Abstract
Methamphetamine use has increased significantly in Southeast Asia in the last 5-10 years, but there is little research on risk behaviors associated with the increase in this region. We evaluate injection and sexual risk behaviors associated with current methamphetamine use among heterosexual persons who inject drugs (PWID) in Hai Phong Vietnam. We recruited 1336 PWID and assessed associations between methamphetamine use, injection and sexual risk behaviors, stratified by HIV serostatus. There were several statistically significant associations between methamphetamine use and sexual risk behaviors among HIV positive PWID, but we did not find any associations between methamphetamine use and injection risk behaviors. Methamphetamine may increase the likelihood of PWID transmitting HIV to non-injecting primary sexual partners as it can reduce ART adherence and can lead to weakening of the immune system and increased HIV viral loads. All participants were injecting heroin, and methamphetamine use may interfere with opiate use treatment. Public health efforts should focus on the large increase in methamphetamine use and the associated sexual risk behaviors. Emphasis on sexual risk behavior, particularly among those that are HIV positive, in conjunction with continued monitoring of ART adherence and HIV viral loads is critical.
Keywords: Methamphetamine, HIV, HCV, Sex risk behavior, Persons who inject drugs
Methamphetamine use has increased globally and has been recognized by the World Health Organization (WHO) as a global health problem (World Health Organization 2006). Recent reports indicate Southeast Asia has seen the highest increases in methamphetamine use, with a fourfold increase from 2009 to 2014, and is responsible for 60% of amphetamine type stimulant (ATS) use in the world (United Nations Office on Drugs and Crime 2016). In Vietnam, methamphetamine use has paralleled this increase, with increases seen not only among young drug users in major cities, but also industrialized areas, villages and communities (UNODC 2017).
The use of methamphetamine has often but not always been associated with increased sexual risk behaviors including having multiple partners, having sex under the influence of drugs, trading sex for money/drugs, and unprotected sexual intercourse (Chettiar et al. 2010; Garofalo et al. 2007; Russell et al. 2008). The inconsistency in associations is likely related to the different samples of participants (including men who have sex with men and female sex workers), route of administration of methamphetamine, and measurements in methamphetamine use in relation to sexual behaviors. Methamphetamine has also been associated with injection risk behaviors among persons who inject drugs (PWID) including sharing of needles/syringes and injection equipment (Molitor et al. 1999).
Methamphetamine has the potential to biologically facilitate Hepatitis C (HCV) replication (Cherner et al. 2005; Ye et al. 2008). Among HIV positive PWID methamphetamine can lead to increased viral replication, lower levels of ART adherence (Reback, Larkins & Shoptaw 2003), weakened immune systems (Salamanca et al. 2015), and decreased effectiveness of antiretroviral therapy (ART) (Ellis et al. 2003).
There are few studies on heterosexual methamphetamine users in Southeast Asia, with most studies focusing on the United States and samples that predominately include men who have sex with men (MSM). Additionally, a recent meta-analysis that aggregated studies evaluating sexual risk behaviors among methamphetamine using heterosexual populations did not include any studies in Asia (Hittner 2016).
Hai Phong, Vietnam, is a city of approximately two million people of whom approximately 5000 inject drugs. Heroin is the primary drug of injection in Vietnam. During the initial pilot of the Drug use and blood-borne Infections in Vietnam (DRIVE-IN) study, methamphetamine use among PWID was approximately 30%, but has increased to over 50% in 2016, with over 97% of methamphetamine users smoking methamphetamine. The HIV epidemic among PWID has been well documented with high HIV prevalence beginning in the 1990s. In 2005 approximately 66% of PWID in Hai Phong were infected with HIV, decreasing to approximately 48% in 2009 (Des Jarlais et al. 2016; National Institute of Hygiene and Epidemiology 2011). In 2014, HIV prevalence was 25% and estimated HIV incidence among new injectors (persons injecting < 5 years) was 1/100 person-years at risk.
The ongoing spread of methamphetamine use in Southeast Asia in the last 5-10 years raises the question of how methamphetamine could affect sexual risk among PWID with dual heroin/methamphetamine use. In this study, we assess the associations between methamphetamine use and sexual and injection risk behaviors among a population of PWID in Hai Phong Vietnam.
Methods
Participant Recruitment
Study participants were recruited in Hai Phong, Vietnam, in 2016-2017. The participants were recruited using both respondent driven sampling (RDS) (Heckathorn, 1997; Heckathorn et al., 2002) and select peer recruitment (Latkin, 1998); we aimed for a diverse group of participants with different ages, genders, and HIV serostatus.
Participants were eligible if they were 18 years or older and capable of giving informed consent. Current injecting drug use was verified through examination of injection marks and urinalysis (participants had to be positive for heroin or methamphetamine).
Interview and HIV/HCV Testing
After eligibility was confirmed, informed consent was obtained and a structured questionnaire was administered by a trained interviewer. The questionnaire examined demographic factors in addition to drug and alcohol use, sexual and injection risk behaviors (in the previous six months), mental health, and participation in harm reduction and treatment programs.
Each participant received counseling and testing for HIV and HCV. HIV antibody and HCV antibody testing were conducted at the laboratory of the Hai Phong Provincial AIDS Committee, using commercially available assays. HIV testing relied on Determine™ HIV-1/2 (Alere™, Waltham, USA) rapid test. HIV confirmation was done using Bioline HIV1/2 3.0 rapid test (Standard Diagnostics Inc., Gyeonggi-do, Republic of Korea) plus the VIKIA® HIV1/2 (Marcy l’étoile, Lyon, France). HCV serology was done using SD Bioline HCV rapid test (Standard Diagnostics Inc., Gyeonggi-do, Republic of Korea).
Participants were compensated VND 150,000 (approximately US $7.50) plus VND 50,000 (approximately USD $2.50) for each PWID they successfully recruited, and received an additional VND 50,000 for transportation to return to the study site for HIV and HCV test results.
Methamphetamine Use and Associated Variables
Current methamphetamine use was defined as self-reported methamphetamine use at least one time in the last thirty days. Unsafe sex was defined as having vaginal or anal intercourse without using a condom anytime in the last six months (as we wanted to capture any unsafe risk among participants with respect to condom use, regardless of how often condoms were used with partners). Primary partners were defined as someone the participants had sex with and had an emotional attachment for at least last 6 months, including husband/wife, boyfriend/girlfriend or lover. Casual partners were defined as someone the participants had sexual relations with other than their primary partner, excluding commercial sex encounters. We did ask about number of partners among causal partner encounters among the PWID. However, because most admitted to only one casual partner, we did not perform analysis based on number of casual partners. We did not ask participants about partner serostatus. Questions on injection risk behaviors, including receptive and distributive sharing, were based on the last six months prior to the interview. There were a small number of participants that identified as men-who-have-sex-with-men (MSM), and as we wanted to focus on heterosexual risk behaviors, they were removed from the sample before performing statistical analysis. We also removed PWID from the analysis that self-reported not using methamphetamine in the last 30 days, but had positive urine toxicology for methamphetamine. For self-report responses in the questionnaire, we had approximately 0.2% missing data among the participants included in the analysis.
Statistical Analysis
We used bivariate analyses (with chi square testing) to assess the association of demographics, drug use (including current methamphetamine use), sexual and injection risk behaviors, stratifying PWID by HIV serostatus. The analysis stratified by HIV serostatus was conducted because it has been shown that those who know their HIV status are more likely to alter their risk behaviors including injection and sexual risk behaviors (Colfax et al. 2002). Multivariable models were tested separately for each HIV stratum examining associations between methamphetamine, injection and sexual risk behaviors and included variables that were statisticially significant in the bivariate tables when stratified by HIV serostatus (at the p<0.05 level). Backwards elimination was used to construct the final multivariable models.
Stata software version 14 (STATA Corp 2017) was used for statistical analyses. The study was approved by the Hai Phong Medical University and Pharmacy and Icahn School of Medicine at Mount Sinai Institutional Review Boards.
Results
We recruited 1,488 participants from October 2016 through the third week of January 2017. Recruitment was most rapid in the first few weeks. Increased police surveillance of drug user congregation sites (“hotspots”), led to lower recruitment numbers in the last two-thirds of the study period. Of the 1,488 that were recruited, 1,385 (93%) were eligible to participate in the study. The main reasons that potential participants were not eligible were lack of recent heroin/methamphetamine use (urinalyses negative), or that the participant did not consent to blood drawing for HIV/HCV testing.
Demographics and Drug Use Characteristics of PWID
A total of 1,336 participants (after excluding PWID who identified as men who have sex with men (MSM), N=20 and those who self-reported not using methamphetamine but tested positive in urinalysis, N=29) were included in the current analyses. Table 1 presents information on demographic factors of these 1336 PWID. The participants were predominately male (94%), the median age was 39 (SD 9) and almost all were injecting heroin, with 80% reporting daily heroin injection. HIV prevalence was 30% and HCV prevalence was 71%.
Table 1.
Demographic and Behavioral Characteristics among PWID in Hai Phong, Vietnam, 2016
| N (%) | |
|---|---|
| Total Sample | 1336 (100) |
| Gender | |
| Male | 1247 (94) |
| Female | 83 (6) |
| Married | 460 (35) |
| Median Age (SD) | 39 (9) |
| Drug Use Characteristics | |
| Heroin Use (in last 30 days) | 1331 (~100) |
| Daily Heroin Injection | 1068 (80) |
| Current Methamphetamine (last 30 days) | 678 (51) |
| Mean Days Using Methamphetamine (in last 30 days) (SD) | 7 (9) |
| Injected Methamphetamine+ | 22 (2) |
| Street Methadone* | 496 (37) |
| Cannabis* | 426 (32) |
| Overdose* | 47 (4) |
| Distributive Sharing of needle/syringe+ | 54 (4) |
| Receptive Sharing of needle/syringe+ | 68 (5) |
| Acquired 30-60 new needles/month | 628 (47) |
| Acquired more than 60 new needles/month | 445 (33) |
| Sexual Risk Behaviors* | |
| Sexually Active | 734 (55) |
| Unsafe Sex (any) | 517/734 (70) |
| Multiple Sex Partners | 76/734 (10) |
| Unsafe Sex with Primary Partner | 474/598 (79) |
| Unsafe Sex with Casual Partner | 36/62 (58) |
| HIV/HCV serostatus | |
| HIV Seropositive | 398 (30) |
| HCV Seropositive# | 941 (71) |
last six months
Any history of use
SD Bioline HCV rapid test
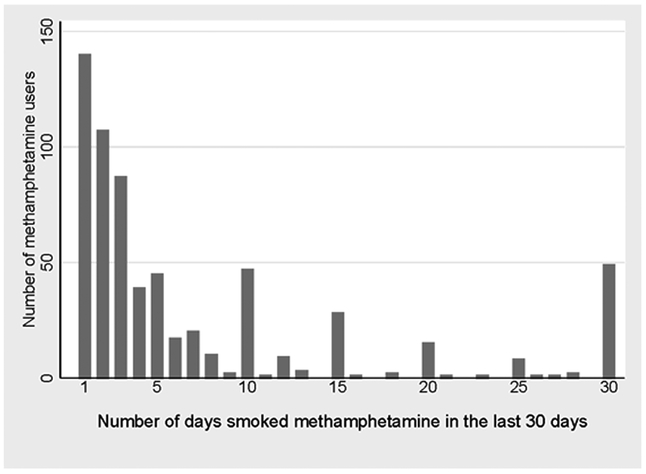
The total number of participants with current methamphetamine use (defined as using at least once in the last thirty days by self-report) was 678 (51%); the average number of days in the last thirty days using methamphetamine was 7 days (SD 9); less than 2% of users reported ever injecting methamphetamine. Figure 1 presents a distribution of the number of days using methamphetamine among those that self-reported current methamphetamine use. The distribution of days using methamphetamine was bimodal, with a high percentage of PWID reporting less than 5 days of use, and a high percentage reporting 25 or more days of use in the last 30 days.
Figure 1.
Distribution of the number of days using methamphetamine among those who self-reported current methamphetamine use.
Injection and Sexual Risk Behaviors
Among all participants, 734 (55%) were sexually active. Of those, 517 (70%) reported unsafe sex and 76 (10%) reported multiple sex partners. Of those with primary partners (n=598), 474 (79%) reported unsafe sex with their primary partners, and among those with casual partners (n=62), 36 (58%) reported unsafe sex with their casual partners.
Injection risk behaviors were low among PWID. Only 54 (4%) reporting distributive sharing and only 68 (5%) reporting receptive sharing. There were high rates of new needle/syringe acquisition, as 628 (47%) reported that they acquired between 30 and 60 sterile needles/syringes per month, and 445 (33%) reported that they acquired 60 or more sterile needles/syringes per month.
Characteristics of PWID by HIV Serostatus
Table 2 presents demographic, drug, injection and sexual risk behaviors stratified by HIV serostatus. Among the 398 HIV positive PWID, 164 (41%) were current methamphetamine users and among the 933 HIV negative PWID, 511 (55%) were current methamphetamine users.
Table 2.
Demographic and Behavioral Characteristics among PWID by HIV Serostatus in Hai Phong, Vietnam, 2016
| HIV Positive (n=398) |
HIV Negative (n=933) |
p value# | |
|---|---|---|---|
| Gender | |||
| Male | 374 (94) | 871 (94) | |
| Female | 22 (6) | 60 (6) | 0.820 |
| Married | 125 (31) | 329 (35) | 0.007 |
| Median Age (SD) | 40 (6) | 39 (9) | 0.09 |
| Drug Use Characteristics | |||
| Daily Heroin Injection | 325 (82) | 741 (79) | 0.307 |
| Current Methamphetamine (last 30 days) | 164 (41) | 511 (55) | <0.001 |
| Injected Methamphetamine | 3 (1) | 18 (2) | 0.116 |
| Street methadone+ | 156 (39) | 339 (36) | 0.320 |
| Cannabis+ | 239 (60) | 185 (20) | <0.001 |
| Overdose+ | 11 (3) | 35 (4) | 0.371 |
| Acquiring new needles/month | 0.042 | ||
| Between 30 and 60 new needles/month | 190 (48) | 438 (47) | |
| More than 60 new needles/month | 114 (29) | 330 (35) | |
| Distributive Sharing of needle/syringe+ | 21 (5) | 32 (3) | 0.113 |
| Receptive Sharing of needle/syringe+ | 22 (6) | 46 (5) | 0.643 |
| Sexual Risk Behaviors+ | |||
| Sexually Active | 197 (50) | 535 (57) | 0.008 |
| Unsafe Sex (any) | 94/197 (48) | 421/535 (79) | <0.001 |
| Multiple Sex Partners | 14/197 (7) | 62/535 (12) | 0.078 |
| Unsafe Sex with Primary Sex Partner | 80/147 (54) | 393/450 (87) | <0.001 |
| Unsafe Sex with Casual Sex Partner | 5/16 (31) | 31/46 (67) | 0.012 |
Current use was defined as methamphetamine use in last 30 days by self-report
Self-reported behaviors in the last six months
Chi-square test
There were significant differences in sexual risk behaviors in the previous six months when stratified by HIV serostatus. Compared to HIV positive PWID, HIV negative PWID were more likely to report being sexually active (57% vs 50%, p=0.008) and to report any unsafe sex (79% vs. 48%, p<0.001). HIV negative PWID were more likely to report unsafe sex with their primary partners (87% vs 54%, p<0.001) and with casual partners (67% vs 31%, p=0.012) compared to HIV positive PWID.
We observed no differences by HIV status for gender, or for distributive or receptive needle sharing. However HIV positives were slightly older (40 vs. 39 years of age; p<0.09), cannabis use was higher among HIV positive (60%) vs HIV negative PWID (20%) (p<0.001), and those that were HIV negative were more likely to acquire more than 60 needles/per month (35%) compared to those that were HIV positive (29%) (p=0.042).
Multivariable Analysis of Sexual and Injection Risk Behaviors
In order to assess the relationship between current methamphetamine use and sexual risk behaviors, we performed multivariable logistic regression, stratified by HIV serostatus, controlling for demographic factors and other drug use (Table 3). We stratified the PWID by HIV serostatus as it has been shown that those who know their HIV status are more likely to alter particular behaviors including sexual risk behaviors (Colfax et al. 2002). Among those who were HIV positive, current methamphetamine use was associated with self-reporting any unsafe sex (AOR 2.30, 95% CI: 1.20–4.42) and self-reporting unsafe sex with primary partners (AOR 2.43, 95% CI: 1.15–5.10). Several other variables were associated with unsafe sexual behaviors among those that were HIV positive. Being female was strongly associated with self-reporting any unsafe sex (AOR 10.57, 95% CI: 2.14–52.35) and self-reporting unsafe sex with primary partners (AOR 16.53, 95% CI: 1.91–143.27). Being married was associated with any unsafe sex (AOR 1.26, 95% CI: 1.06 –1.51). Having health insurance was negatively associated with any unsafe sex (AOR 0.42, 95% CI: 0.22 –0.80) and unsafe sex with primary partners (AOR 0.43, 95% CI: 0.20–0.94).
Table 3.
Logistic Regression of Sexual Risk Behaviors among PWID by HIV Serostatus in Hai Phong, Vietnam, 2016
| HIV Positive | HIV Negative | |||||
|---|---|---|---|---|---|---|
| Unsafe Sex*+
(Any) (N= 196) |
Unsafe Sex*+
(Primary Partner) (N= 146) |
Multiple Sex Partners*+ (N= 196) |
Unsafe Sex*+
(Any) (N= 543) |
Unsafe Sex*+
(Primary Partner) (N= 457) |
Multiple Sex Partners*+ (N= 543) |
|
| AOR (95% CI) | ||||||
| Current Methamphetamine Use (last 30 days) | 2.30 (1.20 – 4.42) | 2.43 (1.15 – 5.10) | 2.08 (0.63 – 6.90) | 1.06 (0.68 – 1.65) | 1.21 (0.68 – 2.16) | 1.43 (0.78 – 2.60) |
| Age | 1.03 (0.98 –1.08) | 1.03 (0.97 – 1.09) | 0.98 (0.89 – 1.08) | 1.00 (0.97 – 1.02) | 1.00 (0.97 – 1.03) | 0.99 (0.96 – 1.03) |
| Female Gender | 10.57 (2.14 – 52.35) | 16.53 (1.91 – 143.27) | 2.14 (0.39 – 11.88) | 1.03 (0.46 – 2.28) | 0.95 (0.31 – 2.89) | 0.59 (0.17 –2.05) |
| Married | 1.26 (1.06 – 1.51) | 1.09 (0.86 – 1.39) | 0.85 (0.62 – 1.17) | 1.36 (1.19 – 1.55) | 0.98 (0.82 – 1.17) | 0.77 (0.65 – 0.91) |
| Health Insurance: Yes | 0.43 (0.22 – 0.94) | 0.43 (0.20 – 0.94) | 0.92 (0.28 – 3.03) | 1.08 (0.63 – 1.84) | 1.14 (0.56 – 2.32) | 0.72 (0.34 – 1.50) |
self-report sexual risk behaviors in last six months
controlling for other drugs of abuse (cannabis, street methadone) and alcohol use/abuse
Among those who were HIV negative, being married was associated with self-reporting any unsafe sex (AOR 1.36, 95% CI: 1.19 – 1.55) and was negatively associated with having multiple sex partners (AOR: 0.77, 95% CI 0.65 – 0.91). There were no associations between methamphetamine use and any sex risk behaviors among PWID who were HIV negative in multivariable analysis.
We did not note any statistically significant associations with methamphetamine use and injection risk behaviors among HIV positive or HIV negative PWID in multivariable analysis (data not shown).
Discussion
Among HIV positive PWID, methamphetamine was associated with several sexual risk behaviors. We did not, however, note any associations between methamphetamine and injection risk behaviors, including a lack of statistically significant differences in distributive and receptive sharing (note that less than 5% of the PWID reported either of these injection risk behaviors). This is one of the first studies to evaluate a predominately heterosexual population of methamphetamine users with respect to sexual risk behaviors in Southeast Asia. Findings support previous cross-sectional studies linking methamphetamine use to risky sexual behaviors among heterosexual drug using populations in the United States and South Africa (Corsi & Booth 2008; Molitor et al. 1998; Semple, Patterson & Grant 2004).
We observed several associations between current methamphetamine use and unsafe sexual behaviors in the last six months in multivariable analysis, including any unsafe sex and unsafe sex with primary partners among those that were HIV positive. These associations, however, were not present among those that were HIV negative.
The literature on sexual behaviors with respect to HIV serostatus remains inconsistent, with some studies documenting that HIV positive individuals aware of their status practice safer sex compared to HIV negative individuals or individuals who are unaware of their HIV serostatus (Noor et al. 2014). However, there are also studies that report that HIV positive individuals were less likely to report safe sex measures compared to HIV negative individuals or individuals unaware of their HIV serostatus (Edwards-Jackson et al. 2012).
Examining unsafe sex by HIV serostatus documented much higher rates of unsafe sex among HIV negative PWID (79%) vs HIV positive PWID (48%). As the level of unsafe sex among HIV negative PWID was very high, this creates a ceiling effect such that any impact of methamphetamine use on sexual risk behavior may be obscured. In contrast, the rate of unsafe sex among HIV positive PWID was less than 50%, thereby allowing for observing any potential impact of methamphetamine use on sexual risk behavior. Finally, for those that have been infected with HIV for long periods of time, maintenance of safe sex behavior may become problematic the longer they are infected with HIV (Crepaz et al. 2006), and could become particularly difficult for those who using drugs such as methamphetamine.
Over time, methamphetamine use can increase rates of unsafe sex among PWID, and this could lead to increased risk of HIV transmission to their sexual partners, who are likely part of the general population of Vietnam, female, and have a low overall HIV prevalence (less than 3%) (AIDS Healthcare Foundation 2017). As the sample of participants in this study included only PWID, further efforts should educate PWID on the risks associated with non-injection drug use and sexually transmission of HIV and other sexually transmitted diseases to sexual partners, particularly primary sexual partners.
There has been significant increases in methamphetamine use in Hai Phong, from 30% in 2014 to 51% in 2016 with almost all of the PWID reporting smoking methamphetamine. This study was conducted in response to the increase in methamphetamine use among PWID, as it is necessary to document how methamphetamine use can affect different risk behaviors among PWID. Several reports have highlighted the widespread availability of precursor chemicals coupled with the long established drug trafficking routes as reasons for the increase in amphetamine type stimulants, including methamphetamine, in South-East Asia (United Nations Office on Drugs and Crime 2012). Future studies should monitor this trend in methamphetamine use and whether it continues to be associated with risk behaviors. Although we did not note any associations between methamphetamine use and injection risk behaviors, likely due to the low levels of methamphetamine injection in our sample (less than 2%) coupled with low levels of sharing (less than 5%). However, this relationship should be monitored, particularly if PWID begin to inject methamphetamine in Hai Phong, as progressing to methamphetamine injection has been associated with much poorer outcomes over time compare to non-injection methamphetamine use (Novak & Kral 2011).
There are several public health implications from the results of this study. As the levels of non-injected methamphetamine have increased significantly in Hai Phong it is important to monitor trends in methamphetamine use, and whether this increased methamphetamine use continues to be associated with risky sexual behaviors, particularly among those PWID who are HIV positive. The increase in methamphetamine use indicates that there is a need for broader approaches for addressing methamphetamine and associated risks among PWID in Hai Phong. There are several study limitations. The data collected on sexual and injection risk behaviors are based on self-report. As there may be stigma related to reporting specific injection and sexual risk behaviors, there may be under-reporting of these risk behaviors. The data collected on injection and sexual risk behaviors among the PWID examined behaviors in the last six months, compared to current methamphetamine use, which was evaluated based on use in the last thirty days. The study was cross-sectional in nature, and does not permit causal inference. Finally, as the PWID in our study represent a RDS sample of the PWID population in Hai Phong, and may not be fully representative of PWID from the city, the results may not be generalizable to the entire PWID population in Hai Phong.
Conclusion
There has been a significant increase in methamphetamine use among PWID in Hai Phong from our initial evaluation in 2014 to the current study population from 2016-2017. In this study, we have documented statistically significant associations between current methamphetamine use and several sexual risk behaviors among HIV positive PWID. However, methamphetamine use was not associated with increased sexual risk behavior among HIV negative PWID. This is one of the first studies to document associations between sexual risk behaviors and methamphetamine use in Southeast Asia among a heterosexual population of PWID. It is important to continue to monitor ART adherence among HIV positive PWID who use methamphetamine, in order to prevent increases in viral load that could lead to transmission of HIV from PWID to their sexual partners. Finally, our study highlights the need for focused harm reduction on the dual epidemic of heroin and methamphetamine use among PWID.
Acknowledgments
This work was supported by grants from the ARNS (France) 12299 and NIDA (US) 1R01DA041978-01. The funding agencies had no role in designing the research, data analyses and preparation of the report.
References
- AIDS Healthcare Foundation 2017. Vietnam HIV Country Profile In: AIDS Healthcare Foundation (Ed.). Los Angeles, CA. [Google Scholar]
- Cherner M; Letendre S; Heaton R; Durelle J; Marquie-Beck J; Gragg B; Grant I & Group, H.N.R.C. 2005. Hepatitis C augments cognitive deficits associated with HIV infection and methamphetamine. Neurology 64(8):1343–1347. doi: 10.1212/01.WNL.0000158328.26897.0D. [DOI] [PubMed] [Google Scholar]
- Chettiar J; Shannon K; Wood E; Zhang R & Kerr T 2010. Survival sex work involvement among street-involved youth who use drugs in a Canadian setting. Journal of Public Health 32(3):322–7. doi: 10.1093/pubmed/fdp126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colfax GN; Buchbinder SP; Cornelisse PGA; Vittinghoff E; Mayer K & Celum C 2002. Sexual risk behaviors and implications for secondary HIV transmission during and after HIV seroconversion. AIDS 16(11):1529–1535. dpo ; 10.1097/00002030-200207260-00010. [DOI] [PubMed] [Google Scholar]
- Corsi K & Booth R 2008. HIV sex risk behaviors among heterosexual methamphetamine users: Literature review from 2000 to present. Current Drug Abuse Review 1(3):292–6. [DOI] [PubMed] [Google Scholar]
- Crepaz N; Lyles CM; Wolitski RJ; Passin WF; Rama SM; Herbst JH; Purcell DW; Malow RM; Stall R & Team, H.A.P.R.S. 2006. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS 20(2):143–157. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC; Thi Huong D; Thi Hai Oanh K; Khue Pham M; Thi Giang H; Thi Tuyet Thanh N; Arasteh K; Feelemyer J; Hammett T; Peries M; Michel L; Vu Hai V; Roustide MJ; Moles JP; Laureillard D & Nagot N 2016. Prospects for ending the HIV epidemic among persons who inject drugs in Haiphong, Vietnam. International Journal of Drug Policy 32:50–6. doi: 10.1016/j.drugpo.2016.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis RJ; Childers ME; Cherner M; Lazzaretto D; Letendre S & Group, H.N.R.C. 2003. Increased human immunodeficiency virus loads in active methamphetamine users are explained by reduced effectiveness of antiretroviral therapy. Journal of Infectious Diseases 188(12):1820–1826. doi: 10.1086/379894. [DOI] [PubMed] [Google Scholar]
- Garofalo R; Mustanski BS; McKirnan DJ; Herrick A & Donenberg GR 2007. Methamphetamine and young men who have sex with men: understanding patterns and correlates of use and the association with HIV-related sexual risk. Archives of Pediatrics & Adolescent Medicine 161(6):591–596. doi: 10.1001/archpedi.161.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hittner JB 2016. Meta-analysis of the association between methamphetamine use and high-risk sexual behavior among heterosexuals: American Psychological Association 30(2):147–57. doi: 10.1037/adb0000162. [DOI] [PubMed] [Google Scholar]
- Massanella M; Gianella S; Schrier R; Dan JM; Pérez-Santiago J; Oliveira MF; Richman DD; Little SJ; Benson CA & Daar ES 2015. Methamphetamine use in HIV-infected individuals affects T-cell function and viral outcome during suppressive antiretroviral therapy. Scientific reports 5:13179. doi: 10.1038/srep13179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molitor F; Ruiz J; Flynn N; Mikanda J; Sun R & Anderson R 1999. Methamphetamine use and sexual and injection risk behaviors among out-of-treatment injection drug users. American Journal of Drug and Alcohol Abuse 25(3):475–493. [DOI] [PubMed] [Google Scholar]
- Molitor F; Truax SR; Ruiz JD & Sun RK 1998. Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. Western Journal of Medicine 168(2):93. [PMC free article] [PubMed] [Google Scholar]
- Moore DJ; Blackstone K; Woods SP; Ellis RJ; Atkinson JH; Heaton RK; Grant I; Group, H. & Group, T. 2012. Methamphetamine use and neuropsychiatric factors are associated with antiretroviral non-adherence. AIDS Care 24(12):1504–13. doi: 10.1080/09540121.2012.672718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Hygiene and Epidemiology, F.V., United States Agency for International Development (USAID), 2011. Results from the HIV/STI Integrated Biological and Behavioral Surveillance (IBBS) in Vietnam. In: Ministry of Health; (Ed.). [Google Scholar]
- Novak SP & Kral AH 2011. Comparing injection and non-injection routes of administration for heroin, methamphetamine, and cocaine users in the United States. Journal of Addictive Diseases 30(3):248–57. doi: 10.1080/10550887.2011.581989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkham S SK 2015. A Global Review of the Harm Reduction Response to Amphetamines: A 2015 Update In: Harm Reduction International (Ed.). London: International Harm Reduction Association. [Google Scholar]
- Reback C; Larkins S & Shoptaw S 2003. Methamphetamine abuse as a barrier to HIV medication adherence among gay and bisexual men. AIDS Care 15(6):775–785. doi: 10.1080/09540120310001618621. [DOI] [PubMed] [Google Scholar]
- Russell K; Dryden DM; Liang Y; Friesen C; O’Gorman K; Durec T; Wild TC & Klassen TP 2008. Risk factors for methamphetamine use in youth: a systematic review. BMC Pediatrics 8:48. doi: 10.1186/1471-2431-8-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salamanca SA; Sorrentino EE; Nosanchuk JD & Martinez LR 2015. Impact of methamphetamine on infection and immunity. Frontiers in Neuroscience 8:445. doi: 10.3389/fnins.2014.00445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple SJ; Patterson TL & Grant I 2004. The context of sexual risk behavior among heterosexual methamphetamine users. Addictive Behaviors 29(4):807–810. doi: 10.1016/j.addbeh.2004.02.013. [DOI] [PubMed] [Google Scholar]
- StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- United Nations Office on Drugs and Crime 2016. World Drug Report 2016. In: United Nations; (Ed.). Vienna. [Google Scholar]
- UNODC. 2012. Amphetamine-Type Stimulants in Vietnam: Revie of the Availability, Use and Implications for Health and Security In: UNODC (Ed.) “Support for developing effective ATS prevention strategies and measures for East Asia: A Pilot in Viet Nam”. [Google Scholar]
- UNODC 2017. Synthetic drugs from Asia are fuelling global public health and crime concerns. In: UNODC Vietnam; (Ed.). Hanoi. [Google Scholar]
- World Health Organization 2006. Management of Substance Abuse. [Google Scholar]
- Ye L; Peng J; Wang X; Wang Y; Luo G & Ho W 2008. Methamphetamine enhances Hepatitis C virus replication in human hepatocytes. Journal of Viral Hepatitis 15(4):261–270. [DOI] [PMC free article] [PubMed] [Google Scholar]