 to 2013. MarketScan contains de-identified longitudinal medical and prescription drug claims for a large number of privately insured patients in the United States, including inpatient hospitalizations, emergency department, outpatient physician, and facility encounters. The database includes claims obtained primarily from large employers. The dataset was stored and managed by the Washington University Center for Administrative Data Research. This study was considered exempt by the Washington University Human Research Protection Office.
Inclusion and Exclusion Criteria
Patients eligible for inclusion were adults aged 18–64 years with International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) procedure or Current Procedural Terminology (CPT) codes for sialoadenectomy (ICD-9-CM codes 26.30–26.32 or CPT codes 42410, 42415, 42420, 42425, 42440) or sialoendoscopy (ICD-9-CM 26.99 or CPT 42699) during an inpatient hospitalization or ambulatory encounter from 7/1/2006 to 11/30/2013, with at least 180 days prior continuous health insurance enrollment. We required a diagnosis of sialolithiasis (ICD-9-CM diagnosis code 527.5) or sialoadenitis (527.2) within 180 days before the procedure to ensure appropriate capture of patients undergoing sialoendoscopy for obstructive salivary gland disease, as the CPT code typically used for sialoendoscopy is unlisted (42699 = Other Procedures on the Salivary Gland and Ducts). This requirement was also applied to sialoadenectomy codes to avoid inclusion of patients undergoing surgery for neoplastic disease. In addition, to exclude patients undergoing procedures for cancer, we excluded patients undergoing either sialoendoscopy or sialoadenectomy for neoplasm (ICD-9-CM diagnosis code 235.0, 142.0–142.9, and 210.2 coded on the day of surgery).
Identifying Patients Undergoing Salivary Gland Procedures
We developed an algorithm to determine most likely procedures dates, due to instances of repeated coding in the MarketScan database. We prioritized procedure dates with matching facility and provider claims for operation. If sialoadenectomy or sialoendoscopy were coded by a provider or a facility only, additional information was used to increase the likelihood that the procedure was performed, including Uniform Billing (UB-04) coding for operating room services (0360, 0361, 0490) and CPT codes for anesthesia for salivary gland, intraoral, or head and neck procedures (00100, 00170, 00300, 00320). In addition, if there was both provider and facility coding for the procedures but the dates did not match, the dates were compared to UB-04 operating room services and anesthesia dates, if available, to determine the most likely date of procedure. Procedures coded on a single line by a facility or provider with no other services coded on that date were excluded.
Baseline clinical characteristics were identified using ICD-9-CM diagnosis, CPT, and Healthcare Common Procedure Coding System (HCPCS) codes within 180 days through the date of operation, including oral cancer (ICD-9-CM 145.0, 145.6, 145.8, and 145.9), radioactive iodine exposure (CPT 79005, HCPCS A9517, A9530), history of radiotherapy (V58.0), Sjögren’s syndrome (ICD-9-CM 710.2), thyroid cancer (ICD-9-CM 193, V10.87), and clotting disorder (ICD-9-CM 286.9). Comorbidities were identified as defined by Elixhauser, using ICD-9-CM diagnosis codes on claims during the 180 days before the first sialoadenectomy or sialoendoscopy date.11,12 The algorithm to identify the Elixhauser comorbidities was performed as described by Klabunde et al., requiring either coding on one inpatient facility claim or at least 2 outpatient/provider claims spaced at least 30 days apart.13
Postoperative complications were identified within 30 days of operation by ICD-9-CM diagnosis codes, including hematoma (998.12), facial nerve injury (951.4), xerostomia (527.7), and surgical site infection (998.5, 998.51, 998.59). Since patients could have more than one procedure, we identified all unique dates coded for sialoadenectomy or sialoendoscopy. The observation time for complications was censored at the time of a subsequent procedure that occurred within 30 days of the prior procedure.
Statistical Analysis
We used descriptive statistics to describe the study population, as well as distribution of demographic and clinical characteristics. Denominators were obtained by using the entire population adults aged 18–64 years in the MarketScan database with at least 6 months’ continuous health insurance enrollment to calculate the rates of procedures over time and in regions of the United States. Because data from 2006 were only available for the latter half of the year, only rates from 2007–2013 were examined for trend analysis. 95% confidence intervals were calculated to display precision of the data. Risk ratios were used to estimate relative risk. SAS Enterprise Guide version 7.1 (Cary, NC) was used to perform the analysis.
RESULTS
We identified 5,111 patients with a diagnosis of sialadenitis, sialolithiasis, or both, who underwent either sialoendoscopy or sialoadenectomy from July 1, 2006 to November 30, 2013. The mean age of all patients was 47.6 years, and patients undergoing sialoendoscopy were less likely to be male (RR=0.84, 95% CI 0.78–0.89), more likely to have a diagnosis of sialolithiasis (RR=1.60, 95% CI 1.53–1.66), and had a similar number of comorbidities (RR=1.00, 95% CI 0.89–1.09) compared to patients undergoing sialoadenectomy. In addition, patients undergoing sialoendoscopy were more likely to have had prior thyroid cancer (RR=4.8, 95% CI 4.8–5.1) or Sjogren’s disease (RR=3.2, 95% CI 2.5–3.5) (Table 1). Of the 641 patients who first underwent a sialoendoscopy, 106 (16.5%) were converted to a sialoadenectomy on the same visit, and an additional 23 (3.6%) subsequently underwent a sialoadenectomy at a later date. In total, 129 patients (20.1%) who had an initial sialoendoscopy subsequently had a sialoadenectomy.
Table 1.
Baseline characteristics of patients undergoing sialoendoscopy or sialoadenectomy.
| All patients N=5,111 patients |
Sialoadenectomy* N=4,470 patients |
Sialoendoscopy* N=641 patients |
Risk Ratio | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | RR | 95% CI | |
|
|
|||||||||||
| Mean age, yrs | 47.6 | - | 47.3–47.9 | 47.9 | - | 47.6–48.3 | 45.5 | - | 44.6–46.5 | 0.95 | 0.94–0.97 |
| Male sex | 2,295 | 44.9 | 43.6–46.3 | 2,048 | 45.8 | 44.4–47.3 | 247 | 38.6 | 34.8–42.3 | 0.84 | 0.78–0.89 |
| Diagnosis | |||||||||||
| Sialadenitis | 4,149 | 81.2 | 80.1–82.3 | 3,729 | 83.4 | 82.3–84.5 | 420 | 65.5 | 61.8–69.2 | 0.79 | 0.75–0.82 |
| Sialolithiasis | 1,459 | 28.5 | 27.3–29.8 | 1,187 | 26.6 | 25.3–27.9 | 272 | 42.4 | 38.6–46.3 | 1.60 | 1.53–1.66 |
| Both | 497 | 9.7 | 8.9–10.5 | 446 | 10.0 | 9.1–10.9 | 51 | 8.0 | 5.9–10.1 | 0.80 | 0.65–0.93 |
| Prior existing diagnosis | |||||||||||
| Sjogren’s | 82 | 1.6 | 1.3–1.9 | 56 | 1.3 | 1.0–1.6 | 26 | 4.1 | 2.5–5.6 | 3.2 | 2.5–3.5 |
| Thyroid cancer | 105 | 2.1 | 1.7–2.4 | 62 | 1.4 | 1.0–1.7 | 43 | 6.7 | 4.8–8.7 | 4.8 | 4.8–5.1 |
| Oral cancer | 7 | 0.1 | 0.0–0.2 | 7 | 0.2 | 0.0–0.3 | 0 | 0.0 | - | - | |
| Elixhauser comorbidities, mean | 0.47 | - | 0.45–0.49 | 0.47 | - | 0.45–0.50 | 0.47 | - | 0.41–0.53 | 1.00 | 0.91–1.06 |
| Procedure setting** | |||||||||||
| Outpatient | 4,739 | 92.7 | 92.0–93.4 | 4,106 | 91.7 | 91.1–92.7 | 633 | 98.8 | 97.9–99.6 | 1.08 | 1.08–1.08 |
As index procedure.
Patients with more than one procedure with at least one inpatient procedure were counted as inpatient.
We identified 105 total complications in 5,111 patients (2.1%). 102 of 105 complications (97.1%) occurred after sialoadenectomy. The most common complication after sialoadenectomy was surgical site infection (1.4%, 95% CI 1.1–1.6%), and the second most common was hematoma (0.8%, 95% CI 0.5–1.0%) (Table 2).
Table 2.
Complications from sialoendoscopy and sialoadenectomy procedures in adults from 2006–2013.
| Sialoendoscopy (n=641) |
Sialoadenectomy* (n=4,469) |
|||||
|---|---|---|---|---|---|---|
| n | % | 95% CI | n | % | 95% CI | |
|
|
||||||
| Complications | ||||||
| Surgical site infection | 1 | 0.2 | 0.0–0.5 | 64 | 1.4 | 1.1–1.8 |
| Hematoma | 1 | 0.2 | 0.0–0.5 | 35 | 0.8 | 0.5–1.0 |
| Facial weakness | 1 | 0.2 | 0.0–0.5 | 3 | 0.1 | 0.0–0.1 |
Sialoendoscopy converted to sialoadenectomy or sialoendoscopy-assisted sialoadenectomy counted as sialoadenectomy.
The rate of sialoendoscopy increased over time, rising from 0.13 (95% CI 0.08–0.18) per 100,000 people in 2007 to 0.42 (95% CI 0.40–0.45) per 100,000 in 2013. In parallel, the rate of sialoadenectomy decreased in the same time period, from 2.41 (95% CI 2.39–2.42) per 100,000 in 2007 to 1.43 (95% CI 1.40–1.44) per 100,000 in 2013 (Figure 1). The highest mean rate of sialoadenectomy over this time period occurred in the southern region of the United States (2.15 per 100,000, 95% CI 2.13–2.16), and the lowest was in the western region (1.59 per 100,000, 95% CI 1.57–1.62) although the rate decreased in all regions throughout the study period (Figure 2).
Figure 1.
Rate of sialoendoscopies and sialoadenectomies from 2007 – 2013 in the MarketScan database.
Figure 2.
Rate of sialoadenectomies over time stratified by US region, 2007 – 2013.
DISCUSSION
In this epidemiologic study of over 5,000 adults in a U.S. private insurance claims database we found that the rates of sialoendoscopy remain low, though utilization has increased slightly over time. The rates of sialoendoscopy and sialoadenectomy varied throughout regions of the country, but trended in the same direction. Patients who underwent sialoendoscopy were more likely to be female, were more likely to have the procedure as an outpatient, and had a similar number of comorbidities as compared to patients who underwent sialoadenectomy. In addition, patients undergoing sialoendoscopy were more likely to have a diagnosis of Sjogren’s or thyroid cancer as compared to patients undergoing sialoadenectomy. Patients with a diagnosis of sialolithiasis were more likely to undergo sialoendoscopy as compared to patients with sialadenitis, as we expected. The most common complication was surgical site infection after sialoadenectomy, with an overall complication rate less than 2%, consistent with other recent studies.5,8,14,15 Complications of sialoendoscopy were too rare to report.
We were unable to provide evidence for or against our main hypothesis: that rates of sialoadenectomy and other secondary outcomes decrease when sialoendoscopy rates increase. The hypothesized trend is consistent with prior work, however, showing that the use of sialoendoscopy may prevent subsequent sialoadenectomy. In Denmark, the increasing use of sialoendoscopy is believed to have directly led to a decreased rate of sialoadenectomy.4,10 Rasmussen et al. also noted regional variation among rates of sialoadenectomy in Denmark.10
Limitations
A limitation of our study is that the data source is administrative claims, which are not designed for research purposes.16 Thus we were limited to the data fields supplied for billing purposes. Because of this, we are not able to determine other events that were not coded as complications and clinical details, including how often endoscopy was aborted due to failure to cannulate the duct, and how many stones were identified but unable to be removed endoscopically, for example. In other studies, reported rates of unsuccessful cannulation ranged from 6–10%, and inability to extract visualized stones ranged from 3–5%.15,17 It is also possible that certain complications were underreported, including facial weakness due to injury to the marginal mandibular nerve. However, we believe that these data allow for an accurate representation of the usage of sialoendoscopy in this patient population, due to the need for appropriate reimbursement to the physician and facility. In the situation where a sialoendoscopy may not be expected to be successful, the patient should be counseled that endoscopy may be attempted, followed by a sialoadenectomy if unsuccessful.
Another limitation of this study is that because sialoendoscopy has an unlisted CPT code in the US, identifying procedures was not straightforward. Due to the fragmented nature of health care delivery in the U.S., use of claims data is the only feasible way to look at utilization of procedures from a population perspective. We identified unlisted procedures within 180 days of a diagnosis of sialadenitis, sialolithiasis, or both, which likely represented sialoendoscopies. We used a complex algorithm including coding for operating room services, administration of anesthesia for salivary gland, oral, or head and neck procedures and matched coding from facilities and providers to increase the accuracy of identification of sialoendoscopy and sialoadenectomy. Given the lack of clinical detail, we were unable to definitively verify the procedure type. However, our rates are consistent with other published literature describing the use of sialoendoscopy and sialadenectomy at other academic centers.14,15,17
Future Research
Future studies could examine whether availability of sialoendoscopy could be utilized as a quality measure for the treatment of patients with salivary gland disorders, as having the option to perform a sialoendoscopy may allow gland preservation by obviating the need for sialoadenectomy. In addition, barriers to incorporating sialoendoscopy into practice should be examined, as the procedure is a safe, low-risk intervention.2
CONCLUSION
Utilization of sialoendoscopy has increased over time, and the overall rate of sialoadenectomy is decreasing in the United States. Both procedures are safe for the treatment of patients with sialadenitis and sialolithiasis. Future research should examine whether the availability of sialoendoscopy leads to a decrease in the rate of sialoadenectomy in patients with salivary gland disease.
Acknowledgments
Financial Support: This work was supported by the Ruth L. Kirschstein National Research Service Award (NRSA) Institutional Research Training Grant (T32DC000022) from the National Institute on Deafness and Other Communication Disorders (NIDCD) of the National Institutes of Health (NIH), the Washington University Institute of Clinical and Translational Sciences grant (UL1TR000448) from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH), a grant (R24 HS19455) from the Agency for Healthcare Research and Quality (AHRQ), and a grant (KM1CA156708) from the National Cancer Institute (NCI) at the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH.
References
- 1.Konigsberger R, Feyh J, Goetz A, Schilling V, Kastenbauer E. Endoscopic controlled laser lithotripsy in the treatment of sialolithiasis. Laryngorhinootologie. 1990;69:322–323. doi: 10.1055/s-2007-998200. [DOI] [PubMed] [Google Scholar]
- 2.Marchal F, Dulguerov P. Sialolithiasis management: the state of the art. Arch Otolaryngol Head Neck Surg. 2003;129:951–956. doi: 10.1001/archotol.129.9.951. [DOI] [PubMed] [Google Scholar]
- 3.Strychowsky JE, Sommer DD, Gupta MK, Cohen N, Nahlieli O. Sialendoscopy for the Management of Obstructive Salivary Gland Disease. Arch Otolaryngol Head Neck Surg. 2012;138:541–547. doi: 10.1001/archoto.2012.856. [DOI] [PubMed] [Google Scholar]
- 4.McGurk M, Escudier MP, Brown JE. Modern management of salivary calculi. Br J Surg. 2005;92:107–112. doi: 10.1002/bjs.4789. [DOI] [PubMed] [Google Scholar]
- 5.Phillips J, Withrow K. Outcomes of Holmium Laser-Assisted Lithotripsy with Sialendoscopy in Treatment of Sialolithiasis. Otolaryngol Head Neck Surg. 2014;150:962–967. doi: 10.1177/0194599814524716. [DOI] [PubMed] [Google Scholar]
- 6.Luers JC, Grosheva M, Stenner M, Beutner D. Sialoendoscopy: prognostic factors for endoscopic removal of salivary stones. Arch Otolaryngol Head Neck Surg. 2011;137:325–329. doi: 10.1001/archoto.2010.238. [DOI] [PubMed] [Google Scholar]
- 7.Maresh A, Kutler DI, Kacker A. Sialoendoscopy in the diagnosis and management of obstructive sialadenitis. Laryngoscope. 2011;121:495–500. doi: 10.1002/lary.21378. [DOI] [PubMed] [Google Scholar]
- 8.Nahlieli O, Baruchin AM. Long-term experience with endoscopic diagnosis and treatment of salivary gland inflammatory diseases. Laryngoscope. 2000;110:988–993. doi: 10.1097/00005537-200006000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Walvekar RR, Razfar A, Carrau RL, Schaitkin B. Sialendoscopy and Associated Complications: A Preliminary Experience. Laryngoscope. 2008;118:776–779. doi: 10.1097/MLG.0b013e318165e355. [DOI] [PubMed] [Google Scholar]
- 10.Rasmussen ER, Lykke E, Wagner N, Nielsen T, Waersted S, Arndal H. The introduction of sialendoscopy has significantly contributed to a decreased number of excised salivary glands in Denmark. Eur Arch Otorhinolaryngol. 2016;273:2223–2230. doi: 10.1007/s00405-015-3755-x. [DOI] [PubMed] [Google Scholar]
- 11.Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP) [Accessed January 26 2016];HCUP comorbidity software, Version 3.7. Available at: http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp.
- 12.Elixhauser A, Steiner C, Harris DR, Coffey RN. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 14.Cordesmeyer R, Winterhoff J, Kauffmann P, Laskawi R. Sialoendoscopy as a diagnostic and therapeutic option for obstructive diseases of the large salivary glands-a retrospective analysis. Clin Oral Investig. 2016;20:1065–1070. doi: 10.1007/s00784-015-1588-z. [DOI] [PubMed] [Google Scholar]
- 15.Pace CG, Hwang KG, Papadaki M, Troulis MJ. Interventional sialoendoscopy for treatment of obstructive sialadenitis. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2014;72:2157–2166. doi: 10.1016/j.joms.2014.06.438. [DOI] [PubMed] [Google Scholar]
- 16.Tyree PT, Lind BK, Lafferty WE. Challenges of Using Medical Insurance Claims Data for Utilization Analysis. American journal of medical quality : the official journal of the American College of Medical Quality. 2006;21:269–275. doi: 10.1177/1062860606288774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Achim V, Light TJ, Andersen PE. Gland Preservation in Patients Undergoing Sialoendoscopy. Otolaryngol Head Neck Surg. 2017;157:53–57. doi: 10.1177/0194599817695547. [DOI] [PubMed] [Google Scholar]